Abstract
CXC chemokine receptor 4 (CXCR4) is a G protein–coupled receptor (GPCR) located on the cell surface that signals upon binding the chemokine stromal derived factor-1 (SDF-1; also called CXCL 12). CXCR4 promotes neuroblastoma proliferation and chemotaxis. CXCR4 expression negatively correlates with prognosis and drives neuroblastoma growth and metastasis in mouse models. All functions of CXCR4 require its expression on the cell surface, yet the molecular mechanisms that regulate CXCR4 cell-surface levels in neuroblastoma are poorly understood. We characterized CXCR4 cell-surface regulation in the related SH-SY5Y and SK-N-SH human neuroblastoma cell lines. SDF-1 treatment caused rapid down-modulation of CXCR4 in SH-SY5Y cells. Pharmacologic activation of protein kinase C similarly reduced CXCR4, but via a distinct mechanism. Analysis of CXCR4 mutants delineated two CXCR4 regions required for SDF-1 treatment to decrease cell-surface CXCR4 in neuroblastoma cells: the isoleucine-leucine motif at residues 328 and 329 and residues 343–352. In contrast, and unlike CXCR4 regulation in other cell types, serines 324, 325, 338, and 339 were not required. Arrestin proteins can bind and regulate GPCR cell-surface expression, often functioning together with kinases such as G protein–coupled receptor kinase 2 (GRK2). Using SK-N-SH cells which are naturally deficient in β-arrestin1, we showed that β-arrestin1 is required for the CXCR4 343–352 region to modulate CXCR4 cell-surface expression following treatment with SDF-1. Moreover, GRK2 overexpression enhanced CXCR4 internalization, via a mechanism requiring both β-arrestin1 expression and the 343–352 region. Together, these results characterize CXCR4 structural domains and β-arrestin1 as critical regulators of CXCR4 cell-surface expression in neuroblastoma. β-Arrestin1 levels may therefore influence the CXCR4-driven metastasis of neuroblastoma as well as prognosis.
Introduction
Neuroblastoma is the most common malignancy in infants, causing one case in every 100,000 children in the United States (Verissimo et al., 2011; Davidoff, 2012). High-risk neuroblastoma patients undergo intensive chemotherapy, stem cell harvesting, and primary tumor resection (Davidoff, 2012), interventions that improve prognosis but cause significant morbidity, developmental delays, leukemia risk, and infertility. There is an urgent need for neuroblastoma treatments that spare normal tissue, including normal developing hematopoietic and other stem cells. In addition to MYCN gene amplification, DNA ploidy changes, and expression of neurotrophin receptors (Vasudevan et al., 2005; Raffaghello et al., 2009; Huang et al., 2011; Davidoff, 2012), elevated expression of the CXCR4 CXC chemokine receptor is a marker and proposed drug target for high-risk neuroblastoma (Shim et al., 2009). CXCR4 expression is associated with neuroblastoma metastatic growth (Liberman et al., 2012), clinical presentation in bone marrow and liver (Geminder et al., 2001; Russell et al., 2004; Meier et al., 2007; Raffaghello et al., 2009; Zhao et al., 2012), and poor prognosis (Russell et al., 2004). Unfortunately, pharmacological targeting of CXCR4 is complicated by the widespread expression of CXCR4 on normal cells. Here, we focus on characterizing the molecular mechanisms that regulate the expression of functional CXCR4 receptors specifically on the neuroblastoma cell surface, information which could potentially lead to more selective approaches for inhibiting the oncogenic activities of CXCR4 in neuroblastoma.
