Abstract
Purpose
A collaborative pharmacist-physician (PharmD-MD) team approach to medication therapy management (MTM), with pharmacists initiating and changing medications at separate office visits, holds promise for cost-effective management of blood pressure (BP), but has not been evaluated in many systematic trials. The primary objective of this study was to examine BP control for hypertensive patients managed by a newly formed PharmD-MD MTM team vs. versus usual care (UC) in a university primary care clinic.
Methods
This was a randomized, pragmatic, clinical trial of hypertensive patients randomly selected for the PharmD-MD MTM team or UC. In the PharmD-MD MTM group pharmacists managed drug therapy initiation, monitoring, medication adjustments, biometric assessments, laboratory tests, and patient education. In the UC group, patients continued to see their primary care provider (PCP). Participants were age 18 years or over, diagnosed with hypertension, most recent BP ≥140/90 mmHg or ≥130/80 mmHg if co-diagnosed with diabetes mellitus, on at least one anti-hypertensive medication, and English speaking. Primary outcome was the difference in mean change in systolic BP (SBP) at 6 months. Secondary outcomes included percent achieving therapeutic BP goal, mean change in diastolic BP, LDL and HDL cholesterol.
Findings
A total of 75 patients were in the PharmD-PCP MTM group and 91 in the UC group. Mean reduction in SBP was significantly greater in the PharmD-PCP MTM group at 6 months [−7.1 (SD=19.4) vs. +1.6 (SD=21.0) mm Hg, (p=0.008)] but the difference was no longer statistically significant at 9 months [−5.2 (SD=16.9) vs. −1.7 (SD=17.7) mmHg, (p=0.22)] based on intent to treat analysis. In the intervention group, a greater percentage of patients who continued to see the MTM pharmacist vs. those who returned to their PCP were at goal at 6 months (88.5% vs. 63.6%) and 9 months (78.9% vs. 47.4%). No significant difference in change of LDL or HDL was detected at 6 or 9 months between groups, however mean initial visit values were near recommended levels. The PharmD-PCP MTM group had significantly fewer mean number of PCP visits than the UC group [1.8 (SD=1.5) vs 4.2 (SD=1.0), p<0.001)
Implications
A PharmD-PCP collaborative MTM service was more effective in lowering blood pressure than UC at 6 months for all patients and at 9 months for patients who continued to see the pharmacist. Incorporating pharmacists in the primary care team can be a successful strategy for managing medication therapy, improving patient outcomes and possibly extending primary care capacity.
Keywords: Hypertension, Collaborative Care, Pharmaceutical Care, Pharmacist, Medication Therapy Management, MTM
Introduction
Achieving blood pressure (BP) control is challenging for busy primary care physicians (PCPs) and may become even more so since it is predicted there will be a shortage of 52,000 PCPs in the United States by 2015.1 Pharmacists are an underutilized resource for extending primary care capacity for medication management. In December 2011 the U.S. Surgeon General released a letter supporting greater involvement of the pharmacist on patient care teams; “… policy makers should further explore ways to optimize the role of pharmacists to deliver a variety of patient-centered care and disease prevention, in collaboration with physicians or as part of the health care team”.2 In September 2013 the American College of Physicians issued a position paper that specifically included clinical pharmacists in the definition of a clinical care team.3 Evidence of favorable outcomes associated with pharmacists on the care team was reported in a systematic review of 298 studies and meta-analyses conducted for hemoglobin A1c, LDL cholesterol, blood pressure (BP) and adverse events.4 The review included studies of pharmacists providing an array of medication therapy management (MTM) services, collaborative with physicians and stand-alone, in many settings (e.g. inpatient hospitals, community pharmacies, out-patient clinics, emergency departments) and for many different types of patients (e.g. diabetes, hypertension, asthma). A limitation of the literature was that only a small percentage (7%) of the 298 studies were randomized controlled trials (RCTs).
A literature review yielded ten RCTs using a collaborative pharmacist-physician team approach for patients with hypertension.5–14 Inclusion criteria varied targeting different patient groups; patients using specific high cost anti-hypertension medications6, high risk patients (i.e. high number of medications, doses per day, or medication changes, and/or poor adherence)7, and patients with uncontrolled hypertension (with varying systolic and diastolic BP criteria)5, 8–14. Time of intervention also varied from six (n=5)5,6,10–12, nine (n=1)9, and 12 (n=4)7,8,13,14 months. Despite these variances, all studies reported reduction in systolic blood pressure (SBP) and diastolic blood pressure (DBP) was greater in the team approach as compared to usual care (mean difference range from 5.5 to 12 points for SBP and 1.8 to 6.7 points for DBP). The difference in percentage of patients at BP goal ranged from 18% to 64% between groups. While the pharmacist was integrated into the patient care team in each study the role of the pharmacist differed with only three12–14 studies including pharmacists independently initiating and changing medication therapy (with various levels of physician oversight and participation), while most (n=7)5–11 included pharmacists only in an advisory role making recommendations to the physician for medication therapy changes. Only one study involved new implementation of a pharmacist into the organization, all others were conducted in environments with pre-existing pharmacist services.7
A collaborative pharmacist-physician team model in which pharmacists independently initiate and change medication therapy and see patients at separate office visits could result in time savings for PCPs as well as improved patient outcomes. However little is known about this model that would be a likely scenario for many organizations wishing to newly integrate pharmacists into the care team for the treatment of hypertension.
