Abstract
Objective
To assess differences in receipt of prescription contraception among women with and without chronic medical conditions.
Methods
This observational study used 3 years of administrative claims records for insured women aged 21–45 years who were enrolled in a commercial insurance company in Michigan between 2004 and 2009. Women were considered to have a chronic medical condition if they had at least two claims for one of the following conditions, in order of prevalence in our study population: hypertension, asthma, hypothyroidism, diabetes, obesity, rheumatoid arthritis, inflammatory bowel disease, or systemic lupus erythematosus. Our primary outcome was receipt of prescription contraception, defined by a pharmacy claim or diagnostic or procedural code. We used multivariable logistic regression to estimate the association of chronic condition status with the odds of receiving prescription contraception within 3 years, adjusting for age, community-level socioeconomic status, total outpatient visits, and cervical cancer screening.
Results
Of 11,649 women studied, 16.0% (n=1,862) had at least one of the chronic conditions we considered. Of those with a chronic condition, 33.5% (n=623) received prescription contraception during the 3-year study period compared to 41.1% (n=4,018) of those without a chronic condition (p<0.001). After adjusting for covariates, women with a chronic condition remained less likely than women without a chronic condition to have received prescription contraception (adjusted odds ratio=0.85; 95% CI 0.76, 0.96; p=0.010).
Conclusion
Despite a greater risk for adverse outcomes with an unplanned pregnancy, women with these chronic conditions were less likely to receive prescription contraception.
BACKGROUND
Women with chronic medical conditions are more likely than women without chronic conditions to report that their pregnancy was unintended(1) and unintended pregnancy rates as high as 50–60% have been reported in this population(2–4). Unintended pregnancy has significant implications for women with many chronic conditions given their higher risk for pregnancy-related maternal and fetal complications, including congenital heart defects in diabetes mellitus(5), stillbirth in rheumatoid arthritis(6), and pre-eclampsia in women with asthma(7).
Among women with chronic medical conditions, family planning services, including contraceptive counseling and provision, are crucial to preventing unintended pregnancy and to reducing pregnancy-related complications.(8–13) Prior studies examining the relationship between chronic conditions and contraceptive use have yielded inconsistent results(1, 14–18) and have been limited by their use of cross-sectional, retrospective(14) and self-reported data(14, 16, 17). Some studies focusing on single diseases, such as diabetes mellitus, have reported lower rates of receipt of contraceptive counseling, prescriptions, or services among women with these conditions.(18) It is unclear whether chronic disease management overall or for specific diseases (e.g., concern over hormonal methods in women with hypertension) impacts the provision of contraception. Additional research is needed to clarify receipt of contraceptive services among reproductive-aged women, especially for a broader range of chronic conditions.
The objective of this study was to examine differentials in receipt of contraception by chronic medical condition status. Specifically, we compared receipt of prescription contraception over a 3-year period between women with and without chronic medical conditions who were enrolled in a commercial health plan.
MATERIALS AND METHODS
This study used administrative claims data from women enrolled in a commercial health plan. Our study sample was drawn from a larger study of women with at least 54 months of continuous enrollment in Blue Care Network of Michigan. Blue Care Network is a large commercial health insurance plan with 4,500 primary care providers, including Title X providers. Blue Care Network provides medical and pharmacy benefits to over 640,000 members. The Blue Care Network insurance claims database contained information regarding member year of birth, zip code, visit-level data on medical diagnoses and procedures, and pharmacy-(i.e. prescription) or provider-dispensed (i.e. inserted) contraception. All study data was extracted from de-identified Blue Care Network administrative claims that were submitted to Blue Care Network by healthcare providers on a daily basis. The Medical Informatics department at Blue Care Network builds tables for claims analysis based upon the claims received. According to Blue Care Network, there is an extensive and rigorous monthly process that checks for data integrity and accuracy before the data is used for analysis, in addition to routine audits to confirm the accuracy of claims submitted by providers. This study was reviewed by the University of Michigan Medical School Institutional Review Board and received exempt status because the data did not contain any identifiable patient information.
Data was available for claims occurring between January 1, 2004 and December 31, 2009. An index date in 2004, 2005 or 2006 was randomly assigned to mark the beginning of a 3-year observation period. International Classification of Diseases, 9th Revision (ICD9), Healthcare Common Procedure Coding System (HCPCS), and Current Procedural Terminology (CPT) codes associated with each billed visit were extracted from the database.
