Abstract
Objective.
To understand how the results of laboratory tests are communicated to patients in primary care and perceptions on how the process may be improved.
Design.
Qualitative study employing staff focus groups.
Setting.
Four UK primary care practices.
Participants.
Staff involved in the communication of test results.
Findings.
Five main themes emerged from the data: (i) the default method for communicating results differed between practices; (ii) clinical impact of results and patient characteristics such as anxiety level or health literacy influenced methods by which patients received their test result; (iii) which staff member had responsibility for the task was frequently unclear; (iv) barriers to communicating results existed, including there being no system or failsafe in place to determine whether results were returned to a practice or patient; (v) staff envisaged problems with a variety of test result communication methods discussed, including use of modern technologies, such as SMS messaging or online access.
Conclusions.
Communication of test results is a complex yet core primary care activity necessitating flexibility by both patients and staff. Dealing with the results from increasing numbers of tests is resource intensive and pressure on practice staff can be eased by greater utilization of electronic communication. Current systems appear vulnerable with no routine method of tracing delayed or missing results. Instead, practices only become aware of missing results following queries from patients. The creation of a test communication protocol for dissemination among patients and staff would help ensure both groups are aware of their roles and responsibilities.
Key words: Diagnostic tests, medical errors/patient safety, practice management, primary care, qualitative research/study, quality of care.
Introduction
Huge numbers of tests continue to be ordered in primary care, with GPs reportedly ordering laboratory tests for nearly a third of all visits (1). Inadequate follow-up of results can lead to serious harm for patients (1–5) and medico-legal concerns for health care providers (1,6,7). Though reasons for ordering tests vary, the timely and accurate communication of results is central to ensuring appropriate action is taken (2). The process of result communication in primary care is complex and relies not only on a range of practice staff with and without clinical expertize but also on external groups in laboratory and hospital settings. Successfully managing the plethora of test results within this fragmented setting is hindered in the UK by the absence of satisfactory guidelines.
A recent study of closed malpractice claims involving diagnostic errors, found that inadequate follow-up of a test result was the basis for complaint in 45% of cases. It has been reported that up to one-third of patients are not notified of abnormal results (3) and nor are normal results routinely communicated, despite the expressed preference of patients (7–9). A study in the USA found only half of general practices had written protocols for any result management steps and few providers documented key stages in the communication system such as patient notification or follow-up for abnormal results (4).
Modern communication technologies appear to offer one solution to improve reliability and consistency of result communication (5,6). However, modern information and communication platforms are only slowly being adopted in health care, and patient aspirations for appropriate information appear to exceed current levels of access (7). In the UK, the National Health Service (NHS) Future Forum recently reported that barriers to fuller utilization of existing technological capability in successful health care communication are more cultural than technical and called for ‘a change of mindset’ within the NHS (8).
Previous attempts to study the issues confronting staff communicating results have relied on surveys (7,8,10,11) or reports of errors (2,4). The attitudes of primary care staff in the UK towards the process of result communication and its implications for quality and safety are yet to be fully explored. Similarly, systematic consultation with staff on the creation and implementation of policies and procedures to improve current systems is absent. Here, we report on interviews with staff, which were carried out as part of a study to explore staff and patient perceptions of strengths and weaknesses in current systems to identify failures in the system. We also explored attitudes to modern communication technology that might ameliorate the problems of test communication.
Design and methodology
Four general practices were selected from 10 Birmingham practices collaborating in Birmingham and Lambeth Liver Evaluation Testing Strategies (BALLETS), a prospective study of abnormal liver function tests in England (12). During BALLETS, we discerned that methods of test result communication varied between practices. Judgement sampling, based on our knowledge of the practices, was used to purposively select four practices in order to include different default pathways for test result communication, encompassing a range of overlapping communication methods and systems (13). A focus group was carried out at each practice with participants selected from all staff groups currently playing a role in the process. GPs, practice nurses, health care assistants, a receptionist and the practice manager (Table 1) were recuited in each practice to meet this requirement. Between six and eight participants attended each focus group (14).
Table 1.
