Abstract
γδ T cells express several different toll-like receptor (TLR)s. The role of MyD88- dependent TLR signaling in TCR activation of murine γδ T cells is incompletely defined. Here, we report that Pam3CSK4 (PAM, TLR2 agonist) and CL097 (TLR7 agonist), but not lipopolysaccharide (TLR4 agonist), increased CD69 expression and Th1-type cytokine production upon anti-CD3 stimulation of γδ T cells from young adult mice (6-to 10-week-old). However, these agonists alone did not induce γδ T cell activation. Additionally, we noted that neither PAM nor CL097 synergized with anti-CD3 in inducing CD69 expression on γδ T cells of aged mice (21-to 22-month-old). Compared to young γδ T cells, PAM and CL097 increased Th-1 type cytokine production with a lower magnitude from anti-CD3- stimulated, aged γδ T cells. Vγ1+ and Vγ4+ cells are two subpopulations of splenic γδ T cells. PAM had similar effects in anti-CD3-activated control and Vγ4+ subset- depleted γδ T cells; whereas CL097 induced more IFN-γ production from Vγ4+ subset-depleted γδ T cells than from the control group. Finally, we studied the role of MyD88-dependent TLRs in γδ T cell activation during West Nile virus (WNV) infection. γδ T cell, in particular, Vγ1+ subset expansion was significantly reduced in both MyD88- and TLR7- deficient mice. Treatment with TLR7 agonist induced more Vγ1+ cell expansion in wild-type mice during WNV infection. In summary, these results suggest that MyD88-dependent TLRs provide co-stimulatory signals during TCR activation of γδ T cells and these have differential effects on distinct subsets.
Introduction
γδ T cells are a minority of CD3+ T cells in lymphoid tissue and blood of humans and rodents, but are well represented at epithelial and mucosal sites [1]. They can rapidly proliferate after parasitic, bacterial, and viral infections and produce inflammatory cytokines, such as IFN-γ and TNF-α [2]–[6]. These cells lack major histocompatibility complex (MHC) restriction and have the potential capacity to respond to antigens without a requirement for conventional antigen processing [7], [8]. Unlike αβ T cells, there are few antigens recognized by γδ T cell receptor [9]. Human Vδ2 T cells recognize small bacterial phosphoantigens, alkylamines and synthetic aminobisphosphonates; whereas Vδ1 T cells recognize stress-inducible MHC-related molecules-MICA/B and other ligands [10], [11]. The class I molecules, including class Ib, and CD1d, are ligands for some murine γδ T cells [12]–[14]. In addition, both murine and human γδ T cells recognize the algae protein phycoerythrin [15]. Taken together, these unique features suggest that γδ T cells play a role in innate immunity during microbial infection. However, the underlying immune mechanisms of γδ T cell activation are not clearly understood.
Toll-like receptors (TLRs) play a fundamental role in host innate immunity by mounting a rapid and potent inflammatory response to pathogen infection by their recognition of conserved structural patterns in diverse microbial molecules. They are expressed by a wide range of cells, including both immune cells and non-immune cells. The core TLR signaling pathway (except for TLR3) utilizes myeloid differentiation factor 88 (MyD88) as the primary adaptor [16]–[18]. Mouse and human γδ T cells express TLR2, TLR3, TLR4 and TLR7/8 [19]–[23]. Some studies suggest TLR-mediated signaling pathways can indirectly activate γδ T cells, mainly via cross- talk between these cells and dendritic cells (DCs) [24]–[27]. For human γδ T cells, TLR ligands are also known to co-stimulate TCR-activation. For example, TLR2, TLR3 and TLR5 ligands induced higher cytokine production and increased expression of cell surface activation markers [28]–[30]. However, the direct effect of TLR ligands on activation of murine γδ T cells is not clearly defined. In this study, we investigated the role of MyD88-dependent TLRs in activating murine γδ T cells.
Materials and Methods
Mice
6-to 10-week-old control C57BL/6 (B6), TLR4 deficient (TLR4−/−) mice and 21-to 22-month-old B6 mice were purchased from Jackson Laboratories (Bar Harbor, ME) and the National Institute of Aging (Bethesda, MD), respectively. MyD88−/− mice were bred to the B6 background by backcrossing for 10 successive generations [31], [32]. TLR7−/− mice (B6×129 F2 background) were obtained from Regeneron Inc. (Tarrytown, NY) and bred to the B6 background by backcrossing for 7 successive generations [33], [34]. Groups were age- and sex-matched for each experiment and housed under identical conditions. This study was carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. All animal experiments were approved by the Animal Care and Use Committee at the University of Texas Medical Branch (Permit #0902011).
Stimulation of γδ T cells with anti-CD3 with or without TLR agonists
γδ T cells were purified from the pooled spleens of 3–5 mice by using a TCRγ/δ+ T Cell Isolation Kit according to the manufacturer's instructions (Miltenyi Biotec, Auburn, CA). The purity of γδ T cells was examined by staining with streptavidin-PE and anti-CD3 FITC. γδ T cells (1×105 cells/well) were cultured for 2 days at 37°C in RPMI-1640 medium (Invitrogen, Carlsbad, CA) in 96-well plates coated with 5 µg/ml anti-CD3 (eBioscience, San Diego, CA) in the presence of 1 µg/ml of Pam3CSK4 (PAM, Invivogen, San Diego, CA), or 10 µg/ml of lipopolysaccharide (LPS, Sigma, St. Louis, MO) or 1 µg/ml of CL097 (Invivogen). At 48 h post-treatment, cells were harvested and stained for cell surface markers. Culture supernatant was harvested for measurement of cytokine production.
Flow cytometry
Cells were stained with monoclonal antibody (mAb) GL3-FITC (hamster anti-mouse TCRδ, BD Biosciences, San Diego, CA), and/or Abs for CD3, CD25, and CD69 (e-Bioscience). In some experiments, γδ T cells were labeled with 2.5 µM carboxyfluorescein succinimidyl ester (CFSE) according to the manufacturer's instructions (Invitrogen) and cultured at 1×105 cells/well for 48 h. γδ T cell proliferation was assessed by flow cytometric analysis of CFSE dilution. After staining, cells were fixed with 0.5% paraformaldehyde in PBS and examined by using a C6 Flow Cytometer (Accuri cytometers, Ann Arbor, MI). To study TLR7 expression, cells were stained with Abs for Vγ1, or Vγ4, fixed in 2% paraformaldehyde, and permeabilized with 0.5% saponin before adding PE-conjugated anti-TLR7 or control IgG (Thermo Scientific Pierce, Waltham, MA). Data were analyzed by using CFlow Plus (Accuri cytometers).
In vivo depletion of γδ subpopulations
Vγ4 T-cell depletion was achieved by two consecutive injections of 100 µg of hamster anti-Vγ4 (mAb UC3, purified from hybridoma culture supernatants [35] intraperitoneally (i.p.). at 2 days and 24 h before mice were euthanized for tissue harvesting [36], [37]. Sham Ab treatments were performed with the same amount of hamster IgG isotype (Innovative Research, Southfield, MI).