In order to examine women who were between 21 and 45 years of age throughout the 3-year observation period, women who were 21–42 years old at baseline were included in this analysis. Additional inclusion criteria were: 1) at least 54 months of continuous enrollment, where the first 6 months were used to identify baseline characteristics and a subsequent 36-month period was used for measuring the exposure and outcome variables, 2) benefit coverage of contraceptive services and prescriptions throughout the 54-month continuous enrollment period, and 3) at least two outpatient visits between 2004 and 2009. While Blue Care Network offers several HMO plans, including Medicaid, only women enrolled in commercial insurance plans were included in this study (no Medicaid beneficiaries met the 54-month continuous enrollment criteria). Women with a hysterectomy were excluded, as were women with a code consistent with ineligibility for contraception (i.e. sterilization). We also excluded women with evidence of a pregnancy during the observation period to ensure that all women were potentially eligible for contraception.
Our primary outcome was receipt (yes or no) of prescription contraception during the 3-year study period. We examined pharmacy claims for hormonal contraceptive methods (i.e. oral contraceptives [OCs], medroxyprogesterone acetate injections, vaginal rings, and transdermal contraceptives). Outpatient visit claims were used to identify provision of long-acting reversible contraception (intrauterine devices [IUDs] and subdermal implants). Diagnostic or procedural codes were used to identify IUD and implant placement, surveillance, and removal. Our secondary outcome was the proportion of months with a supply of contraception over the 36-month study period among women who had ever received prescription contraception. For pills, patches, and rings, we added the number of months supplied based on pharmacy claims. Each Depo-Provera injection was converted to a 3-month supply. Months supplied for intrauterine contraception and implants were calculated based on the number of months between the date of placement and the date of removal. For those with only placement or removal codes, months of coverage were calculated as the study end date minus the device placement date or as the removal date minus the index date. Those with no IUD placement or removal date who had an ICD9 code for IUD surveillance were assigned a full 12 months of contraception for the year in which surveillance occurred.
Our primary exposure variable was the presence or absence of one or more chronic medical conditions, for which we coded women yes or no as having any of the following chronic conditions (in order of prevalence within our study population): uncomplicated hypertension, asthma, hypothyroidism, diabetes, obesity, rheumatoid arthritis (RA), inflammatory bowel disease, and systemic lupus erythematosus (SLE). We considered a range of chronic conditions that are relatively common among reproductive-aged women(19), require frequent interaction with health care providers, and provided a sufficient analytic sample size. Other conditions, such as depression and sickle cell disease, were initially included but ultimately excluded due to insufficient sub-sample sizes, unreliable diagnostic coding, or both. We classified individuals as having a chronic medical condition if they had one or more of the eligible conditions identified by at least two visits with diagnostic codes corresponding to that specific condition.(20–22) Women were classified as having "no chronic condition” if they did not have any of the chronic diagnoses listed above or if they had fewer than two visits with a disease code.
Cervical cancer screening was included as a covariate because we hypothesized that contraceptive services might occur at the time of other preventive reproductive health services, such as cervical cancer screening. All outpatient visits were used to identify receipt of cervical cancer screening using relevant CPT and HCPCS codes. This covariate was categorized into none, one episode, or two or more episodes over the 3-year observation period.
Other covariates included characteristics of health care visits and participants. Visits were classified as problem-focused or health maintenance based on HCPCS codes. Age was included as a categorical variable (21–29 years old or 30–42 years old, because recommendations for the frequency of cervical cancer screening differ by these age groups).(23) Member zip codes were used to link to the 2006–2010 American Community Survey data from the Census Bureau to create a community-level indicator of socioeconomic status (median income at <200% or ≥200% of the federal poverty level for 2006).(24)
We first examined bivariate associations between chronic condition status (overall and for specific diseases), covariates and our primary outcome (i.e., receipt of prescription contraception), using Chi-square tests. A sub-analysis of those who received any contraception was performed using the Wilcoxon Rank Sum test to examine differences in the mean proportion of months of contraception over the 3-year study period between women with and without chronic conditions. Multivariable logistic regression was then used to examine the relationship between the presence of a chronic condition and receipt of prescription contraception within 3 years while controlling for other covariates. Covariates that were significantly related to the exposure, outcome, or the exposure and outcome in bivariate analyses (p <0.05) were included in the multivariable regression analysis. Finally, differences in the proportion of months with a supply of contraception between women with and without chronic conditions were examined using multivariable linear regression.
In order to detect a 15% difference in receipt of contraception between women with and without a chronic medical condition(18), with an alpha of 0.05 and 80% power, we needed a sample of 382 women per group. All data analyses were performed using SAS statistical software version 9.3 (SAS Institute, Cary, NC). A two-sided p-value < 0.05 was considered statistically significant.