We conducted a randomized, pragmatic, trial examining the outcomes and processes of initiating and integrating a pharmacist-physician team model, with the pharmacist having ability to initiate and change medication therapy, for the management of uncontrolled hypertension within a university-based internal medicine medical group. Our primary objective was to examine the BP control for hypertensive patients collaboratively managed by a newly formed pharmacist-physician team versus those who were solely managed by their physicians over a nine-month period.
Patients and Methods
We randomly assigned patients with uncontrolled high blood pressure to either a pharmacist-physician collaborative MTM (PharmD-PCP MTM) or to usual care in a university general internal medicine clinic where each patient had a primary care physician (PCP). The Institutional Review Boards (IRBs) of University of California, San Diego and University of California, Los Angeles approved the study protocol.
Patients
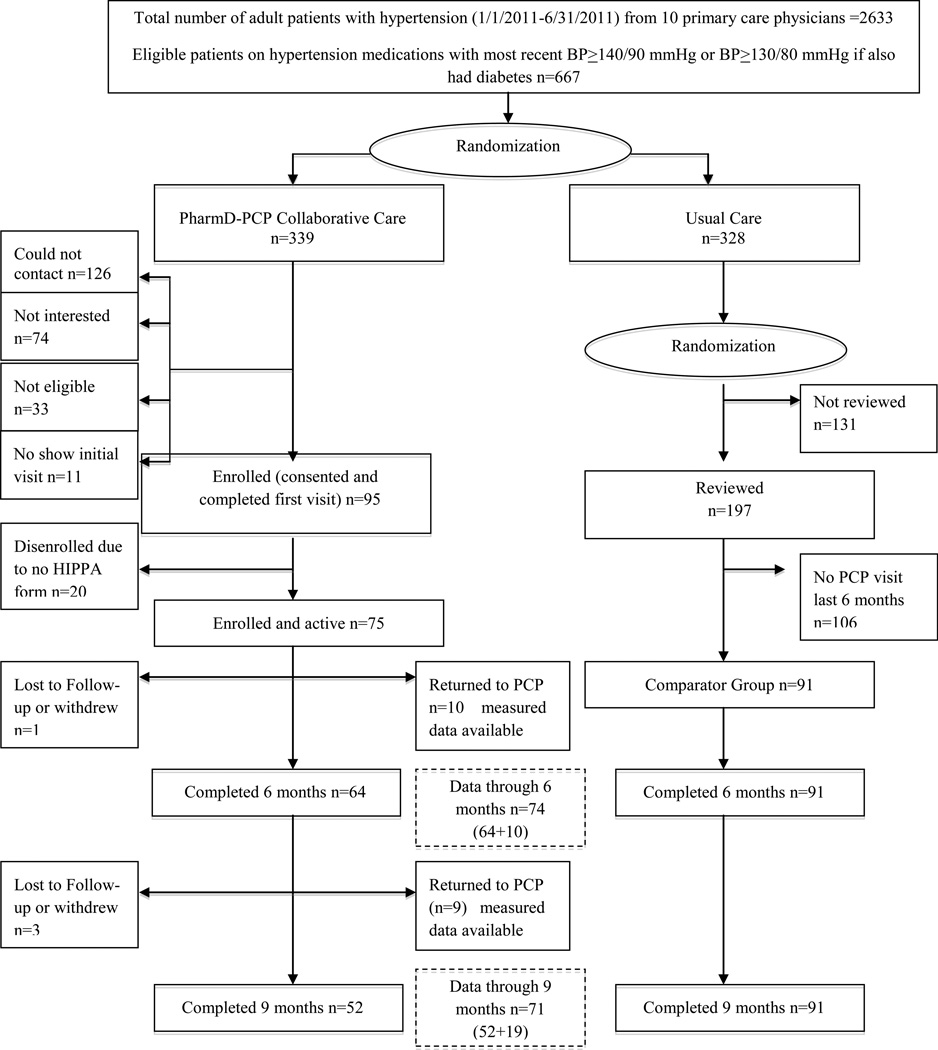
Patients with uncontrolled hypertension were identified through an electronic medical record (EMR) database. Inclusion criteria were: age 18 years or over, diagnosis of hypertension with most recent blood pressure ≥140/90 mmHg or blood pressure ≥130/80 mmHg if patients also had diabetes mellitus, treated with at least one anti-hypertensive medication, continuous active patient (at least one visit) of the clinic for at least the past 6 months (1/1/2010–6/31/2010), English speaking, and able to complete questionnaires in English. Patients were excluded if they did not meet provisions of the clinical collaborative agreement protocol in the judgment of the patient’s physician or the clinical pharmacist. Eligible patients were randomized, via computer-generated random sequence, to either the PharmD-PCP MTM or usual care group. (Figure 1) The study coordinator contacted patients in the PharmD-PCP MTM group, determined participation interest, and scheduled first clinical pharmacist visits where written informed consent was obtained. Usual care patients were not contacted but continued to see their PCP. A random subset of usual care patients was selected for retrospective chart review covering the same time interval as the active intervention. The additional inclusion criteria of “had a clinic visit in 6 month period before 6/2012.” was applied to ensure patients had continued to receive PCP care at least 9 months after their index visit.
