Abstract
The early immune response to microbes is dominated by the recruitment of neutrophils whose primary function is to clear invading pathogens. However, there is emerging evidence that neutrophils play additional effector and regulatory roles. The present study demonstrates that human neutrophils assume antigen cross-presenting functions, and suggests a plausible scenario for the local generation of APC-like neutrophils through the mobilization of unconventional T-cells in response to microbial metabolites. Vγ9/Vδ2 T-cells and MAIT cells are abundant in blood, inflamed tissues and mucosal barriers. Here, both human cell types responded rapidly to neutrophils after phagocytosis of Gram-positive and Gram-negative bacteria producing the corresponding ligands, and in turn mediated the differentiation of neutrophils into APCs for both CD4+ and CD8+ T-cells through secretion of GM-CSF, IFN-γ and TNF-α. In patients with acute sepsis, circulating neutrophils displayed a similar APC-like phenotype and readily processed soluble proteins for cross-presentation of antigenic peptides to CD8+ T-cells, at a time when peripheral Vγ9/Vδ2 T-cells were highly activated. Our findings indicate that unconventional T-cells represent key controllers of neutrophil-driven innate and adaptive responses to a broad range of pathogens.
INTRODUCTION
Neutrophils are the first cells that are recruited to sites of microbial infection. While classically being viewed as terminally differentiated cells, there is emerging evidence that neutrophils represent key components of the effector and regulatory arms of the innate and adaptive immune system (1-3). As such, neutrophils regulate the recruitment and function of various cell types, and interact with immune and non-immune cells. Intriguingly, neutrophils directly affect antigen-specific responses by facilitating monocyte differentiation and DC maturation, and by interacting with T-cells and B-cells (4-10). Murine neutrophils have been shown to present antigens to both CD4+ and CD8+ T-cells (11-13), and to differentiate into “neutrophil-DC hybrids” in vitro and in vivo (14, 15). In humans, neutrophils with a phenotype consistent with a possible APC function, including expression of MHC class II, have been found in diverse inflammatory and infectious conditions (16-22). This notwithstanding, direct antigen presentation by neutrophils has thus far not been demonstrated in patients, especially with respect to an induction of antigen-specific CD8+ T-cell responses upon cross-presentation of exogenous proteins.
The physiological context underlying the differentiation of neutrophils into APCs and the implications for antigen-specific immune responses remain unclear. Unconventional T-cells such as human γδ T-cells, NKT cells and mucosal-associated invariant T (MAIT) cells represent unique sentinel cells with a distinctive responsiveness to low molecular weight compounds akin to pathogen and danger-associated molecular patterns (23-25). Such unconventional T-cells represent a substantial proportion of all T-cells in blood and mucosal epithelia, accumulate in inflamed tissues, and constitute an efficient immune surveillance network in inflammatory and infectious diseases as well as in tumorigenesis. Besides orchestrating local responses by engaging with other components of the inflammatory infiltrate (26-29), unconventional T-cells are also ideally positioned in lymphoid tissues to interact with freshly recruited monocytes and neutrophils (30-32). We previously showed that human γδ T-cells enhance the short-term survival of neutrophils but did not characterize these surviving neutrophils on a phenotypical and functional level (28). We here studied the outcome of such a crosstalk of human neutrophils with both γδ T-cells and MAIT cells in vitro and translated our findings to patients with severe sepsis. We demonstrate that neutrophils with APC-like features can be found in blood during acute infection, and that the phenotype and ex vivo function of circulating sepsis neutrophils was replicated in vitro upon priming of neutrophils by human γδ T cells and MAIT cells. Our findings thus provide a possible physiological context and propose a cellular mechanism for the local generation of neutrophils with APC functions, including their potential to cross-present soluble antigens to CD8+ T-cells, in response to a broad range of microbial pathogens.
MATERIALS AND METHODS
Subjects
This study was approved by the South East Wales Local Ethics Committee under reference numbers 08/WSE04/17 and 10/WSE04/21 and conducted according to the principles expressed in the Declaration of Helsinki and under local ethical guidelines. Sampling of adult patients with sterile systemic inflammatory response syndrome (SIRS) or with acute sepsis (defined as patients with SIRS in conjunction with a proven or suspected infection) was carried out within the UK Clinical Research Network under study portfolio UKCRN ID #11231 “Cellular and biochemical investigations in sepsis”. All study participants provided written informed consent for the collection of samples and their subsequent analysis. A waiver of consent system was used where patients were unable to provide prospective informed consent due to the nature of their critical illness or therapeutic sedation at the time of recruitment. In all cases, retrospective informed consent was sought as soon as the patient recovered and regained capacity. In cases where a patient died before regaining capacity, the initial consultee’s approval would stand.
Sepsis patients had a proven infection as confirmed by positive culture of at least one relevant sample according to the local microbiology laboratory overseen by Public Health Wales, and developed at least 3 of the 4 following SIRS criteria over the previous 36h: (i) temperature from any site >38°C or core <36°C; (ii) heart rate of >90 beats/min (unless individual had a medical condition or was receiving treatment preventing tachycardia); (iii) respiratory rate of >20 breaths/min, arterial PaCO2 <32 mmHg or mechanical ventilation for an acute process; and (iv) total WBC >12,000 cells/mm3 or <4,000 cells/mm3 or differential WBC count showing >10% immature (band) forms (n=37; age range 35-82 years, median 63 years; 51% female). Patients with sterile SIRS developed at least 3 of the 4 SIRS criteria but had no suspected or proven microbial infection (n=14; age range 26-70 years, median 48 years; 21% female). All patients with sepsis or SIRS had at least one documented organ failure on recruitment to the study and were either mechanically ventilated, on inotropic support or received acute renal replacement therapy. Healthy donors served as controls for the patient cohorts (n=10; age range 31-68 years, median 59 years; 20% female). Individuals were excluded from the study if pregnant or breastfeeding; suffering from documented severe immune deficiency or severe liver failure; admitted post-cardiac arrest; treated with high dose steroids or immunosuppressant drugs for the last six months; or unlikely to survive for the duration of the study period regardless of treatment.
Media, reagent and antibodies
Culture medium was RPMI-1640 medium supplemented with 2 mM L-glutamine, 1% sodium pyruvate, 50 μg/ml penicillin/streptomycin and 10% fetal calf serum (Invitrogen). Synthetic (E)-4-hydroxy-3-methyl-but-2-enyl pyrophosphate (HMB-PP) was provided by Dr Hassan Jomaa, Justus-Liebig University Giessen, Germany; synthetic 6,7-dimethyl-8-d-ribityllumazine (DMRL) was provided by Dr Boris Illarionov, Hamburg School of Food Science, Germany. Staphylococcus aureus toxic shock syndrome toxin-1 (TSST-1) was purchased from Toxin Technology; Mycobacterium tuberculosis purified protein derivate (PPD) was purchased from Statens Serum Institut, Copenhagen, Denmark. Salmonella abortus equi LPS, brefeldin A and BSA-FITC were purchased from Sigma. Recombinant IFN-γ, TNF-α and GM-CSF were purchased from Miltenyi. Human T-Activator CD3/CD28 Dynabeads, CFSE and 10 kDa dextran-FITC were purchased from Life Technologies.
The following mAbs were used for surface labeling: anti-CD3 (UCHT1, SK7, HIT3a), anti-CD4 (SK3, RPA-T4), anti-CD8 (SK1, HIT8a, RPA-T8), anti-CD11c (S-HCL-3), anti-CD14 (M5E2, MOP9), anti-CD15 (HI98), anti-CD16 (3G8), anti-CD25 (M-A251), anti-CD27 (M-T271), anti-CD31 (WM-59), anti-CD32 (FLI8.26), anti-CD45RO (UCHL1), anti-CD49d (9F10), anti-CD50 (TU41), anti-CD54 (HA58), anti-CD56 (B159), anti-CD62L (DREG-56), anti-CD64 (10.1), anti-CD69 (FN50), anti-CD70 (Ki24), anti-CD71 (M-A712), anti-CD72 (J4-112), anti-CD83 (HB15e), anti-CD86 (2331), anti-CD209 (DCN46), anti-HLA-DR (L243), anti-TCR-Vδ2 (B6.1), anti-CCR4 (1G1), anti-CCR5 (2D7), anti-CCR7 (3D12) and anti-CXCR3 (1C6) from BD Biosciences; anti-TCR-Vβ2 (MPB2D5), anti-TCR-Vγ9 (Immu360) and anti-CD40 (mAB89) from Beckman Coulter; anti-CD11a (HI111), anti-CD66b (G10F5), anti-CD154 (24-31), anti-CD161 (HP-3G10), anti-HLA-ABC (w6/32) and anti-TCR-Vα7.2 (3C10) from Biolegend; anti-CD11b (ICRF44), anti-CD14 (61D3), anti-CD19 (SJ25C1), anti-CD25 (BC96), anti-CD45RA (HI100) and anti-CD80 (2D10.4) from eBioscience; anti-HLA-A2 (BB7.2) from Serotec; and anti-CCR9 (248601) and anti-CCR10 (314305) from R&D Systems; together with appropriate isotype controls. Intracellular cytokines were detected using anti-IFN-γ (B27, BD Biosciences; 4S.B3, eBioscience) and anti-TNF-α (6401.1111, BD Biosciences; 188, Beckman Coulter). Blocking reagents used included anti-Vα7.2 (3C10; Biolegend); anti-TCR-Vγ9 (Immu360; Beckman Coulter); anti-TLR4 (HTA125; eBioscience); anti-CD277 (103.2; Dr Daniel Olive, Université de la Méditerranée, Marseille, France); anti-MR1 (26.5; Dr Ted Hansen, Washington University School of Medicine, St. Louis, Missouri, USA); anti-IFN-γ (25718) and anti-GM-CSF (3209) (Biolegend); and sTNFR p75-IgG1 fusion protein (etanercept/Enbrel; Amgen).
Cells
Total leukocytes from healthy donors and patients were isolated from heparinized blood by mixing with HetaSep (StemCell Technologies) followed by sedimentation of red blood cells (supplemental Fig. 1A). Neutrophils were purified from whole blood or Lymphoprep (Axis-Shield) separated granulocytes by HetaSep sedimentation followed by negative selection using the EasySep neutrophil enrichment kit (StemCell Technologies) (33), resulting in purities of >99.2% CD14− CD66b+ CD15+ and <0.1% contaminating monocytes (supplemental Fig. 1B). Total CD3+ T-cells (>98%) were isolated from PBMC using the pan T-cell isolation kit II (Miltenyi); CD4+ and CD8+ T-cells (>98%) were obtained using the corresponding EasySep kits (StemCell Technologies). Vγ9+ T-cells (>98%) were purified using anti-Vγ9-PE-Cy5 (Immu360; Beckman-Coulter) and anti-PE microbeads (Miltenyi); Vα7.2+ T-cells (>98%) were purified using anti-Vα7.2-PE (3C10; Biolegend) and anti-PE microbeads. Alternatively, Vγ9+ CD3+ γδ T-cells or Vα7.2+ CD161+ CD3+ MAIT cells were sorted to purities >99% using a FACSAria II (BD Biosciences).