Cytokine assays
Culture supernatant was collected for analysis of cytokine production by using a Bio-Plex Pro Mouse Cytokine Assay (Bio-Rad, Hercules, CA) or an ELISA (BD Bioscience).
West Nile virus (WNV) infection in mice
The WNV NS4B-P38G attenuated mutant infectious clone-derived virus [38] was passaged once in Vero cells to make a virus stock for infection studies. Mice were inoculated i.p. with 1500 plaque forming units (PFU) of WNV NS4B-P38G mutant. In some experiments, mice were injected i.p. with 30 µg of R848 (R848 VacciGrade, Invivogen) [39] 4 h before WNV infection. At various time points post-infection, splenocytes were harvested from WNV- infected mice and non-infected controls and stained for CD3 and TCRγδ.
Statistical analysis
Data analysis was performed by using Prism software (Graph-Pad) statistical analysis. Values for phenotype analysis and cytokine production experiments were presented as means ± SEM. P values of these experiments were calculated with a non-paired Student's t test or Mann-Whitney test. Statistical significance was accepted at P<0.05.
Results
TLR2 and TLR7, but not TLR4 agonists act in synergy with anti-CD3 treatment in the activation of murine γδ T cells in vitro
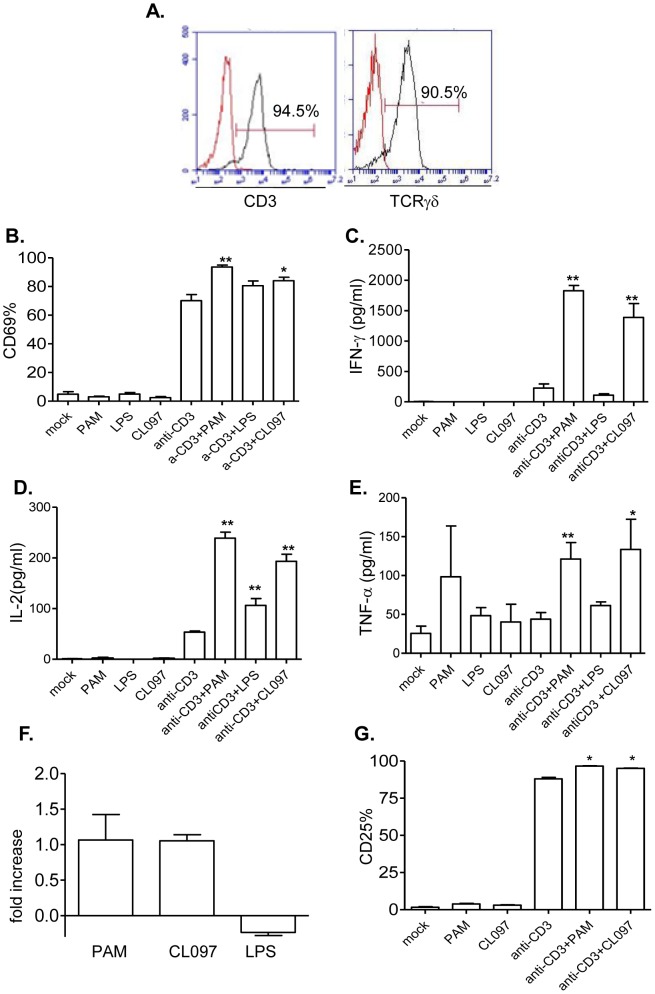
Murine γδ T cells express TLR2, TLR3, TLR4 and TLR7 [18], [21]. Here, we examined the role of MyD88-dependent TLR ligands in activating murine γδ T cells. We isolated splenic γδ T cells of B6 mice by magnetic beads. Flow cytometry analysis showed that the purified cells were more than 90% positive for CD3 or TCRγδ ( Figure 1A ). These cells were next treated with anti-CD3 and TLR agonists, including PAM (Pam3CSK4, TLR2 ligand), LPS (TLR4 ligand) or CL097 (TLR7 ligand). At 48 h after the treatment, we detected about 70% upregulation of the early activation marker- CD69 expression on anti-CD3-stimulated γδ T cells ( Figure 1B ). PAM, LPS or CL097 alone did not induce CD69 expression. However, PAM and CL097 increased CD69 expression by 33% or 20% respectively, when used together with anti-CD3 (P<0.01 or P<0.05). LPS did not have the same effect on CD69 expression (Figure 1B). We also measured T- helper 1 (Th1) -type cytokine production in cell culture supernatant. Both PAM and CL097 synergized with anti-CD3 in inducing IFN-γ, IL-2 and TNF-α production from γδ T cells (P<0.01 or P<0.05); whereas LPS did not have the same effect, except in the study with anti-CD3-treated γδ T cells from which IL-2 was produced ( Figure 1C–E , P>0.05). Furthermore, none of the TLR agonists could induce γδ T cell proliferation by itself (data not shown). However, PAM and CL097, but not LPS increased γδ T cell number following treatment with anti-CD3 ( Figure 1F ). Concurrent with these findings, PAM and CL097 also enhanced CD25 expression on anti-CD3-treated γδ T cells ( Figure 1G , P<0.05).
Figure 1. The effects of TLR2, 4 and 7 agonists on anti-CD3- treated murine γδ T cells.
A, Flow cytometry analysis of splenic γδ T cells stained with antibodies to TCRγδ and CD3. B–E, splenic γδ T cells were cultured with anti-CD3 with or without TLR agonists. Cells were harvested at 48 h post-stimulation and examined for CD69 expression (B), and IFN-γ (C), IL-2 (D) and TNF-α (E) production in culture supernatant. F. In vitro T cell proliferation assay. CFSE- labeled γδ+ T cells were cultured for 48 h in the presence of anti-CD3 with or without TLR agonists. Data shown are fold of increase of T cell proliferation compared to anti-CD3 treated cells. G. CD25 expression. Data are presented as means ± SEM, n = 4–7. ** P<0.01 or * P<0.05 compared to anti-CD3- treated cells. Data presented are one representative of at least four similar experiments.