Figure 1.
Patient selection, randomization and flow.
Intervention
Two clinical pharmacists and an internal medicine physician, who would serve as the medical director of the clinic, collaborated closely to develop a clinical collaborative practice protocol using national hypertension guidelines and updated hypertension management literature for the PharmD-PCP MTM group. The collaborative practice protocol was approved by the University of California San Diego Medical Center and by the IRBs as part of the study approval process. The protocol specified types of patients for whom clinical pharmacists would provide services (i.e. patients with blood pressure above target goals) and MTM activities that included initiating, adjusting or discontinuing antihypertensive medications, and approving appropriate antihypertensive drug refill requests. Therapeutic decisions and timing of patient labs and follow-up visits (except 9 month study close) were left to pharmacists’ clinical judgment, in consultation with a physician if needed. The two clinical pharmacists providing MTM services had a doctor of pharmacy degree, one year of pharmacy practice residency training, and more than seven years of experience in ambulatory care. Prior to study initiation they (ML and RS) reviewed the BP assessment method used at the clinic with the study medical director (YW) to ensure consistency of measurement between the PharmD-PCP MTM and usual care groups. BP assessment was conducted using the manual wall-mounted sphygmomanometer, with the patient seated in a chair for at least 5 minutes, with the measured arm elevated to heart level. Pharmacists measured BP at the beginning of each study visit as was customary for all clinic patients, whereas nursing staff measured blood pressure for usual care patients.
Patients were scheduled for four, 30-minute, PharmD visits (initial, three, six and nine months), independent of PCP visits, and as needed for follow-up by the pharmacists (additional clinic visit or via phone). The intervention was to be a limited time period of intensive medication management after which the patient would return to their PCP for hypertension treatment. At the initial PharmD visit the pharmacist assessed patient knowledge of their hypertension and current treatment, reviewed current treatment goals, self-monitoring behavior, medical and medication history, and current medications. Pharmacists also helped the patient set individual BP goal, reviewed and/or ordered laboratory tests, made adjustments to hypertension medication regimen (i.e. dosage adjustments, medication initiation or discontinuation). Each visit was documented in the EMR system and routed to the patient’s PCP. During subsequent visits pharmacists reviewed progress toward goals, laboratory values, medication adherence, self-monitoring behavior and continued to make changes to the hypertension medication regimen as needed. A physician was always present in the medical practice during the pharmacist clinic times, and was available for consultation, as needed. Patients received $22 for each pharmacist visit ($25 for the 9 month visit).
Outcome Measures
The primary outcome measure was change in systolic blood pressure (SBP) at six months after initial visit. Secondary outcomes included percent of patients at BP goal (<140/90 mmHg or <130/80 mmHg if patients also had diabetes mellitus), mean change in diastolic blood pressure (DBP), LDL and HDL cholesterol. In addition, for the PharmD-PCP MTM group outcomes included number and type of medication changes, number and type of drug therapy problems identified and patient satisfaction with the clinical pharmacist. Patient satisfaction was assessed using the 22-item Pharmacist Service Questionnaire (PSPrSQ).15 Questions were related to patient perception of the quality of pharmacist-provided care, interpersonal relationship, and overall satisfaction. Higher scores (0–100 scale) indicated greater satisfaction. All data, except patient reported satisfaction, were collected from the EMR. Existing data for the usual care group was collected via retrospective chart review after the completion of the PharmD-PCP MTM intervention period. Since the usual care group did not have scheduled visits, data closest to 6 and 9 months post index date were used, with a +/− 6 weeks window, as best estimate of blood pressure. Chart reviews were conducted by two clinical coordinators (one of whom was the study coordinator for this study) from the Clinical and Translational Research Institute at the University of California, San Diego.
Statistical Analysis
Difference in mean SBP change at 6 months between the PharmD-PCP MTM and usual care groups was evaluated using a t-test. A target sample size of 85 patients per group was estimated as sufficient to detect a mean difference-in-change in SBP of 5 mmHg (SD=10) with 90% power, assuming a two-sided test of significance, and alpha=0.05. Descriptive statistics were calculated on all variables. Proportions were used to describe categorical variables and the significance of group comparisons was estimated with chi-square tests. A sensitivity analysis was conducted because of an imbalance in age, gender, Charlson Comorbidity Index, and total number of medications to determine if findings were sensitive to these differences between groups. SAS version 9.2 (SAS Institute Inc., Cary, NC) was used to conduct all analyses.