Bacteria
Clinical isolates of Enterobacter cloacae, Enterococcus faecalis, Klebsiella pneumoniae and Staphylococcus aureus (28) were grown in liquid LB broth and on solid Columbia blood agar (Oxoid). The distribution of the non-mevalonate and riboflavin pathways across microbial species was determined based on the absence or presence of the enzymes HMB-PP synthase (EC 1.17.7.1) and DMRL synthase (EC 2.5.1.78) in the corresponding genomes, according to the Kyoto Encyclopedia of Genes and Genomes (KEGG; http://www.genome.jp/kegg).
T-cell culture
PBMC were stimulated with 0.1-100 nM HMB-PP or 0.1-100 μM DMRL. Vγ9+ T-cells or Vα7.2+ T-cells were co-cultured with autologous monocytes at a ratio of 1:1, in the presence of 25% (v/v) cell-free supernatants from neutrophils that had phagocytosed live bacteria as described previously (28). For blocking experiments, anti-TCR-Vα7.2, anti-TCR-Vγ9, anti-CD277, and anti-MR1 were used at 1-20 μg/ml.
Neutrophil culture
Freshly isolated neutrophils were cultured for up to 48 hours in the absence or presence of autologous Vγ9/Vδ2 T-cells or MAIT cells at a ratio of 10:1, and 10 nM HMB-PP or anti-CD3/CD28 dynabeads (1 bead per T cell). Alternatively, neutrophils were cultured with 25-50 % (v/v) conditioned medium obtained from purified Vγ9/Vδ2 T-cells or MAIT cells stimulated for 24 hours with anti-CD3/CD28 dynabeads (1 bead per cell) or 100 nM HMB-PP. Other stimuli included 100 ng/ml LPS and 100 U/ml recombinant IFN-γ, TNF-α and/or GM-CSF. sTNFR p75-IgG1 fusion protein, anti-IFN-γ and anti-GM-CSF were used at 10 μg/ml. Neutrophil survival and activation were assessed by flow cytometry, after gating on CD15+ cells and exclusion of Vγ9+ or Vα7.2+ cells where appropriate. For morphological analyses, neutrophils were centrifuged onto cytospin slides, stained with May-Grünwald-Giemsa solution and analyzed by light microscopy.
Functional assays
Endocytosis and APC functions were assessed as before (34-38). Freshly purified neutrophils and neutrophils cultured for 24 hours in the presence or absence of unconventional T-cell conditioned medium were incubated with 500 μg/ml 10 kDa dextran-FITC or BSA-FITC for up to 60 minutes at 4°C or 37°C. Endocytic uptake was measured immediately by flow cytometry; the specific uptake of each reagent was calculated by subtracting the background MFI at 4°C from the MFI obtained at 37°C.
For MHC class II restricted presentation of antigens, activated neutrophils were generated by 48 hour culture with a combination of IFN-γ, GM-CSF and/or TNF-α, or with unconventional T-cell conditioned medium. Neutrophils were pulsed with 10 ng/ml TSST-1 for 1 hour. After extensive washing, neutrophils were mixed with autologous CD4+ T cells at a ratio of 1:1; 1 hour later 10 μg/ml brefeldin A was added and cultures were incubated for a further 4 hours. Activation of TSST-1 responsive Vβ2+ CD4+ T cells was assessed by intracellular cytokine staining and analysis by flow cytometry (35). To assess CD4+ and CD8+ T cell responses to complex antigen preparations, neutrophils were pulsed with 1-10 μg/ml PPD for the last 18 hours of the 48 hour culture phase. After extensive washing neutrophils were mixed with CFSE-labeled autologous CD3+ T cells at a ratio of 1:1 and incubated for 7 days. CFSE dilution in the CD4+ and CD8+ T cell populations was assessed by flow cytometry, after exclusion of CD66b+ cells.
For MHC class I restricted antigen presentation, antigen-specific HLA-A2-restricted CD8+ T cell lines were generated using the immunodominant peptide of influenza matrix protein, M1(p58-66) (GILGFVFTL), as described before (37, 38). M1(p58-66)-specific responder CD8+ T cells used in APC assays were >95% pure, as confirmed by tetramer staining (data not shown). Activated neutrophils from HLA-A2+ donors were generated as above, using unconventional T-cell conditioned medium or recombinant cytokines, and pulsed for 1 hour with 0.1 μM peptide. For cross-presentation assays, 0.01-1 μM recombinant influenza M1 protein were added during the last 18 hours of the 48 hour neutrophil culture period. Fresh neutrophils from HLA-A2+ sepsis patients were incubated with 0.01-1 μM recombinant influenza M1 protein for 18 hours or cultured in medium for 17 hours prior to addition of 0.1 μM M1(p58-66) peptide for a further 1 hour. In each case, following extensive washing, neutrophils were incubated with HLA-A2+ peptide-specific CD8+ T cells at a ratio of 1:1; after 1 hour 10 μg/ml brefeldin was added and cultures were incubated for a further 4 hours. Activation of CD8+ T cells was assessed by intracellular cytokine staining and analysed by flow cytometry, after exclusion of CD66b+ cells.
Flow cytometry
Cells were acquired on an eight-color FACSCanto II (BD Biosciences) and analyzed with FlowJo (TreeStar). Single cells of interest were gated based on their appearance in side and forward scatter area/height, exclusion of live/dead staining (fixable Aqua; Invitrogen) and surface staining. Apoptotic cells were identified using annexin-V (BD Biosciences).
ELISA
Cell culture supernatants were analyzed on a Dynex MRX II reader, using ELISA kits for IL-17A (R&D Systems) as well as IFN-γ and TNF-α (eBioscience). Cell-free plasma samples and unconventional T-cell conditioned media were analyzed on a SECTOR Imager 6000 using the ultra-sensitive human pro-inflammatory 9-plex kit (Meso Scale Discovery).
Statistics
Data were analyzed using two-tailed Student’s t-tests for normally distributed data and Mann-Whitney tests for non-parametric data (GraphPad Prism). Differences between groups were analyzed using one-way ANOVA with Bonferroni’s post tests or with Kruskal-Wallis and Dunn’s post tests; two-way ANOVA was used when comparing groups with independent variables.
RESULTS
Unconventional human T-cells respond to neutrophil-released microbial metabolites
Vγ9/Vδ2+ γδ T-cells recognize the isoprenoid precursor HMB-PP, which is produced via the non-mevalonate pathway by a broad range of Gram-negative and Gram-positive bacteria (27, 39). Vα7.2+ CD161+ MAIT cells show a very similar responsiveness to an overlapping but distinct spectrum of microorganisms by sensing intermediates of the microbial vitamin B2 biosynthesis (Table 1) (40-43). We therefore sought to investigate the anti-microbial responses of these two types of unconventional T cells side by side. Here, Vγ9/Vδ2 T-cells but not MAIT cells responded to HMB-PP, as judged by induction of CD69 expression (Fig. 1A). In contrast, the riboflavin precursor DMRL induced a dose-dependent activation of MAIT cells but not Vγ9/Vδ2 T-cells. Blocking experiments confirmed a requirement for butyrophilin 3A (BTN3A/CD277) for Vγ9/Vδ2 T-cells and the MHC-related protein MR1 for MAIT cells (Fig. 1B), in support of current models of antigen recognition (41-45).
TABLE 1. Distribution across clinically relevant microbial pathogens of key biosynthetic pathways that produce metabolites targeted by human unconventional T cells.
|
Non-mevalonate pathway (Vγ9/Vδ2 T cell activation) |
Vitamin B2 synthesis (MAIT cell activation) |
|
|---|---|---|
| Gram-negative bacteria | ||
| Acinetobacter baumannii | + | + |
| Chryseobacterium gleum | − | + |
| Enterobacter cloacae | + | + |
| Escherichia coli | + | + |
| Haemophilus influenzae | + | + |
| Helicobacter pylori | + | + |
| Klebsiella pneumoniae | + | + |
| Legionella pneumophila | − | + |
| Neisseria meningitidis | + | + |
| Pseudomonas aeruginosa | + | + |
| Shigella dysenteriae | + | + |
|
| ||
| Gram-positive bacteria | ||
| Bacillus anthracis | + | + |
| Clostridium difficile | + | + |
| Corynebacterium diphtheriae | + | + |
| Enterococcus faecalis | − | − |
| Listeria monocytogenes | + | − |
| Mycobacterium tuberculosis | + | + |
| Propionibacterium acnes | + | + |
| Staphylococcus aureus | − | + |
| Streptococcus pyogenes | − | − |
|
| ||
| Other bacteria | ||
| Borrelia burgdorferi | − | − |
| Leptospira interrogans | + | + |
| Mycoplasma genitalium | − | − |
| Mycoplasma penetrans | + | − |
| Treponema pallidum | − | − |
|
| ||
| Yeasts, fungi | ||
| Aspergillus fumigatus | − | + |
| Candida albicans | − | + |
| Crytococcus neoformans | − | + |
| Saccharomyces cerevisiae | − | + |
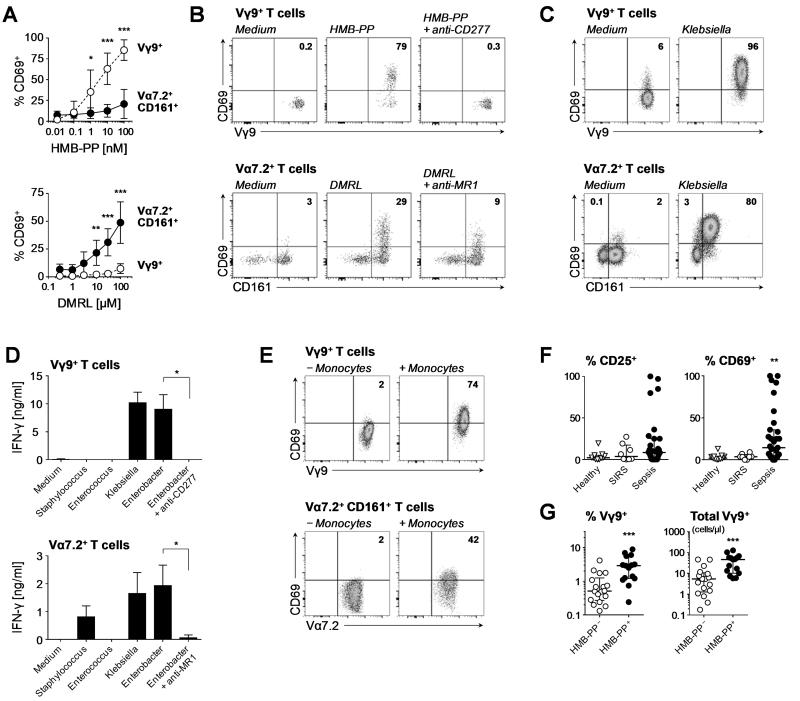
FIGURE 1. Unconventional human T-cell responses to microbial metabolites in vitro and in vivo.