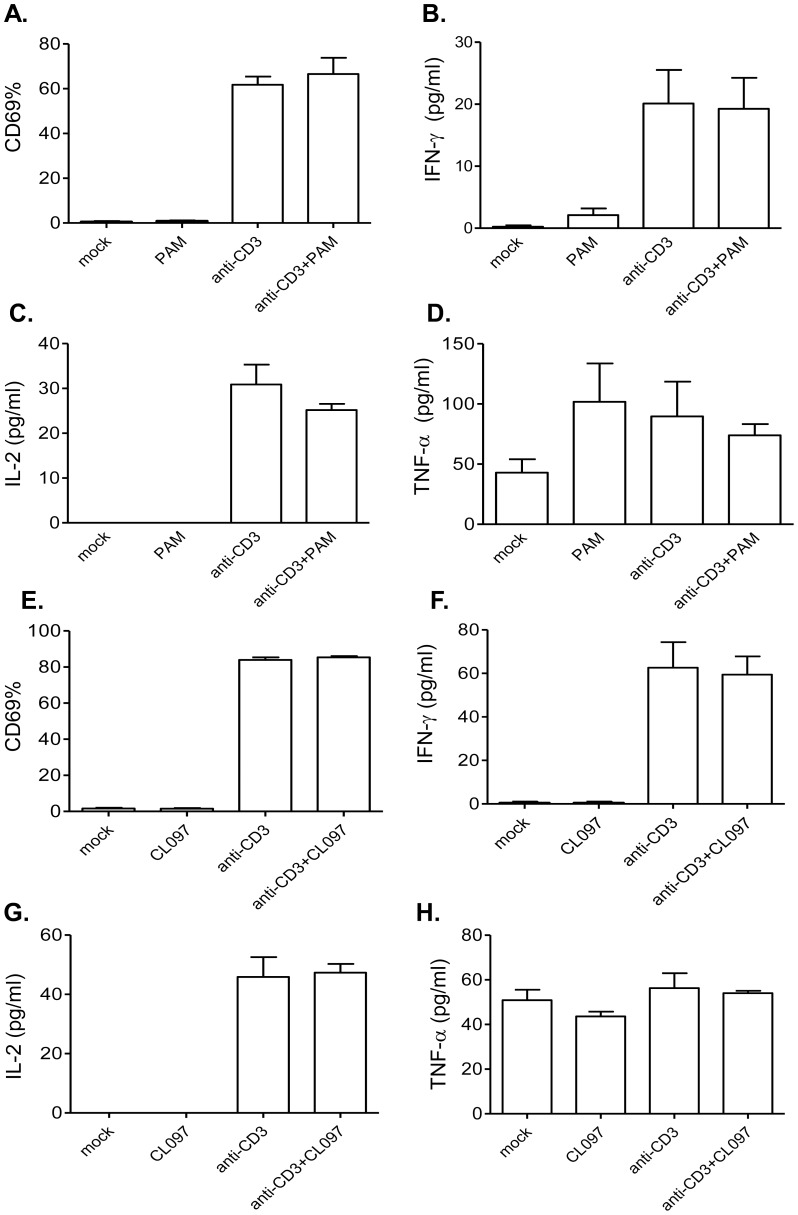
To verify these findings, we next measured CD69 expression and Th-1 type cytokine production from γδ T cells of MyD88−/− or TLR7−/− mice following 48 h of stimulation with anti-CD3 and PAM or CL097. As found in wild-type γδ T cells, anti-CD3 induced CD69 expression and Th-1 type cytokine production from γδ T cells isolated from MyD88−/− ( Figure 2A–D ) or TLR7−/− mice ( Figure 2E–H ). Neither PAM nor CL097 had synergistic effects with anti-CD3 in inducing the expression of CD69 ( Figures 2A & 2E , P>0.05) and IFN-γ, IL-2 and TNF-α production ( Figures 2B–D & 2F–H , P>0.05). Furthermore, LPS treatment had the same effect on anti-CD3-activated γδ T cells of TLR4−/− mice, compared to that on wild-type γδ T cells (Figure S1, P>0.05). These data suggest that TLR2 and TLR7 act as co-stimulatory factors during in vitro TCR-activation of murine γδ T cells.
Figure 2. The effects of TLR2 and TLR7 ligands on anti-CD3- activated γδ T cells isolated from MyD88−/− and TLR7−/− mice.
Splenic γδ T cells of MyD88−/− (A–D) or TLR7−/− mice (E–H) were cultured with anti-CD3 with or without TLR agonists. Cells were harvested at 48 h post-stimulation and analyzed for CD69 expression (A) & (E) and IFN-γ (B) & (F), IL-2 (C) & (G) and TNF-α (D) & (H) production in culture supernatant. Data are presented as means ± SEM, n = 3–4. ** P<0.01 or * P<0.05 compared to anti-CD3- treated cells. Results presented are one representative of three similar experiments.
Effects of TLRs 2 and 7 agonists on the activation of γδ T cells from aged mice
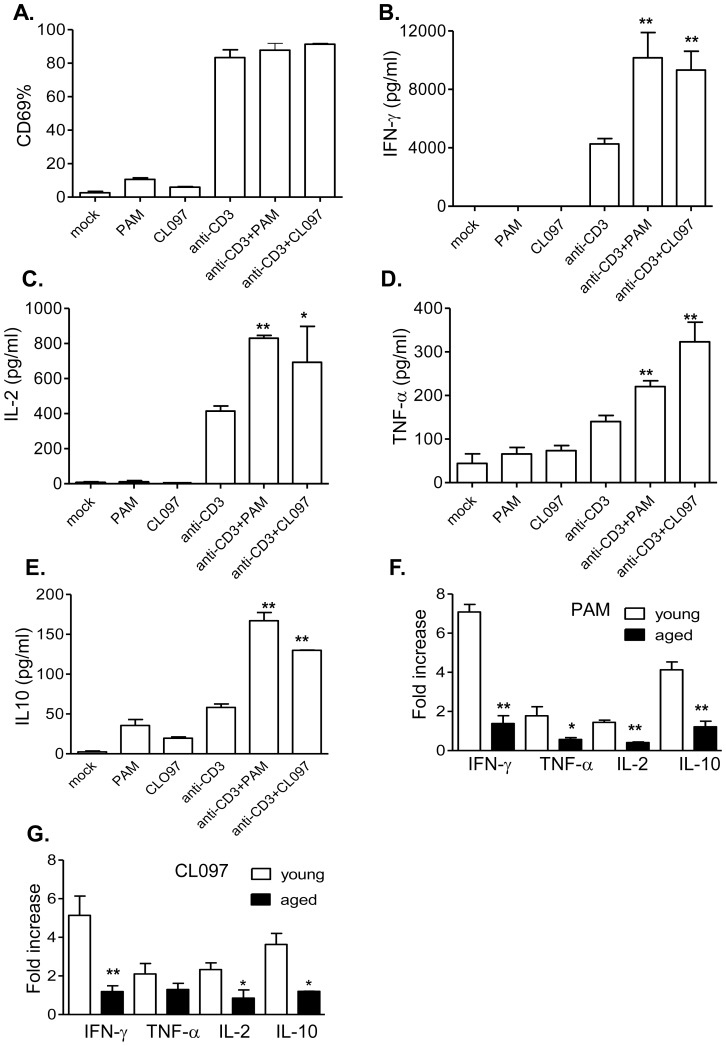
Age-associated dysregulation of TLR signaling has been reported to contribute to the increased morbidity and mortality from infectious diseases found in geriatric patients [40], [41]. γδ T cells are also known to display numerical and functional alteration with aging [37], [42]–[44]. Nevertheless, the role of TLRs in dysfunction of aged γδ T cells is not well understood. Here, we isolated γδ T cells from aged (21-to 22-month-old) B6 mice and stimulated them with anti-CD3 and TLRs 2 and 7 agonists. Although anti-CD3 induced CD69 expression on aged γδ T cells, neither PAM nor CL097 increased CD69 expression when treated with anti-CD3 ( Figure 3A , P>0.05). PAM or CL097 enhanced the production of IFN-γ, IL-2, and TNF-α from anti-CD3 stimulated aged γδ T cells ( Figure 3B–3D , P<0.01 or P<0.05). We also measured the production of regulatory cytokines, including IL-10 and TGF-β. Both PAM and CL097 increased the production of IL-10 following anti-CD3 treatment on aged γδ T cells ( Figure 3E , P<0.01). No changes in TGF-β levels were noted following any of the treatments on γδ T cells (data not shown). Furthermore, the magnitude of the synergistic effects of TLR agonists with anti-CD3 was much lower compared to that in young γδ T cells ( Figure 3F & 3G , P<0.05 or P<0.01), except for induction of TNF-α production following CL097 and anti-CD3 treatment ( Figure 3G , P>0.05). These results indicate that TLR2 and TLR7 have reduced co-stimulatory effects on activating γδ T cells of aged mice.