Results
Figure 1 presents the flow of patients from randomization to study completion in each group. The first patient was enrolled July 2010 and the last patient completed the intervention in June 2012. A total of 64 (85.3%) of enrolled and active study patients (n=75) continued in the pharmacist program at 6 months and 52 (69.3%) at 9 months. EMR data were included in study analyses using the intent-to-treat approach for 19 patients who had returned to their PCP. A total of 91 patients in the usual care comparison group were included for initial, 6 and 9 month observations.
At the initial visit the PharmD-PCP MTM group (n=75) was similar to the usual care group (n=91) for all eight measured clinical variables; however PharmD-PCP MTM patients were slightly younger mean age 65.4 (SD=13.0) vs. 69.6 (SD=11.4) years, had lower Charlson Comorbidity Index scores 3.1 (SD=1.9) vs. 4.1 (SD=2.6), and were more likely to be men (53.3% vs. 31.9%). (Table 1) There was no difference in mean number of anti-HTN medications between the PharmD-PCP MTM [1.7 (SD=0.8)] and usual care [1.8 (SD=1.0)] groups (p=0.44). However, PharmD-PCP MTM patients had a lower total number of medications [8.8 (SD=4.2)] than usual care patients [11.3 (SD=5.2)] (p=0.001).
Table 1.
Patient Characteristics and Clinical Outcomes at Baseline
| PharmD-PCP MTM (n=75) |
Usual Care (n=91) |
p value | |
|---|---|---|---|
| Age - mean (SD)a | 65.4 (13.0) | 69.6 (11.4) | 0.03 |
| Male - n (%) | 40 (53%) | 29 (32%) | 0.005 |
| Systolic BP (mmHg) - mean (SD) | 134.8 (17.4) n=75 |
134.4 (16.5) n=89 |
0.89 |
| Diastolic BP (mmHg) - mean (SD) | 75.1 (12.5) n=75 |
75.7 (13.4) n=89 |
0.75 |
| At recommended BP goal – n (%)b | 40 (53.0) n=75 |
41 (45.1) n=89 |
0.35 |
| HDL (mg/DL) - mean (SD) | 59.7 (23.6) n=75 |
58.1 (22.3) n=90 |
0.65 |
| LDL (mg/DL) - mean (SD) | 99.5 (31.9) n=74 |
98.6 (31.0) n=90 |
0.85 |
| HbA1c (%) - mean (SD) | 6.6 (1.2) n=50 |
6.5 (1.5) n=68 |
0.85 |
| BMI (kg/m2) - mean (SD) | 30.2 (6.3) n=70 |
29.8 (5.7) n=82 |
0.71 |
| BUN (mg/dl) - mean (SD) | 19.7(12.5) n=75 |
18.5 (7.2) n=90 |
0.45 |
| Creatinine (mg/dl) - mean (SD) | 0.9 (0.2) n=75 |
0.9 (0.2) n=90 |
0.18 |
| Charlson Comorbidity Index (age adjusted) - mean (SD) | 5.3 (2.6) | 6.6 (3.2) | 0.004 |
| Number of Total Medications - mean (SD) | 8.8 (4.2) | 11.3 (5.2) | 0.001 |
| Number of Hypertension Medications - mean (SD) | 1.7 (0.8) | 1.8 (1.0) | 0.44 |
SD = standard deviation
140/90 mmHg or 130/80 mmHg if patient also had diabetes
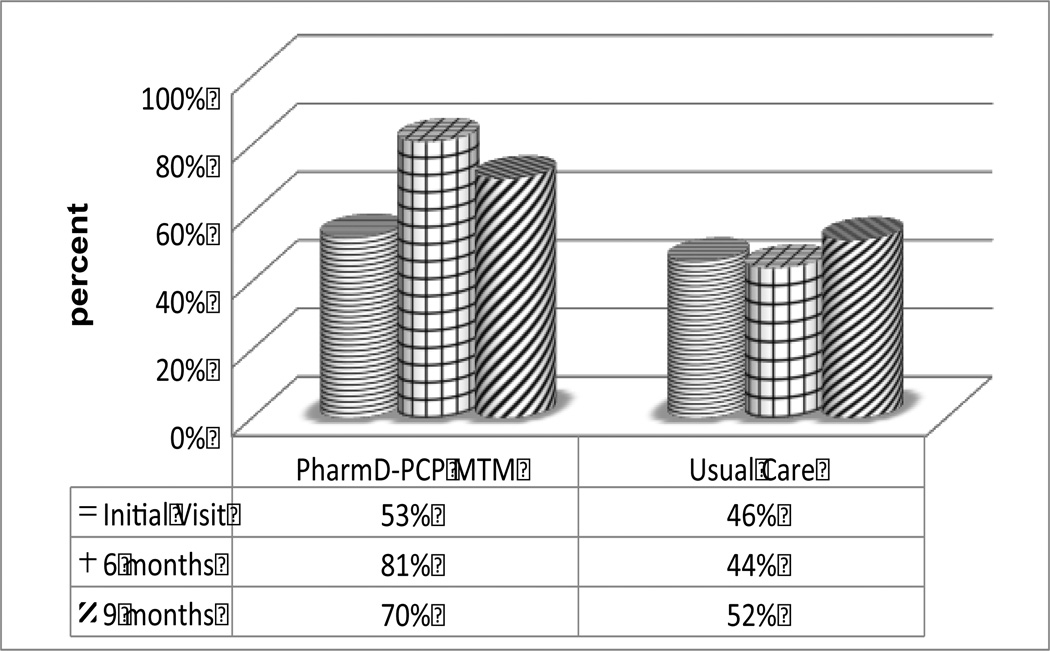
Mean improvement in SBP in the PharmD-PCP MTM group was significantly greater at 6 months than the usual care group, −7.1 (SD=19.4) vs. +1.6 (SD=21.0) mm Hg, (p=0.008) but the difference was no longer statistically significant at 9 months −5.2 (SD=16.9) vs. −1.7 (SD=17.7) mmHg, (p=0.22) based on intent treat analysis. (Table 2) No significant difference in change of LDL or HDL was detected at 6 or 9 months between groups, however mean values were near recommended goal level at initial visit in both groups (Table 1). The patterns of statistical significance in Table 2 did not change after adjusting for age, gender, Charlson Comorbidity Index, total number of medications, and number of PCP visits. When