CXCR4 is a member of the superfamily of seven transmembrane–spanning G protein–coupled receptors (GPCRs) (Hanyaloglu and von Zastrow, 2008; Wu et al., 2010; Zlotnik and Yoshie, 2012). CXCR4 is also a chemotactic cytokine, or “chemokine” receptor, that functions to mediate cellular migration toward its chemokine ligand, stromal derived factor-1 (SDF-1; also called CXCL 12) (Zlotnik and Yoshie, 2012). Like other GPCRs, CXCR4 requires expression at the cell surface to bind its ligand. CXCR4 undergoes a conformational change upon binding extracellular ligand that activates the signal transduction function of one or more heterotrimeric G proteins associated with the cytoplasmic face of the receptor, including pertussis toxin–sensitive Gi/o-type G proteins (Zlotnik and Yoshie, 2012). CXCR4 is widely expressed, and has been implicated in regulating the normal migration patterns of immune (Kremer et al., 2011) and other cell types (Dziembowska et al., 2005) into regions that express SDF-1, including the lymph nodes, bone marrow, liver, lung, and brain. Similar to its chemotactic roles for many normal cells, CXCR4 chemotactic signaling drives cancer metastasis, including breast cancer (Liu et al., 2010), lymphoma (Wu et al., 2009), and neuroectodermal cancers (Domanska et al., 2013). The diverse physiologic roles of CXCR4 are highlighted by the effects of genetic knockout of either CXCR4 or SDF-1 in mice, which results in neonatal lethality with defective formation of the brain, gastrointestinal tract, vasculature, and immune system (Tachibana et al., 1998; Baird et al., 1999; Bajetto et al., 2001; Holman et al., 2011). The immune system, including lymphocyte migration and hematopoietic stem cell homing, is also acutely disrupted in humans and mice treated with CXCR4 antagonists (De Clercq, 2009; Modak et al., 2012).
Until now, mechanisms for regulating CXCR4 cell-surface expression have primarily been characterized using epithelial (Cheng et al., 2000; Barker and Benovic, 2011) and immune cells (Kremer et al., 2011; Kumar et al., 2011) rather than neuroblastoma cells. For CXCR4 and other GPCRs, this process typically involves the clustering of ligated receptors into clathrin-coated pits on the plasma membrane followed by membrane invagination and then the pinching off of an endosome and the trafficking of the receptors into early endosomes. Following endocytosis, additional CXCR4 trafficking results in either receptor degradation or recycling back to the cell surface (Kumar et al., 2011). Others have extensively characterized the CXCR4 structural domains and binding proteins important for CXCR4 endocytosis in non-neuronal cell types. These studies have often implicated as a critical control region the carboxyl-terminal “tail” region of CXCR4 that spans approximately the amino acid residues 319–352. For example, in human embryonic kidney 293 (HEK293) epithelial cells, the carboxyl-terminal region of CXCR4 was shown to contain serine phosphorylation sites for G protein–coupled receptor kinases (GRKs), which mediate the direct binding of β-arrestin scaffold proteins responsible for linking CXCR4 to the endocytosis machinery (Busillo et al., 2010). Moreover, within this larger region of CXCR4, the isoleucine-leucine (IL) residues at residues 324 and 325 and a specific serine at residue 338 were found to be important for CXCR4 endocytosis in HEK293 cells (Orsini et al., 2000). In contrast, the 319–352 region of CXCR4 was not required for ligand-dependent CXCR4 internalization in a leukemic cell line (Haribabu et al.,1997). Thus, the mechanisms responsible for mediating CXCR4 endocytosis may differ among cell types.
Here, we characterize the distinctive molecular mechanisms that control how SDF-1 treatment regulates and modulates the levels of cell-surface CXCR4 expression in neuroblastoma. For these studies, we used the well characterized human MYCN-amplified neuroblastoma and neuronal model cell line SH-SY5Y together with its parent line SK-N-SH, derived from a metastatic neuroblastoma tumor (Biedler and Spengler, 1976; Huang et al., 2011). We show evidence that, although protein kinase C (PKC) can activate CXCR4 internalization via phorbol 12-myristate 13-acetate (PMA), PKC is not required for SDF-1 to mediate CXCR4 internalization in neuroblastoma. The mechanistically related phospholipase Cs (PLCs) are similarly not required for SDF-1–mediated CXCR4 endocytosis in neuroblastoma, nor are pertussis toxin (PTX)–sensitive G proteins. Moreover, we identify two portions of the carboxyl-terminal tail region of CXCR4 that are involved in SDF-1–mediated CXCR4 endocytosis, we show that one of these CXCR4 regions is important because it permits CXCR4 endocytosis regulation by β-arrestin1, and we show that CXCR4 endocytosis in neuroblastoma occurs independently of several specific CXCR4 phosphorylation sites that critically mediate CXCR4 endocytosis in other cell types. Furthermore, we show that GRK2 can enhance the ligand-dependent internalization of CXCR4 in these cells, via a mechanism requiring both the carboxyl-terminal tail region of CXCR4 and β-arrestin1 overexpression. Together, these results significantly increase understanding of the molecular mechanisms regulating cell-surface CXCR4 expression in neuroblastoma. Targeting these molecular mechanisms may permit the development of more selective CXCR4-focused treatments for high-risk neuroblastoma patients.