Figure 3. The effects of TLR2 and TLR7 ligands on anti-CD3- activated γδ T cells of aged mice.
Splenic γδ T cells isolated from aged mice were cultured with anti-CD3 with or without TLR agonists. Cells were harvested at 48 h post-stimulation and analyzed for CD69 expression (A) and the production of IFN-γ (B), IL-2 (C), TNF-α (D) and IL-10 (E) in culture supernatant. Data are presented as means ± SEM, n = 3–8. ** P<0.01 or * P<0.05 compared to anti-CD3- treated alone. F–G. Fold of increase of cytokine production by TLR2 (E) or TLR7 agonists (F) of young and aged γδ T cells compared to anti-CD3 treated alone. ** P<0.01 compared to young γδ T cells.
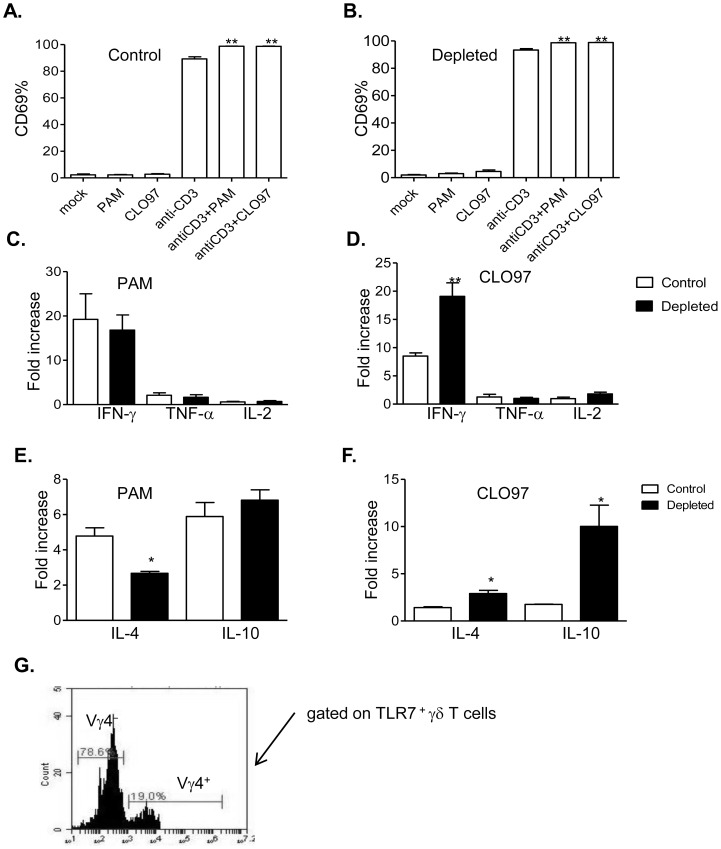
Effects of TLRs 2 and 7 agonists on activation of γδ T cells in the absence of Vγ4+ subsets
γδ T cells are divisible into functionally distinct subsets, which distribute in an organ-specific manner [45]. Vγ1+ and Vγ4+ T cells represent two major populations of splenic γδ T cells in B6 mice [37]. We evaluated the effects of TLRs 2 and 7 agonists on splenic Vγ4+ T cell activation. Mice were first depleted with control IgG or Vγ4+ antibodies, as described before [36], [37]. Next, γδ T cells were isolated and stimulated in vitro with anti-CD3 and TLR agonists. Both PAM and CL097 increased CD69 expression on anti-CD3-treated controls and Vγ4+ cell-depleted γδ T cells ( Figure 4A & 4B , P<0.01 or P<0.05). Further, PAM enhanced the production of all three cytokines from anti-CD3 stimulated cells in both groups in a similar manner ( Figure 4C , P>0.05). Compared to the control group, CL097 induced more IFN-γ production from anti-CD3 activated -γδ T cells that were depleted of Vγ4+ cells ( Figure 4D , P<0.01). To determine the regulatory role of Vγ4+ T cells, we next measured IL-4 and regulatory cytokine production. While no changes in TGF-β expression was noted following the treatment (data not shown), PAM induced less IL-4 production from anti-CD3 treated -Vγ4+ cell-depleted γδ T cells compared to the control group ( Figure 4E , P<0.05). CL097 treatment induced more IL-4 and IL-10 production from Vγ4+ cell-depleted cells following anti-CD3 stimulation ( Figure 4F , P<0.05). Finally, we determined TLR7 expression on the two splenic γδ T cell subsets. We found that nearly 80% of TLR7-positive γδ T cells were Vγ4−; while only 20% were Vγ4+ cells ( Figure 4G ). Thus, these results indicate that the differences in TLR7 expression among γδ T cell subsets contribute to a differential co-stimulatory effect of TLR7 agonist on these cells.
Figure 4. The effects of TLR2 and TLR7 ligands on anti-CD3- activated γδ T cells depleted of Vγ4+ subsets.
Splenic γδ T cells isolated from mice depleted with control IgG or antibody to Vγ4+ were cultured with anti-CD3 with or without TLR agonists. Cells were harvested at 48 h post-stimulation and analyzed for CD69 expression. A. Control group. B. Vγ4+ cell-depleted γδ T cells. C–F. Fold of increase of Th-1 cytokine, IL-4 and IL-10 production by TLR2 (C–E) or TLR7 agonists (D–F) of Control and Vγ4+ cell-depleted γδ T cells compared to anti-CD3 treated alone. ** P<0.01 compared to young mice. ** P<0.01 or * P<0.05 compared to anti-CD3- treated alone. G. γδ T cells were stained with Abs for γδ T cell subsets and TLR7. TLR7-positive cells were gated for phenotypic analysis of γδ T cell subsets. ** P<0.01 or * P<0.05 compared to Vγ4+ cell-depleted γδ T cells. Results presented are one representative of three similar experiments.