compared to usual care patients, a greater percentage of PharmD-PCP MTM patients were at blood pressure goal (SBP and DBP) at 6 months (81 % vs. 44%, p<0.001) and 9 months (70% vs. 52%, p=0.02). (Figure 2) The PharmD-PCP MTM group had significantly fewer PCP visits during the intervention period than the usual care group [mean = 1.8 (SD=1.5) vs mean=4.2 (SD=1.0) respectively, p<0.001) The mean number of total visits during the intervention period (PCP and PharmD combined) was not significantly greater than for the usual care group [mean=4.4 (SD=1.9) versus mean=4.2 (SD=1.0), (p=0.38)].
Table 2.
Tests of Differences-in-Change Between Groups in Clinical Outcomes Measures
| Mean (SD)a | Change Initial Visit vs. 6 months |
Change Initial Visit vs. 9 months |
||||
|---|---|---|---|---|---|---|
| PharmD- PCP MTM |
Usual Care | Significance p value |
PharmD- PCP MTM |
Usual Care | Significance p value |
|
| Systolic blood pressure | −7.1 (19.4) | 1.6 (21.0) | 0.008 | −5.2 (16.9) | −1.7 (17.7) | 0.22 |
| Diastolic blood pressure | −3.8 (10.5) | 1.7 (13.9) | 0.006 | −2.5 (10.2) | −0.3 (13.8) | 0.27 |
| LDL | 0.1 (19.9) | 4.6 (24.1) | 0.21 | −3.5 (26.3) | −3.1 (41.9) | 0.95 |
| HDL | 2.4 (28.3) | 0.3 (11.5) | 0.54 | −1.0 (20.4) | 0.4 (20.9) | 0.67 |
SD = standard deviation
Intent to treat analysis
PharmD-PCP MTM: n=74 (initial visit), 74 (6 months), 71 (9 months); note 1 patient missing BP at 6-month visit not included in this analysis
Usual Care: n=89 (index visit), 89 (6 months), 89 (9mos); note 2 patients missing BP data at index visit not included in this analysis
Figure 2.
Percentage of patients at blood pressure goala.
a In control = <140/90 or <130/80 if had diabetes
p values between groups: baseline=0.35, 6 mos=<0.001, 9 mos=0.02
PharmD-PCP MTM: n=75 (initial visit), 74 (6 months), 71 (9 months)
Usual Care: n=89 (index visit), 91 (6 months), 91 (9mos)
Within the PharmD-PCM MTM group, the mean change in SBP from initial visit to 9 months for patients who had returned to their PCP (n=19) was +1.9 (SD=13.8) compared to −7.8 (SD=17.3) for those (n=52) who continued to see the MTM pharmacist through the 9-month visit (p=0.03). Similarly the mean change in DBP was +2.8 (SD=9.9) for patients who had returned to their PCP and −4.5 (SD=9.7) for patients continuing to see the MTM pharmacist through 9 months (p=0.007). The percentage of patients who were at blood pressure goal (SBP and DBP) for the group of patients who returned to their PCP after 6 months was 63.6% at 6 months and 47.4% at 9 months, compared to 88.5% and 78.9% for patients continuing to see the MTM pharmacist. Differences in baseline characteristics for patients who returned to their PCP after 6 months vs. those who continued to see their MTM pharmacist through 9 months were non-significant for all variables. Mean patient satisfaction with the pharmacist was 92.4 (SD=10.9, n=49) at 6 months and 92.7 (SD=11.0, n=44) at 9 months. For those patients who were at their blood pressure target or better at the initial visit (or index visit for usual care group), a larger percentage remained in control in the PharmD-PCP MTM group vs. the usual care group at both 6 and 9 months (85% vs. 53.7%, p=0.002 and 81.6% vs. 63.4%, p=0.07 respectively).