Materials and Methods
Cell Lines.
The related neuroblastoma cell lines SH-SY5Y and SK-N-SH were obtained from American Type Culture Collection (Manassas, VA) and grown in Dulbecco’s modified Eagle’s medium (DMEM; 1X) supplemented with 10% fetal bovine serum, 4.5 g/l d-glucose, 2 mM l-glutamine, and 110 mg/l sodium pyruvate, penicillin/streptomycin, and 5 mM HEPES pH 7.4 (Life Technologies, Green Island, NY). Cells were grown until approximately 80% confluence, then adherent cells were removed from the flasks using 1.5 mM EDTA in 1× phosphate-buffered saline and replated at one-fifth density. SH-SY5Y and SK-N-SH cells were derived from a human metastatic neuroblastoma tumor by Biedler et al. (Biedler and Spengler, 1976; Huang et al., 2011; Zhao et al., 2012; Yusuf et al., 2013). The NTera-2 cell line was obtained from American Type Culture Collection and grown in DMEM and 10% fetal bovine serum (Life Technologies), as previously described (Carlin and Andrews, 1985). The Jurkat human T lymphocyte cell line was maintained as previously described (Kumar et al., 2006, 2011; Kremer et al., 2011). The KG1a leukemia cell line was grown and used for control experiments as previously described (Kremer et al., 2013).
Plasmids, Pharmaceuticals, and Antibodies.
The expression plasmid encoding the human CXCR4 fused to yellow fluorescent protein (YFP) (CXCR4-YFP) was previously described (Kumar et al., 2006). The CXCR4 mutations were constructed in this plasmid using site-directed mutagenesis and confirmed by DNA sequencing. Untagged wild-type CXCR4 (CXCR4wt) and CXCR4Δ322-352 containing green fluorescent protein were also constructed in this manner, used in Supplemental Fig. 1B. The expression plasmid encoding FLAG-tagged β-arrestin1 was a generous gift from Robert Lefkowitz (Luttrell and Lefkowitz, 2002). The expression plasmid encoding bovine GRK2 was a generous gift from Jon Willets (Morris et al., 2011), and the expression plasmid encoding bovine GRK2-K220R was from Addgene (plasmid number 14691; Cambridge, MA). Either 10−7 M SDF-1α (R&D Systems, Minneapolis, MN) or 10 ng/ml PMA (EMD Millipore, Billerica, MA) was used for cell stimulation. All cell stimulations were performed at 37°C for 60 minutes unless otherwise indicated. For inhibition of specific signaling pathways, cells were pretreated for 30 minutes with either 1 μM UCN-01 (7-hydroxystaurosporine; Sigma-Aldrich, St. Louis, MO) or 5 μM U73122 (1-[6-[[(17β)-3-methoxyestra-1,3,5(10)-trien-17-yl]amino]hexyl]-1H-pyrrole-2,5-dione; EMD Millipore) or 15 minutes with 100 ng/ml PTX (Sigma-Aldrich) or 1 hour with 0.6 M sucrose (Sigma-Aldrich), and control cells were pretreated in parallel with equivalent amounts of vehicle (dimethylsulfoxide, ethanol, or inactive b-oligomer toxin, respectively). Activity of dissolved PTX was confirmed using an extracellular signal-regulated kinase (ERK) activation assay as previously described (Kremer et al., 2013). A CXCR4 monoclonal antibody conjugated to APC (R&D Systems) was used for flow cytometric detection of cell-surface CXCR4. β-Arrestin1, GRK2, and ERK2 antisera used for immunoblotting were from Santa Cruz Biotechnology (Santa Cruz, CA); β-actin anti-sera was from Novus Biologicals (Littleton, CO).
Transient Transfection of Neuroblastoma Cell Lines.
