Summary
Significant integrative advances are needed for intraoperative optical coherence tomography (iOCT) to achieve widespread use across ophthalmic surgery. A surgeon feedback system that provides microscope integration, heads-up display, and foot pedal control of the OCT scan location represents a major interval advance in ophthalmic surgery. In this report, we describe the preliminary findings of the DISCOVER study, a multi-surgeon investigational device study examining the role of microscope integrated iOCT systems with surgeon heads-up display feedback (e.g., Carl Zeiss Meditec RESCAN 700, Cole Eye Institute iOCT prototype). During surgical maneuvers in anterior segment and posterior segment surgery, this technology provides rapid visualization of the area of interest and provides the surgeon with information regarding instrument-tissue interactions. This system represents a major advance in iterative technology for iOCT and may provide the first widely available platform for surgeons to seamlessly assimilate this technology into the operating room theater.
Introduction
The widespread adoption of optical coherence tomography (OCT) across ophthalmology has transformed clinical care for ophthalmic diseases. Evidence continues to build regarding the utility of intraoperative OCT (iOCT).[1-6] Reports have suggested surgical maneuvers may significantly the microanatomy of the eye and that iOCT may provide the surgeon with information that is otherwise unavailable through the en face view of the microscope.[1-4]
As clinical utility is established, iOCT systems will need to be developed that provide the surgeon with rapid feedback and minimal disruption to surgical flow. Many reports have documented use of portable SD-OCT systems used in a handheld or microscope-mounted fashion.[2-6] Additionally, microscope integrated prototype iOCT systems have been described that allow for real-time visualization of instrument-tissue interactions.[5 7-9] To our knowledge, heads-up display systems and foot pedal surgeon control of the OCT scan system has not been described in human use.
In order to better understand the impact of a microscope integrated iOCT system with heads-up surgeon display of OCT feedback of the OCT scanner on ophthalmic surgery, we initiated the DISCOVER study. The purpose of this report is to describe the early results of DISCOVER and describe one novel integrative iOCT system included in the study: the RESCAN 700 (Carl Zeiss Meditec, Germany).
Methods
The DISCOVER study (Determination of feasibility of Intraoperative Spectral domain microscope Combined/integrated OCT Visualization during En face Retinal and ophthalmic surgery) is an IRB-approved multi-surgeon investigational device study. The study adhered to the tenets of the Declaration of Helsinki. Informed consent was obtained from all participants.
Intraoperative imaging for this portion of the DISCOVER study was performed using the RESCAN 700, a prototype microscope integrated iOCT system that includes a heads-up display system, external video display panel, and foot pedal control of the OCT scanner (Figure 1). The system is based on the Lumera 700 (Carl Zeiss Meditec) platform. Anterior segment imaging was achieved the standard microscope viewing system. For posterior segment imaging, the RESIGHT lens system or a contact lens was utilized for surgical and iOCT visualization. The RESCAN 700 includes Z-tracking and focus control for image stabilization and quality control. Each surgeon underwent a lab-based training session with model eyes to provide foundational experience with the heads-up display system and foot pedal controls prior to human imaging.
Figure 1.
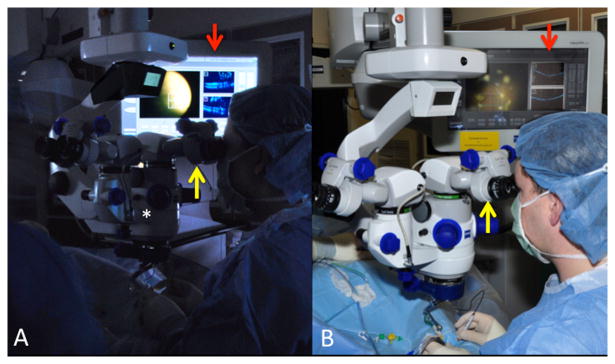
RESCAN 700. (A) Microscope integrated intraoperative OCT system, the RESCAN 700 (*) with simultaneous display monitor revealing OCT data stream (red arrow) and surgeon oculars with heads-up display (yellow arrow). (B) Similar image with full view of RESCAN 700 with the heads-up display in surgeon oculars (yellow arrow) and Callisto display monitor with OCT feedback (red arrow).
iOCT scanning was performed during key milestones with continuous visualization and motion. In addition, iOCT capture of volume and raster scans were also obtained. Surgeons could select the scan length, angle, and location through either foot-pedal control or input through the video monitor display system.
