Abstract
Background
Previous meta-analyses of cognitive-behavioural therapy (CBT) for children and young people with anxiety disorders have not considered the efficacy of transdiagnostic CBT for the remission of childhood anxiety.
Aim
To provide a meta-analysis on the efficacy of transdiagnostic CBT for children and young people with anxiety disorders.
Methods
The analysis included randomised controlled trials using transdiagnostic CBT for children and young people formally diagnosed with an anxiety disorder. An electronic search was conducted using the following databases: ASSIA, Cochrane Controlled Trials Register, Current Controlled Trials, Medline, PsycArticles, Psychlnfo, and Web of Knowledge. The search terms included ‘anxiety disorder(s)’, ‘anxi*’, ‘cognitive behavio*, ‘CBT’, ‘child*’, ‘children’, ‘paediatric’, ‘adolescent(s)’, ‘adolescence’, ‘youth’, and ‘young pe*’. The studies identified from this search were screened against the inclusion and exclusion criteria, and 20 studies were identified as appropriate for inclusion in the current meta-analysis. Pre- and post- treatment (or control period) data were used for analysis.
Results
Findings indicated significantly greater odds of anxiety remission from pre- to post- treatment for those engaged in the transdiagnostic CBT intervention compared with those in the control group, with children in the treatment condition 9.15 times more likely to recover from their anxiety diagnosis than children in the control group. Risk of bias was not correlated with study effect sizes.
Conclusions
Transdiagnostic CBT seems effective in reducing symptoms of anxiety in children and young people. Further research is required to investigate the efficacy of CBT for children under the age of 6.
Introduction
Considerable interest in childhood anxiety disorders has emerged, which (Klein, 2009) attributes to their prevalence, economic and medical cost, and the early onset of anxiety disorders in comparison to other mental health difficulties. Prevalence of anxiety disorders in children and young people is relatively high, although a meta-analysis has indicated that there is a wide range of prevalence rates (from 2.6% to 41.2%) across studies (Cartwright-Hatton, McNicol, & Doubleday, 2006). Children are affected by a range of anxiety disorders, including generalised anxiety disorder, social phobia, panic disorder, agoraphobia, and separation anxiety disorder (Klein, 2009). Boys have been found to develop anxiety disorders at a younger age compared with girls, with 7-12 year old boys and adolescent girls (aged 13-19 years) being more frequently referred for treatment than boys and girls in other age groups (Hoff Esbjørn, Hoeyer, Dyrborg, Leth, & Kendall, 2010). Overall though, the prevalence of anxiety disorders tends to increase with age (Hoff Esbjørn et al., 2010; Kendall et al., 2010).
Cognitive-behavioural approaches assume that anxiety is maintained through safety behaviours and avoidance (Hofmann, 2007), as well as through worrying, causal attributions, and memory processes (Prins, 2001). Compared with adults, children are assumed to be more threatened by anxiety-provoking situations and to feel less confident in their ability to cope with the situation (Prins, 2001). CBT has been developed to treat anxiety disorders in children and young people, with techniques of ‘cognitive restructuring, coping self-talk, in vivo exposure, modelling, and relaxation training’ (Muris, Mayer, den Adel, Roos, & van Wamelen, 2009, p.14).
Meta-analyses are a useful way of drawing together a number of studies that test similar questions, such as the efficacy of treatments for psychological disorders. Individual studies based on small samples are likely to suffer more bias than large-sample studies, but a meta-analysis makes use of the data from a number of studies, thus reducing this risk of bias (Field & Gillett, 2010). In addition, it is possible to test the variability in effect sizes between the studies using a meta-analysis (Field & Gillett, 2010).
Reviews of the literature examining the efficacy of treatments for anxiety in children suggest that CBT is a ‘probably efficacious’ or ‘well-established’ intervention for a variety of childhood anxiety disorders, including specific phobias, social phobia, obsessive compulsive disorder (OCD), and post-traumatic stress disorder (PTSD) (Compton et al., 2004; Davis, May, & Whiting, 2011). A recent meta-analysis indicated that the efficacy of CBT is not moderated by age, with children and adolescents demonstrating similar benefits from the treatment, although the authors of that analysis acknowledge that modifications carried out on the CBT may explain this finding (Bennett et al., 2013).
CBT for disorders such as OCD, PTSD, social anxiety disorder and specific phobias tends to be adapted according to the specific anxiety disorder that is being treated. For example, Spence, Donovan, and Brechman-Toussaint (2000) adapted CBT for children with social anxiety disorder by placing an emphasis on social skills training, and Williams et al. (2010) adapted CBT for children with OCD by targeting cognitions specific to OCD. Whilst CBT that is adapted for these conditions might be effective for those specific diagnoses (Cohen & Mannarino, 1996, 1998; Spence et al., 2000; Williams et al., 2010), many general Child and Adolescent Mental Health Services (CAMHS) will not have the skills or throughput of clients to provide specialised interventions for each of the anxiety disorders. Moreover, given the very high level of comorbidity amongst the anxiety disorders of childhood (Leyfer, Gallo, Cooper-Vince, & Pincus, 2013), a more generic, or transdiagnostic, approach is often more practical. And indeed, children are usually offered a transdiagnostic CBT package, which aims to address the common elements of all anxiety disorders (in particular, avoidance, anxiogenic cognition, and sometimes anxiogenic parenting). A question which remains currently unanswered is whether transdiagnostic CBT is beneficial to children and adolescents with anxiety disorders. This study presents a meta-analysis of studies that treat anxious children using transdiagnostic CBT interventions that are intended for the whole range of childhood anxiety disorders.