At the initial visit the clinical pharmacist identified a hypertension-related drug therapy problem for almost half (45.2%) of the patients. (Table 3) The two most prevalent problems were the need for additional therapy (42.4%) and dosage increase (33.3%). Approximately one-third of patients had a medication change at their initial visit; the most common changes (increased dosage and adding a medication) aligned with the most frequent type of medication problems detected. The percentage of patients with drug therapy problems and subsequent medications changes were much lower at six months (20.0%, and 11.3% respectively). At nine months only two patients required a medication adjustment (increased dosage).
Table 3.
Pharmacist Actions for Anti-Hypertensive Medication Therapy Management
| Initial Visit (n=73) |
6 Month Visit (n=60) |
9 Month Visit (n=51) |
|
|---|---|---|---|
| Patients with a drug therapy problem identified n (%) | 33 (45.2%) | 12 (20.0%) | 4 (7.8%) |
| Type of drug therapy problem n (%) of total w/problems | |||
| Need for additional therapy | 14 (42.4%) | 7 (58.3%) | 1 (25.0%) |
| Drug dose too low | 11 (33.3%) | 3 (25.0%) | 1 (25.0%) |
| Non-adherence to therapy | 5 (15.2%) | 1 (8.3%) | 1 (25.0%) |
| Adverse drug reaction | 2 (6.1%) | 2 (16.7%) | 0 (0.0%) |
| Patients with a medication change at visit n (%) | 25 (34.3%) | 7 (11.7%) | 2 (3.9%) |
| Patients with type of change made n (%) of total w/change | |||
| Added Medication | 8 (32.0%) | 2 (28.6%) | 0 (0.0%) |
| Increased Dose | 15 (60.0%) | 3 (42.9%) | 2 (100.0%) |
| Decreased Dose | 2 (8.0%) | 1 (14.3%) | 0 (0.0%) |
| Changed Medication | 3 (12.0%) | 1 (14.3%) | 0 (0.0%) |
Note: Patients may have had multiple drug therapy problems or medication changes.
Discussion
In comparison to usual care, PharmD-PCP team approach produced significantly greater mean reduction in SBP and DBP and higher percentage of patients at blood pressure goals at 6 months. The subgroup of patients who continued to see the MTM pharmacist at 9 months continued to have significantly better BP control compared to the usual care group.” A drug therapy problem was identified for almost half of the patients; the two most common being need for additional therapy and/or a dosage increase. Approximately one-third of patients had a medication change at their initial MTM pharmacist visit. Patient satisfaction with the pharmacist was high. Also, patients who continued to see the MTM pharmacist had better outcomes than those who did not. Their mean change in SBP was almost 10 points better, and approximately 30% more of these patients were at BP goal at 9 months. In the subgroup of patients who were at BP goal at their initial visit (or index visit for usual care) the percentage remaining at goal at 9 months was almost 20% higher for those in the PharmD-PCP MTM group vs. the usual care.
Our results are consistent with a recent literature review that found 84% of published studies regarding pharmacists involved with HTN management showed favorable results.4 However, this finding was across studies with various study designs, few studies were RCTs, most provided MTM recommendations only, and very few were an integrated team model. Our finding of greater percentage of patients with controlled HTN in the PharmD-PCP MTM group was consistent with RCTs of this team model for HTN patients.5–14 For example, a study of 179 patients with uncontrolled hypertension (101 MTM vs. 78 control), with pharmacists making recommendations to the physician (96% accepted), 89.1% of the MTM group were at goal at 9 months vs. 52.9% in the control group.9 Similarly in a trial more closely aligned with ours where the pharmacist was able to initiate and change medications under a collaborative protocol, 62% of MTM patients vs. 44% of control patients were treated to goal at 12 months.13
In our study the clinical collaborative practice protocol allowed pharmacists to initiate, adjust or discontinue antihypertensive medications independently and pharmacists saw patients independently of an MD visit, as opposed to many studies where the pharmacist only makes recommendations for therapy changes and/or sees the patient as part of an MD visit. PharmD-PCP MTM patients had fewer PCP visits than usual care patients and there was no difference in total visits between groups. This finding suggests the intervention was cost-effective via two mechanisms; the substitution effect of the less costly pharmacist resource and achievement of better blood pressure control. The value of a PharmD saving PCP time by providing medication therapy management services in this type of collaborative care model to an increasing number of insured patients warrants further investigation in larger patient populations with a wide range of disease states. However, an essential component of this type of collaborative care model is for the PharmD and PCP to have access to the patient’s complete EMR regardless of the location or timing of the visit. Given a shared EMR, implementing the same type of collaborative protocol agreement in non-clinic settings (e.g. community pharmacies) could be pursued with appropriate communication channels, PCP availability, and adherence to patient privacy requirements.