Results
iOCT images were successfully obtained in 10 of 10 cases. Both anterior segment and posterior segment imaging was obtained. Anterior segment images included iOCT evaluation of corneal incisions, scleral closure, phacoemulsification groove depth, and intraocular lens position (Figure 2, Supplemental Video 1). Posterior segment iOCT imaging included evaluation of hyaloid release with triamcinolone and completeness of peel in macular hole, epiretinal membrane, and vitreomacular traction cases (Figure 3). Contrast enhancement with triamcinolone and real-time capture of hyaloid release was achieved (Figure 3A, Supplemental Video 2). Following hyaloid elevation, formation of an occult full-thickness macular hole was identified with iOCT, resulting in a change in the surgical procedure (e.g., internal limiting membrane peeling, gas tamponade), Figure 4A. The real-time imaging and heads-up display system facilitated visualization of instrument-tissue interactions, including the diamond dusted membrane scraper and intraocular forceps (Figures 4B, 5; Supplemental Videos 3, 4). Metallic instruments resulted in significant shadowing of underlying tissues (Figure 5; Supplemental Video 4). No intraoperative adverse events occurred during in these initial cases of the DISCOVER study.
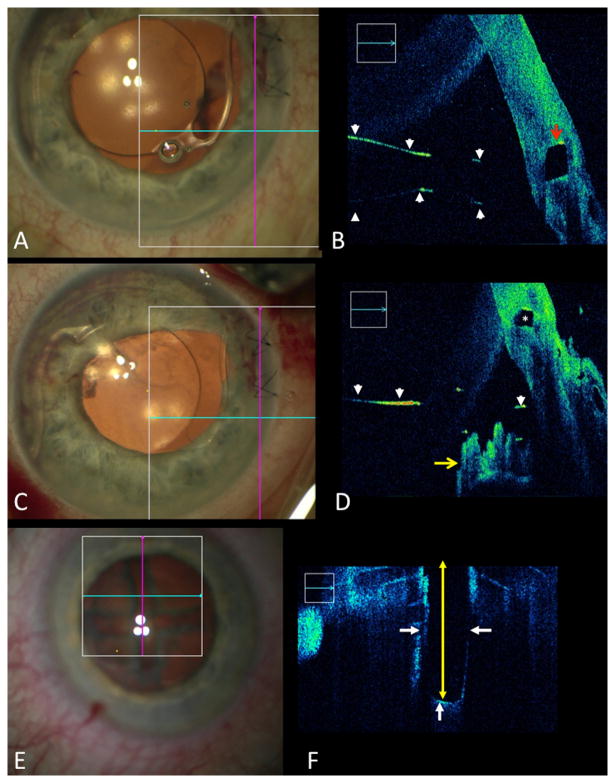
Figure 2.
Anterior segment intraoperative OCT (iOCT) with real-time feedback. (A) Surgical view of subluxed anterior chamber intraocular lens (ACIOL) with haptic trapped in corneal wound. (B) B-scan with iOCT feedback identifying elevated ACIOL (white arrowheads) and entrapment of haptic in corneal wound (red arrow). (C) Surgical view following ACIOL repositioning with B-scan crosshairs visible on display. (D) B-scan with iOCT feedback confirming optimal ACIOL position (white arrowheads) with haptic in the sulcus resting on the iris (yellow arrow). Residual corneal gap is present and identified (*). (E) Surgical view during phacoemulsification following groove formation. (F) B-scan of iOCT revealing grove depth (yellow arrow) and lens edge at groove (white arrows).