Other meta-analyses have found CBT to be efficacious in treating childhood anxiety disorders, but do not answer the present question, for a number of reasons: Some have included studies of CBT that have been adapted to treat a specific anxiety disorder such as OCD, Social Anxiety Disorder and PTSD (Cartwright-Hatton, Roberts, Chitsabesan, Fothergill, & Harrington, 2004; Ishikawa, Okajima, Matsuoka, & Sakano, 2007; Silverman, Pina, & Viswesvaran, 2008), or have not used diagnostic outcome measures of the children’s anxiety disorder (In-Albon & Schneider, 2007). Others included non-CBT treatments within the meta-analysis, such as eye-movement desensitisation and reprocessing therapy, and exposure and response prevention therapy (Reynolds, Wilson, Austin, & Hooper, 2012; Silverman et al., 2008) or included studies using ‘treatment elements’ of CBT (such as behavioural treatments or social effectiveness training instead of transdiagnostic CBT) (Ishikawa et al., 2007) and were therefore unable to answer the question as to whether transdiagnostic CBT was an efficacious treatment for children and adolescents with anxiety disorders. A meta-analysis undertaken by James, James, Cowdrey, Soler, and Choke (2013) included studies in which anxiety disorders were not always the primary diagnosis (for instance, they included studies by Chalfant, Rapee, and Carroll (2007), McNally Keehn, Lincoln, Brown, and Chavira (2013) and Wood et al. (2009), which considered the efficacy of CBT for children with autistic spectrum disorders and comorbid anxiety, and a study by Masia-Warner et al. (2011) which considered children with primary somatic complaints).
The current meta-analysis intends to fill this gap in the literature by exploring the efficacy of transdiagnostic CBT for the remission of children and young people’s anxiety disorder diagnoses at post-treatment. In addition, the current review sought to investigate whether recent research had been conducted for children under the age of six, following the assertion by Cartwright-Hatton et al. (2004) that this was an area lacking in research evidence.
Inclusion criteria
The following inclusion criteria were used for the review:
The study was a randomised controlled trial
The sample included children and young people up to the age of 18 at the time of entry into the study
Participants had a primary clinical diagnosis of an anxiety disorder, formally assessed as part of the trial
The intervention was CBT
Interventions used non-active controls (defined as those given no treatment or who were placed in a wait-list control)
Anxiety diagnosis outcome data was available at post-treatment
Reports of research were published in English
The sample size of the study was greater than 1
Trials were excluded from the analysis if:
They didn’t specifically treat anxiety disorders or exclusively treated a single anxiety disorder (studies treating just obsessive compulsive disorder (OCD), post-traumatic stress disorder (PTSD), social anxiety disorder or specific phobias, were found but excluded).
They only used self-report outcome measures. The exclusion of self-report outcome measures was necessary since the aim of the current meta-analysis was to measure change in clinical diagnosis following the intervention, which cannot be assessed by self-report measures.
They employed active controls. These were excluded since few studies with comparison interventions were found, and where available, the comparison interventions frequently included cognitive-behavioural elements.
Parent-only interventions were used which meant that children were not involved in the treatment.
Method
A search was initially conducted to ensure that all trials included in previous meta-analyses were considered for eligibility for the current meta-analysis. A search was then conducted to include other relevant trials, up to and including July 2012. The following electronic databases were used to search for appropriate trials: Applied Social Sciences Index and Abstracts (ASSIA); Cochrane Controlled Trials Register; Current Controlled Trials; Medline; PsycArticles; PsycInfo; and Web of Knowledge. A text search was conducted for keywords, taking into consideration synonyms, variant spellings (such as ‘behaviour’ versus ‘behavior’), and plurals (such as ‘child’ versus ‘children’). The search terms used were: ‘anxiety disorder(s)’ OR ‘anxi*’ AND ‘cognitive behavio*’ OR ‘CBT’ AND ‘child*’ OR ‘children’ OR ‘adolescent(s)’ OR ‘adolescence’ OR ‘youth’ OR ‘young pe*’ OR ‘paediatric’.
The titles and abstracts of the articles generated by the search were screened to assess their applicability to this meta-analysis. The full text was downloaded and screened for those studies that appeared to meet the inclusion criteria. Details of the study design were extracted to ensure that the design met the inclusion criteria for the review and those not meeting the criteria were excluded. Further details were then extracted from the remaining articles including type of anxiety disorder, age of participants, experimentation and control conditions, diagnostic outcome measures used, exclusion criteria and outcome of the intervention. To minimise the risk of publication bias, the authors of papers both included and excluded in this analysis were contacted to identify any relevant unpublished manuscripts that should be considered.
Search Results
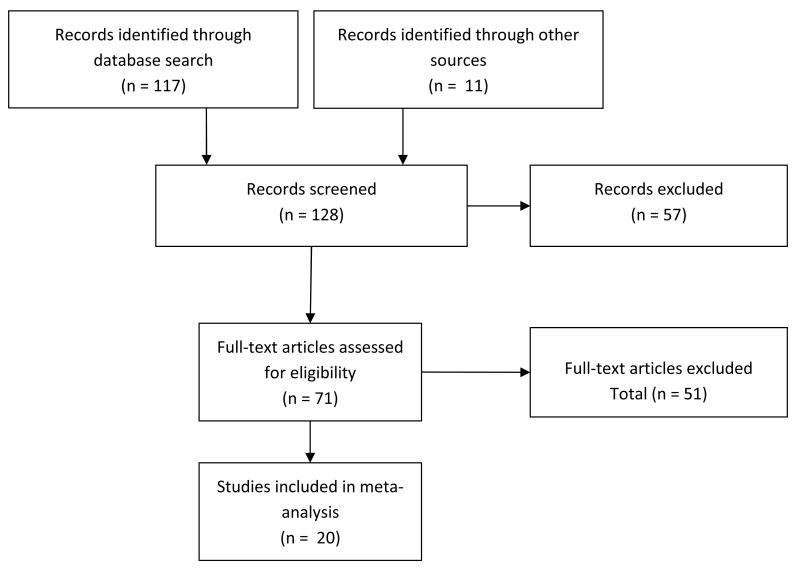
The search identified 117 trials that required consideration for this meta-analysis, including those trials used in previous meta-analyses. The studies were checked against the inclusion criteria, which resulted in the exclusion of 97 studies (please refer to Appendix A for the references of the included and excluded studies). Twenty studies remained for analysis (see Appendix B). The flow diagram of the search results (Moher, Liberati, Tetzlaff, & Altman, 2009) is displayed in Figure 1.
Figure 1. Flow-diagram of search results.