Almost half of the PharmD-PCP MTM collaborative care patients had a drug therapy problem identified at their initial pharmacist visit with one third requiring a medication change This finding highlights the value of the MTM collaborative practice model that allows pharmacists to make medication changes, under protocol, as opposed to only making recommendations to the patient and/or physician. If pharmacists in this study were limited to making recommendations changes in medication therapy would have required contacting the PCP, PCP assessing a recommendation, and the PCP taking action to change the medication. Reduced physician time and expense may be achieved in well thought-out and planned collaborative practice protocols with pharmacists providing MTM services.
We attempted to make our study a real-world, pragmatic trial of integrating a new provider, clinical pharmacist, into a clinic to build a PharmD-PCP MTM team. Two key points regarding enrolling and retaining patients may inform future implementation efforts. First, to minimize clinic staff involvement and time commitment for this new service we chose to use a retrospective registry database from our EMR to identify intervention and control patients and enroll intervention patients. However, we learned that a more current BP measure may be needed since almost 50% of our patients (both groups) were at goal on their initial pharmacist visit (or index visit for usual care group). We elected to include these patients in our study since BP measures fluctuate, and this would occur in a real-world scenario, although none of the other randomized HTN MTM trials have done so. This proved to be an important decision since BP measures for many of these patients were above targeted goals at 6 and 9 months (PharmD-PCP MTM group; 15% and 18%, usual care group; 46% and 37%, respectively). Thus in future, selection of patients for an anti-hypertension intervention may be better based on multiple BP measures over time or BP measures in combination with other indicators such as medication regimen complexity, cost, or evidence of poor adherence. Second, retaining patients was somewhat problematic, for example 19% (n=12 of 64 with 6 month visit) did not return to the PharmD after their 6-month PharmD visit. Achieving BP goal did not account for all of these patients since more than a third of these patients were not at goal at their 6 month pharmacist visit. Although there are likely many reasons for drop out, having providers and staff more involved in reinforcing the pharmacist role and benefits, or improving convenience of pharmacist visits may improve patient engagement and retention.
This study has several limitations that should be considered. Study subjects were from a single university-based general internal medicine practice, therefore results are not generalizable to patients from different practice settings nor to all patients with hypertension. Since our study design was a randomized pragmatic trial, our results may not be representative of those achieved in usual practice. However, we allowed much of the trial conduct to be as naturalistic as possible. In addition, patients had to speak, read and write English, so our study population may have been more English literate than some sections of the population. Patients received a small payment for each clinic visit that may have influenced their behavior (e.g. medication adherence). Randomization at the patient level may have allowed for contamination of the usual care group since physicians had patients in both the PharmD-PCP MTM intervention group and the usual care groups. However, physicians did not know which patients would be randomly selected for the usual care group since the sample was drawn after the intervention was complete. In our trial patients were randomly selected to be offered participation in the PharmD-PCP MTM group but because there was a proportion who declined post-randomization it is likely that selection accounts for the few observed differences in patient characteristics between those who ultimately chose to participate and the usual care group for which there was no offer of participation. Since patients in the PharmD-PCP MTM group knew they were in a trial and usual care patients did not our results may have been effected by a Hawthorne effect or participation bias. BP measurement in the PharmD-PCP MTM group was performed by the two clinical pharmacists, while usual care group BP measurements were performed by licensed vocational nurses which could have affected group comparisons. Although, the pharmacists training prior to study start helped to ensure they were using the same method as for other clinic patients it is possible there was bias in the pharmacist’s assessment since they were aware of the study. This study examined pharmacists managing patients’ hypertension medications. Outcomes achieved as well as the number of drug therapy problems identified and medication changes made would likely differ if the pharmacists also managed medications for patients’ comorbid conditions.
Conclusion
A pharmacist-physician collaborative medication therapy management service was more effective in lowering blood pressure than usual care at 6 months and 9 months for patients who continued to see the pharmacist. Recognizing the pharmacist’s contribution to improving drug therapy management in collaboration with physicians, and given the shortages of PCPs and the aging population, incorporating pharmacists in the primary care team to provide MTM services can be a successful strategy for managing medication therapy and improving patient outcomes and possibly extending primary care capacity.
ACKNOWLEDGEMENTS
We greatly appreciate the work of our project coordinator, Archana Bhatt, and the leadership and staff at the University of California San Diego Medical Group (Dr. Larry Friedman) and the Internal Medicine Group - La Jolla (Dr. Neil Farber), without which this study would not have been possible. This study was conducted in support of the California Right Care Initiative (RCI); a public-private partnership, launched in 2008 and co-lead by the California Department of Managed Healthcare and the UC Schools of Public Health. The collaborative includes stakeholders across the healthcare system (medical groups, clinics, health plans, military health systems, consumer groups, government agencies, universities, business groups, and professional associations), dedicated to reducing morbidity and mortality among Californians due to heart disease, hypertension and diabetes by implementing evidence based promising interventions.