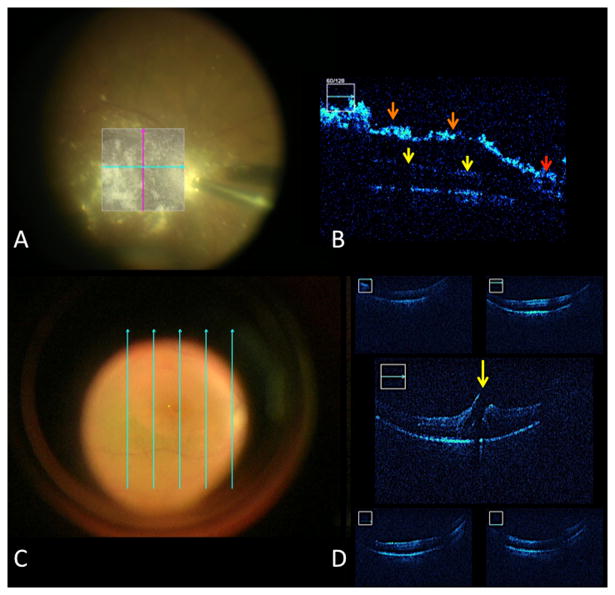
Figure 3.
Posterior segment intraoperative OCT (iOCT). (A) Surgical view following triamcinolone installation to visualize the hyaloid. (B) B-scan following OCT contrast enhancement with triamcinolone with excellent visualization of the posterior hyaloid (orange arrow) and attachment at the optic nerve (red arrow). Underlying retina is shadowed due to density of triamcinolone (yellow arrow). (C) Surgical view following internal limiting membrane (ILM) peeling with 5-line raster display. (D) Following ILM peeling, iOCT reveals persistence of the retinal flap and full-thickness macular hole (yellow arrow).
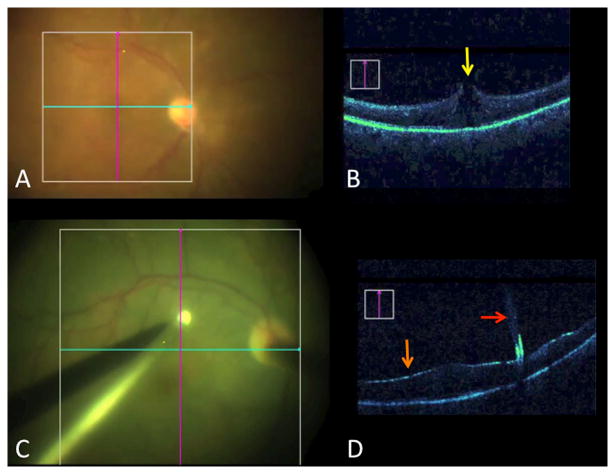
Figure 4.
Visualizing the impact of surgical maneuvers. (A) Surgical view with crosshairs of OCT scanner following elevation of the posterior hyaloid in a vitreomacular traction (VMT) case. (B) B-scan following hyaloid elevation in VMT case reveals occult full-thickness macular hole (yellow arrow), altering surgical planning (e.g., internal limiting membrane peeling, gas tamponade). (C) Surgical view of diamond dusted membrane scraper initiating membrane peel. (D) Real-time visualization with intraoperative OCT of instrument tissue-interaction (red arrow). Indocyanine green staining results in shadowing of underlying tissue and enhanced visualization of the internal limiting membrane (orange arrow).
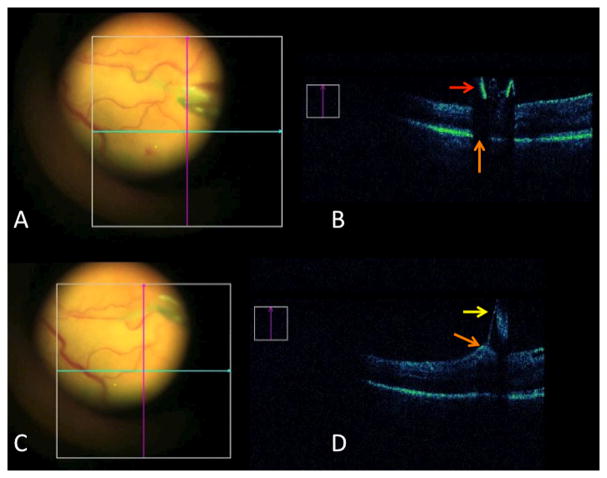
Figure 5.