RESULTS
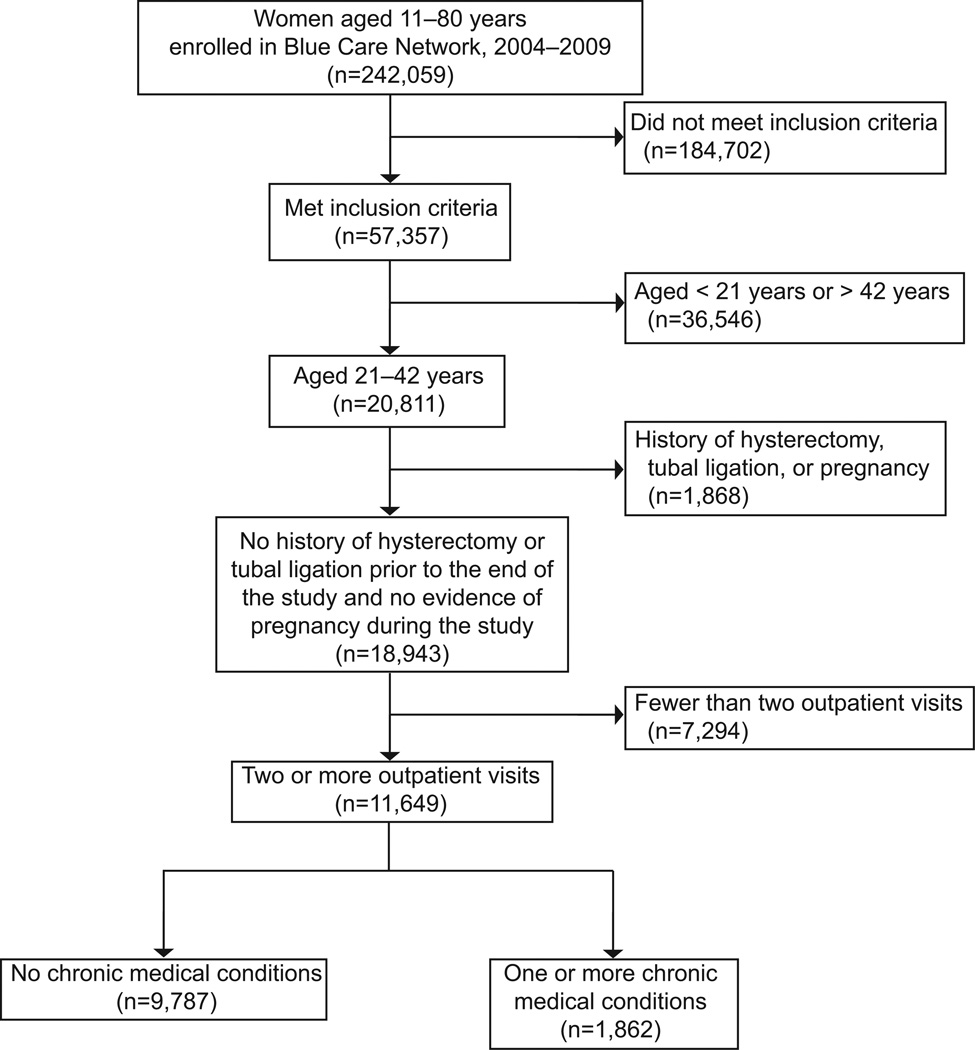
The selection of our sample is presented in Figure 1. Of our final sample (n=11,649), 16.0% (n=1,862) met criteria for at least one chronic condition. The prevalence rates of chronic conditions were as follows: hypertension (5.5%), asthma (4.6%), hypothyroidism (3.7%), diabetes (3.3%), obesity (2.9%), RA (0.6%), inflammatory bowel disease (0.4%), and SLE (0.2%). Table 1 presents the baseline characteristics of women by chronic condition status. A higher proportion of women with chronic conditions experienced a health maintenance examination (58.3% vs. 30.1%; p<0.001) compared to their counterparts. Women with chronic conditions also had more outpatient visits on average over the 3 years than women without a chronic condition (mean visits 16.0 vs. 4.9; p<0.001). Similarly, higher proportions of women with chronic conditions had cervical cancer screening at least once in 3 years than their counterparts without a chronic condition (56.8% vs. 44.1% for women 21–29 years old and 57.2% vs. 44.2% for women 30–42 years old; p<0.001 for both comparisons).
Figure 1. Study Design.
Inclusion criteria: subjects were required to have 1) at least 54 months of continuous enrollment, 2) benefit coverage of contraceptive services and prescriptions throughout the 54-month continuous enrollment period, and 3) at least two outpatient visits between 2004 and 2009.
Table 1.