Characteristics of each practice and subsequent focus group
| Practice characteristics | Practice 1000 | Practice 2000 | Practice 3000 | Practice 4000 |
|---|---|---|---|---|
| Number of GPs by full-time equivalent (fte) sessions | 7.3 fte | 3.0 fte | 6.3 fte | 12.3 fte |
| IMD rankinga | 25 | 13 866 | 871 | 8447 |
| Number of patients | 23727 | 5914 | 7059 | 27500 |
| Attendees | Focus group 1 | Focus group 2 | Focus group 3 | Focus group 4 |
| GPs | 6 | 7 | 2 | 2 |
| Practice managers | 1 | 0 | 1 | 1 |
| Registered nurses | 2 | 2 | 3 | 0 |
| Administrative staff | 1 | 1 | 1 | 2 |
| Health care assistants | 1 | 0 | 1 | 1 |
aIndex of multiple deprivation ranking out of 32482 lower super output levels in England.
The topic guide explored staff perceptions of strengths and weaknesses of existing systems for communicating test results in primary care; how they felt the service could be improved; the role of patients in the process and how different patient wishes could best be accommodated. Participants were asked to speak frankly about barriers to a more effective system, including force of habit, relationships between staff, the question of who should bear responsibility and logistic constraints.
The focus groups were conducted over a 2-month period during the second half of 2010 and were recorded and transcribed. The focus groups were moderated by IJL (research fellow with a background in occupational medicine) who was not known to practice staff. Field notes were taken by LMB (a senior research nurse) who was known to some of the staff present from her involvement in the BALLETS study (12). Any new issue arising from a focus group was fed into a subsequent topic guide. Each transcript was read and the findings analysed thematically by IJL, LMB and SMG who met and agreed emerging themes to decide on a coding framework. Transcripts were analysed alongside the field notes, using constant comparative analysis (15).
Results
Participating practices varied in size and deprivation status (Table 1) (16). The composition of focus groups also varied in number and type of staff who took part, although all included GPs and administrative staff.
Five main themes emerged from the data: current methods of communicating results, factors that should influence the methods for communicating results, bearing responsibility for the task of communicating test results, barriers to communicating results, problems inherent in different methods of test result communication and perceptions of patients’ expectations. These are now presented in turn illustrated by selected quotations to reflect the issues which emerged.
Methods of communicating results
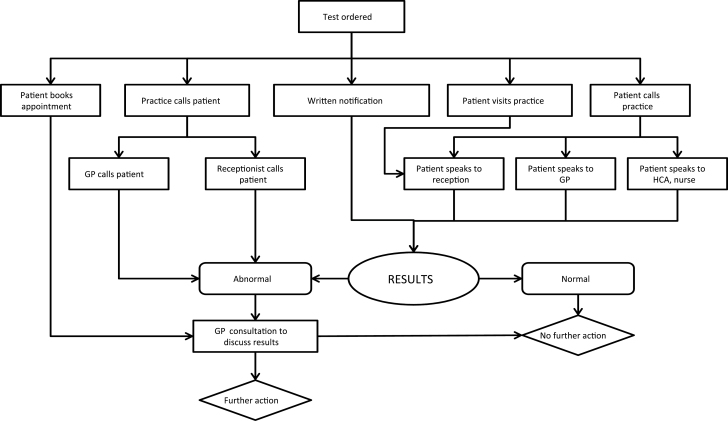
When tests are ordered, patients are often not given clear instructions on how they will be informed of the result. In all four practices, patients were most commonly told by a GP or phlebotomist to telephone the practice after a stated time interval. When the patient places a call, normal results (defined here as results requiring no further action) were relayed by the member of administrative staff who answered the phone. Patients were also advised of abnormal results by reception staff and typically advised to book an appointment with a GP if one was not in place. In certain circumstances (discussed below), GPs contacted patients directly. We have summarized the range of communication in a “system pathway” diagram (Fig. 1).
Figure 1.
Communication pathway diagram.
What appeared to be an agreed procedure was not always followed to the letter and varied according to individual clinician behaviour and preferences.
Well, here there is a set procedure and the degree to which the clinicians use the procedure is, I think, variable to a degree. The first thing to say is that it is at the clinician’s discretion … (Practice Manager; FG4)
There were differences between practices as to precisely when the patient is instructed to phone for results, what the patient is told and by whom. Some had an allotted time for receiving calls requesting results alongside an automated system to capture patient messages. However, this appeared to have led to increased time spent by administrative staff responding to messages left by patients seeking results.