Role of TLR7 in γδ T cell activation and expansion in response to WNV infection
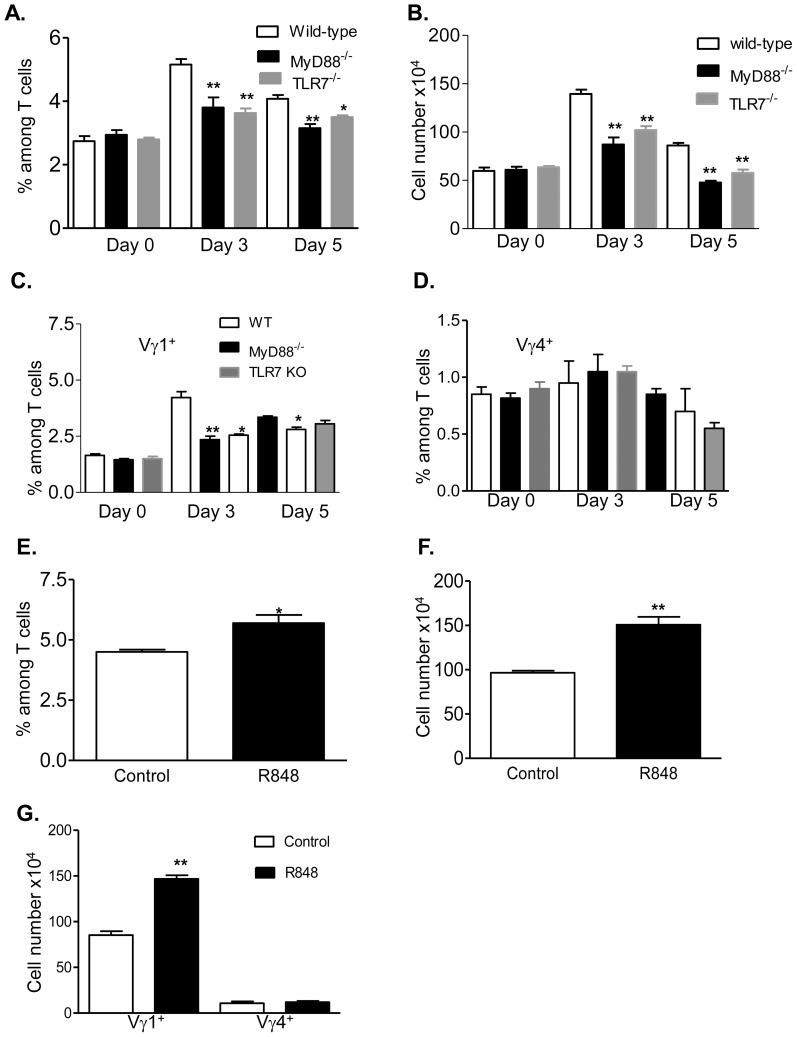
WNV is a mosquito-borne flavivirus with a positive-sense, single-stranded RNA genome. Following wild-type WNV infection, γδ T cells expand significantly in mice, produce IFN-γ and protect the host from lethal encephalitis [46]. TLR7 is required for host protective immunity during wild-type or the attenuated WNV NS4B-P38G mutant infection [32], [34], [47]. To determine the role of MyD88-dependent TLR signaling in γδ T cell activation during WNV NS4B-P38G mutant infection, splenocytes were isolated and assessed before infection (day 0) and at early (day 3) and later (day 5) intervals post infection. The percentage of γδ T cells in wild-type mice increased significantly at day 3 post infection, and decreased though remained higher than non-infected controls at day 5 post-infection. The percentage of γδ T cells was also increased in MyD88−/−or TLR7−/− mice at day 3, but became not significant at day 5 following infection ( Figure 5A , P>0.05). In comparison to wild-type mice, the magnitude of γδ T cell expansion at day 3 post-infection was much lower in MyD88−/− and TLR7−/− mice ( Figure 5B , P<0.05 or P<0.01). Among splenic γδ T cells, Vγ1+ subsets in wild-type mice increased significantly at days 3 and 5 post-infection. The magnitude of Vγ1+ T cell expansion in MyD88−/− or TLR7−/− mice was reduced at day 3 and remained lower in MyD88−/− mice at day 5 post-infection ( Figure 5C , P<0.05 or P<0.01). No changes were observed on Vγ4+ T cells in these mice following infection ( Figure 5D , P>0.05). Furthermore, treatment with R848–a TLR7 agonist reduced viral load and increased host survival following WNV infection (Xie G. and Wang T. et al. manuscript in preparation). Here, we infected mice with the WNV NS4B-P38G mutant following i.p. injection with R848. As shown in Figure 5E , R848-treated mice had more γδ T cell expansion than did the control group, as analyzed by both percentage among splenic T cells ( Figure 5F , P<0.05) and the total cell number (P<0.01). In further phenotypic analysis of γδ T cells in these mice, we found that R848 treatment increased the expansion of Vγ1+ T cells, but not Vγ4+ T cells ( Figure 5G , P<0.01). In summary, these results suggest to us that TLR7-MyD88 signaling is involved in the expansion of γδ T cells in particular, Vγ1+ T cells during WNV infection.
Figure 5. TLR7-mediated γδ T cell activation during WNV infection.
Splenic T cells of wild type, MyD88−/− and TLR7−/− mice were isolated before infection (day 0) and at days 3 and 5 post-infection and stained for TCRγδ, Vγ1+, Vγ4+ and CD3. ** P<0.01 or * P<0.05 compared to wild-type mice. A. Total γδ+ percentage among splenic T cells. B. Splenic γδ cell number per mouse. C–D. Vγ1+ (C) or Vγ4+ (D) percentage among splenic T cells. E–G. Wild-type B6 mice were injected with R848 followed by infection with WNV NS4B-P38G mutant. Cells were harvested at day 3 post-infection and stained for TCRγδ, Vγ1+, Vγ4+ and CD3. E. Total γδ+ percentage among splenic T cells. F. Splenic γδ cell number per mouse. G. Total number of Vγ1+ and Vγ4+ cells per mouse. ** P<0.01 or * P<0.05 compared to control group.
Discussion
Besides TCR, γδ T cells express different types of TLRs [19]–[22]. It is known that the TLR-mediated signaling pathways are indirectly involved in γδ T cell activation in mice and humans, mainly via cross- talk with DCs [24]–[27]. Others also reported that TLR ligands co-stimulated IFN-γ and chemokine secretion in TCR-activated human γδ T cells [28], [29]. In this study, we have identified TLR2 and TLR7 as co-stimulating factors during in vitro TCR-activation of murine γδ T cells in inducing CD69 expression and Th-1-type cytokine production. Increasing evidence suggests that TLR-mediated signaling pathways alter with aging [40], [48]. One early study by Colonna-Romano et al. showed that γδ T cells from old people and centenarians with enhanced levels of CD69 both after culture in medium alone and in TLR ligand-stimulated cells [49]. Here, we found that TLR2 and TLR7 agonists failed to induce higher CD69 expression and produced less Th-1 type cytokines upon anti-CD3 stimulation of aged γδ T cells compared to young γδ T cells. In addition, increased levels of CD69 expression were noted on γδ T cells of aged mice after culture in medium alone. One possibility is that aging is often associated with increasing levels of both proinflammatory cytokine and regulatory cytokines, like IL-10 and TGF-β [50], [51]. Nevertheless, we found TGF-β levels unchanged after treatment. The magnitude of induction of IL-10 by PAM and CL097 was also reduced on aged γδ T cells after anti-CD3 treatment. The dysregulation of TLR signaling has been associated with impaired functions of monocytes, DCs, and macrophages with aging [52]. Here, our results indicate an impaired TLR signaling contributes to the dysfunction of γδ T cells in aged mice.