Excluded studies often met more than one criterion for exclusion. One study was excluded for not meeting the criteria of using a sample of children and young people up to the age of 18, and another was excluded for not being a randomised controlled trial. Twenty-nine studies were excluded for not using CBT (or a non-adapted CBT) as the treatment method, and two studies were excluded for using parent-only CBT methods. Four studies were excluded for not being published in English. Twelve studies were excluded for not using a sample of children and young people with clinically diagnosed anxiety disorders, and one study was excluded for not using pre-waitlist diagnostic criteria. Twenty studies were excluded for not using a diagnostic outcome measure of anxiety, and a further four were excluded for not having post-treatment data available for analysis (only follow-up data was available). Nineteen studies were excluded for exclusively treating either OCD, PTSD, social anxiety disorder or a specific phobia. A further seven studies were excluded as the studies did not relate directly to the treatment of anxiety disorders. Finally, thirty-six studies were excluded because they did not use a control group or used an active control group. All studies used a sample size greater than 1.
In addition to the 117 trials identified by the database search, twenty-six authors were contacted about unpublished data suitable for consideration in this meta-analysis. These authors were provided with the inclusion and exclusion criteria for this meta-analysis to help them identify any relevant unpublished data. Sixteen of these responded confirming that there were no unpublished manuscripts to consider. One author suggested a paper under review, but this was excluded because it lacked a control group. A further nine published papers were offered for consideration, but none of these fully met the inclusion criteria and were excluded from the analysis. Two of these papers did not use a control group, three examined long-term follow-up, two did not include clinical anxiety diagnoses, one examined mediator effects rather than the efficacy of the intervention, and one study only included children with OCD.
Risk of Bias Assessment
To assess the risk of bias in the trials used in this meta-analysis, a modified version of the bias assessment form used in Cartwright-Hatton et al.’s (2004) paper (based on the form produced by the University of York, 2001) was used. This form lists the criteria expected of an ideal trial design, with studies assigned a score of 0-3 for each criterion. A score of 0 indicated that the trial did not meet any of the ideal aspects (or not enough information was provided to be scored) for that criterion; a score of 1 indicated that the trial met one ideal aspect; a score of 2 indicated that the trial met most ideal aspects; and a score of 3 indicated that all ideal aspects of the criterion had been met. The results of this assessment suggested that there was a moderate risk of bias, since not all criteria were sufficiently met (see Appendix C). Two of the authors (D.E. and E.T.) independently rated the included trials for risk of bias, with double-ratings available for 85% of the studies. There was substantial inter-rater agreement across the criteria (Kappa range = 0.64 – 1.00).
Statistical Analysis
The log odds ratios for remission of anxiety following treatments were estimated for each study. The log odds ratio was chosen since it uses positive and negative values, thus creating a normal distribution of scores. However, the raw odds ratio can be skewed since it does not use negative values (Bland & Altman, 2000). A conservative analysis was used for the intent-to-treat cases which assumed successful remission for those not followed up from the waiting list condition, and non-remission for those not followed up from the treatment condition. Different types of CBT method used within a study (e.g. group/individual/family) were pooled to provide an overall score for remission following transdiagnostic CBT. The meta-analysis was conducted using random effects methods and the Dersimonian-Laird estimate of between-study variability.
Results
Participant characteristics
Across the 20 studies appropriate for the current review, there was a total of 2,099 participants (Mean = 105 participants per study; range = 37 to 488), with 1,251 placed in the treatment conditions and 601 placed in control conditions. For many of the studies, there was more than one CBT treatment condition (e.g. group, family and individual), which explains the larger number placed for treatment than for the wait-list.
The age range of participants was 4 – 18 years. However, very few studies used participants at the lower end of the range, with two studies including children from four years of age (and a further four studies including children from 6 years of age). The majority of studies considered children between the ages of 7-14, and five studies included children aged 15 years and over. It was not possible to explore pooled outcomes for independent age groups as overlapping ranges were used across studies.
Of the participants, 822 (30%) presented with (as their primary diagnosis) Generalised Anxiety Disorder (GAD), 20 (1%) with Panic Disorder (PD), 634 (23%) with Separation Anxiety Disorder (SAD), 440 (16%) with Social Phobia (SoP), 604 (22%) with specific phobia (SP), 21 (1%) with agoraphobia (AP), and 174 (6%) with over-anxious disorder (OAD). Many participants had more than one anxiety disorder diagnosis, which is reflected in these figures.
Meta-analysis
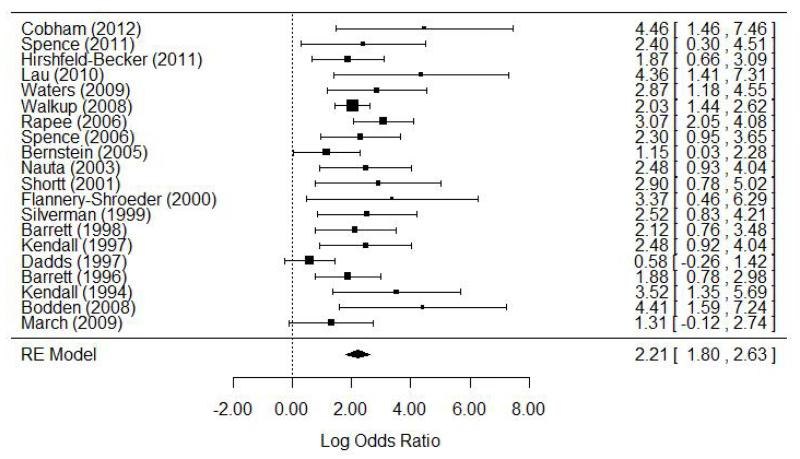
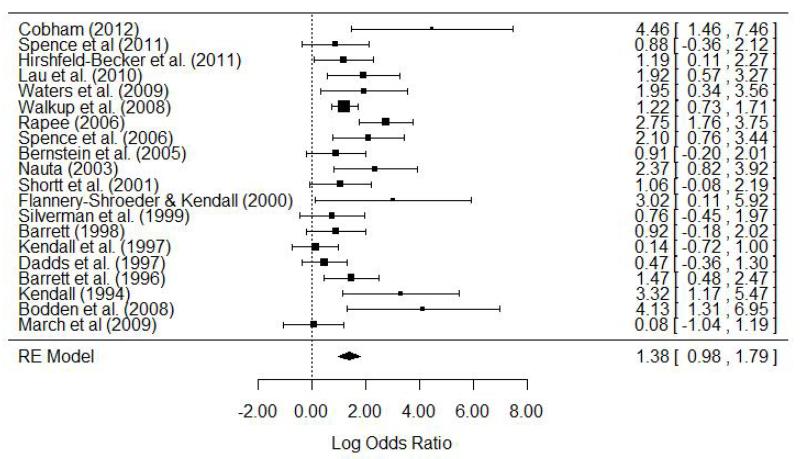
Table 1 shows the log odds ratios for remission from anxiety in each of the studies. The log odds ratios are also represented as forest plots1 for completers and intent-to-treat samples in Figures 2 and 3.