… it constantly rings while you are on the phone...And then you might have, whilst you are on the phone to one person, four or five other people will ring and leave a message and you still have to get back then to the patients. (Health Care Assistant; FG4)
Influences on methods of communicating results
A number of factors influence the method of test result communication, including the clinical impact of the result. Where the doctor has an expectation that the result was likely to be abnormal then the practice may be more proactive in communicating the result and would inform the patient of this at the time of ordering.
… if you are expecting an abnormal result you will book the patient in ahead, because you want to see them face-to face. (GP; FG2)
Staff acknowledged that the choice of communication method depended upon the characteristics of the patient, such as anxiety levels or health literacy.
I think knowing your patient and the level of anxiety it’s going to cause. So if you think that by phoning or sending a letter is going to cause them anxiety you would actually phone them. (GP; FG2)
Communicating the results of patients with chronic conditions appeared comparatively straightforward; despite potentially more serious outcomes, diagnostic testing appeared less well regulated.
[] we are probably quite good at catching those [patients with chronic conditions] … that might be as much as half of them and then the other half would be tests done in response to a patient presenting a particular problem and I think those are the ones that I think we are worst at. (GP; FG3)
If the results required further action, then the GP could assume responsibility for telephoning patients.
I would say: ‘Ring in a week and see if the results are back … if they are abnormal I will contact you anyway.’ (GP; FG2)
Where GPs have decided they will call the patient, then they can introduce flexibility in the timing of when they place that call. Where the implications are serious, discretion is exercised based on the knowledge of the patient and the outcome of the test.
I had an abnormal result given to me on Thursday before the Easter weekend for a patient that had cancer so I thought ‘what would this patient want?’ so I kept it to the Monday or Tuesday. (GP; FG2)
Practice responsibilities regarding communicating test results
Exactly whose responsibility it was for communicating results appeared unclear. One participant felt responsibility rested with the GP who had ordered the test, helping ensure safe and effective care.
I think the doctor that has authorised the test should be responsible, because so often I’ve seen when somebody else has checked results … they’ve looked at it as a general test rather than a specific reason for doing the test and I think that’s quite dangerous. (Practice Nurse; FG3)
At one practice, discussion centred on the divided responsibility between patient and doctor for communicating results and it appeared only if the result was abnormal did responsibility lie with the doctor to make contact.
We sort of go on the side of, well generally speaking, it’s the patient’s responsibility for their result. If something really weird comes back it’s that individual’s doctor. (GP; FG1)
Barriers to communicating results
One problem highlighted was the staggered return to the practice of results relating to a single patient, which could lead them to receive misleading information.
[] they may not all come in at the same time... we have had patients only being told one set, because their biochemistry had been returned but they are very seriously anaemic, and that comes in with later results. And they are very upset because they say, ‘Well I was told they’re normal’. (GP; FG2)
Practices had no structured system for confirming tests ordered had been completed and results returned to the practice or then reached patients.
… it’s hard, if the patient hasn’t called for the result we may never know that they didn’t get the result, especially with an abnormal result. (GP; FG3)
This variation in the amount of information is problematic in the case of an abnormal result, prompting anxiety in the patient and triggering the need for further information from those not qualified to provide it.
They could keep you on the phone for nearly ten minutes with some patients asking every little bit of information. (Health Care Assistant; FG4)
In some cases where results are abnormal, reception staff advise patients they need to see their GP to retrieve results, causing anxiety.
… when the patients are asked to ring up and the result isn’t normal and the staff have to ask them to make an appointment and that doesn’t bode very well because the patient goes, “Well I want to know!” (GP; FG3)
Problems of different methods of communication
Some staff expressed frustration at patients pursuing results that, it transpires, are not clinically significant.
The majority of these [results] are normal, they’re fine. They’re not results that the doctor has felt the patient needs; that’s taking valuable clinical time out. (Practice Manager; FG4)
Greater utilization of text messaging was discussed as a time saving mechanism. However, staff expressed concern over the demographic of mobile phone users and problems of maintaining an accurate record of telephone numbers.
We probably do more blood tests on the older population who probably have less mobile phones, certainly my grandmother wouldn’t have a clue how to use a mobile phone … So for the majority of them it wouldn’t work anyway (GP; FG2)
It relies on the mobile numbers being up to date … so I’m not a fan of it. (GP; FG1)
The confidentiality of SMS messages was another consideration, notably in shared households.