(A) CD69 surface expression by Vγ9+ T-cells and Vα7.2+ CD161+ T-cells in PBMC stimulated overnight with HMB-PP or DMRL (means ± SD, n=5). Data were analyzed by two-way ANOVA with Bonferroni’s post-hoc tests. (B) Representative FACS plots of two donors showing CD69 expression by Vγ9+ T-cells and Vα7.2+ T-cells in PBMC stimulated overnight with 100 nM HMB-PP or 100 μM DMRL, in the absence or presence of anti-CD277 or anti-MR1 mAb. (C) CD69 expression by MACS-purified Vγ9+ T-cells or Vα7.2+ T-cells co-cultured overnight with autologous monocytes in the presence of supernatants from neutrophils after phagocytosis of Klebsiella pneumoniae (representative of three donors). (D) IFN-γ secretion by MACS-purified Vγ9+ T-cells or Vα7.2+ T-cells co-cultured overnight with autologous monocytes in the presence of supernatants from neutrophils after phagocytosis of different bacteria: HMB-PP− DMRL+, Staphylococcus aureus; HMB-PP− DMRL−, Enterococcus faecalis; and HMB-PP+ DMRL+, Enterobacter cloacae and Klebsiella pneumoniae (means ± SD, n=3-4 donors). Differences between mAb-treated and untreated cultures were analyzed using Mann-Whitney tests. (E) CD69 expression by FACS-sorted Vγ9+ T-cells or Vα7.2+ CD161+ T-cells co-cultured overnight with or without autologous monocytes in the presence of supernatants from neutrophils after phagocytosis of Enterobacter cloacae (representative of two donors). (F) Surface expression by CD25 and CD69 on circulating Vγ9+ T-cells in healthy controls and in patients with SIRS or sepsis. Each data point represents an individual, lines and error bars depict medians and interquartile ranges. Data were analyzed using Kruskal-Wallis tests and Dunn’s multiple comparison tests; comparisons were made with sepsis patients. (G) Proportion of Vγ9+ T-cells among all circulating T-cells and absolute counts of circulating Vγ9+ T-cells (in cells/μl blood) in sepsis patients with microbiologically confirmed infections caused by HMB-PP producing (E. coli, Enterobacter aerogenes, Haemophilus influenzae, Klebsiella pneumoniae, Pseudomonas aeruginosa, Stenotrophomonas maltophilia, anaerobic Gram-negative bacilli, diphtheroid bacteria) or HMB-PP deficient organisms (Aspergillus fumigatus, Candida spp., Staphylococcus spp., Streptococcus pneumoniae). Data were analyzed using Mann-Whitney tests. Differences were considered significant as indicated in the figures: *, p<0.05; **, p<0.01; ***, p<0.001.
We previously identified a crucial role for neutrophils in facilitating access to HMB-PP by Vγ9/Vδ2 T-cells (28). As control, purified Vγ9+ T-cells readily responded to neutrophils after phagocytosis of clinically relevant bacteria, in accordance with the distribution of the non-mevalonate pathways across the different pathogens (Table 1). Strikingly, purified Vα7.2+ T-cells showed very similar responses depending on the utilization of the riboflavin biosynthesis pathway by the phagocytosed species. Activated Vγ9+ T-cells and Vα7.2+ T-cells upregulated CD69 (Fig. 1C) and secreted IFN-γ (Fig. 1D) but not IL-17A (data not shown). The response of Vα7.2+ T-cells to microbial compounds was confined to the CD161+ bona fide MAIT cell population (Fig. 1C-D). Both Vγ9/Vδ2 T-cells and MAIT cells failed to respond to neutrophil-released microbial compounds in the presence of anti-CD277 and anti-MR1, respectively (Fig. 1D), and in the absence of autologous monocytes (Fig. 1E), highlighting a requirement for presentation by accessory cells. These findings reveal a remarkable similarity in the responsiveness of Vγ9/Vδ2 T-cells and MAIT cells to microbial metabolites.
Patients with acute sepsis caused by HMB-PP producing pathogens display elevated levels of activated γδ T-cells
In order to resolve the existence of APC-like neutrophils in human infectious disease and determine a possible link with anti-microbial unconventional T-cell responses, we recruited adult patients with newly diagnosed severe sepsis and characterized their circulating leukocytes phenotypically and functionally. As proof of principle for the involvement of unconventional T-cells in early inflammatory responses, patients with acute sepsis revealed a substantial activation of Vγ9/Vδ2 T-cells as judged by CD69 expression but not SIRS patients who served as non-infected controls (Fig. 1F; supplemental Fig. 1A). Of note, we found a significant increase in the absolute counts and the proportion of Vγ9/Vδ2 T-cells among all circulating T-cells between patients with microbiologically confirmed infections caused by HMB-PP producing as opposed to HMB-PP deficient species (Fig. 1F). These clinical findings evoke earlier studies in patients with acute peritonitis (28), and further support the notion of a differential responsiveness of unconventional T-cells to defined pathogen groups which can be detected both locally at the site of infection (46) and systemically in blood (Fig. 1F).
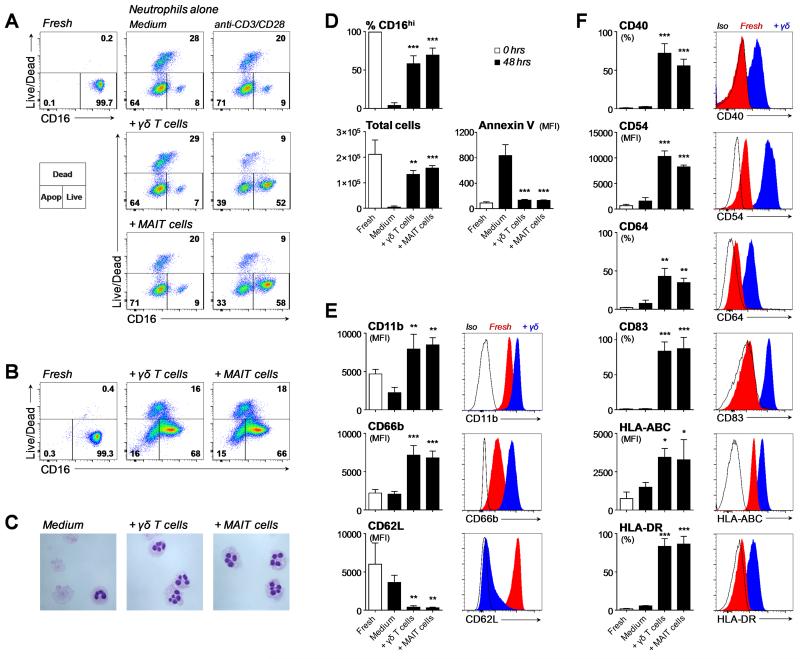
Unconventional human T-cells induce prolonged neutrophil survival and activation
We recently showed that Vγ9/Vδ2 T-cells trigger short-term (<20 hours) survival of autologous neutrophils (28). Here, highly purified neutrophils co-cultured for extended periods with activated Vγ9/Vδ2 T-cells or MAIT cells displayed a prolonged survival as judged by exclusion of amine reactive dyes and retention of surface CD16 (FcγRIII) for at least 48 hours (Fig. 2A). A similar effect was observed when incubating purified neutrophils with Vγ9/Vδ2 T-cell or MAIT cell conditioned culture supernatants, indicating a significant contribution of soluble factors in mediating the observed effects (Fig. 2B). In contrast to the highly active metabolite HMB-PP as specific activator of Vγ9/Vδ2 T-cells, the MAIT cell activator used in the present study, DMRL, only possesses a relatively modest bioactivity. The true MAIT cell activator is far more potent than DMRL and active at subnanomolar concentrations but not commercially available and difficult to synthesize chemically (41, 43). Most stimulation experiments with purified MAIT cells were therefore conducted with anti-CD3/CD28 coated beads. Importantly, use of either anti-CD3/CD28 beads or HMB-PP to activate Vγ9/Vδ2 T-cells elicited identical neutrophil responses (Fig. 2A-C and data not shown). Surviving neutrophils possessed a highly activated morphology as judged by the presence of hypersegmented nuclei (Fig. 2C). The anti-apoptotic effect of unconventional T-cells was confirmed by the preservation of the total number of neutrophils present after 48 hours of culture and the lack of annexin-V binding (Fig. 2D). As confirmation of their activated status, surviving neutrophils showed pronounced upregulation of CD11b and CD66b expression and complete loss of CD62L (Fig. 2E).
FIGURE 2. Survival, activation and expression of APC markers by unconventional T-cell primed neutrophils.
(A) Neutrophil survival judged by retention of CD16 expression and exclusion of live/dead staining after 48 hour co-culture with FACS-sorted Vγ9/Vδ2 T-cells or MAIT cells, in the absence or presence of anti-CD3/CD28 beads. FACS plots are representative of three donors and depict total neutrophils after gating on CD15+ Vγ9− or CD15+ Vα7.2− cells. (B) Neutrophil survival after 48 hour culture in the presence of HMB-PP activated Vγ9/Vδ2 T-cell or anti-CD3/CD28 activated MAIT cell conditioned medium (representative of three donors). (C) Morphological analysis of surviving neutrophils after 48 hour culture in the absence or presence of HMB-PP activated Vγ9/Vδ2 T-cell or anti-CD3/CD28 activated MAIT cell conditioned medium (representative of two donors). Images were acquired with ×400 original magnification. (D) Neutrophil survival after 48 hour culture in the absence or presence of HMB-PP activated Vγ9/Vδ2 T-cell or anti-CD3/CD28 activated MAIT cell conditioned medium. Shown are means ± SD for the proportion of CD16hi cells (n=9-10), the total number of neutrophils (n=3) and annexin V staining on CD16hi neutrophils (n=3). Expression of (E) activation markers and (F) APC markers on freshly isolated neutrophils and CD16hi neutrophils after 48 hour culture in the absence or presence of HMB-PP activated Vγ9/Vδ2 T-cell or anti-CD3/CD28 activated MAIT cell conditioned medium. Data shown are means ± SD and representative histograms from 3 individual donors. Data were analyzed by one-way ANOVA with Bonferroni’s post-hoc tests; comparisons were made with medium controls. Differences were considered significant as indicated in the figures: *, p<0.05; **, p<0.01; ***, p<0.001.
Unconventional T-cell primed neutrophils have a unique APC-like phenotype
Circulating neutrophils in healthy people do not express CD40, CD64 (FcγRI), CD83 or HLA-DR, yet all these surface markers were found on unconventional T-cell primed neutrophils (Fig. 2F). Moreover, these neutrophils also showed a marked upregulation of CD54 (ICAM-1) and HLA-ABC (Fig. 2F), suggestive of a possible function of unconventional T-cell primed neutrophils as APCs for both CD4+ and CD8+ T-cells.
The chemokine receptors CCR7, CCR9 and CCR10 remained undetectable under those culture conditions (data not shown), arguing against trafficking of APC-like neutrophils to non-inflamed lymph nodes, the intestine or the skin. In contrast, APC-like neutrophils displayed enhanced expression levels of CXCR3 and CCR4 (data not shown), indicative of an increased responsiveness to inflammatory chemokines and supporting a local role during acute inflammation.