Demographic and Health Care Visit Characteristics of Eligible, Insured Women Aged 21–42 Years Enrolled in Blue Care Network of Michigan by Chronic Condition Status
| Total (n=11,649) |
No Chronic Condition (n=9,787) |
Chronic Condition (n=1,862) |
P | ||
|---|---|---|---|---|---|
| Age (y)† | 0.065 | ||||
| 21–29 | 2,637 (22.6) | 2,246 (23.0) | 391 (21.0) | ||
| 30–42 | 9,012 (77.4) | 7,541 (77.0) | 1,471 (79.0) | ||
| Race† | |||||
| White | 8,435 (72.4) | 7,087 (72.4) | 1,348 (72.4) | 0.380 | |
| Black | 1,408 (12.1) | 1,179 (12.1) | 229 (12.3) | ||
| Other (non-Hispanic) | 359 (3.1) | 313 (3.2) | 46 (2.5) | ||
| Missing | 1,447 (12.4) | 1,208 (12.3) | 239 (12.8) | ||
| Community-level socioeconomic status† | 0.038 | ||||
| < 200% FPL | 1,636 (14.1) | 1,346 (13.8) | 290 (15.7) | ||
| ≥ 200% FPL | 9,952 (85.9) | 8,390 (86.2) | 1,562 (84.3) | ||
| Missing | 61 (0.5) | 51 (0.5) | 10 (0.5) | ||
| No. of chronic conditions | -- | ||||
| 1 | -- | -- | 1,396 (75.0) | ||
| ≥2 | -- | -- | 466 (25.0) | ||
| Outpatient visits ‡ | <0.001 | ||||
| Total in 3 years | 6.7 ± 0.1 | 4.9 ± 0.1 | 16.0 ± 0.4 | ||
| Average per year | 2.2 ± 0.0 | 1.6 ± 0.0 | 5.3 ± 0.1 | ||
| Had a health maintenance visit† | 4,026 (34.6) | 2,941 (30.1) | 1,085 (58.3) | <0.001 | |
| No. years with cervical cancer screening, by age (y)† | |||||
| 21–29 | <0.001 | ||||
| 0 | 1,425 (56.4) | 1,256 (55.9) | 169 (43.2) | ||
| 1 | 842 (31.9) | 725 (32.3) | 117 (29.9) | ||
| ≥2 | 370 (14.0) | 265 (11.8) | 105 (26.9) | ||
| 30–42 | <0.001 | ||||
| 0 | 4,844 (53.8) | 4,214 (55.9) | 630 (42.8) | ||
| 1 | 2,745 (30.5) | 2,289 (30.4) | 456 (31.0) | ||
| ≥2 | 1,423 (15.8) | 1,038 (13.8) | 385 (26.2) | ||
| Received contraception in 3 years, by age (y)† | |||||
| Overall | 4,641 (39.8) | 4,018 (41.1) | 623 (33.5) | <0.001 | |
| 21–29 | 1,708 (64.8) | 1,489 (66.3) | 219 (56.0) | ||
| 30–45 | 2,933 (32.6) | 2,529 (33.5) | 404 (27.5) | ||
| Proportion of months in 3 years with contraception supply among contraceptive users, by age (y) ‡ | 0.025 | ||||
| Overall | 0.54 ± 0.0 | 0.55 ± 0.0 | 0.51 ± 0.0 | ||
| 21–29 | 0.54 ± 0.0 | 0.54 ± 0.0 | 0.52 ± 0.0 | ||
| 30–42 | 0.55 ± 0.0 | 0.55 ± 0.0 | 0.51 ± 0.0 | ||
FPL, federal poverty level.
Data are n(%). Proportions with chronic conditions across covariate groups were compared using the Chi-square test.
Data are mean ± standard error of the mean. Mean proportions of contraceptive supply across age groups were compared using the Wilcoxon Rank Sum test.
Overall, 39.8 % (n=4,641) of women ever received prescription contraception during their 3-year observation period. Among contraceptive users, hormonal methods (n=4,367 [94.1%]) were more common than long-acting reversible methods (n=274 [5.9%]).
Fewer women with chronic conditions (33.5%) than without a chronic condition (41.1%) ever received prescription contraception (p<0.001) (Table 1). After adjusting for covariates, women with at least one chronic condition were less likely than those without a chronic condition to have received any prescription contraception (adjusted odds ratio [OR] = 0.85, 95% CI: 0.76 – 0.96; Table 2).
Table 2.