Support:
This research was funded by National Institutes of Health (NIH) – National Heart, Lung and Blood Institute (NHLBI, 1RC2HL101811-01) and by the National Institutes of Health (Grant UL RR031980 and UL1TR000100). The content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH. Dr. Mangione's effort was also supported in part by the UCLA Robert Wood Johnson Clinical Scholars Program and the U.S. Department of Veterans Affairs (Grant #67799). Dr. Mangione also receives support from the University of California, Los Angeles, Resource Centers for Minority Aging Research Center for Health Improvement of Minority Elderly (RCMAR/CHIME) under NIH/NIA Grant P30-AG021684, and from the NIH/NCATS UCLA CTSI Grant Number UL1TR000124.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICT OF INTEREST STATEMENT
None of the authors have any conflicts of interest to report. The study sponsors had no involvement in the study design, nor collection, analysis and interpretation of data, nor writing of the manuscript, nor decision to submit.
Prior presentation:
Portions of this article were presented at the Society for General Internal Medicine Annual Meeting, April 26th, 2013.
References
- 1.Petterson SM, Liaw WR, Phillips RL, et al. Projecting US primary care physician workforce needs: 2010–2025. Ann Fam Med. 2012;10:503–509. doi: 10.1370/afm.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benjamin R. Rockville, MD: U.S. Public Health Service, Department of Health and Human Services; 2011. Dec. [Accessed October 18, 2013]. (U.S. Public Health Service, Department of Health and Human Services, Rockville, MD). Letter to: Scott Giberson. Available at: http://www.accp.com/docs/positions/misc/Support_Letter_from_US_Surgeon_General.pdf. [Google Scholar]
- 3.Doherty RB, Crowley RA, for the Health and Public Policy Committee of the American College of Physicians Principles Supporting Dynamic Clinical Care Teams: An American College of Physicians Position Paper. Ann Intern Med. 2013;159 doi: 10.7326/0003-4819-159-9-201311050-00710. [DOI] [PubMed] [Google Scholar]
- 4.Chisolm-Burns MA, Kim Lee J, Spivey CA, et al. US pharmacists’ effect as team members on patient care: systematic review and meta-analyses. Medical Care. 2010;48(10):923–933. doi: 10.1097/MLR.0b013e3181e57962. [DOI] [PubMed] [Google Scholar]
- 5.Mehos BM, Saseen JJ, MacLaughlin EJ. Effect of pharmacist intervention and initiation of home blood pressure monitoring in patients with uncontrolled hypertension. Pharmacotherapy. 2000 Nov;20(11):1384–1389. doi: 10.1592/phco.20.17.1384.34891. [DOI] [PubMed] [Google Scholar]
- 6.Okamoto MP, Nakahiro RK. Pharmacoeconomic evaluation of a pharmacist-managed hypertension clinic. Pharmacotherapy. 2001 Nov;21(11):1337–1344. doi: 10.1592/phco.21.17.1337.34424. [DOI] [PubMed] [Google Scholar]
- 7.Taylor CT, Byrd DC, Krueger K. Improving primary care in rural Alabama with a pharmacy initiative. Am J Health Syst Pharm. 2003 Jun 1;60(11):1123–1129. doi: 10.1093/ajhp/60.11.1123. [DOI] [PubMed] [Google Scholar]
- 8.Green BB, Cook AJ, Ralston JD, et al. Effectiveness of Home Blood Pressure Monitoring, Web Communication, and Pharmacist Care on Hypertension Control. A Randomized Controlled Trial. JAMA. 2008;229(24):2857–2867. doi: 10.1001/jama.299.24.2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carter BL, Bergus GR, Dawson JD, et al. A cluster-randomized trial to evaluate physician/pharmacist collaboration to improve blood pressure control. J Clin Hypertens (Grennwich) 2008 Apr;10:260–271. doi: 10.1111/j.1751-7176.2008.07434.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carter BL, Ardery G, Dawson JD, et al. Physician and pharmacist collaboration to improve blood pressure control. Arch Intern Med. 2009 Nov 23;169(21):1996–2002. doi: 10.1001/archinternmed.2009.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Albsoul-Younes AM, Hammad EA, Yasein NA, et al. Pharmacist-physician collaboration improves blood pressure control. Saudi Med J. 2011 Mar;32(3):288–292. [PubMed] [Google Scholar]
- 12.Vivian EM. Improving blood pressure control in a pharmacist-managed hypertension clinic. Pharmacotherapy. 2002 Dec;22(12):1533–1540. doi: 10.1592/phco.22.17.1533.34127. [DOI] [PubMed] [Google Scholar]