Neutrophils stimulated with defined microbial compounds on their own, in the absence of Vγ9/Vδ2 T-cells or MAIT cells, failed to acquire a similar phenotype. Most notably, neutrophils cultured for 48 hours in the presence of LPS did not show increased levels of HLA-ABC, HLA-DR, CD40, CD64 or CD83 compared to neutrophils cultured in medium alone (data not shown), emphasizing the crucial and non-redundant contribution of unconventional T-cells and their specific ligands to the acquisition of APC characteristics by neutrophils.
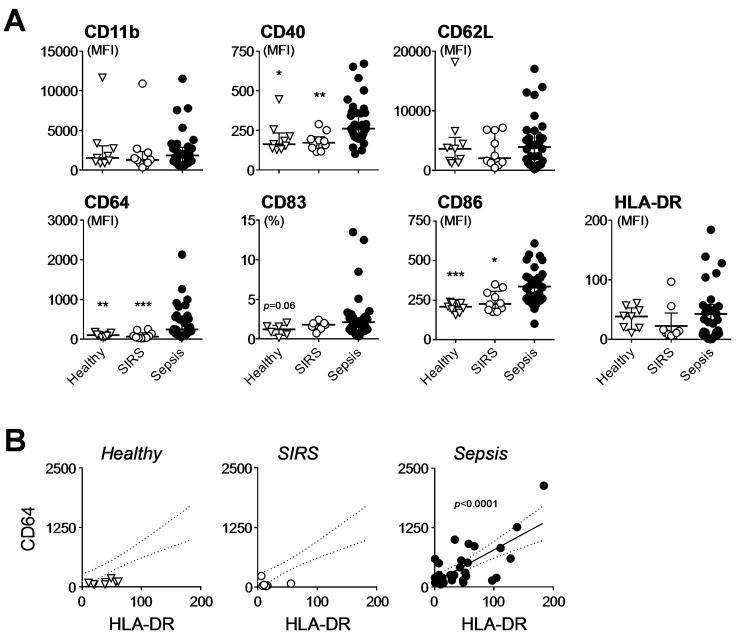
Circulating neutrophils in sepsis patients display an APC-like phenotype
In order to resolve the existence of APC-like neutrophils in human infectious disease, we characterized circulating leukocytes in sepsis patients as a means to access neutrophils that had recently been activated in different infected tissues. Sepsis neutrophils displayed a strikingly altered phenotype compared to neutrophils from healthy individuals and SIRS patients and were characterized by markedly higher expression of CD40, CD64 and CD86 (Fig. 3A). We also found increased surface levels of CD83 and HLA-DR on circulating neutrophils in some patients with sepsis, although this was not significant across the cohort as a whole. Of note, there was a correlation between the expression of CD64 and HLA-DR on sepsis neutrophils, supporting a link between neutrophil activation and APC phenotype (Fig. 3B). These findings indicate the presence of APC-like neutrophils in sepsis patients, despite the generally presumed immune suppression in those individuals as judged by reduced HLA-DR expression levels on monocytes (data not shown) (47).
FIGURE 3. APC-like phenotype of circulating neutrophils during acute sepsis.
(A) Surface expression of the indicated markers on circulating neutrophils in patients with SIRS (n=14) or sepsis (n=37) and in healthy controls (n=10). Each data point represents an individual, lines and error bars depict medians and interquartile ranges. Data were analyzed using Kruskal-Wallis tests and Dunn’s multiple comparison tests; comparisons were made with sepsis patients. (B) Correlation between surface expression of CD64 and HLA-DR on circulating neutrophils in healthy controls and in patients with SIRS or sepsis. Lines depict linear regression and 95% confidence bands as calculated for sepsis neutrophils. Differences were considered significant as indicated in the figures: *, p<0.05; **, p<0.01; ***, p<0.001.
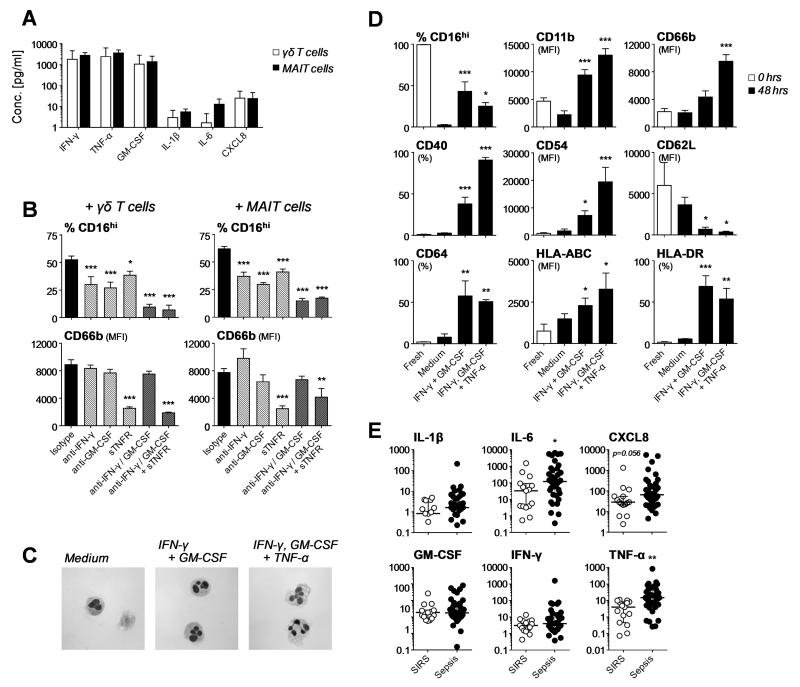
Neutrophil survival and APC marker expression is mediated via unconventional T-cell secreted cytokines
To identify the unconventional T-cell derived factor(s) exerting the observed effects on neutrophils, we quantified pro-inflammatory mediators in the culture supernatants. These experiments revealed a dominant production (>1,000 pg/ml on average) of GM-CSF, IFN-γ and TNF-α by activated Vγ9/Vδ2 T-cells and MAIT cells but only very low levels (<25 pg/ml) of IL-1β, IL-6 and CXCL8, indicating that both unconventional T-cell populations share a similar cytokine profile (Fig. 4A). Experiments using blocking reagents identified an involvement of GM-CSF, IFN-γ and TNF-α in promoting neutrophil survival by both Vγ9/Vδ2 T-cells and MAIT cells (Fig. 4B). While neutralization of each individual cytokine on its own had a partial effect, combined blocking of GM-CSF and IFN-γ was most effective in inhibiting neutrophil survival, with blocking of TNF-α having little additive effect. In contrast, CD66b upregulation was mainly triggered by TNF-α (Fig. 4B). Of note, the effect of unconventional T-cells on neutrophils could be mimicked in part by using recombinant GMCSF, IFN-γ and TNF-α. In this respect, only neutrophils cultured with a combination of all three cytokines exhibited a morphology characterized by hypersegmented nuclei (Fig. 4C). TNF-α was particularly important for the induction of CD40, CD54, CD66b and MHC class I expression (Fig. 4D). Taken together, these experiments identify microbe-responsive unconventional T-cells as rapid physiological source of GM-CSF, IFN-γ and TNF-α and imply that the unique combination of cytokines secreted by unconventional T-cells is key for the observed impact on neutrophils.
FIGURE 4. Effect of unconventional T-cell derived cytokines on neutrophil survival and APC marker expression.
(A) Secretion of the indicated mediators into the culture supernatant by FACS-sorted Vγ9+ T-cells or Vα7.2+ CD161+ T-cells stimulated overnight in the presence of HMB-PP or anti-CD3/CD28 beads, respectively, as detected using multiplex ELISA (means + SD, n=2-3). (B) Neutrophil survival (as proportion of CD16hi cells) and CD66b expression on CD16hi neutrophils after 48 hour culture in the presence of HMB-PP activated Vγ9/Vδ2 T-cell or anti-CD3/CD28 MAIT cell conditioned medium and neutralizing agents against GMCSF, IFN-γ and/or TNF-α (means + SD, n=3). Data were analyzed by one-way ANOVA with Bonferroni’s post-hoc tests; comparisons were made with isotypes. (C) Morphological analysis of surviving neutrophils after 48 hour culture in the absence or presence of GM-CSF, IFN-γ and/or TNF-α (representative of two donors). Images were acquired with ×400 original magnification. (D) Neutrophil survival and expression of the indicated markers on CD16hi neutrophils after 48 hour culture in the absence or presence of recombinant GM-CSF, IFN-γ and/or TNF-α (means + SD, n=3). Data were analyzed by one-way ANOVA with Bonferroni’s post hoc tests; comparisons were made with medium controls. (E) Plasma levels of IL-1β, IL-6, CXCL8, GM-CSF, IFN-γ and TNF-α in SIRS and sepsis patients (in pg/ml). Each data point represents an individual, lines and error bars depict medians and interquartile ranges. Differences between the two groups were analyzed using Mann-Whitney tests. Differences were considered significant as indicated in the figures: *, p<0.05; **, p<0.01; ***, p<0.001.
The particular requirement for TNF-α in the acquisition of the full APC phenotype is especially noteworthy when considering the cytokine/chemokine profiles in acutely infected patients. Plasma proteins that were highly elevated in sepsis patients included TNF-α as well as IL-6 and CXCL8 (Fig. 4E). Of note, there was a trend toward higher levels of TNF-α in patients with HMB-PP positive infections (p=0.09; data not shown). A proportion of individuals with sepsis also had increased plasma levels of GM-CSF, IFN-γ and IL-1β, although this was not significant across the whole cohort (Fig. 4E). These findings confirm that the blood of sepsis patients contains pro-inflammatory mediators implicated in driving survival and activation of neutrophils, including their differentiation into APCs.
Unconventional T-cell primed neutrophils readily take up soluble antigens
We next tested the capacity of APC-like neutrophils to take up soluble antigens. While freshly isolated neutrophils were not very efficient at endocytosing FITC-labeled BSA and dextran (10,000 Da) as model compounds, short-term exposure to Vγ9/Vδ2 T-cell conditioned medium led to a greatly enhanced uptake (Fig. 5A). With unconventional T-cell primed neutrophils kept in culture for 24 hours before addition of BSA-FITC, antigen endocytosis was confined to the CD16hi APC-like population whereas no such uptake was seen in the apoptotic CD16lo population (Fig. 5B). In contrast, neutrophils cultured in medium alone showed no specific uptake of BSA in the CD16hi population. These data indicate that unconventional T-cells promote the uptake of exogenous antigens as a prerequisite for antigen processing and presentation by neutrophils.
FIGURE 5. Efficient endocytosis of exogenous molecules and presentation of microbial antigens by unconventional T-cell primed neutrophils.