Bivariate and Multivariable Logistic Regression of Receipt of Prescription Contraception in 3-Year Study Period by Chronic Medical Condition Status
| OR* | 95% CI | P | Adjusted OR† | 95% CI | P | ||
|---|---|---|---|---|---|---|---|
| Presence of ≥1 chronic medical conditions | 0.72 | 0.65, 0.80 | <0.001 | 0.85 | 0.76, 0.96 | 0.010 | |
| Age (y) | |||||||
| 21–29 | 3.81 | 3.48, 4.17 | <0.001 | 3.82 | 3.49, 4.19 | <0.001 | |
| 30–42 | Ref | -- | -- | Ref | -- | -- | |
| Community-level socioeconomic status | |||||||
| < 200% FPL | 0.93 | 0.84, 1.04 | 0.205 | 0.91 | 0.81, 1.02 | 0.094 | |
| ≥ 200% FPL | Ref | -- | -- | Ref | -- | -- | |
| No. years with cervical cancer screening | |||||||
| 0 | Ref | -- | -- | Ref | -- | -- | |
| 1 | 1.08 | 0.99, 1.17 | 0.078 | 1.11 | 1.02, 1.21 | 0.022 | |
| ≥2 | 0.82 | 0.73, 0.91 | <0.001 | 0.97 | 0.86, 1.10 | 0.587 | |
| Total outpatient visits | 0.98 | 0.98, 0.99 | <0.001 | 0.99 | 0.98, 0.99 | <0.001 | |
OR, odds ratio; CI, confidence interval; FPL, federal poverty level.
Point estimates shown for each variable from univariate models.
Point estimates from multivariable regression models for the effect of each disease on the odds of receipt of contraception adjusting for all covariates including: age group, community-level socioeconomic status, no. of years with cervical cancer screening, and total outpatient visits.
Other covariates significantly associated with receipt of contraception in multivariable models included the number of outpatient visits over 3 years (adjusted OR = 0.99, 95% CI: 0.98 – 0.99), yearly cervical cancer screening (adjusted OR = 1.11, 95% CI: 1.02 – 1.21), and younger age group (adjusted OR = 3.82, 95% CI: 3.49 – 4.19) (Table 2).
Results were similar in nearly all sub-analyses for specific chronic conditions. In unadjusted analyses, women with hypertension, hypothyroidism, diabetes, asthma, inflammatory bowel disease, and RA had lower rates of receiving contraception than women without those conditions (Table 3). In multivariable models, there were no longer any differences in receipt of contraception between women with each individual chronic condition and those with no chronic condition after adjusting for covariates (Table 3).
Table 3.
Logistic Regression of Receipt of Prescription Contraception in 3-Year Study Period by Chronic Medical Condition Status for Selected Conditions
| Univariate* | Multivariate† | ||||||
|---|---|---|---|---|---|---|---|
| Proportion using contraception in 3 years (%) |
OR | 95% CI | P | Adjusted OR |
95% CI | P | |
| No chronic condition | 41.1 | -- | -- | -- | -- | -- | -- |
| Hypertension | 31.4 | 0.66 | 0.55, 0.78 | <0.001 | 0.83 | 0.68, 1.00 | 0.051 |
| Asthma | 35.7 | 0.80 | 0.67, 0.96 | 0.014 | 1.01 | 0.82, 1.23 | 0.943 |
| Hypothyroidism | 33.3 | 0.72 | 0.58, 0.88 | 0.001 | 0.95 | 0.76, 1.19 | 0.668 |
| Diabetes | 34.2 | 0.75 | 0.60, 0.93 | 0.008 | 0.95 | 0.75, 1.20 | 0.663 |
| Obesity | 35.8 | 0.80 | 0.64, 1.01 | 0.058 | 1.05 | 0.82, 1.35 | 0.683 |
| Rheumatoid arthritis | 20.0 | 0.36 | 0.20, 0.66 | 0.001 | 0.53 | 0.28, 1.00 | 0.051 |
| Inflammatory bowel disease | 24.0 | 0.45 | 0.24, 0.87 | 0.017 | 0.56 | 0.28, 1.12 | 0.099 |
| Systemic lupus erythematosus | 21.7 | 0.40 | 0.15, 1.08 | 0.070 | 0.75 | 0.26, 2.12 | 0.582 |
OR, odds ratio; CI, confidence interval.
Point estimates from univariate models for the effect of each disease on the odds of receipt of contraception.
Point estimates from multivariable regression models for the effect of each disease on the odds of receipt of contraception adjusting for all covariates including: age group, community-level socioeconomic status, no. of years with cervical cancer screening, and total outpatient visits.
Among those who received prescription contraception (n=4,641), the unadjusted mean proportion of months of contraceptive supply was lower in women with chronic conditions (0.51) than in women without chronic conditions (0.55; p=0.025). After adjusting for covariates, however, the mean proportion of months of supply was similar between women with and without chronic conditions (β = −0.02, 95% CI: −0.05 – 0.01, p=0.255; data not shown).