The Vγ4+ subset is a subpopulation of splenic γδ T cells. CL097 induced more IFN-γ production from non-Vγ4+ γδ T cells (most Vγ1+ T cells) compared to total splenic γδ T cells. One possibility is that Vγ4+ γδ T cells may exert a regulatory role on Vγ1+ T cells. Murine Vγ1+ and Vγ4+ T cells were reported to regulate each other's activity via secreting Th2 and regulatory cytokines [36], [53]. Nevertheless, we noted that there were more IL-4 and IL-10 induced by CL097 upon anti-CD3 treatment on non-Vγ4+ T cells. Furthermore, while we noted PAM had the same effect in activating Vγ4+ T cells and non- Vγ4+ γδ T cells, there was less IL-4 induction by PAM on anti-CD3 treated non-Vγ4+ T cells than control group. It seems to be unlikely that these cytokines contribute to a reduced costimulatory effect of CL097. Moreover, we found that TLR7 expression was higher on non-Vγ4+ T cells than on Vγ4+ T cells. Thus, the differences in TLR7 expression among splenic γδ T cell subsets lead to a differential co-stimulatory effect of TLR7 ligand upon TCR activation. γδ T cells are also the major producer of IL-17 during the early stage of some microbial infection [54], [55]. It is known that distinct γδ T cell subpopulations are committed to produce IFN-γ and IL-17 [56]. In particular, Vγ4 T cell-producing IL-17 contributes to the exacerbation of many diseases, such as collagen-induced arthritis [57], autoimmune encephalomyelitis [55] or psoriasis [58]. Interestingly, the MyD88-dependent TLRs, including TLR2 or 4, are required for the IL-17A response of Vγ4 T cells [59], [60]. Therefore, we conclude that the co-stimulatory effects of TLR ligands on γδ subsets may vary depending on induced cytokine profile and/or TLR expression levels.
The underlying mechanisms of γδ T cell activation during microbial infection are not clearly understood. Previous studies showed that γδ T cell activation in response to Borrelia burgdorferi infection in a TLR2-dependent manner, suggesting an involvement of MyD88 signaling during in vivo activation [25], [61]. The TLR7-mediated signaling pathway is known to protect the host from lethal WNV infection mainly by promoting IL- 23-dependent immune cell infiltration and homing to the central nervous system [32]. In this study, our results suggest TLR7/MyD88 signaling pathways are involved in γδ T cell activation during WNV infection. Among splenic γδ T cells, Vγ1+ but not Vγ4+ population, expanded and were activated quickly in response to WNV infection [37]. We have previously shown that Vγ4+ T cell- depleted mice had a higher expansion of Vγ1+ T cells and were more resistant to WNV infection [36]. Here, we reported that TLR7 signaling preferentially mediated Vγ1+ T cell expansion during WNV infection and had a stronger co-stimulatory effect on IFN-γ- induction from Vγ1+ T cells upon TCR activation. This is mainly due to a higher expression of TLR7 on this subset. Moreover, Vγ1+ T cells of aged mice exhibited a slower and reduced response to WNV infection, which partially contributes to the higher susceptibility to WNV encephalitis [37]. Results from this study now suggest that the reduced effector functions of γδ T cells could be due to the dysregulation of TLR signaling pathways in aged mice. γδ T cell expansion and activation is an important event in host immunity during WNV infection, which is involved in many protective activities, including controlling WNV dissemination and facilitating memory T cell development [46], [62]. Here, we have mainly focused on studying the IFN-γ-producing activity of γδ T cells as it was known to play a predominant role in host protection against lethal WNV infection. For example, adoptive transfer of the splenocytes from TCRβ−/−IFNγ−/− mice, which have a defect in the IFN-γ-producing capacity of γδ T cells, did not affect host susceptibility in TCRδ−/− mice [46]. Further, irradiated mice reconstituted with IFN-γ-deficient γδ T cells had enhanced levels of viral loads in blood and brain during WNV infection compared to mice reconstituted with IFN-γ sufficient γδ T cells [63]. The cytolytic function is another important mechanism of viral control attributed to γδ T cells. Future studies will also be focused on investigation of innate immune factors regulating CTL activity during WNV infection. Overall, our data suggests that the MyD88-dependent TLRs are required for the activation and expansion of γδ T cells during microbial infection. γδ T cells are known to form a unique link between innate and adaptive immunity. Due to their unique role in host immunity, understanding of the underlying mechanisms of γδ T cell activation in response to pathogen infection may provide important insights into immunotherapy and vaccine development.
Supporting Information
The effects of LPS on anti-CD3- activated γδ T cells of TLR4−/− mice. Splenic γδ T cells were cultured with anti-CD3 with or without LPS. Cells were harvested at 48 h post-stimulation and analyzed for CD69 expression (A) and the production of IFN-γ (B), IL-2 (C) and TNF-α (D) in culture supernatant. ** P<0.01 or * P<0.05 compared to anti-CD3- treated alone. Results presented are one representative of two similar experiments.
(TIF)
Acknowledgments
We thank Regeneron Inc., Dr. Richard Flavell (Howard Hughes Medical Institute, Yale University School of Medicine, New Haven) and Dr. Shizuo Akira (Osaka University, Japan) for providing the TLR7−/− and MyD88−/− mice. We also thank Tao Wang for technical support and Ms. Mardelle Susman for assisting in manuscript preparation.