Visualizing instrument-tissue interactions. (A) Surgical view with OCT crosshairs near forceps engaging the internal limiting membrane (ILM). (B) Intraoperative OCT (iOCT) of forceps (red arrow). Metallic material results in absolute shadowing of the underlying tissues (orange arrow). (C) Surgical view of forceps actively peeling the ILM. (D) iOCT revealing ILM (yellow arrow) with focal traction and the internal retinal surface (orange arrow).
Discussion
In this study, we demonstrate the feasibility of real-time iOCT for anterior and posterior segment surgery with a microscope integrated iOCT system with heads-up display surgeon feedback. Both real-time and static imaging was obtained to provide feedback to the surgeon with minimal disruption of surgical flow and outstanding visualization of tissues during surgery. Current metallic surgical instrumentation was noted to have significant shadowing of underlying tissues, limiting the visualization of instrument-tissue interaction.[7]
The integration of the OCT scanner into the surgical environment has been one of the major limiting factors for wider utilization of iOCT technology. Preliminary studies have described portable systems that were initially used in a handheld fashion.[2 3 10] Microscope mounting of portable SD-OCT systems have more recently described which provide foot-pedal control of X-Y-Z translation and increased stability for the scan axis.[2-4 11] Microscope integrated prototypes have also been developed that allow for simultaneous surgical maneuvers and OCT scanning.[5 7 8] To date and to our knowledge, all microscope integrated iOCT systems have been add-on systems that mounted within the optical path (e.g., before the objective lens) or accessed a side port for introducing the OCT beam, altering the overall ergonomics of the microscope profile.[5 7] Additionally, most of these systems utilized an OCT engine that resided outside of the housing of the surgical microscope, increasing the footprint of the overall system.[5 7] The RESCAN 700 integration of microscope and OCT technology is a unique melding of the technologies that does not alter the external physical presence of the microscope head and has minimal alterations to the overall footprint of the system in the operating room. The RESCAN 700 is one of two prototypes that have been reported that includes the heads-up display system, and the first to be described in human use. The second system with heads-up display capability is the Cole Eye Institute microscope integrated iOCT prototype.[9 12]
The progression of technology to include improved surgeon feedback, minimal disruption to surgical work-flow, and enhanced independent control will likely help facilitate the utilization of this technology. Further research is needed to continue to enhance our understanding of the role of iOCT in the surgical management of ophthalmic disease and to better delineate how iOCT can maximize surgical outcomes. We hope the final results of the DISCOVER study will help to improve our understanding of the role of microscope integrated iOCT in the management of ophthalmic surgery.
Supplementary Material
Real time visualization with intraoperative OCT of scleral wound closure revealing initial wound gape and subsequent complete apposition on the OCT.
Real-time visualization of hyaloid elevation off the macular surface utilizing intraoperative OCT. Triamcinolone has been instilled to provide increased visualization and OCT contrast enhancement.
Real-time visualization of the diamond dusted membrane scraper engaging the retinal surface to initiate the peel. Shadowing from the metallic shaft is noted on the horizontal cut. Minimal shadowing from the silicone tip is visualized on the vertical cut.
Real-time visualization of membrane peeling utilizing intraocular forceps. Underlying tissue shadowing is noted due to the metallic material of the instrument. Following membrane engagement, peeling is visualized with intraoperative OCT revealing focal traction at the inner retinal surface.
Acknowledgments
Funding: The following funding sources provided support for this activity:
NIH/NEI K23-EY022947-01A1 (JPE); Ohio Department of Development TECH-13-059 (JPE, SKS); Research to Prevent Blindness (PKK)
Footnotes
Competing Interests: The following competing interests may be relevant to this publication: JE-Bioptigen (P); PK-Carl Zeiss Meditec (C), Alcon (C); SS-Bausch and Lomb (C); Bioptigen (P).