Table 1. Outcome data and odds ratios.
| CBT | Waiting list | Followed-up cases | Intent-to-treat cases | |||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|
|
|
| Study | WD | R/FU | WD | R/FU | Odds ratio (95% CI) | Log odds ratio | Odds ratio (95% CI) | Log odds ratio |
| Cobham (2012) | 0 | 18/23 | 2 | 0/12 | 86.4 (4.31 – 1730.98) | 4.46 | 25.2 (4.24 – 149.79) | 3.07 |
| Spence (2011) | 4 | 13/40 | 3 | 1/24 | 11.07 (1.34 – 91.21) | 2.40 | 2.41 (0.70 – 8.36) | 0.88 |
| Hirshfeld-Becker(2011) | 5 | 17/29 | 2 | 5/28 | 6.52 (1.93 – 22.01) | 1.87 | 3.29 (1.12 – 9.68) | 1.19 |
| Lau (2010) | 3 | 13/20 | 4 | 0/21 | 78 (4.08 – 1492.19) | 4.36 | 6.83 (1.77 – 26.33) | 1.92 |
| March (2009) | 10 | 9/30 | 4 | 3/29 | 3.71 (0.89 – 15.48) | 1.31 | 1.08 (0.353 – 3.29) | 0.08 |
| Waters (2009) | 15 | 39/49* | 0 | 2/11* | 17.55 (3.26 – 94.38) | 2.87 | 7.02 (1.40 – 35.20) | 1.95 |
| Bodden (2008) | 14 | 71/114 | 0 | 0/25 | 82.56 (4.90 – 1391.86) | 4.41 | 62.28 (3.71 – 1045.93) | 4.13 |
| Walkup (2008) | 19 | 196/279* | 15 | 18/76* | 7.61 (4.23 – 13.70) | 2.03 | 3.38 (2.07 – 5.51) | 1.22 |
| Rapee (2006) | 14 | 46/76 | 12 | 5/75 | 21.47 (7.76 – 59.37) | 3.07 | 5.04 (2.59 – 9.82) | 1.62 |
| Spence (2006) | 4 | 27/45 | 0 | 3/23 | 10 (2.59 – 38.66) | 2.30 | 8.18 (2.15 – 31.18) | 2.10 |
| Bernstein (2005) | 5 | 19/37 | 0 | 6/24 | 3.17 (1.03 – 9.77) | 1.15 | 2.48 (0.82 – 7.49) | 0.91 |
| Nauta (2003) | 0 | 32/59 | 0 | 2/20 | 10.67 (2.27 – 50.16) | 2.37 | 10.67 (2.27 – 50.16) | 2.37 |
| Shortt (2001) | 1 | 33/53 | 5 | 1/12 | 18.15 (2.18 – 151.38) | 2.90 | 2.88 (0.93 – 8.97) | 1.06 |
| Flannery-Schroeder (2000) | 6* | 17/31 | 0* | 0/12 | 29.14 (1.58 – 538.22) | 3.37 | 20.4 (1.12 – 371.46) | 3.02 |
| Silverman (1999) | 12 | 16/25 | 3 | 2/16 | 12.44 (2.29 – 67.56) | 2.52 | 2.13 (0.64 – 7.16) | 0.76 |
| Barrett (1998) | 6 | 25/34 | 4 | 4/16 | 8.33 (2.13 – 32.60) | 2.12 | 2.5 (0.83 – 7.51) | 0.92 |
| Kendall (1997) | 13* | 25/47* | 11* | 2/23* | 11.93 (2.51 – 56.75) | 2.48 | 1.15 (0.49 – 2.73) | 0.14 |
| Dadds (1997) | 1 | 27/41 | 1 | 27/52 | 1.79 (0.77 – 4.15) | 0.58 | 1.61 (0.70 – 3.69) | 0.47 |
| Barrett (1996) | 0 | 37/53 | 3 | 6/23 | 6.55 (2.18 – 19.68) | 1.88 | 4.37 (1.61 – 11.85) | 1.47 |
| Kendall (1994) | 2* | 16/25* | 0 | 1/20 | 33.78 (3.8 – 295.95) | 3.52 | 27.64 (3.21 – 237.83) | 3.32 |
| Pooled | 134 | 696/1110 | 69 | 88/542 | 8.62 (6.65 – 11.16) | 2.15 | 3.65 (2.95 – 4.52) | 1.29 |
Data extrapolated from other information in the paper.
Notes: WD = withdrawn; R/FU = recovery of those followed-up.
Figure 2. Forest plot for the log odds ratios of the completer sample.
Figure 3. Forest plot of the log odds ratios for the intent-to-treat sample.
Meta-analytic calculations were conducted, weighting the odds ratios according to the inverse of their variance. There was a positive, significant weighted mean effect size for the completer sample, LOR = 2.21; 95% CI = 1.80 – 2.63; se = 0.21; z = 10.37, p < .001. The log odds ratio for the completer sample was exponentiated to allow interpretation of the odds ratio, OR = 9.15. Thus, the odds of recovery from an anxiety disorder was 9.15 times higher for those children in the transdiagnostic CBT treatment group compared to those children in the control group. The data were not homogenous, suggesting that there were between study differences, x2(20) = 31.85, p < .05.