On Friday, two gents that lived at the same house have got the same mobile number for both of them, one was the man’s and one was his partner’s. I could have been texting results to his partner. (Secretary; FG2)
Discussion
Findings
Current systems for communicating test results in primary care are informal and none of the practices interviewed had protocols in place. That said, the subject is more complex than might be immediately apparent because there is no single method that could suit all circumstances. Clinical urgency varies greatly and patients have different preferences. It was therefore recognized that protocols would need to encompass more than one option for communication of results.
Study limitations
Focus groups consisted of mixed staff grades that may have inhibited the openness of some participants. However, creating groups of mixed staff grade reflected the reality of the practice environment where a range of practice staff interact with each other throughout the testing and result communication process. The number of focus groups was limited to four, this is however within the range reported in existing literature (17) and similar experiences were repeatedly described across the four groups, suggesting that we were approaching theoretical saturation (18). Views were obtained from primary health care professionals involved in communicating results and there was a range of staff types, gender and ethnicities. While we cannot claim that the perspectives of staff at the study practices are representative of those across the world, previous studies in the USA have similarly found that the testing and result communication process is haphazard (1,5).
Alternative methods considered
The majority of patients are instructed to contact the practice for results. The volume of enquiries by patients was a source of frustration for staff due to the time spent dealing with requests for ‘normal’ results. We explored alternative methods for communicating the bulk of ‘normal’ results that would reduce pressure on administrative staff. Previous work suggested patients prefer mailed results, which precludes the need to phone to obtain normal results and can also act as a memory aid for follow-up (7–9). Use of computer-generated letters was deemed too expensive by staff; however, none of the study practices had undertaken a cost comparison of current or prospective methods. One cost-effective solution to meeting growing demand is the greater utilization of modern information and communication technologies. However, despite the encouragement of the Department of Health, the use of Information and Communication Technology across the whole of primary care remains variable (10) and staff within our sample felt the use of SMS was inappropriate and risked compromising patient confidentiality.
Anxiety and information
Non-clinical staff in our sample recognized the anxiety experienced by patients when they learn of abnormal results from administrative staff who are unable to respond to their concerns. Previous evidence has indicated that providing patients with clear, appropriate descriptions of tests and the implications of results during the initial consultation may reduce patient concern and increase levels of reassurance (19). Providing supporting information for patients receiving results, either first hand or via sources readily accessible to patients, may also reduce anxiety. This was addressed in 2010 when NHS England introduced ‘Information Prescriptions’ to provide information for patients on diseases, treatment options and local services (20).
Missing results and patient safety
A notable aspect of current systems within the study practices is the lack of a method for detecting delayed or missing results, despite the capability of existing clinical management systems to create alerts for absent results. Instead, for the majority of tests, it took a patient initiated request for results for the practice to become aware that a result had not been returned from the laboratory. This has serious implications for patient safety when considering the findings of a previous study that indicated the probability of a patient collecting a result is not necessarily influenced by the reason for testing (11).
Conclusions
It is apparent that dealing with an increasing number of tests in the complex environment of primary care necessitates some flexibility on behalf of both patients and staff in the testing and result communication process. The routine automated provision of non-significant results is one way of dealing with the increasing number of tests ordered. However, for this to be successful, patients may require greater access to supporting information about the test and the implications of the result than is currently provided. Whichever way results are communicated, it appears imperative that we improve patient awareness of their responsibility for results to help reduce the potential for error (21). Practices should be encouraged to address the risk to patient safety, adopt a more effective utilization of modern technologies and increase engagement of patients as partners in the process. By doing so, it may be possible to establish a framework for the improvement of test result communication that heeds the dual requirements of patient-centred care and logistical constraint. To enable this, a more complete appreciation of patient perception of the result communication process is needed. Further research is required to gain insight into valuable patient perspectives, to challenge practice assumptions and offer sustainable solutions.
Declaration
Funding: National Institute for Health Research for Patient Benefit programme in England (PB-PG-1208–18219); Primary Care Research Network for Central England.
Ethical approval: favourable opinion of NRES Committee West Midlands—The Black Country; approval of the Birmingham and Black Country Comprehensive Local Research Network.
Conflict of interest: none.
Acknowledgements
Our thanks to staff at the four participating practices for taking part in the study and to NIHR Collaborations for Leadership in Applied Health Research and Care (CLAHRC) for Birmingham and Black Country. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the RfPB programme, NIHR, NHS or the Department of Health, in England.