DISCUSSION
We found that commercially insured women with chronic conditions received prescription contraception at a lower rate than their healthy counterparts, potentially placing them at risk for unintended pregnancy and pregnancy-related sequelae. Our findings, along with others (18), point to missed opportunities to reduce these risks among women with chronic conditions.
Women in our study had insurance coverage for contraception and were seen at least twice by a health care provider over 3 years. While other preventive services, like cancer screening, might benefit from a higher frequency of health care encounters (25), we found that more frequent visits were associated with a lower odds of receiving contraception. Although understudied, time constraints, competing medical priorities, and a lack of provider knowledge appear to be barriers to contraceptive-related service delivery in women with chronic conditions. (18, 26) In addition, the considerable amount of time required for contraceptive counseling and the fact that contraceptive services are poorly integrated into preventive care may further compound the problem.(26)
We recognize that women with chronic conditions may have contraindications to some contraceptive methods, which we were unable to measure here. However, even women with chronic conditions should have at least one effective option (e.g. non-hormonal copper-containing IUD)(27, 28), but may not be offered these methods by their providers. Previous studies demonstrate that providers overestimate the adverse health consequences of contraceptive methods in certain chronic conditions. For instance, Eisenberg et al(29) and Toomey et al(30) suggest that providers are uncomfortable prescribing contraceptives to patients they perceive to be at higher risk for adverse events, such as those with diabetes and hypertension. This reluctance persists despite the availability of evidence-based guidelines on contraception eligibility among women with chronic conditions.(27, 28)
Under the Affordable Care Act, insurance coverage of the full range of contraceptive methods and associated office visits is required without co-payment. The ongoing debate surrounding contraceptive coverage provides an opportunity to clarify what aspects of our health system should be targeted to decrease unintended pregnancy, including contraceptive services for women with chronic conditions. For instance, our previous work demonstrated that lower out-of-pocket costs are associated with an increase in IUD use among commercially insured women.(31) By requiring insurance coverage for long-acting contraceptive methods, women with chronic medical conditions may have improved access to safe, highly effective methods. Further research on the impact of the ACA on women’s health should include an assessment of its effects on the delivery of all preventive women’s health services, including contraceptive services.
We recognize several limitations in our study. First, the use of claims data limited our ability to directly measure pregnancy intention and contraceptive behaviors. We could not measure whether women actually used their contraceptive pills. Second, we could not assess the use of out-of-plan services or uncovered methods, such as non-formulary pills, condoms, or partner sterilization. Thus, we may have underestimated the prevalence of contraceptive use in this population. Additionally, our results may not be representative of all reproductive-aged women with chronic conditions. As would be expected due to our selection criteria, our study population is slightly older than women in the National Survey of Family Growth, but similar otherwise. Rates of prescription contraception in our study seem slightly lower than expected based on National Survey of Family Growth data for privately insured, non-sterilized women.(32) In part, this observation may be due to differences in ascertainment (claims data vs. self-report), use of out-of-plan services, or regional practice patterns, which make direct comparisons difficult. Moreover, there is a dearth of information on population-based contraceptive prevalence rates among women with chronic conditions. Finally, an adequate analysis of specific chronic conditions was precluded by small sample sizes and inadequate power.
Despite these limitations, findings from our study provide additional evidence that women with a range of chronic conditions are at increased risk for unintended pregnancy compared to their healthy counterparts. Multifaceted interventions targeting provider training, care coordination, and individual behavior are likely required to improve contraception use among women with chronic conditions. Women with chronic conditions often receive their care from primary care providers, who may lack sufficient knowledge and training to offer the full range of contraceptive options.(33, 34) These encounters represent missed opportunities. Enhancing contraception education in residency training programs is clearly needed. Possible approaches include enhanced contraception education in primary care training, adoption of clinical decision support aids to increase the efficiency and accuracy of contraceptive counseling, and engaging health plans or systems to include family planning in ongoing efforts to improve coordination between providers, including adopting relevant quality measures.
Acknowledgments
Supported by the Blue Cross Blue Shield of Michigan Foundation (Dalton; Award #1814II). The research training program for Anna DeNoble was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (Grant #2TL1TR000435) through the Michigan Institute for Clinical and Health Research. Kelli Hall’s work was supported by NICHD Building Interdisciplinary Research Careers in Women’s Health “BIRCWH” K-12 Career Development Award #K12HD001438 (PI Johnson).
Financial Disclosure: Dr. Dalton has received funding from McNeil to participate on an advisory committee.
The authors thank Tom Fraser, Kathleen Pruchnik, and Blue Care Network of Michigan for providing the study data and logistical support.
Footnotes
The other authors did not report any potential conflicts of interest.