(A) Endocytosis of FITC-labeled BSA and 10 kDa dextran by freshly isolated neutrophils incubated for 60 minutes at 4°C or at 37°C in the absence or presence of HMB-PP activated γδ T-cell supernatant. FACS plots are representative of 2-3 donors; specific uptake of FITC-labeled BSA and dextran by freshly isolated neutrophils was determined over 30 and 60 minutes (means + SD, n=2-3). (B) Endocytosis of FITC-labeled BSA over 60 minutes by neutrophils that had been cultured overnight in the absence or presence of HMB-PP activated γδ T-cell supernatant. FACS plots are representative of three healthy donors; specific uptake of FITC-labeled BSA by γδ T-cell primed neutrophils was determined over 30 and 60 minutes (means + SD, n=2-3). Data were analyzed by two-way ANOVA with Bonferroni’s post-hoc tests; comparisons were made with (A) medium controls or (B) CD16lo cells. (C) IFN-γ production by superantigen-specific CD4+ Vβ2+ T-cells in response to autologous neutrophils cultured for 48 hours in medium or the absence or presence of HMB-PP activated Vγ9/Vδ2 T-cell conditioned medium or a combination of IFN-γ, GM-CSF and TNF-α prior to pulsing with 10 ng/ml TSST-1 (representative of two donors). (D) Proliferation of CD4+ and CD8+ T-cells in response to freshly isolated neutrophils and neutrophils cultured for 48 hours in the presence of HMB-PP activated Vγ9/Vδ2 T-cell or anti-CD3/CD28 activated MAIT cell conditioned medium. Neutrophils were pulsed with 10 μg/ml PPD for 18 hours prior to addition of CFSE-labeled bulk CD3+ T-cells; CFSE dilution of responder T-cells was assessed after 7 days of co-culture (representative of three donors). (E) Proliferation of CFSE-labeled CD4+ and CD8+ T-cells in response to PPD-pulsed freshly isolated neutrophils and neutrophils cultured for 48 hours in the presence of HMB-PP activated Vγ9/Vδ2 T-cell conditioned medium with and without sTNFR. CFSE dilution of responder T-cells was assessed after 7 days of co-culture (means + SD, n=3). Data were analyzed by one-way ANOVA with Bonferroni’s post-hoc tests; comparisons were made with Vγ9/Vδ2 T-cell + sTNFR treated neutrophils. Differences were considered significant as indicated in the figures: *, p<0.05; **, p<0.01; ***, p<0.001.
Unconventional T-cell primed neutrophils are efficient APCs for CD4+ and CD8+ T-cells
The functionality of cell surface expressed HLA-DR on activated neutrophils was confirmed using the Staphylococcus aureus superantigen, toxic shock syndrome toxin-1 (TSST-1), which crosslinks MHC class II molecules with the TCR of CD4+ T-cells expressing a Vβ2 chain (35). Neutrophils exposed to Vγ9/Vδ2 T-cell conditioned medium or to a combination of GM-CSF, IFN-γ and TNF-α were both capable of presenting TSST-1 to autologous Vβ2+ CD4+ T-cells (Fig. 5C). When using the complex Mycobacterium tuberculosis antigen, purified protein derivate (PPD), which requires intracellular processing, unconventional T-cell primed neutrophils displayed a striking capacity to trigger proliferation of both CD4+ and CD8+ T-cells (Fig. 5D). Sequestration of TNF-α during the neutrophil priming period by addition of sTNFR diminished both CD4+ and CD8+ T-cell responses (Fig. 5E) as further confirmation of the key role for unconventional T-cell derived TNF-α in the acquisition of APC features by neutrophils.
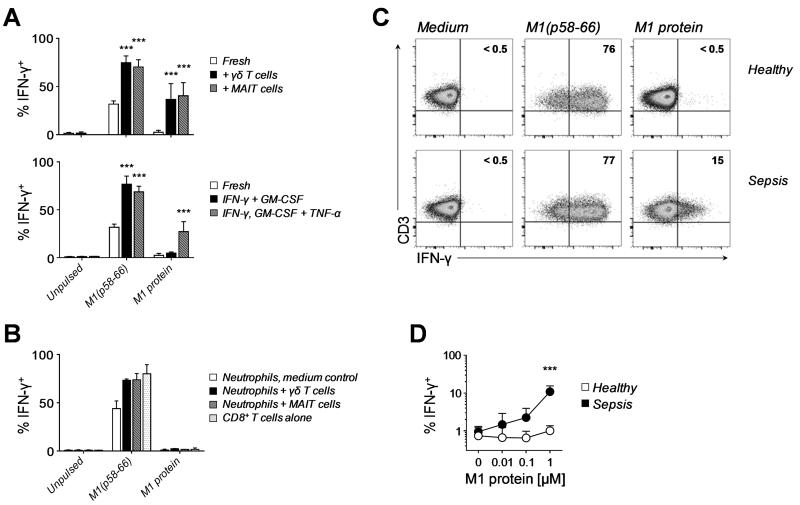
Unconventional T-cell primed neutrophils cross-present antigens to CD8+ T-cells
Following up from the striking induction of PPD-specific CD4+ and CD8+ T-cell responses we assessed the potential of APC-like neutrophils to trigger CD8+ T-cell responses, by taking advantage of HLA-A2 restricted responder T-cell lines specific for M1(p58-66), the immunodominant epitope of the influenza M1 protein (36-38). Using the M1(p58-66) peptide, which can be readily pulsed onto cell surface-associated MHC class I molecules for direct presentation to CD8+ T-cells, unconventional T-cell primed neutrophils showed a significantly improved antigen presentation, compared with freshly isolated neutrophils (Fig. 6A) and in agreement with the elevated levels of MHC class I molecules on APC-like neutrophils. Importantly, only unconventional T-cell primed neutrophils but not freshly isolated neutrophils were also able to induce robust responses by M1(p58-66)-specific responder CD8+ T-cells when utilizing the full-length M1 protein (Fig. 6A), a 251 amino acid long antigen that requires uptake, processing and loading of M1(p58-66) onto intracellular MHC class I molecules for cross-presentation to CD8+ T-cells (36-38). Control experiments supported the need for antigen uptake and processing as recombinant M1 protein could not be pulsed directly onto neutrophils, demonstrating the absence of potential degradation products in the M1 protein preparation that might be able to bind directly to cell surface-associated MHC class I molecules on neutrophils or CD8+ T-cells (Fig. 6B). Neutrophils cultured for 48 hours in the presence of GM-CSF and IFN-γ were also capable of enhanced presentation of M1(p58-66) peptide to M1-specific CD8+ T-cells. However, only neutrophils generated by incubation with a combination of GM-CSF, IFN-γ and TNF-α readily processed the full-length M1 protein (Fig. 6A), demonstrating that TNF-α plays a pivotal role in the acquisition of a fully competent APC phenotype and function by neutrophils.
FIGURE 6. Cross-presentation of exogenous antigens by unconventional T-cell primed neutrophils and sepsis neutrophils.
(A) IFN-γ production by antigen-specific CD8+ T-cells in response to neutrophils cultured for 48 hours in the presence of HMB-PP activated Vγ9/Vδ2 T-cell or anti-CD3/CD28 activated MAIT cell conditioned medium (top), or neutrophils cultured for 48 hours with the recombinant cytokines indicated (bottom). Neutrophils were pulsed for 1 hour with 0.1 μM influenza M1(p58-66) peptide or for 18 hours with recombinant M1 protein (means + SD, n=3). Data were analyzed by two-way ANOVA with Bonferroni’s post-hoc tests; comparisons were made with freshly isolated neutrophils. (B) Failure of M1 protein to be pulsed directly onto neutrophils as judged by IFN-γ production of antigen-specific CD8+ T-cells alone or in response to neutrophils cultured for 48 hours in the absence or presence of HMB-PP activated Vγ9/Vδ2 T-cell or anti-CD3/CD28 activated MAIT cell conditioned medium. Neutrophils were pulsed for 1 hour with either 0.1 μM influenza M1(p58-66) peptide or 1 μM recombinant M1 protein; CD8+ T-cells were incubated directly with the peptide or M1 protein (means + SD, n=2). (C) IFN-γ production by M1-specific CD8+ T-cells in response to freshly isolated neutrophils loaded with 0.1 μM synthetic M1(p58-66) peptide or 1 μM M1 protein. Data shown are representative of three HLA-A2+ sepsis patients and three HLA-A2+ healthy volunteers as controls. Sepsis patients recruited for these APC assays had confirmed infections as identified by positive culture results: E. coli (urine), Klebsiella pneumoniae (respiratory culture) and Staphylococcus epidermidis (blood), respectively. (D) Summary of all stimulation assays conducted, shown as percentage of IFN-γ positive CD8+ T-cells in response to freshly isolated neutrophils loaded with peptide or the indicated concentrations of M1 protein (means ± SD, n=3). Data were analyzed by two-way ANOVA with Bonferroni’s post-hoc tests. Differences were considered significant as indicated in the figures: *, p<0.05; **, p<0.01; ***, p<0.001.
Circulating neutrophils from sepsis patients are capable of cross-presenting antigens to CD8+ T-cells
It has not yet been established whether neutrophils are capable of triggering antigen-specific T-cell responses in vivo. To translate our findings on APC-like neutrophils to the situation in acute infections, we isolated untouched neutrophils from sepsis patients to purities of 99.2-99.8%. Our experiments show that sepsis neutrophils and control neutrophils had a similar capacity to activate M1-specific responder CD8+ T-cells when pulsed with the peptide itself (Fig. 6C). Strikingly, only sepsis neutrophils but not control neutrophils were also able to take up the full-length M1 protein and cross-present the M1(p58-66) peptide to responder CD8+ T-cells (Fig. 6C-D), consistent with the differences in APC marker expression between patients and healthy individuals. These findings indicate that in acute sepsis neutrophils acquire an APC-like phenotype with the capacity to induce antigen-specific CD8+ T-cell responses that is reminiscent of neutrophils primed by unconventional T-cells.
DISCUSSION
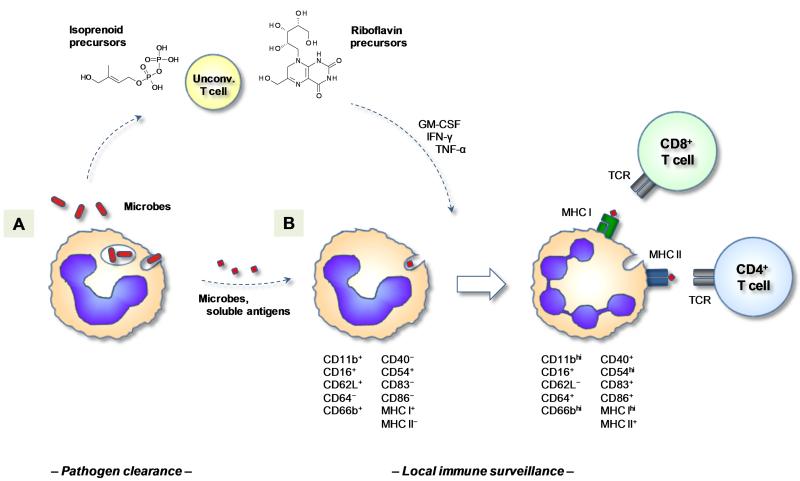
The present study is the first demonstration that human neutrophils can assume antigen cross-presenting properties. Although our work does not formally demonstrate a causal link for the interaction of unconventional T-cells and neutrophils in vivo, it does suggest a plausible scenario for the generation of APC-like neutrophils during acute infection. Our data support a model where different types of unconventional T-cells respond rapidly to neutrophils after phagocytosis of a broad range of bacteria at the site of infection, and in turn mediate the local differentiation of bystander neutrophils into APCs for both CD4+ and CD8+ T-cells (Fig. 7). APC-like neutrophils may be particularly relevant for local responses by tissue resident memory and/or freshly recruited effector CD4+ and CD8+ T-cells at the site of infection, rather than the priming of naïve CD4+ and CD8+ T-cells in secondary lymphoid tissues. Expression of the lymph node homing receptor CCR7 by activated neutrophils was reported before (30) but could not be confirmed in the present study (data not shown). Still, APC-like neutrophils may also gain access to inflamed draining lymph nodes through the action of inflammatory chemokines (7-10). Irrespective of the anatomical context, APC-like neutrophils may contribute to protective immune responses, by fighting the “first hit” infection as a result of inducing antigen-specific CD4+ and CD8+ T cells and by harnessing the T-cell compartment against potential “second hit” infections. However, it is also thinkable that such an early induction of cytotoxic CD8+ T cells may add to the systemic inflammatory response and ultimately lead to tissue damage and organ failure. While the generation of APC-like neutrophils is likely to occur locally in the context of infected tissues, in severe inflammatory conditions including sepsis such APC-like neutrophils may eventually leak into the circulation and become detectable in blood. Larger stratified approaches are clearly needed to define the role of APC-like neutrophils in different infectious scenarios, locally and systemically, in clinically and microbiologically well-defined patient subgroups.