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by a NIH grant to T.W. (R01AI072060). G.X. was supported by a fellowship from the Sealy Center for Vaccine Development at UTMB. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Hayday AC (2000) Gammadelta cells: a right time and a right place for a conserved third way of protection. Annu Rev Immunol 18: 975–1026. [DOI] [PubMed] [Google Scholar]
- 2. Perera M, Carter R, Goonewardene R, Mendis KN (1994) Transient increase in circulating g/d T cells during Plasmodium vivax malarial paroxysms. Journal of Experimental Medicine 179: 311–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Barnes PF, Grisso CL, Abrams JS, Band H, Rea TH, et al. (1992) gd T lymphocytes in human tuberculosis. Journal of Infectious Diseases 165: 506–512. [DOI] [PubMed] [Google Scholar]
- 4. Hara T, Mizuno Y, Takaki K, Takada H, Akeda H, et al. (1992) Predominant activation and expansion of V gamma 9-bearing gamma delta T cells in vivo as well as in vitro in Salmonella infection. J Clin Invest 90: 204–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dechanet J, Merville P, Lim A, Retiere C, Pitard V, et al. (1999) Implication of gammadelta T cells in the human immune response to cytomegalovirus. J Clin Invest 103: 1437–1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kabelitz D, Wesch D (2001) Role of gamma delta T-lymphocytes in HIV infection. Eur J Med Res 6: 169–174. [PubMed] [Google Scholar]
- 7. Ferrick DA, King DP, Jackson KA, Braun RK, Tam S, et al. (2000) Intraepithelial gamma delta T lymphocytes: sentinel cells at mucosal barriers. Springer Semin Immunopathol 22: 283–296. [DOI] [PubMed] [Google Scholar]
- 8. Wang L, Kamath A, Das H, Li L, Bukowski JF (2001) Antibacterial effect of human V gamma 2V delta 2 T cells in vivo. J Clin Invest 108: 1349–1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Born WK, O'Brien RL (2009) Antigen-restricted gammadelta T-cell receptors? Arch Immunol Ther Exp (Warsz) 57: 129–135. [DOI] [PubMed] [Google Scholar]
- 10. Carding SR, Egan PJ (2002) Gammadelta T cells: functional plasticity and heterogeneity. Nat Rev Immunol 2: 336–345. [DOI] [PubMed] [Google Scholar]
- 11. Hayes SM, Love PE (2002) Distinct structure and signaling potential of the gamma delta TCR complex. Immunity 16: 827–838. [DOI] [PubMed] [Google Scholar]
- 12. Shin S, El-Diwany R, Schaffert S, Adams EJ, Garcia KC, et al. (2005) Antigen recognition determinants of gammadelta T cell receptors. Science 308: 252–255. [DOI] [PubMed] [Google Scholar]
- 13. Vidovic D, Roglic M, McKune K, Guerder S, MacKay C, et al. (1989) Qa-1 restricted recognition of foreign antigen by a gamma delta T-cell hybridoma. Nature 340: 646–650. [DOI] [PubMed] [Google Scholar]
- 14. Dieude M, Striegl H, Tyznik AJ, Wang J, Behar SM, et al. (2011) Cardiolipin binds to CD1d and stimulates CD1d-restricted gammadelta T cells in the normal murine repertoire. J Immunol 186: 4771–4781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zeng X, Wei YL, Huang J, Newell EW, Yu H, et al. (2012) gammadelta T cells recognize a microbial encoded B cell antigen to initiate a rapid antigen-specific interleukin-17 response. Immunity 37: 524–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Iwasaki A, Medzhitov R (2004) Toll-like receptor control of the adaptive immune responses. Nat Immunol 5: 987–995. [DOI] [PubMed] [Google Scholar]
- 17. Akira S, Hemmi H (2003) Recognition of pathogen-associated molecular patterns by TLR family. Immunol Lett 85: 85–95. [DOI] [PubMed] [Google Scholar]
- 18. Fang H, Welte T, Zheng X, Chang GJ, Holbrook MR, et al. (2010) gammadelta T cells promote the maturation of dendritic cells during West Nile virus infection. FEMS Immunol Med Microbiol 59: 71–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Beetz S, Marischen L, Kabelitz D, Wesch D (2007) Human gamma delta T cells: candidates for the development of immunotherapeutic strategies. Immunol Res 37: 97–111. [DOI] [PubMed] [Google Scholar]
- 20. Beetz S, Wesch D, Marischen L, Welte S, Oberg HH, et al. (2008) Innate immune functions of human gammadelta T cells. Immunobiology 213: 173–182. [DOI] [PubMed] [Google Scholar]
- 21. Shimura H, Nitahara A, Ito A, Tomiyama K, Ito M, et al. (2005) Up-regulation of cell surface Toll-like receptor 4-MD2 expression on dendritic epidermal T cells after the emigration from epidermis during cutaneous inflammation. J Dermatol Sci 37: 101–110. [DOI] [PubMed] [Google Scholar]
- 22. Peng G, Wang HY, Peng W, Kiniwa Y, Seo KH, et al. (2007) Tumor-infiltrating gammadelta T cells suppress T and dendritic cell function via mechanisms controlled by a unique toll-like receptor signaling pathway. Immunity 27: 334–348. [DOI] [PubMed] [Google Scholar]
- 23. Schwacha MG, Rani M, Zhang Q, Nunez-Cantu O, Cap AP (2014) Mitochondrial damage-associated molecular patterns activate gammadelta T-cells. Innate Immun 20: 261–268. [DOI] [PubMed] [Google Scholar]
- 24. Kunzmann V, Kretzschmar E, Herrmann T, Wilhelm M (2004) Polyinosinic-polycytidylic acid-mediated stimulation of human gammadelta T cells via CD11c dendritic cell-derived type I interferons. Immunology 112: 369–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Collins C, Shi C, Russell JQ, Fortner KA, Budd RC (2008) Activation of gammadelta T cells by Borrelia burgdorferi is indirect via a TLR- and caspase-dependent pathway. J Immunol 181: 2392–2398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Martino A, Casetti R, D'Alessandri A, Sacchi A, Poccia F (2005) Complementary function of gamma delta T-lymphocytes and dendritic cells in the response to isopentenyl-pyrophosphate and lipopolysaccharide antigens. J Clin Immunol 25: 230–237. [DOI] [PubMed] [Google Scholar]
- 27. Devilder MC, Allain S, Dousset C, Bonneville M, Scotet E (2009) Early triggering of exclusive IFN-gamma responses of human Vgamma9Vdelta2 T cells by TLR-activated myeloid and plasmacytoid dendritic cells. J Immunol 183: 3625–3633. [DOI] [PubMed] [Google Scholar]
- 28. Pietschmann K, Beetz S, Welte S, Martens I, Gruen J, et al. (2009) Toll-like receptor expression and function in subsets of human gammadelta T lymphocytes. Scand J Immunol 70: 245–255. [DOI] [PubMed] [Google Scholar]
- 29. Wesch D, Beetz S, Oberg HH, Marget M, Krengel K, et al. (2006) Direct costimulatory effect of TLR3 ligand poly(I∶C) on human gamma delta T lymphocytes. J Immunol 176: 1348–1354. [DOI] [PubMed] [Google Scholar]
- 30. Deetz CO, Hebbeler AM, Propp NA, Cairo C, Tikhonov I, et al. (2006) Gamma interferon secretion by human Vgamma2Vdelta2 T cells after stimulation with antibody against the T-cell receptor plus the Toll-Like receptor 2 agonist Pam3Cys. Infect Immun 74: 4505–4511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Adachi O, Kawai T, Takeda K, Matsumoto M, Tsutsui H, et al. (1998) Targeted disruption of the MyD88 gene results in loss of IL-1- and IL-18-mediated function. Immunity 9: 143–150. [DOI] [PubMed] [Google Scholar]