REFERENCES
- 1.Chor J, Rankin K, Harwood B, Handler A. Unintended pregnancy and postpartum contraceptive use in women with and without chronic medical disease who experienced a live birth. Contraception. 2011;84(1):57–63. doi: 10.1016/j.contraception.2010.11.018. [DOI] [PubMed] [Google Scholar]
- 2.Holing EV, Beyer CS, Brown ZA, Connell FA. Why don't women with diabetes plan their pregnancies? Diabetes care. 1998;21(6):889–895. doi: 10.2337/diacare.21.6.889. [DOI] [PubMed] [Google Scholar]
- 3.Davis AR, Pack AM, Kritzer J, Yoon A, Camus A. Reproductive history, sexual behavior and use of contraception in women with epilepsy. Contraception. 2008;77(6):405–409. doi: 10.1016/j.contraception.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84(5):478–485. doi: 10.1016/j.contraception.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu S, Joseph KS, Lisonkova S, Rouleau J, Van den Hof M, Sauve R, et al. Association Between Maternal Chronic Conditions and Congenital Heart Defects: A Population-Based Cohort Study. Circulation. 2013;128(6):583–589. doi: 10.1161/CIRCULATIONAHA.112.001054. [DOI] [PubMed] [Google Scholar]
- 6.Nørgaard M, Larsson H, Pedersen L, Granath F, Askling J, Kieler H, et al. Rheumatoid arthritis and birth outcomes: a Danish and Swedish nationwide prevalence study. J Intern Med. 2010;268(4):329–337. doi: 10.1111/j.1365-2796.2010.02239.x. [DOI] [PubMed] [Google Scholar]
- 7.Murphy VE, Namazy JA, Powell H, Schatz M, Chambers C, Attia J, et al. A meta-analysis of adverse perinatal outcomes in women with asthma. BJOG. 2011;118(11):1314–1323. doi: 10.1111/j.1471-0528.2011.03055.x. [DOI] [PubMed] [Google Scholar]
- 8.Lipscombe LL, McLaughlin HM, Wu W, Feig DS. Pregnancy planning in women with pregestational diabetes. J Matern Fetal Neonatal Med. 2011;24(9):1095–1101. doi: 10.3109/14767058.2010.545929. [DOI] [PubMed] [Google Scholar]
- 9.Tripathi A, Rankin J, Aarvold J, Chandler C, Bell R. Preconception counseling in women with diabetes: a population-based study in the north of England. Diabetes care. 2010;33(3):586–588. doi: 10.2337/dc09-1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ray JG, O'Brien TE, Chan WS. Preconception care and the risk of congenital anomalies in the offspring of women with diabetes mellitus: A meta-analysis. QJM. 2001;94(8):435–444. doi: 10.1093/qjmed/94.8.435. [DOI] [PubMed] [Google Scholar]
- 11.Schwarz EB, Manzi S. Risk of unintended pregnancy among women with systemic lupus erythematosus. Arthritis Rheum. 2008;59(6):863–866. doi: 10.1002/art.23712. [DOI] [PubMed] [Google Scholar]
- 12.Kinsley B. Achieving better outcomes in pregnancies complicated by type 1 and type 2 diabetes mellitus. Clin Ther. 2007;29(Suppl D):S153–S160. doi: 10.1016/j.clinthera.2007.12.015. [DOI] [PubMed] [Google Scholar]
- 13.McElvy SS, Miodovnik M, Rosenn B, Khoury JC, Siddiqi T, Dignan PS, et al. A focused preconceptional and early pregnancy program in women with type 1 diabetes reduces perinatal mortality and malformation rates to general population levels. J Matern Fetal Med. 2000;9(1):14–20. doi: 10.1002/(SICI)1520-6661(200001/02)9:1<14::AID-MFM5>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 14.Perritt JB, Burke A, Jamshidli R, Wang J, Fox M. Contraception counseling, pregnancy intention and contraception use in women with medical problems: an analysis of data from the Maryland Pregnancy Risk Assessment Monitoring System (PRAMS) Contraception. 2013;88(2):263–268. doi: 10.1016/j.contraception.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 15.Steinkellner A, Chen W, Denison SE. Adherence to oral contraception in women on Category X medications. Am J Med. 2010;123(10):929.e1–934.e1. doi: 10.1016/j.amjmed.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 16.Chuang CH, Chase GA, Bensyl DM, Weisman CS. Contraceptive use by diabetic and obese women. Womens Health Issues. 2005;15(4):167–173. doi: 10.1016/j.whi.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 17.Yazdany J, Trupin L, Kaiser R, Schmajuk G, Gillis JZ, Chakravarty E, et al. Contraceptive counseling and use among women with systemic lupus erythematosus: a gap in health care quality? Arthritis Care Res. 2011;63(3):358–365. doi: 10.1002/acr.20402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schwarz EB, Postlethwaite D, Hung YY, Lantzman E, Armstrong MA, Horberg MA. Provision of contraceptive services to women with diabetes mellitus. J Gen Intern Med. 2012;27(2):196–201. doi: 10.1007/s11606-011-1875-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hayes DK, Fan AZ, Smith RA, Bombard JM. Trends in selected chronic conditions and behavioral risk factors among women of reproductive age, behavioral risk factor surveillance system, 2001–2009. Prev Chronic Dis. 2011;8(6):A120. [PMC free article] [PubMed] [Google Scholar]