References
- 1. Hickner JM, Fernald DH, Harris DM, Poon EG, Elder NC, Mold JW. Issues and initiatives in the testing process in primary care physician offices. Jt Comm J Qual Patient Saf 2005; 31: 81–9 [DOI] [PubMed] [Google Scholar]
- 2. Hickner J, Graham DG, Elder NC, et al. Testing process errors and their harms and consequences reported from family medicine practices: a study of the American Academy of Family Physicians National Research Network. Qual Saf Health Care 2008; 17: 194–200 [DOI] [PubMed] [Google Scholar]
- 3. Boohaker EA, Ward RE, Uman JE, McCarthy BD. Patient notification and follow-up of abnormal test results. A physician survey. Arch Intern Med 1996; 156: 327–31 [PubMed] [Google Scholar]
- 4. Callen JL, Westbrook JI, Georgiou A, Li J. Failure to follow-up test results for ambulatory patients: a systematic review. J Gen Intern Med 2012; 27: 1334–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Elder NC, McEwen TR, Flach JM, Gallimore JJ. Management of test results in family medicine offices. Ann Fam Med 2009; 7: 343–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Callen JL, Westbrook JI, Braithwaite J. The effect of physicians’ long-term use of CPOE on their test management work practices. J Am Med Inform Assoc 2006; 13: 643–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Leekha S, Thomas KG, Chaudhry R, Thomas MR. Patient preferences for and satisfaction with methods of communicating test results in a primary care practice. Jt Comm J Qual Patient Saf 2009; 35: 497–501 [DOI] [PubMed] [Google Scholar]
- 8. Department of Health. 2011 Information: A Report From the NHS Future Forum https://www.gov.uk/government/uploads/system/uploads/ attachment_data/file/216424/dh_132086.pdf (accessed on 14 July 2014).
- 9. Meza JP, Webster DS. Patient preferences for laboratory test results notification. Am J Manag Care 2000; 6: 1297–300 [PubMed] [Google Scholar]
- 10. Baldwin DM, Quintela J, Duclos C, Staton EW, Pace WD. Patient preferences for notification of normal laboratory test results: a report from the ASIPS Collaborative. BMC Fam Pract 2005; 6: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kelly MH, Barber JH. Use of laboratory services and communication of results to patients in an urban practice: an audit. J R Coll Gen Pract 1988; 38: 64–6 [PMC free article] [PubMed] [Google Scholar]
- 12. Lilford RJ, Bentham L, Girling A, et al. Birmingham and Lambeth Liver Evaluation Testing Strategies (BALLETS): a prospective cohort study. Health Technol Assess 2013; 17: i–xiv, 1–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P. Qualitative research methods in health technology assessment: a review of the literature. Health Technol Assess 1998; 2: iii–ix, 1–274. [PubMed] [Google Scholar]
- 14. Gill P, Stewart K, Treasure E, Chadwick B. Methods of data collection in qualitative research: interviews and focus groups. Br Dent J 2008; 204: 291–5 [DOI] [PubMed] [Google Scholar]
- 15. Hewitt-Taylor J. Use of constant comparative analysis in qualitative research. Nurs Stand 2001; 15: 39–42 [DOI] [PubMed] [Google Scholar]
- 16. UK Government Department for Communities and Local Government. The English Indices of Deprivation 2010; Index of Multiple Deprivation https://www.gov.uk/government/collections/english-indices-of-deprivation (accessed on 26 April 2012).
- 17. Carlsen B, Glenton C. What about N? A methodological study of sample-size reporting in focus group studies. BMC Med Res Methodol 2011; 11: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mason M. Sample size and saturation in PhD studies using qualitative interviews. Forum: Qual Soc Res 2010; 11: Art.8. http://www.quali tative-research.net/index.php/fqs/article/view/1428/3028 (accessed on 14 July 2014) [Google Scholar]
- 19. Petrie KJ, Müller JT, Schirmbeck F, et al. Effect of providing information about normal test results on patients’ reassurance: randomised controlled trial. BMJ 2007; 334: 352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Department of Health. Your Health, Your Way – A Guide to Long Term Conditions and Self Care. Information for Healthcare Professionals webarchive.nationalarchives.gov.uk/20130107105354/http:/www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/ digitalasset/dh_097586.pdf
- 21. Unruh KT, Pratt W. Patients as actors: the patient’s role in detecting, preventing, and recovering from medical errors. Int J Med Inform 2007; 129 (suppl 1): 236–44 [DOI] [PubMed] [Google Scholar]