FIGURE 7. Proposed model for the local induction of APC-like neutrophils under the influence of microbe-responsive unconventional T-cells.
(A) Upon pathogen clearance, neutrophils release microbial metabolites into the microenvironment where they stimulate local or freshly recruited unconventional T-cells to release pro-inflammatory cytokines. (B) In the presence of unconventional T-cell derived mediators like GM-CSF, IFN-γ and TNF-α, bystander neutrophils acquire the capacity to act as APCs for tissue resident and/or newly arriving effector and memory CD4+ and CD8+ T-cells. Activated neutrophils may also gain access to inflamed draining lymph nodes and prime T-cell responses in secondary lymphoid tissues (not depicted).
The presence of cross-presenting neutrophils in patients with sepsis is intriguing and may point to an essential role of APC-like neutrophils in acute disease. Sepsis patients who survive the primary infection often show signs of reduced surface expression of HLA-DR on monocytes and a relative tolerance of monocytes to LPS stimulation (47). As consequence of what is generally perceived as a loss of immune function, many patients are susceptible to subsequent nosocomial infections including reactivation of latent viruses that are associated with high mortality rates (48, 49). Trials specifically targeted at reversing this apparent monocyte deactivation have shown promising clinical results (50). However, our present findings suggest that HLA-DR expression by circulating monocytes is a poor surrogate marker for a systemic immune suppression and rather indicate that, contrary to the proposed general loss of function, certain cells such as neutrophils may actually assume APC properties under such conditions, as evidence of a gain of new function. Yet, with a complex and multilayered clinical phenomenon such as sepsis it is challenging to dissect the relevance of APC-like neutrophils for infection resolution and clinical outcome in vivo.
With their unique ability to recognize microbial metabolites in a non-MHC restricted manner, unconventional T-cells such as Vγ9/Vδ2 T-cells and MAIT cells greatly outnumber antigen-specific conventional CD4+ and CD8+ T-cells at the site of infection and represent early and abundant sources of pro-inflammatory cytokines (23, 27), amongst which GM-CSF, IFN-γ and TNF-α each make key contributions. Although conventional T-cells may produce a similar combination of cytokines and provide similar signals to neutrophils, preliminary findings in our laboratory indicate that Vγ9/Vδ2 T cells and MAIT cells represent together up to 50% of all TNF-α producing T cells among peritoneal cells stimulated with bacterial extracts, suggesting that these two cell types are indeed major producers of pro-inflammatory cytokines in response to microbial stimulation (A.R.L and M.E., unpublished observations). While we cannot rule out a further contribution of contact-dependent mechanisms this observation builds upon earlier studies describing the generation of human neutrophils expressing MHC class II through the action of recombinant cytokines in vitro (22, 51-56) and in vivo (57-59). Previous investigations reported an upregulation of MHC class II on activated neutrophils under the control of GM-CSF and IFN-γ, albeit the physiological source of those mediators during acute infection was not defined. Most importantly, we here describe a direct role for TNF-α in the efficient induction of MHC class I restricted CD8+ T-cell responses by neutrophils. Of note, plasma from sepsis patients was previously shown to induce some (upregulation of CD64) but not other features (upregulation of CD11b, loss of CD62L) (60) that are characteristic for unconventional T-cell primed neutrophils, indicating that circulating cytokines alone do not confer APC properties. In support of local cell-mediated processes at the site of inflammation, our findings evoke earlier descriptions of APC-like neutrophils characterized by MHC class II expression in infectious and non-infectious inflammatory scenarios such as periodontitis (17) and tuberculous pleuritis (20), where locally activated Vγ9/Vδ2 T-cells were found (61-63). These associations lend further support to the existence of a peripheral immune surveillance network comprised of distinct types of unconventional T-cells and their crosstalk with local immune and non-immune cells. In the absence of unconventional T-cell derived signals, such as during sterile inflammation induced by LPS administration (64), neutrophils may not become fully primed, in accordance with our failure to induce APC-like neutrophils using LPS alone. Of note, a possible feedback regulation may require the activation of unconventional T-cells to reach a certain threshold to overcome the inhibitory effect of bystander neutrophils (65-67).
Our present data demonstrate that both isoprenoid and riboflavin precursors are released by human neutrophils upon phagocytosis of live bacteria and depend on uptake by monocytes and loading onto BTN3A and MR1, respectively. The surprising similarities between Vγ9/Vδ2 T-cells and MAIT cells illustrate their overlapping yet distinct roles. Given the broad distribution of the non-mevalonate and riboflavin pathways across pathogenic, opportunistic and commensal species, the vast majority of invading microbes is likely to be detected by either Vγ9/Vδ2 T-cells or MAIT cells, or both. Our analysis of sepsis patients identified a systemic mobilization of Vγ9/Vδ2 T-cells in response to HMB-PP producing species, in support of their differential responsiveness to distinct groups of bacteria (28, 46). Since the present clinical study was conceived before information about the responsiveness of MAIT cells for riboflavin metabolites became available in the literature, we did not conduct a differential analysis for MAIT cells during acute sepsis. Of note, except for two cases of streptococcal infections, all bacterial and fungal pathogens identified in this patient cohort in fact possessed the riboflavin pathway, i.e. were theoretically capable of stimulating MAIT cells. Intriguingly, Grimaldi et al. 68 recently reported a specific depletion of peripheral MAIT cells in sepsis patients with non-streptococcal (i.e. riboflavin producing) bacteria compared to infections caused by riboflavin-deficient species, which may indicate differences in the recruitment and retention of different types of unconventional T-cells at sites of infection, depending on the nature of the causative pathogen and the underlying pathology (69-72). The contribution of tissue-resident and freshly recruited unconventional T-cells to acute inflammatory responses has implications for clinical outcome and for the development of novel diagnostics and therapeutic interventions (46).
Taken together, our present study provides evidence (i) that Vγ9/Vδ2 T-cells and MAIT cells respond similarly to microbial pathogens that produce the corresponding ligands when phagocytosed by human neutrophils; (ii) that once activated both types of unconventional T-cells trigger longer-term survival and differentiation of neutrophils into APC-like cells; (iii) that unconventional T-cell primed neutrophils readily process exogenous antigens and prime both CD4+ and CD8+ T-cells; and (iv) that circulating neutrophils from patients with acute sepsis possess a similar APC-like phenotype and are capable of cross-presenting soluble proteins to antigen-specific CD8+ T-cells ex vivo. These findings define a possible physiological context for the generation of APC-like neutrophils in response to a broad range of microbial pathogens, and imply a unique and decisive role for human unconventional T-cells in orchestrating local inflammatory events and in shaping the transition of the innate to the adaptive phase of the anti-microbial immune response, with implications for diagnosis, therapy and vaccination.
Supplementary Material
ACKNOWLEDGMENTS
We are grateful to all patients and volunteers for participating in this study, and the clinicians and nurses for their cooperation. We also thank Mark Toleman for clinical pathogens; Hassan Jomaa and Boris Illarionov for HMB-PP and DMRL; Andy Thomas for recombinant M1 protein and HLA-A2 tetramers; Ted Hansen and Daniel Olive for mAbs; Ann Kift-Morgan for multiplex ELISA measurements; Catherine Naseriyan for cell sorting; Chia-Te Liao for help with cytospins; and Marco Cassatella, Adrian Hayday, Ian Sabroe and Phil Taylor for the stimulating discussion.
This research was supported by the UK Clinical Research Network Study Portfolio, the National Institute for Social Care and Health Research (NISCHR), the NISCHR/Wellcome Trust Institutional Strategic Support Fund, the Severnside Alliance for Translational Research (SARTRE)/South East Wales Academic Health Science Partnership (SEWAHSP) Health Technology Challenge Scheme, the EU-FP7 Marie Curie Initial Training Network “European Training & Research in Peritoneal Dialysis” (EuTRiPD), a Medical Research Council PhD Studentship (to C.J.T.), and Cancer Research UK.