The analysis was repeated for the intent-to-treat sample. There was a positive and significant weighted mean effect size for remission from anxiety for the intention to treat sample, suggesting that transdiagnostic CBT is successful in freeing children from their anxiety disorder diagnoses, LOR = 1.39; 95% CI = 0.98 – 1.79; se = 021; z = 6.71, p < .001. The log odds ratio for the intent=to-treat sample was exponentiated to allow interpretation of the odds ratio, OR = 3.99. Thus, even after adopting a conservative intent-to-treat analysis, the odds of recovery from an anxiety disorder was 3.99 times higher for those children in the transdiagnostic CBT treatment group compared to those children in the control group. The data for this analysis were not homogenous, suggesting that there were between study differences, x2(19) = 43.36, p < .01. However, the Forest Plots in Figures 2 and 3 suggest that the studies were not too dissimilar in both the completer and intent-to-treat samples, as all studies indicated a positive intervention effect and there was considerable overlap of confidence intervals across all of the studies.
Format of treatment delivery
To compare the efficacy of individual and group formats of CBT delivery, meta-analytic calculations were conducted separately for studies that adopted individual versus group formats. Ten studies used individual CBT formats, and eleven studies used group CBT formats (one study used both formats, which is represented in these numbers). There was no significant difference between the log odds ratios of studies adopting individual or group CBT formats for both followed up cases (individual LOR = 2.18 (95% CI = 1.79 – 2.57; OR = 8.83); group LOR = 2.20 (95% CI = 1.48 – 2.92; OR = 9.00)), and for intent-to-treat participants (individual LOR = 1.36 (95% CI = 0.77 – 1.94; OR = 3.88); group LOR = 1.36 (95% CI = 0.84 – 1.87; OR = 3.88)).
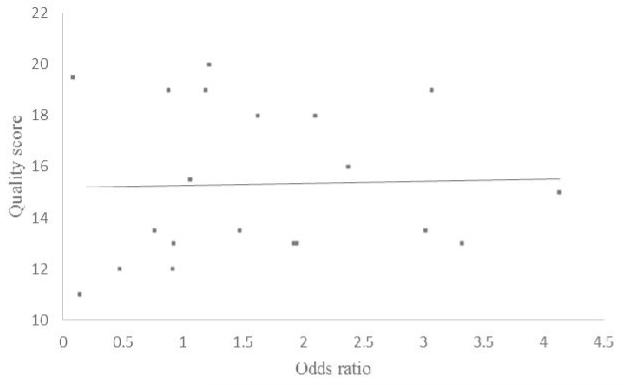
Risk of Bias
A correlational analysis was computed to investigate whether there was a relationship between odds ratio and risk of bias score. Results indicated no significant correlation between effect size and risk of bias score, r = .027, p = .909. A scatter plot of the relationship between these variables is shown in Figure 4.
Figure 4. Scatter plot for the relationship between odds ratios and quality scores for the trials used in the meta-analysis.
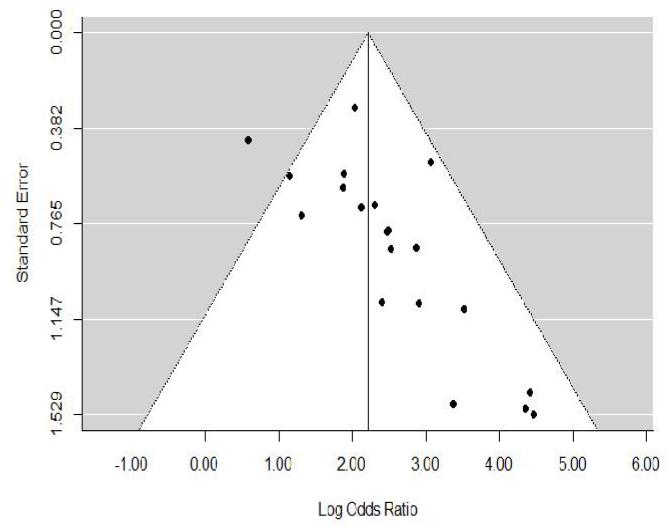
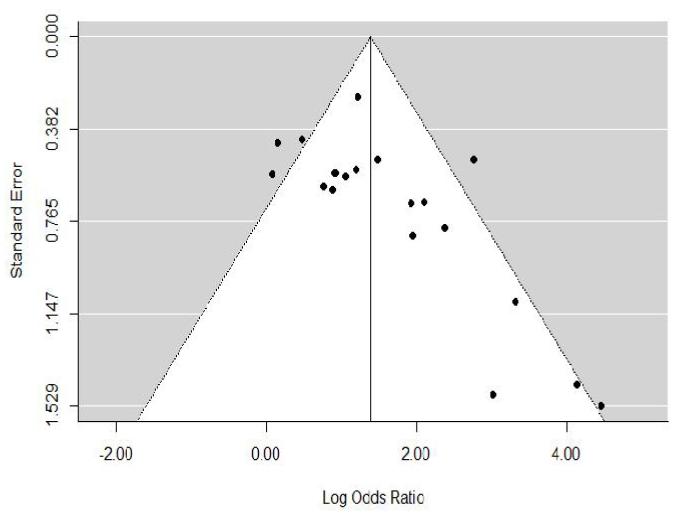
Publication Bias
Funnel plots for the effect sizes of both the completer and intent-to-treat samples were conducted to check for publication bias (Figures 5 and 6). Larger and therefore more precise studies with lower standard errors are expected to have odds ratios closer to the pooled estimate of the treatment effect (indicated by the vertical line through the tip of the funnel), whereas the odds ratios of smaller and less precise studies (higher standard errors) are expected to be more widely distributed around the pooled estimate, thus forming an inverted funnel shape (Cochrane Collaboration, 2002). The results of these funnel plots suggest that there may be an issue of publication bias given the asymmetrical shape of the plot, with no small scale studies with low odds ratios included in this analysis.
Figure 5. Funnel plot of the log odds ratios for the completer sample.
Figure 6. Funnel plot of the log odds ratios for the intent-to-treat sample.