- 32. Town T, Bai F, Wang T, Kaplan AT, Qian F, et al. (2009) Toll-like receptor 7 mitigates lethal West Nile encephalitis via interleukin 23-dependent immune cell infiltration and homing. Immunity 30: 242–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lund JM, Alexopoulou L, Sato A, Karow M, Adams NC, et al. (2004) Recognition of single-stranded RNA viruses by Toll-like receptor 7. Proc Natl Acad Sci U S A 101: 5598–5603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Welte T, Reagan K, Fang H, Machain-Williams C, Zheng X, et al. (2009) Toll-like receptor 7-induced immune response to cutaneous West Nile virus infection. J Gen Virol 90: 2660–2668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hahn YS, Taube C, Jin N, Sharp L, Wands JM, et al. (2004) Different potentials of gamma delta T cell subsets in regulating airway responsiveness: V gamma 1+ cells, but not V gamma 4+ cells, promote airway hyperreactivity, Th2 cytokines, and airway inflammation. J Immunol 172: 2894–2902. [DOI] [PubMed] [Google Scholar]
- 36. Welte T, Aronson J, Gong B, Rachamallu A, Mendell N, et al. (2011) Vgamma4+ T cells regulate host immune response to West Nile virus infection. FEMS Immunol Med Microbiol 63: 183–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Welte T, Lamb J, Anderson JF, Born WK, O'Brien RL, et al. (2008) Role of two distinct gammadelta T cell subsets during West Nile virus infection. FEMS Immunol Med Microbiol 53: 275–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Wicker JA, Whiteman MC, Beasley DW, Davis CT, McGee CE, et al. (2012) Mutational analysis of the West Nile virus NS4B protein. Virology 426: 22–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hemmi H, Kaisho T, Takeuchi O, Sato S, Sanjo H, et al. (2002) Small anti-viral compounds activate immune cells via the TLR7 MyD88-dependent signaling pathway. Nat Immunol 3: 196–200. [DOI] [PubMed] [Google Scholar]
- 40. Panda A, Qian F, Mohanty S, van Duin D, Newman FK, et al. (2010) Age-associated decrease in TLR function in primary human dendritic cells predicts influenza vaccine response. J Immunol 184: 2518–2527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Shaw AC, Panda A, Joshi SR, Qian F, Allore HG, et al. (2011) Dysregulation of human Toll-like receptor function in aging. Ageing Res Rev 10: 346–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Argentati K, Re F, Donnini A, Tucci MG, Franceschi C, et al. (2002) Numerical and functional alterations of circulating gammadelta T lymphocytes in aged people and centenarians. J Leukoc Biol 72: 65–71. [PubMed] [Google Scholar]
- 43. Cardillo F, Falcao RP, Rossi MA, Mengel J (1993) An age-related gamma delta T cell suppressor activity correlates with the outcome of autoimmunity in experimental Trypanosoma cruzi infection. Eur J Immunol 23: 2597–2605. [DOI] [PubMed] [Google Scholar]
- 44. Weerkamp F, de Haas EF, Naber BA, Comans-Bitter WM, Bogers AJ, et al. (2005) Age-related changes in the cellular composition of the thymus in children. J Allergy Clin Immunol 115: 834–840. [DOI] [PubMed] [Google Scholar]
- 45. Heilig JS, Tonegawa S (1986) Diversity of murine gamma genes and expression in fetal and adult T lymphocytes. Nature 322: 836–840. [DOI] [PubMed] [Google Scholar]
- 46. Wang T, Scully E, Yin Z, Kim JH, Wang S, et al. (2003) IFN-gamma-producing gammadelta T cells help control murine West Nile virus infection. J Immunol 171: 2524–2531. [DOI] [PubMed] [Google Scholar]
- 47. Xie G, Welte T, Wang J, Whiteman MC, Wicker JA, et al. (2013) A West Nile virus NS4B-P38G mutant strain induces adaptive immunity via TLR7-MyD88-dependent and independent signaling pathways. Vaccine 31: 4143–4151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kong KF, Delroux K, Wang X, Qian F, Arjona A, et al. (2008) Dysregulation of TLR3 Impairs the Innate Immune Response to West Nile Virus in the Elderly. J Virol 82: 7613–7623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Colonna-Romano G, Potestio M, Aquino A, Candore G, Lio D, et al. (2002) Gamma/delta T lymphocytes are affected in the elderly. Exp Gerontol 37: 205–211. [DOI] [PubMed] [Google Scholar]
- 50. Doyle KP, Cekanaviciute E, Mamer LE, Buckwalter MS (2010) TGFbeta signaling in the brain increases with aging and signals to astrocytes and innate immune cells in the weeks after stroke. J Neuroinflammation 7: 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Alvarez-Rodriguez L, Lopez-Hoyos M, Munoz-Cacho P, Martinez-Taboada VM (2012) Aging is associated with circulating cytokine dysregulation. Cell Immunol 273: 124–132. [DOI] [PubMed] [Google Scholar]
- 52. Shaw AC, Goldstein DR, Montgomery RR (2013) Age-dependent dysregulation of innate immunity. Nat Rev Immunol 13: 875–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Hao J, Dong S, Xia S, He W, Jia H, et al. (2011) Regulatory role of Vgamma1 gammadelta T cells in tumor immunity through IL-4 production. J Immunol 187: 4979–4986. [DOI] [PubMed] [Google Scholar]
- 54. O'Brien RL, Roark CL, Born WK (2009) IL-17-producing gammadelta T cells. Eur J Immunol 39: 662–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Sutton CE, Lalor SJ, Sweeney CM, Brereton CF, Lavelle EC, et al. (2009) Interleukin-1 and IL-23 induce innate IL-17 production from gammadelta T cells, amplifying Th17 responses and autoimmunity. Immunity 31: 331–341. [DOI] [PubMed] [Google Scholar]
- 56. Schmolka N, Serre K, Grosso AR, Rei M, Pennington DJ, et al. (2013) Epigenetic and transcriptional signatures of stable versus plastic differentiation of proinflammatory gammadelta T cell subsets. Nat Immunol 14: 1093–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Roark CL, French JD, Taylor MA, Bendele AM, Born WK, et al. (2007) Exacerbation of Collagen-Induced Arthritis by Oligoclonal, IL-17-Producing {gamma}{delta} T Cells. J Immunol 179: 5576–5583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Cai Y, Shen X, Ding C, Qi C, Li K, et al. (2011) Pivotal role of dermal IL-17-producing gammadelta T cells in skin inflammation. Immunity 35: 596–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Roark CL, Huang Y, Jin N, Aydintug MK, Casper T, et al. (2013) A canonical Vgamma4Vdelta4+ gammadelta T cell population with distinct stimulation requirements which promotes the Th17 response. Immunol Res 55: 217–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Zuo A, Liang D, Shao H, Born WK, Kaplan HJ, et al. (2012) In vivo priming of IL-17(+) uveitogenic T cells is enhanced by Toll ligand receptor (TLR)2 and TLR4 agonists via gammadelta T cell activation. Mol Immunol 50: 125–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Shi C, Sahay B, Russell JQ, Fortner KA, Hardin N, et al. (2011) Reduced immune response to Borrelia burgdorferi in the absence of gammadelta T cells. Infect Immun 79: 3940–3946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Wang T, Gao Y, Scully E, Davis CT, Anderson JF, et al. (2006) Gammadelta T cells facilitate adaptive immunity against West Nile virus infection in mice. J Immunol 177: 1825–1832. [DOI] [PubMed] [Google Scholar]
- 63. Shrestha B, Wang T, Samuel MA, Whitby K, Craft J, et al. (2006) Gamma interferon plays a crucial early antiviral role in protection against West Nile virus infection. J Virol 80: 5338–5348. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The effects of LPS on anti-CD3- activated γδ T cells of TLR4−/− mice. Splenic γδ T cells were cultured with anti-CD3 with or without LPS. Cells were harvested at 48 h post-stimulation and analyzed for CD69 expression (A) and the production of IFN-γ (B), IL-2 (C) and TNF-α (D) in culture supernatant. ** P<0.01 or * P<0.05 compared to anti-CD3- treated alone. Results presented are one representative of two similar experiments.
(TIF)
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.