All reagents were first slowly brought to room temperature. For each transfection, 2 μg of plasmid DNA, 9 μl of FuGene HD (Promega, Madison, WI), and 200 μl of 1% bovine serum albumin in DMEM were combined and allowed to sit at room temperature for 20 minutes. The particular plasmid(s) included in each transfection varied as indicated. This mixture was then added to 35 mm × 10 mm cell culture dishes containing adherent neuroblastoma cells at approximately 50% confluency together with 1 ml of conditioned cell culture media without penicillin/streptomycin. The dishes were placed at 37°C and analyzed 24 hours later. Transfection efficiencies in different experiments, estimated from the percentage of YFP+ fluorescent cells as detected by flow cytometry, ranged from 1 to 40%. For selected experiments, CXCR4-YFP expression and subcellular localization was also visualized in living, transfected cells using confocal microscopy as in Kumar et al. (2011).
Assay of Cell-Surface CXCR4 Regulation on Neuroblastoma Cells.
Cells were pretreated with inhibitors in some cases, then CXCR4 endocytosis was stimulated by removing the culture media and adding 1 ml of conditioned media containing either SDF-1 or PMA. Following 2–60 minutes of incubation at 37°C, cell-surface CXCR4 levels were assayed by flow cytometry as follows. Stimulated cells were washed in cold fluorescence-activated cell sorter (FACS) buffer consisting of 1× Hanks’ balanced salt solution, 10 mg/ml bovine serum albumin, 10 mM HEPES, and 0.2% sodium azide. Twenty microliters of CXCR4-APC antibody (R&D Systems) was added to the cells and incubated for 20 minutes at 4°C, then cells were washed twice with cold FACS buffer and fixed in 2% paraformaldehyde before being analyzed on either a FACS Canto or FACS Caliber dual color flow cytometer (BD Biosystems, Bedford, MA). WinMDI software (Scripps Research Institute, La Jolla, CA) was used to analyze flow cytometric data; electronic gating was used to selectively analyze transfected YFP+ cells. Similar results were obtained when non–YFP-tagged CXCR4 was used, although the detection of transfected cells was less precise (not shown).
Results
Endogenous CXCR4 Is Expressed on the Surface of SH-SY5Y Cells and Is Rapidly Downregulated in Response to Treatment with SDF-1.
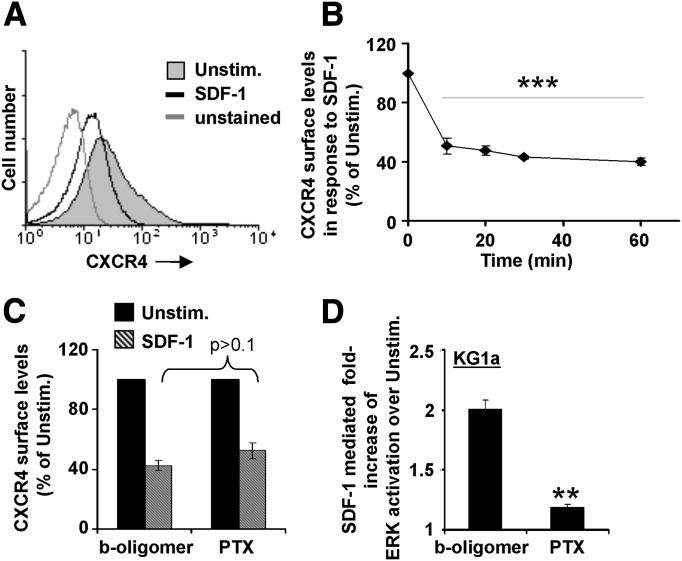
SDF-1 binding has been shown to induce the endocytosis and intracellular trafficking of its receptor, CXCR4, in many cell types (Cheng et al., 2000; Bardi et al., 2006; Ben-Baruch, 2009; Kremer et al., 2011); however, the molecular mechanisms regulating this process have not previously been characterized in neuroblastoma. We began by assaying the expression of CXCR4 on the surface of SH-SY5Y neuroblastoma cells and by characterizing the effects of SDF-1 treatment. To quantitatively compare cell-surface CXCR4 levels, we used flow cytometry to assay the fluorescence associated with individual cells following the staining of the intact cells with fluorescently labeled monoclonal antibody specific for CXCR4. SH-SY5Y cells expressed endogenous CXCR4 on the cell surface, with a mean fluorescence of CXCR4 staining that was greater than that of unstained control cells analyzed the same day (Fig. 1A). In contrast, SH-SY5Y cells treated with SDF-1 for 60 minutes at 37°C prior to staining for cell-surface CXCR4 showed distinctly lower mean fluorescence (Fig. 1A), indicating that CXCR4 