Discussion and conclusion
This meta-analysis provides an important update to the literature of the efficacy of transdiagnostic CBT for treating anxiety disorders in children and young people. The results suggest that transdiagnostic CBT is efficacious for the treatment of anxiety in this age group. The raw odds ratio scores indicated that for the conservative intent-to-treat sample, children in the transdiagnostic CBT group were 3.99 times more likely to remit from their anxiety disorder by post-treatment compared to children in the control group. For completers, children receiving transdiagnostic CBT were 9.15 times more likely to remit by post-treatment than children in the control group. These findings suggest that providing children with transdiagnostic CBT is very efficacious, and would therefore be a suitable alternative for when resources are unavailable to provide specific anxiety-disorder focussed interventions. Previous meta-analyses have generally included trials that adapt CBT according to different anxiety disorders, and so the results of this paper add to the literature by providing support for the use of a transdiagnostic CBT procedure for childhood anxiety disorders. In addition, given the recent changes to the Diagnostic and Statistical Manual for Mental Health Disorders (DSM-5) which removed OCD and PTSD from the anxiety disorder chapter (APA, 2013), it is useful to have results for the efficacy of transdiagnostic CBT for the disorders that remain classified as anxiety disorders. Two of the papers included in this meta-analysis included participants with either PTSD (Cobham, 2012) or OCD (Rapee, Abbott, & Lyneham, 2006), but very few participants out of the sample had these disorders (PTSD, N = 1 out of 55 participants; OCD, N = 13 out of 267 participants) and so it is not expected that the inclusion of these papers has affected the results significantly.
The log odds of recovery found for the intent-to-treat sample of children engaged in transdiagnostic CBT was comparable to the log odds found by Ishikawa et al. (2007), who included studies using specific anxiety disorder focussed interventions (LOR = 1.23, converted from Cohen’s d). This may suggest that transdiagnostic CBT is similarly effective as disorder-specific interventions for the treatment of childhood anxiety disorders. On the other hand, Reynolds et al. (2012) compared generic CBT with disorder-specific CBT and found only a moderate effect size for the effectiveness of generic CBT compared to a medium to large effect size for disorder-specific CBT. However, the disorder-specific CBT trials included different anxiety diagnoses than the generic CBT trials (for example, PTSD, social phobia, OCD, and specific phobias were used in the disorder-specific CBT trials, whereas separation anxiety disorder, social phobia and GAD were used in the generic CBT trials), which does not provide a like-for-like comparison and may explain this different result. In addition, the generic CBT trials used by Reynolds et al. included trials with social phobia diagnoses, yet these trials tend to additionally include social skills training. It is arguable, therefore, that the generic CBT referred to in Reynolds et al.’s paper is not purely transdiagnostic. Further research is needed to compare the efficacy of transdiagnostic CBT with CBT that has been tailored for specific anxiety disorders in children so that conclusions can be drawn as to whether or not it is beneficial to adapt CBT procedures according to type of anxiety. Findings within the adult literature suggest that a transdiagnostic approach to treatment is equally as effective as a disorder-specific treatment, particularly where comorbid disorders are also present (McManus, Shafran, & Cooper, 2010; Norton & Barrera, 2012).
There is a possibility that this meta-analysis is subject to publication bias, as indicated by the results of the funnel plots. However, this risk is considered to be minimal since key authors in the field were contacted to request unpublished articles, and many confirmed that they had no relevant papers to be included in this analysis. Similarly, it is possible that a bias was introduced by only including publications printed in English. Unfortunately resources were unavailable to include studies printed in alternative languages. The risk of bias assessment indicated a moderate risk of bias due to the methods adopted within the studies, which has the potential to lead to inflated effect sizes. However, there was no significant correlation between risk of bias and log odds ratio, which suggests that risk of bias does not significantly influence the conclusions drawn from the results of this meta-analysis.
A decision was made to exclude self-report measures in the current meta-analysis. A limitation of this choice is that beneficial effects of treatment that fell short of reaching clinical cut-offs may not have been recognised. However, the aim of the current analysis was to determine the efficacy of transdiagnostic CBT for helping children to be free from their anxiety disorder diagnosis, and it is only possible to measure this through the use of diagnostic measures.
The use of non-active control groups in the meta-analysis has the potential to inflate effect sizes. However, a decision was made to exclude active controls on the basis that most active control groups contained elements of CBT, which would invalidate a pure comparison of the effectiveness of CBT against controls. Given that this meta-analysis aimed to consider the efficacy of a pure, non-adapted form of CBT on the treatment of anxiety disorders, it seemed logical to also ensure that the control groups were ‘pure’ and contained no elements of CBT. Ideally, we now need randomised controlled trials that allocate control participants to an active control group free of cognitive-behavioural elements, although it is appreciated that designing such an intervention will be challenging.
In specifying inclusion and exclusion criteria, many authors of the papers included in this analysis chose to exclude participants with co-morbid disorders such as behavioural and emotional disorders, learning disabilities, or autistic spectrum disorders. Although their reasons for exclusion are valid, it may be useful for future research to consider the impact of these co-morbidities on the success of CBT. Evidence reported by Ginsburg et al. (2011) suggests that the presence of comorbid internalising disorders can negatively impact remission from an anxiety disorder, although comorbid externalising disorders did not show this same negative effect. By excluding children with comorbid disorders, the generalisability of the studies is compromised, especially considering the evidence that many children with anxiety disorders also suffer from co-morbid disorders such as those excluded from these studies (Hoff Esbjørn et al., 2010; Kendall et al., 2010).
The studies included in this analysis have provided evidence for the efficacy of transdiagnostic CBT across a number of anxiety disorders, including generalised anxiety disorder, separation anxiety disorder, and social phobia. Although children with panic disorder and agoraphobia were also included, there were very few cases of these disorders in any of the trials and so it is not possible to conclude about the efficacy of CBT for these disorders. Moreover, none of the studies included here reported intervention effects for the different disorders, meaning that we do not know whether transdiagnostic CBT is differentially effective for the different anxiety disorders: there is emerging evidence (e.g. Ginsburg et al., 2011) that some anxiety disorders may respond better than others to transdiagnostic CBT. For instance, participants with a social phobia diagnosis at baseline were less likely to remit from their diagnosis after 12 weeks of treatment compared to those without a social phobia diagnosis, whereas this significant difference was not also the case for those with or without generalised anxiety disorder or separation anxiety disorder diagnoses (Ginsburg et al., 2011).