References
- 1.Ehlers JP, Kernstine K, Farsiu S, Sarin N, Maldonado R, Toth CA. Analysis of pars plana vitrectomy for optic pit-related maculopathy with intraoperative optical coherence tomography: a possible connection with the vitreous cavity. Archives of ophthalmology. 2011;129(11):1483–6. doi: 10.1001/archophthalmol.2011.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ehlers JP, Ohr MP, Kaiser PK, Srivastava SK. Novel microarchitectural dynamics in rhegmatogenous retinal detachments identified with intraoperative optical coherence tomography. Retina. 2013;33(7):1428–34. doi: 10.1097/IAE.0b013e31828396b7. [DOI] [PubMed] [Google Scholar]
- 3.Ehlers JP, Tam T, Kaiser PK, Martin DF, Smith G, Srivastava SK. Utility of intraoperative optical coherence tomography during vitrectomy surgery for vitreomacular traction syndrome. Retina. 2014 doi: 10.1097/IAE.0000000000000123. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ehlers JP, Xu D, Kaiser PK, Singh RP, Srivastava SK. Intrasurgical Dynamics of Macular Hole Surgery: An Assessment of Surgery-Induced Ultrastructural Alterations with Intraoperative Optical Coherence Tomography. Retina. 2013 doi: 10.1097/IAE.0b013e318297daf3. [DOI] [PubMed] [Google Scholar]
- 5.Binder S, Falkner-Radler CI, Hauger C, Matz H, Glittenberg C. Feasibility of intrasurgical spectral-domain optical coherence tomography. Retina. 2011;31(7):1332–6. doi: 10.1097/IAE.0b013e3182019c18. [DOI] [PubMed] [Google Scholar]
- 6.Dayani PN, Maldonado R, Farsiu S, Toth CA. Intraoperative use of handheld spectral domain optical coherence tomography imaging in macular surgery. Retina. 2009;29(10):1457–68. doi: 10.1097/IAE.0b013e3181b266bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ehlers JP, Tao YK, Farsiu S, Maldonado R, Izatt JA, Toth CA. Integration of a spectral domain optical coherence tomography system into a surgical microscope for intraoperative imaging. Investigative ophthalmology & visual science. 2011;52(6):3153–9. doi: 10.1167/iovs.10-6720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ehlers JP, Tao YK, Farsiu S, Maldonado R, Izatt JA, Toth CA. Visualization of real-time intraoperative maneuvers with a microscope-mounted spectral domain optical coherence tomography system. Retina. 2013;33(1):232–6. doi: 10.1097/IAE.0b013e31826e86f5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ehlers JP, Tao YK, Srivastava SK. The value of intraoperative optical coherence tomography imaging in vitreoretinal surgery. Current opinion in ophthalmology. 2014 doi: 10.1097/ICU.0000000000000044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chavala SH, Farsiu S, Maldonado R, Wallace DK, Freedman SF, Toth CA. Insights into advanced retinopathy of prematurity using handheld spectral domain optical coherence tomography imaging. Ophthalmology. 2009;116(12):2448–56. doi: 10.1016/j.ophtha.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ray R, Baranano DE, Fortun JA, et al. Intraoperative Microscope-Mounted Spectral Domain Optical Coherence Tomography for Evaluation of Retinal Anatomy during Macular Surgery. Ophthalmology. 2011;118(11):2212–7. doi: 10.1016/j.ophtha.2011.04.012. [DOI] [PubMed] [Google Scholar]
- 12.Ehlers JP, Kaiser PK, Singh RP, Martin DF, Yuan A, Srivastava SK. Application of intraoperative OCT to ophthalmic surgery: PIONEER 18-month iOCT vitreoretinal results. American Society of Retina Specialists Annual Meeting; Toronto, Canada. 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Real time visualization with intraoperative OCT of scleral wound closure revealing initial wound gape and subsequent complete apposition on the OCT.
Real-time visualization of hyaloid elevation off the macular surface utilizing intraoperative OCT. Triamcinolone has been instilled to provide increased visualization and OCT contrast enhancement.
Real-time visualization of the diamond dusted membrane scraper engaging the retinal surface to initiate the peel. Shadowing from the metallic shaft is noted on the horizontal cut. Minimal shadowing from the silicone tip is visualized on the vertical cut.
Real-time visualization of membrane peeling utilizing intraocular forceps. Underlying tissue shadowing is noted due to the metallic material of the instrument. Following membrane engagement, peeling is visualized with intraoperative OCT revealing focal traction at the inner retinal surface.