was downregulated from the cell surface in response to SDF-1 treatment. Figure 1B plots the mean CXCR4 cell-surface levels of SH-SY5Y cells analyzed at variable times after SDF-1 addition. The ability of SDF-1 to reduce the cell-surface expression of CXCR4 was seen as early as 10 minutes after SDF-1 treatment and was maximal at 60 minutes (Fig. 1B). Not all cell-surface CXCR4 was removed following SDF-1 treatment, most likely because of the existence of refractory receptors or because some internalized CXCR4 recycles back to the cell surface (Kumar et al., 2011). Thus, SDF-1 treatment significantly reduced cell-surface CXCR4 on these neuroblastoma cells by 50–60%. CXCR4 can signal through PTX-sensitive Gi/o-type G proteins; therefore, we also determined the effects of PTX on this process. We found that the SDF-1–mediated internalization of CXCR4 expressed in SH-SY5Y cells was not significantly impaired by pretreatment with PTX as compared with the control inactive b-oligomer (Fig. 1C). As a control, we showed that the same aliquot of PTX significantly inhibited the SDF-1–dependent activation of ERK mitogen-activated protein kinase activity in a leukemic cell line (Fig. 1D), as expected based on a previous publication (Kremer et al., 2013). Thus, SDF-1 treatment induces the endocytosis of CXCR4 in neuroblastoma cells, and does so via a mechanism that is independent of the activity of PTX-sensitive Go/i-type G proteins.
Fig. 1.
Endogenous CXCR4 is expressed on the surface of SH-SY5Y cells, and is rapidly downregulated in response to treatment with SDF-1 independent of Gαi. SH-SY5Y neuroblastoma cells were treated with either nothing (Unstim.) or SDF-1 at 37°C for the indicated times. Cell-surface CXCR4 levels were assayed on individual cells via flow cytometry after staining of intact cells with APC-conjugated CXCR4 monoclonal antibody (mAb). (A) Representative flow cytometric data from one experiment, showing the decreased cell-surface CXCR4 levels on neuroblastoma cells following 60-minute treatment with SDF-1. (B) Summary of multiple experiments performed as in A for various times of SDF-1 treatment. Each point denotes the mean ± S.E.M. CXCR4 cell-surface level of SDF-1–treated as compared with unstimulated cells for three independent experiments ***Significantly different from results using unstimulated cells; P < 0.001. (C) The Gαi/o inhibitor, PTX, fails to inhibit the ability of SDF-1 to decrease cell-surface CXCR4 on neuroblastoma cells. SH-SY5Y cells were pretreated with either inactive control toxin (b-oligomer) or PTX. Cells were then stimulated with SDF-1 for 60 minutes, and cell-surface CXCR4 was assayed as in A and B. A summary of multiple experiments is shown; bars denote the mean ± S.E.M. CXCR4 cell-surface level of SDF-1–treated as compared with unstimulated cells for three independent experiments. Results of cells treated with PTX were not significantly different from control cells; P > 0.5. (D) Positive control for C, showing that PTX pretreatment inhibits ERK activation in the KG1a cell line in response to SDF-1. Bars denote the mean ± S.E.M. ERK activation of three independent experiments. **Significantly different from vehicle-treated cells; P < 0.01.
Treatment with the PKC-Stimulating Drug PMA Downregulates CXCR4 on SH-SY5Y Cells, whereas Treatment with SDF-1 Downregulates CXCR4 on These Cells via a Mechanism Independent of Both PKC and PLC.