The current meta-analysis includes studies that deliver transdiagnostic CBT using both group and individual CBT formats. The results of the separate analyses for individual and group CBT delivery suggest that transdiagnostic CBT was effective in treating anxiety in children regardless of the format of the treatment. This suggests that there is no additional benefit in Child and Adolescent Mental Health Services offering individual over group CBT treatments for children with anxiety disorders.
In contrast to Cartwright-Hatton et al.’s (2004) findings that there were no randomised controlled studies for the role of CBT in reducing anxiety symptoms for children under the age of six, this review found two studies that included children from the age of four. However, further research is still required to be able to draw conclusions about the success of transdiagnostic CBT with this younger age group, especially considering that many anxiety disorders have very early onsets. Similarly, further research is required to investigate the success of transdiagnostic CBT with adolescents aged 15-18, which is another area with minimal evidence from randomised controlled trials.
In conclusion, this paper confirms that transdiagnostic CBT appears to be an effective treatment for the remission of anxiety in children and young people. It identifies some remaining gaps in the literature, including the efficacy of transdiagnostic CBT across separate anxiety disorders and the impact of comorbid disorders on anxiety remission. There is also a need for more research evidence for the efficacy of transdiagnostic CBT for young children and older teenagers.
Supplementary Material
Acknowledgements
This report is independent research arising, in part, from an NIHR Career Development Award supported by the National Institute for Health Research, and MRC Clinician Scientist Fellowship G108/604, to S. Cartwright-Hatton. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
Footnotes
The forest plot is a representation of the effect size for each study. The squares represent the mean effect size (the size of the square represents the weight of the study in this analysis), and the lines represent the confidence intervals. Effect sizes to the right of the vertical line at zero indicate a positive intervention effect.
References
- APA . Highlights of Changes from DSM-IV-TR to DSM-5. American Psychiatric Association; 2013. Retrieved from http://www.dsm5.org/Pages/Default.aspx. [Google Scholar]
- Bennett K, Manassis K, Walter SD, Cheung A, Wilansky-Traynor P, Diaz-Granados N, Wood JJ. Cognitive behavioral therapy age effects in child and adolescent anxiety: an individual patient data metaanalysis. Depression and Anxiety. 2013 doi: 10.1002/da.22099. doi:10.1002/da.22099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bland JM, Altman DG. Statistics Notes. The odds ratio. British Medical Journal. 2000;320:1468. doi: 10.1136/bmj.320.7247.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cartwright-Hatton S, McNicol K, Doubleday E. Anxiety in a neglected population: prevalence of anxiety disorders in pre-adolescent children. Clinical Psychology Review. 2006;26(7):817–833. doi: 10.1016/j.cpr.2005.12.002. doi:10.1016/j.cpr.2005.12.002. [DOI] [PubMed] [Google Scholar]
- Cartwright-Hatton S, Roberts C, Chitsabesan P, Fothergill C, Harrington R. Systematic review of the efficacy of cognitive behaviour therapies for childhood and adolescent anxiety disorders. The British Journal of Clinical Psychology. 2004;43:421–436. doi: 10.1348/0144665042388928. doi:10.1348/0144665042388928. [DOI] [PubMed] [Google Scholar]
- Chalfant AM, Rapee R, Carroll L. Treating anxiety disorders in children with high functioning autism spectrum disorders: a controlled trial. Journal of Autism and Developmental Disorders. 2007;37(10):1842–57. doi: 10.1007/s10803-006-0318-4. doi:10.1007/s10803-006-0318-4. [DOI] [PubMed] [Google Scholar]
- Cobham VE. Do anxiety-disordered children need to come into the clinic for efficacious treatment? Journal of Consulting and Clinical Psychology. 2012;80(3):465–76. doi: 10.1037/a0028205. doi:10.1037/a0028205. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP. A treatment outcome study for sexually abused preschool children: Initial findings. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35(1):42–50. doi: 10.1097/00004583-199601000-00011. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP. Interventions for sexually abused children: Initial treatment outcome findings. Child Maltreatment. 1998;3(1):17–26. doi:10.1177/1077559598003001002. [Google Scholar]
- Compton SN, March JS, Brent D, Albano AM, Weersing VR, Curry J. Cognitive-behavioral psychotherapy for anxiety and depressive disorders in children and adolescents: An evidence-based medicine review. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(8):930–959. doi: 10.1097/01.chi.0000127589.57468.bf. doi:10.1097/01.chi.0000127589.57468.bf. [DOI] [PubMed] [Google Scholar]
- Davis TE, May A, Whiting SE. Evidence-based treatment of anxiety and phobia in children and adolescents: current status and effects on the emotional response. Clinical Psychology Review. 2011;31(4):592–602. doi: 10.1016/j.cpr.2011.01.001. doi:10.1016/j.cpr.2011.01.001. [DOI] [PubMed] [Google Scholar]
- Field AP, Gillett R. How to do a meta-analysis. The British Journal of Mathematical and Statistical Psychology. 2010;63:665–94. doi: 10.1348/000711010X502733. doi:10.1348/000711010X502733. [DOI] [PubMed] [Google Scholar]
- Ginsburg GS, Kendall PC, Sakolsky D, Compton SN, Piacentini J, Albano AM, March J. Remission after acute treatment in children and adolescents with anxiety disorders: Findings from the CAMS. Journal of Consulting and Clinical Psychology. 2011;79(6):806–813. doi: 10.1037/a0025933. doi:10.1037/a0025933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esbjørn BH, Hoeyer M, Dyrborg J, Leth I, Kendall PC. Prevalence and co-morbidity among anxiety disorders in a national cohort of psychiatrically referred children and adolescents. Journal of Anxiety Disorders. 2010;24(8):866–872. doi: 10.1016/j.janxdis.2010.06.009. doi:10.1016/j.janxdis.2010.06.009. [DOI] [PubMed] [Google Scholar]