Abbreviations used in this article
- BTN3A
butyrophilin 3A
- DMRL
6,7-dimethyl-8-d-ribityllumazine
- HMB-PP
(E)-4-hydroxy-3-methyl-but-2-enyl pyrophosphate
- MAIT cell
mucosal-associated invariant T cell
- MR1
MHC-related protein 1
- PPD
Mycobacterium tuberculosis purified protein derivate
- TSST-1
Staphylococcus aureus toxic shock syndrome toxin-1
REFERENCES
- 1.Nathan C. Neutrophils and immunity: challenges and opportunities. Nat. Rev. Immunol. 2006;6:173–182. doi: 10.1038/nri1785. [DOI] [PubMed] [Google Scholar]
- 2.Mantovani A, Cassatella MA, Costantini C, Jaillon S. Neutrophils in the activation and regulation of innate and adaptive immunity. Nat. Rev. Immunol. 2011;11:519–531. doi: 10.1038/nri3024. [DOI] [PubMed] [Google Scholar]
- 3.Mócsai A. Diverse novel functions of neutrophils in immunity, inflammation, and beyond. J. Exp. Med. 2013;210:1283–1299. doi: 10.1084/jem.20122220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Müller I, Munder M, Kropf P, Hänsch GM. Polymorphonuclear neutrophils and T lymphocytes: strange bedfellows or brothers in arms? Trends Immunol. 2009;30:522–530. doi: 10.1016/j.it.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 5.Pillay J, Tak T, Kamp VM, Koenderman L. Immune suppression by neutrophils and granulocytic myeloid-derived suppressor cells: similarities and differences. Cell. Mol. Life Sci. 2013;70:3813–3827. doi: 10.1007/s00018-013-1286-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cerutti A, Puga I, Magri G. The B cell helper side of neutrophils. J. Leukoc. Biol. 2013;94:677–682. doi: 10.1189/jlb.1112596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kesteman N, Vansanten G, Pajak B, Goyert SM, Moser M. Injection of lipopolysaccharide induces the migration of splenic neutrophils to the T cell area of the white pulp: role of CD14 and CXC chemokines. J. Leukoc. Biol. 2008;83:640–647. doi: 10.1189/jlb.0807578. [DOI] [PubMed] [Google Scholar]
- 8.Puga I, Cols M, Barra CM, He B, Cassis L, Gentile M, Comerma L, Chorny A, Shan M, Xu W, et al. B cell-helper neutrophils stimulate the diversification and production of immunoglobulin in the marginal zone of the spleen. Nat. Immunol. 2011;13:170–180. doi: 10.1038/ni.2194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abadie V, Badell E, Douillard P, Ensergueix D, Leenen PJ, Tanguy M, Fiette L, Saeland S, Gicquel B, Winter N. Neutrophils rapidly migrate via lymphatics after Mycobacterium bovis BCG intradermal vaccination and shuttle live bacilli to the draining lymph nodes. Blood. 2005;106:1843–1850. doi: 10.1182/blood-2005-03-1281. [DOI] [PubMed] [Google Scholar]
- 10.Chtanova T, Schaeffer M, Han SJ, van Dooren GG, Nollmann M, Herzmark P, Chan SW, Satija H, Camfield K, Aaron H, Striepen B, Robey EA. Dynamics of neutrophil migration in lymph nodes during infection. Immunity. 2008;29:487–496. doi: 10.1016/j.immuni.2008.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beauvillain C, Delneste Y, Scotet M, Peres A, Gascan H, Guermonprez P, Barnaba V, Jeannin P. Neutrophils efficiently cross-prime naive T cells in vivo. Blood. 2007;110:2965–2973. doi: 10.1182/blood-2006-12-063826. [DOI] [PubMed] [Google Scholar]
- 12.Abi Abdallah DS, Egan CE, Butcher BA, Denkers EY. Mouse neutrophils are professional antigen-presenting cells programmed to instruct Th1 and Th17 T cell differentiation. Int. Immunol. 2011;23:317–226. doi: 10.1093/intimm/dxr007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ostanin DV, Kurmaeva E, Furr K, Bao R, Hoffman J, Berney S, Grisham MB. Acquisition of antigen-presenting functions by neutrophils isolated from mice with chronic colitis. J. Immunol. 2012;188:1491–1502. doi: 10.4049/jimmunol.1102296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matsushima H, Geng S, Lu R, Okamoto T, Yao Y, Mayuzumi N, Kotol PF, Chojnacki BJ, Miyazaki T, Gallo RL, Takashima A. Neutrophil differentiation into a unique hybrid population exhibiting dual phenotype and functionality of neutrophils and dendritic cells. Blood. 2013;121:1677–1689. doi: 10.1182/blood-2012-07-445189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Geng S, Matsushima H, Okamoto T, Yao Y, Lu R, Page K, Blumenthal RM, Ward NL, Miyazaki T, Takashima A. Emergence, origin, and function of neutrophil-dendritic cell hybrids in experimentally induced inflammatory lesions in mice. Blood. 2013;121:1690–1700. doi: 10.1182/blood-2012-07-445197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iking-Konert C, Vogt S, Radsak M, Wagner C, Hänsch GM, Andrassy K. Polymorphonuclear neutrophils in Wegener’s granulomatosis acquire characteristics of antigen presenting cells. Kidney Int. 2001;60:2247–2262. doi: 10.1046/j.1523-1755.2001.00068.x. [DOI] [PubMed] [Google Scholar]
- 17.Bisson-Boutelliez C, Miller N, Demarch D, Bene MC. CD9 and HLA-DR expression by crevicular epithelial cells and polymorphonuclear neutrophils in periodontal disease. J. Clin. Periodontol. 2011;28:650–656. doi: 10.1034/j.1600-051x.2001.028007650.x. [DOI] [PubMed] [Google Scholar]
- 18.Cross A, Bucknall RC, Cassatella MA, Edwards SW, Moots RJ. Synovial fluid neutrophils transcribe and express class II major histocompatibility complex molecules in rheumatoid arthritis. Arthritis Rheum. 2003;48:2796–2806. doi: 10.1002/art.11253. [DOI] [PubMed] [Google Scholar]
- 19.Iking-Konert C, Ostendorf B, Sander O, Jost M, Wagner C, Joosten L, Schneider M, Hänsch GM. Transdifferentiation of polymorphonuclear neutrophils to dendritic-like cells at the site of inflammation in rheumatoid arthritis: evidence for activation by T cells. Ann. Rheum. Dis. 2005;64:1436–1442. doi: 10.1136/ard.2004.034132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alemán M, de la Barrera SS, Schierloh PL, Alves L, Yokobori N, Baldini M, Abbate E, Sasiain MC. In tuberculous pleural effusions, activated neutrophils undergo apoptosis and acquire a dendritic cell-like phenotype. J. Infect. Dis. 2005;192:399–409. doi: 10.1086/431680. [DOI] [PubMed] [Google Scholar]
- 21.Sandilands GP, McCrae J, Hill K, Perry M, Baxter D. Major histocompatibility complex class II (DR) antigen and costimulatory molecules on in vitro and in vivo activated human polymorphonuclear neutrophils. Immunology. 2006;119:562–571. doi: 10.1111/j.1365-2567.2006.02471.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wagner C, Iking-Konert C, Hug F, Stegmaier S, Heppert V, Wentzensen A, Hänsch GM. Cellular inflammatory response to persistent localized Staphylococcus aureus infection: phenotypical and functional characterization of polymorphonuclear neutrophils (PMN) Clin. Exp. Immunol. 2006;143:70–77. doi: 10.1111/j.1365-2249.2005.02963.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gold MC, Lewinsohn DM. Co-dependents: MR1-restricted MAIT cells and their antimicrobial function. Nat. Rev. Microbiol. 2013;11:14–19. doi: 10.1038/nrmicro2918. [DOI] [PubMed] [Google Scholar]
- 24.Brennan PJ, Brigl M, Brenner MB. Invariant natural killer T cells: an innate activation scheme linked to diverse effector functions. Nat. Rev. Immunol. 2013;13:101–117. doi: 10.1038/nri3369. [DOI] [PubMed] [Google Scholar]
- 25.Vantourout P, Hayday A. Six-of-the-best: unique contributions of γδ T cells to immunology. Nat. Rev. Immunol. 2013;13:88–100. doi: 10.1038/nri3384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bonneville M, O’Brien RL, Born WK. γδ T cell effector functions: a blend of innate programming and acquired plasticity. Nat. Rev. Immunol. 2010;10:467–478. doi: 10.1038/nri2781. [DOI] [PubMed] [Google Scholar]
- 27.Eberl M, Moser B. Monocytes and γδ T cells: close encounters in microbial infection. Trends Immunol. 2009;30:562–568. doi: 10.1016/j.it.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 28.Davey MS, Lin CY, Roberts GW, Heuston S, Brown AC, Chess JA, Toleman MA, Gahan CG, Hill C, Parish T, Williams JD, Davies SJ, Johnson DW, Topley N, Moser B, Eberl M. Human neutrophil clearance of bacterial pathogens triggers anti-microbial γδ T cell responses in early infection. PLoS Pathog. 2011;7:e1002040. doi: 10.1371/journal.ppat.1002040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Welton JL, Morgan MP, Martí S, Stone MD, Moser B, Sewell AK, Turton J, Eberl M. Monocytes and γδ T cells control the acute-phase response to intravenous zoledronate: insights from a phase IV safety trial. J. Bone Miner. Res. 2013;28:464–471. doi: 10.1002/jbmr.1797. [DOI] [PubMed] [Google Scholar]
- 30.Beauvillain C, Cunin P, Doni A, Scotet M, Jaillon S, Loiry ML, Magistrelli G, Masternak K, Chevailler A, Delneste Y, Jeannin P. CCR7 is involved in the migration of neutrophils to lymph nodes. Blood. 2011;117:1196–1204. doi: 10.1182/blood-2009-11-254490. [DOI] [PubMed] [Google Scholar]
- 31.Kastenmüller W, Torabi-Parizi P, Subramanian N, Lämmermann T, Germain RN. A spatially-organized multicellular innate immune response in lymph nodes limits systemic pathogen spread. Cell. 2012;150:1235–1248. doi: 10.1016/j.cell.2012.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barral P, Sánchez-Niño MD, van Rooijen N, Cerundolo V, Batista FD. The location of splenic NKT cells favours their rapid activation by blood-borne antigen. EMBO J. 2012;31:2378–2390. doi: 10.1038/emboj.2012.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Davey MS, Tamassia N, Rossato M, Bazzoni F, Calzetti F, Bruderek K, Sironi M, Zimmer L, Bottazzi B, Mantovani A, Brandau S, Moser B, Eberl M, Cassatella MA. Failure to detect production of IL-10 by activated human neutrophils. Nat. Immunol. 2011;12:1017–1018. doi: 10.1038/ni.2111. [DOI] [PubMed] [Google Scholar]
- 34.Brandes M, Willimann K, Moser B. Professional antigen-presentation function by human γδ T cells. Science. 2005;309:264–268. doi: 10.1126/science.1110267. [DOI] [PubMed] [Google Scholar]
- 35.Eberl M, Roberts GW, Meuter S, Williams JD, Topley N, Moser B. A rapid crosstalk of human γδ T cells and monocytes drives the acute inflammation in bacterial infections. PLoS Pathog. 2009;5:e1000308. doi: 10.1371/journal.ppat.1000308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brandes M, Willimann K, Bioley G, Lévy N, Eberl M, Luo M, Tampé R, Lévy F, Romero P, Moser B. Cross-presenting human γδ T cells induce robust CD8+ αβ T cell responses. Proc. Natl. Acad. Sci. USA. 2009;106:2307–2312. doi: 10.1073/pnas.0810059106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Meuter S, Eberl M, Moser B. Prolonged antigen survival and cytosolic export in cross-presenting human γδ T cells. Proc. Natl. Acad. Sci. USA. 2010;107:8730–8735. doi: 10.1073/pnas.1002769107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Khan MWA, Curbishley SM, Chen HC, Thomas AD, Pircher H, Mavilio D, Steven NM, Eberl M, Moser B. Expanded human blood-derived γδ T cells display potent antigen-presentation functions. Front. Immunol. 2014;5:344. doi: 10.3389/fimmu.2014.00344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Morita CT, Jin C, Sarikonda G, Wang H. Nonpeptide antigens, presentation mechanisms, and immunological memory of human Vγ2Vδ2 T cells: discriminating friend from foe through the recognition of prenyl pyrophosphate antigens. Immunol. Rev. 2007;215:59–76. doi: 10.1111/j.1600-065X.2006.00479.x. [DOI] [PubMed] [Google Scholar]