- 20.O'Connor PJ, Rush WA, Pronk NP, Cherney LM. Identifying diabetes mellitus or heart disease among health maintenance organization members: sensitivity, specificity, predictive value, and cost of survey and database methods. Am J Manag Care. 1998;4(3):335–342. [PubMed] [Google Scholar]
- 21.Chibnik LB, Massarotti EM, Costenbader KH. Identification and validation of lupus nephritis cases using administrative data. Lupus. 2010;19(6):741–743. doi: 10.1177/0961203309356289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rector TS, Wickstrom SL, Shah M, Thomas Greeenlee N, Rheault P, Rogowski J, et al. Specificity and sensitivity of claims-based algorithms for identifying members of Medicare+Choice health plans that have chronic medical conditions. Health Serv Res. 2004;39(6 Pt 1):1839–1857. doi: 10.1111/j.1475-6773.2004.00321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.American College of Obstetricians and Gynecologists. ACOG Practice Bulletin Number 131: Screening for cervical cancer. Obstet Gynecol. 2012:1222–1238. doi: 10.1097/aog.0b013e318277c92a. [DOI] [PubMed] [Google Scholar]
- 24.University of Michigan Population Studies Center. Zip Code Characteristics: Mean and Median Household Income. Ann Arbor, MI: University of Michigan Institute for Social Research; Available at: http://www.psc.isr.umich.edu/dis/census/Features/tract2zip/index.html. Retrieved August 12, 2013. [Google Scholar]
- 25.Fontana SA, Baumann LC, Helberg C, Love RR. The delivery of preventive services in primary care practices according to chronic disease status. Am J Public Health. 1997;87(7):1190–1196. doi: 10.2105/ajph.87.7.1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Akers AY, Gold MA, Borrero S, Santucci A, Schwarz EB. Providers' perspectives on challenges to contraceptive counseling in primary care settings. J Womens Health (Larchmt) 2010;19(6):1163–1170. doi: 10.1089/jwh.2009.1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Curtis KM, Jamieson DJ, Peterson HB, Marchbanks PA. US medical eligibility criteria for contraceptive use, 2010: adapted from the World Health Organization Medical Eligibility Criteria for Contraceptive Use: Department of Health and Human Services. Centers for Disease Control and Prevention. 2010 [Google Scholar]
- 28.World Health Organization. Reproductive Health and Research, K4Health. Medical eligibility for contraceptive use. World Health Organization; 2009. [Google Scholar]
- 29.Eisenberg DL, Stika C, Desai A, Baker D, Yost KJ. Providing contraception for women taking potentially teratogenic medications: a survey of internal medicine physicians' knowledge, attitudes and barriers. J Gen Intern Med. 2010;25(4):291–297. doi: 10.1007/s11606-009-1215-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Toomey D, Waldron B. Family planning and inflammatory bowel disease: the patient and the practitioner. Family Practice. 2013;30(1):64–68. doi: 10.1093/fampra/cms035. [DOI] [PubMed] [Google Scholar]
- 31.Pace LE, Dusetzina SB, Fendrick AM, Keating NL, Dalton VK. The Impact of Out-of-Pocket Costs on the Use of Intrauterine Contraception Among Women With Employer-sponsored Insurance. Med Care. 2013;51(11):959–963. doi: 10.1097/MLR.0b013e3182a97b5d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jones J, Mosher W, Daniels K. Current contraceptive use in the United States, 2006–2010, and changes in patterns of use since 1995. National health statistics reports. 2012;60:1–25. [PubMed] [Google Scholar]
- 33.Schreiber CA, Harwood BJ, Switzer GE, Creinin MD, Reeves MF, Ness RB. Training and attitudes about contraceptive management across primary care specialties: a survey of graduating residents. Contraception. 2006;73(6):618–622. doi: 10.1016/j.contraception.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 34.Spencer AL, Kern LM. Primary care program directors' perceptions of women's health education: a gap in graduate medical education persists. J Womens Health (Larchmt) 2008;17(4):549–556. doi: 10.1089/jwh.2007.0473. [DOI] [PubMed] [Google Scholar]