- Hofmann SG. Cognitive factors that maintain social anxiety disorder: a comprehensive model and its treatment implications. Cognitive Behavioral Therapy. 2007;36(4):193–209. doi: 10.1080/16506070701421313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- In-Albon T, Schneider S. Psychotherapy of childhood anxiety disorders: A meta-analysis. Psychotherapy and Psychosomatics. 2007;76(1):15–24. doi: 10.1159/000096361. doi:10.1159/000096361. [DOI] [PubMed] [Google Scholar]
- Ishikawa S, Okajima I, Matsuoka H, Sakano Y. Cognitive behavioural therapy for anxiety disorders in children and adolescents: A meta-analysis. Child and Adolescent Mental Health. 2007;12(4):164–172. doi: 10.1111/j.1475-3588.2006.00433.x. doi:10.1111/j.1475-3588.2006.00433.x. [DOI] [PubMed] [Google Scholar]
- James AC, James G, Cowdrey FA, Soler A, Choke A. Cognitive behavioural therapy for anxiety disorders in children and adolescents (Review) Cochrane Database of Systematic Reviews. 2013;(6) doi: 10.1002/14651858.CD004690.pub3. doi:10.1002/14651858.CD004690.pub3. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Compton SN, Walkup JT, Birmaher B, Albano AM, Sherrill J, Piacentini J. Clinical characteristics of anxiety disordered youth. Journal of Anxiety Disorders. 2010;24(3):360–365. doi: 10.1016/j.janxdis.2010.01.009. doi:10.1016/j.janxdis.2010.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein RG. Anxiety disorders. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2009;50(1-2):153–162. doi: 10.1111/j.1469-7610.2008.02061.x. doi:10.1111/j.1469-7610.2008.02061.x. [DOI] [PubMed] [Google Scholar]
- Leyfer O, Gallo KP, Cooper-Vince C, Pincus DB. Patterns and predictors of comorbidity of DSM-IV anxiety disorders in a clinical sample of children and adolescents. Journal of Anxiety Disorders. 2013;27(3):306–11. doi: 10.1016/j.janxdis.2013.01.010. doi:10.1016/j.janxdis.2013.01.010. [DOI] [PubMed] [Google Scholar]
- Warner CM, Colognori D, Kim RE, Reigada LC, Klein RG, Browner-Elhanan KJ, Benkov K, et al. Cognitive-behavioral treatment of persistent functional somatic complaints and pediatric anxiety: an initial controlled trial. Depression and Anxiety. 2011;28(7):551–9. doi: 10.1002/da.20821. doi:10.1002/da.20821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McManus F, Shafran R, Cooper Z. What does a transdiagnostic approach have to offer the treatment of anxiety disorders? The British Journal of Clinical Psychology. 2010;49:491–505. doi: 10.1348/014466509X476567. doi:10.1348/014466509X476567. [DOI] [PubMed] [Google Scholar]
- McNally Keehn RH, Lincoln AJ, Brown MZ, Chavira DA. The Coping Cat program for children with anxiety and autism spectrum disorder: a pilot randomized controlled trial. Journal of Autism and Developmental Disorders. 2013;43(1):57–67. doi: 10.1007/s10803-012-1541-9. doi:10.1007/s10803-012-1541-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris P, Mayer B, den Adel M, Roos T, van Wamelen J. Predictors of change following cognitive-behavioral treatment of children with anxiety problems: a preliminary investigation on negative automatic thoughts and anxiety control. Child Psychiatry and Human Development. 2009;40(1):139–151. doi: 10.1007/s10578-008-0116-7. doi:10.1007/s10578-008-0116-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton PJ, Barrera TL. Transdiagnostic versus diagnosis-specific cbt for anxiety disorders: a preliminary randomized controlled noninferiority trial. Depression and Anxiety. 2012;29(10):874–82. doi: 10.1002/da.21974. doi:10.1002/da.21974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins P. Anxiety disorders in children and adolescents: Research, Assessment and Intervention. Cambridge University Press; Cambridge: 2001. Affective and cognitive processes and the development and maintenance of anxiety and its disorders; pp. 23–44. Retrieved from http://dare.uva.nl/record/113786. [Google Scholar]
- Rapee RM, Abbott MJ, Lyneham HJ. Bibliotherapy for children with anxiety disorders using written materials for parents: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2006;74(3):436–44. doi: 10.1037/0022-006X.74.3.436. doi:10.1037/0022-006X.74.3.436. [DOI] [PubMed] [Google Scholar]
- Reynolds S, Wilson C, Austin J, Hooper L. Effects of psychotherapy for anxiety in children and adolescents: a meta-analytic review. Clinical Psychology Review. 2012;32(4):251–262. doi: 10.1016/j.cpr.2012.01.005. doi:10.1016/j.cpr.2012.01.005. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Pina AA, Viswesvaran C. Evidence-based psychosocial treatments for phobic and anxiety disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2008;37(1):105–30. doi: 10.1080/15374410701817907. doi:10.1080/15374410701817907. [DOI] [PubMed] [Google Scholar]
- Spence SH, Donovan C, Brechman-Toussaint M. The treatment of childhood social phobia: the effectiveness of a social skills training-based, cognitive-behavioural intervention, with and without parental involvement. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2000;41(6):713–726. [PubMed] [Google Scholar]
- Williams TI, Salkovskis PM, Forrester L, Turner S, White H, Allsopp MA. A randomised controlled trial of cognitive behavioural treatment for obsessive compulsive disorder in children and adolescents. European Child and Adolescent Psychiatry. 2010;19(5):449–56. doi: 10.1007/s00787-009-0077-9. doi:10.1007/s00787-009-0077-9. [DOI] [PubMed] [Google Scholar]
- Wood JJ, Drahota A, Sze K, Har K, Chiu A, Langer DA. Cognitive behavioral therapy for anxiety in children with autism spectrum disorders: a randomized, controlled trial. Journal of Child psychology and Psychiatry, and Allied Disciplines. 2009;50(3):224–34. doi: 10.1111/j.1469-7610.2008.01948.x. doi:10.1111/j.1469-7610.2008.01948.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.