- 40.Le Bourhis L, Martin E, Péguillet I, Guihot A, Froux N, Coré M, Lévy E, Dusseaux M, Meyssonnier V, Premel V, Ngo C, Riteau B, Duban L, Robert D, Huang S, Rottman M, Soudais C, Lantz O. Antimicrobial activity of mucosal-associated invariant T cells. Nat. Immunol. 2010;11:701–708. doi: 10.1038/ni.1890. [DOI] [PubMed] [Google Scholar]
- 41.Kjer-Nielsen L, Patel O, Corbett AJ, Le Nours J, Meehan B, Liu L, Bhati M, Chen Z, Kostenko L, Reantragoon R, Williamson NA, Purcell AW, Dudek NL, McConville MJ, O’Hair RA, Khairallah GN, Godfrey DI, Fairlie DP, Rossjohn J, McCluskey J. MR1 presents microbial vitamin B metabolites to MAIT cells. Nature. 2012;491:717–723. doi: 10.1038/nature11605. [DOI] [PubMed] [Google Scholar]
- 42.López-Sagaseta J, Dulberger CL, McFedries A, Cushman M, Saghatelian A, Adams EJ. MAIT recognition of a stimulatory bacterial antigen bound to MR1. J. Immunol. 2013;191:5268–5277. doi: 10.4049/jimmunol.1301958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Corbett AJ, Eckle SB, Birkinshaw RW, Liu L, Patel O, Mahony J, Chen Z, Reantragoon R, Meehan B, Cao H, Williamson NA, Strugnell RA, Van Sinderen D, Mak JY, Fairlie DP, Kjer-Nielsen L, Rossjohn J, McCluskey J. T-cell activation by transitory neo-antigens derived from distinct microbial pathways. Nature. 2014;509:361–365. doi: 10.1038/nature13160. [DOI] [PubMed] [Google Scholar]
- 44.Harly C, Guillaume Y, Nedellec S, Peigné CM, Mönkkönen H, Mönkkönen J, Li J, Kuball J, Adams EJ, Netzer S, Déchanet-Merville J, Léger A, Herrmann T, Breathnach R, Olive D, Bonneville M, Scotet E. Key implication of CD277/butyrophilin-3 (BTN3A) in cellular stress sensing by a major human γδ T cell subset. Blood. 2012;120:2269–2279. doi: 10.1182/blood-2012-05-430470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sandstrom A, Peigné CM, Léger A, Crooks JE, Konczak F, Gesnel MC, Breathnach R, Bonneville M, Scotet E, Adams EJ. The intracellular B30.2 domain of butyrophilin 3A1 binds phosphoantigens to mediate activation of human Vγ9Vδ2 T cells. Immunity. 2014;40:490–500. doi: 10.1016/j.immuni.2014.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lin CY, Roberts GW, Kift-Morgan A, Donovan KL, Topley N, Eberl M. Pathogen-specific local immune fingerprints diagnose bacterial infection in peritoneal dialysis patients. J. Am. Soc. Nephrol. 2013;24:2002–2009. doi: 10.1681/ASN.2013040332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hotchkiss RS, Monneret G, Payen D. Sepsis-induced immunosuppression: from cellular dysfunctions to immunotherapy. Nat. Rev. Immunol. 2013;13:862–874. doi: 10.1038/nri3552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Angus DC, van der Poll T. Severe sepsis and septic shock. N. Engl. J. Med. 2013;369:840–851. doi: 10.1056/NEJMra1208623. [DOI] [PubMed] [Google Scholar]
- 49.Osawa R, Singh N. Cytomegalovirus infection in critically ill patients: a systematic review. Crit. Care. 2009;13:R68. doi: 10.1186/cc7875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Meisel C, Schefold JC, Pschowski R, Baumann T, Hetzger K, Gregor J, Weber-Carstens S, Hasper D, Keh D, Zuckermann H, Reinke P, Volk HD. Granulocyte-macrophage colony-stimulating factor to reverse sepsis-associated immunosuppression: a double-blind, randomized, placebo-controlled multicenter trial. Am. J. Respir. Crit. Care Med. 2009;180:640–648. doi: 10.1164/rccm.200903-0363OC. [DOI] [PubMed] [Google Scholar]
- 51.Gosselin EJ, Wardwell K, Rigby WF, Guyre PM. Induction of MHC class II on human polymorphonuclear neutrophils by granulocyte/macrophage colony-stimulating factor, IFN-gamma, and IL-3. J. Immunol. 1993;151:1482–1490. [PubMed] [Google Scholar]
- 52.Smith WB, Guida L, Sun Q, Korpelainen EI, van den Heuvel C, Gillis D, Hawrylowicz CM, Vadas MA, Lopez AF. Neutrophils activated by granulocyte-macrophage colony-stimulating factor express receptors for interleukin-3 which mediate class II expression. Blood. 1995;86:3938–3944. [PubMed] [Google Scholar]
- 53.Fanger NA, Liu C, Guyre PM, Wardwell K, O’Neil J, Guo TL, Christian TP, Mudzinski SP, Gosselin EJ. Activation of human T cells by major histocompatability complex class II expressing neutrophils: proliferation in the presence of superantigen, but not tetanus toxoid. Blood. 1997;89:4128–4135. [PubMed] [Google Scholar]
- 54.Oehler L, Majdic O, Pickl WF, Stöckl J, Riedl E, Drach J, Rappersberger K, Geissler K, Knapp W. Neutrophil granulocyte-committed cells can be driven to acquire dendritic cell characteristics. J. Exp. Med. 1998;187:1019–1028. doi: 10.1084/jem.187.7.1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yamashiro S, Wang JM, Yang D, Gong WH, Kamohara H, Yoshimura T. Expression of CCR6 and CD83 by cytokine-activated human neutrophils. Blood. 2000;96:3958–3963. [PubMed] [Google Scholar]
- 56.Radsak M, Iking-Konert C, Stegmaier S, Andrassy K, Hänsch GM. Polymorphonuclear neutrophils as accessory cells for T cell activation: major histocompatibility complex class II restricted antigen-dependent induction of T cell proliferation. Immunology. 2000;101:521–530. doi: 10.1046/j.1365-2567.2000.00140.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mudzinski SP, Christian TP, Guo TL, Cirenza E, Hazlett KR, Gosselin EJ. Expression of HLA-DR (major histocompatibility complex class II) on neutrophils from patients treated with granulocyte-macrophage colony-stimulating factor for mobilization of stem cells. Blood. 1995;86:2452–2453. [PubMed] [Google Scholar]
- 58.Zarco MA, Ribera JM, Villamor N, Balmes A, Urbano Ispizua A, Feliu E. Phenotypic changes in neutrophil granulocytes after G-CSF administration in patients with acute lymphoblastic leukemia under chemotherapy. Haematologica. 1998;83:573–575. [PubMed] [Google Scholar]
- 59.Reinisch W, Lichtenberger C, Steger G, Tillinger W, Scheiner O, Gangl A, Maurer D, Willheim M. Donor dependent, interferon-gamma induced HLA-DR expression on human neutrophils in vivo. Clin. Exp. Immunol. 2003;133:476–484. doi: 10.1046/j.1365-2249.2003.02245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lewis SM, Treacher DF, Bergmeier L, Brain SD, Chambers DJ, Pearson JD, Brown KA. Plasma from patients with sepsis up-regulates the expression of CD49d and CD64 on blood neutrophils. Am. J. Respir. Cell. Mol. Biol. 2009;40:724–732. doi: 10.1165/rcmb.2008-0252OC. [DOI] [PubMed] [Google Scholar]
- 61.Yokobori N, Schierloh P, Geffner L, Balboa L, Romero M, Musella R, Castagnino J, De Stéfano G, Alemán M, de la Barrera S, Abbate E, Sasiain MC. CD3 expression distinguishes two γδ T cell receptor subsets with different phenotype and effector function in tuberculous pleurisy. Clin. Exp. Immunol. 2009;157:385–394. doi: 10.1111/j.1365-2249.2009.03974.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kawahara K, Fukunaga M, Takata T, Kawamura M, Morishita M, Iwamoto Y. Immunohistochemical study of γδ T cells in human gingival tissues. J. Periodontol. 1995;66:775–779. doi: 10.1902/jop.1995.66.9.775. [DOI] [PubMed] [Google Scholar]
- 63.Gemmell E, Seymour GJ. γδ T lymphocytes in human periodontal disease tissue. J. Periodontol. 1995;66:780–785. doi: 10.1902/jop.1995.66.9.780. [DOI] [PubMed] [Google Scholar]
- 64.Pillay J, Kamp VM, van Hoffen E, Visser T, Tak T, Lammers JW, Ulfman LH, Leenen LP, Pickkers P, Koenderman L. A subset of neutrophils in human systemic inflammation inhibits T cell responses through Mac-1. J. Clin. Invest. 2012;122:327–336. doi: 10.1172/JCI57990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wingender G, Hiss M, Engel I, Peukert K, Ley K, Haller H, Kronenberg M, von Vietinghoff S. Neutrophilic granulocytes modulate invariant NKT cell function in mice and humans. J. Immunol. 2012;188:3000–3008. doi: 10.4049/jimmunol.1101273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sabbione F, Gabelloni ML, Ernst G, Gori MS, Salamone G, Oleastro M, Trevani A, Geffner J, Jancic CC. Neutrophils suppress γδ T cell function. Eur. J. Immunol. 2014;44:819–830. doi: 10.1002/eji.201343664. [DOI] [PubMed] [Google Scholar]
- 67.Kalyan S, Chandrasekaran V, Quabius ES, Lindhorst TK, Kabelitz D. Neutrophil uptake of nitrogen-bisphosphonates leads to the suppression of human peripheral blood γδ T cells. Cell Mol Life Sci. 2014;71:2335–2346. doi: 10.1007/s00018-013-1495-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Grimaldi D, Le Bourhis L, Sauneuf B, Dechartres A, Rousseau C, Ouaaz F, Milder M, Louis D, Chiche JD, Mira JP, Lantz O, Pène F. Specific MAIT cell behaviour among innate-like T lymphocytes in critically ill patients with severe infections. Intensive Care Med. 2014;40:192–201. doi: 10.1007/s00134-013-3163-x. [DOI] [PubMed] [Google Scholar]
- 69.Matsushima A, Ogura H, Fujita K, Koh T, Tanaka H, Sumi Y, Yoshiya K, Hosotsubo H, Kuwagata Y, Shimazu T, Sugimoto H. Early activation of γδ T lymphocytes in patients with severe systemic inflammatory response syndrome. Shock. 2004;22:11–15. doi: 10.1097/01.shk.0000129203.84330.b3. [DOI] [PubMed] [Google Scholar]
- 70.Venet F, Bohé J, Debard AL, Bienvenu J, Lepape A, Monneret G. Both percentage of γδ T lymphocytes and CD3 expression are reduced during septic shock. Crit. Care Med. 2005;33:2836–2840. doi: 10.1097/01.ccm.0000189745.66585.ae. [DOI] [PubMed] [Google Scholar]
- 71.Andreu-Ballester JC, Tormo-Calandín C, Garcia-Ballesteros C, Pérez-Griera J, Amigó V, Almela-Quilis A, Ruiz del Castillo J, Peñarroja-Otero C, Ballester F. Association of γδ T cells with disease severity and mortality in septic patients. Clin. Vaccine Immunol. 2013;20:738–746. doi: 10.1128/CVI.00752-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Heffernan DS, Monaghan SF, Chung CS, Cioffi WG, Gravenstein S, Ayala A. A divergent response of innate regulatory T cells to sepsis in humans: Circulating invariant natural killer T cells are preserved. Hum. Immunol. 2014;75:277–282. doi: 10.1016/j.humimm.2013.11.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.