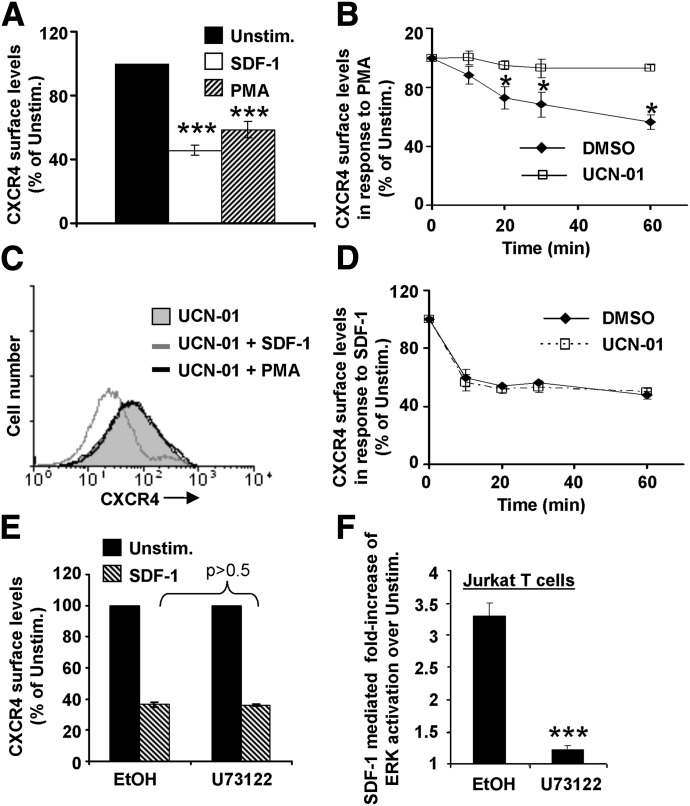
Many GPCRs, including CXCR4, signal by activating PLC (Li et al., 2000; Hwang et al., 2005; Bach et al., 2007; Kremer et al., 2011). PLC activity, in turn, can lead to PKC activation (Geisler, 2004), and PKC can phosphorylate and thereby induce the endocytosis of multiple GPCRs. We therefore tested the effects of the pan-PKC activator drug, PMA, on CXCR4 cell-surface regulation in neuroblastoma cells. We found that PMA treatment of SH-SY5Y cells elicited CXCR4 cell-surface downregulation to a similar extent as did SDF-1 treatment (Fig. 2A). The PKC inhibitor drug UCN-01 blocked the ability of PMA to downregulate CXCR4 cell-surface expression, indicating that the effects of PMA depend on PKC, and that increased PKC activity significantly decreases CXCR4 cell-surface expression in neuroblastoma cells (Fig. 2B). Nevertheless, SDF-1 treatment did not similarly require PKC activity to downregulate cell-surface CXCR4 expression in SH-SY5Y cells. UCN-01 had no effect on the ability of SDF-1 treatment to cause downregulation of cell-surface CXCR4, even though UCN-01 abrogated PMA-mediated downregulation of CXCR4 in the same experiments (Fig. 2, C and D). Additionally, pretreatment with the pan-PLC inhibitor drug U73122 had no effect on SDF-1–mediated downregulation of cell-surface CXCR4 in SH-SY5Y cells (Fig. 2E). Yet the same aliquot of U73122 efficiently blocked SDF-1–stimulated ERK activation in the Jurkat cell line (Fig. 2F), as expected (Kremer et al., 2011). Thus, whereas PMA is capable of eliciting downregulation of CXCR4 from the surface of neuroblastoma cells, neither PKC nor PLC activity is required for the mechanism by which SDF-1 treatment results in the downregulation of cell-surface CXCR4 expression in neuroblastoma cells.
Fig. 2.
Treatment with the PKC-stimulating drug PMA downregulates CXCR4 on SH-SY5Y cells, whereas treatment with SDF-1 downregulates CXCR4 on these cells via a mechanism independent of both PKC and PLC. (A) PMA stimulates the downregulation of cell-surface CXCR4 on neuroblastoma cells. SH-SY5Y cells were treated with nothing, SDF-1, or 10 ng/ml PMA for 60 minutes, then assayed for cell-surface CXCR4 levels as in Fig. 1. A summary of multiple experiments is shown; bars denote the mean ± S.E.M. CXCR4 cell-surface level of SDF-1–treated or PMA-treated cells as compared with unstimulated cells (Unstim.) for three independent experiments. ***Significantly different from unstimulated cells; P < 0.001. (B) The PKC inhibitor UCN-01 blocks the effects of PMA on neuroblastoma cells. SH-SY5Y cells were pretreated with either vehicle (dimethylsulfoxide; DMSO) or UCN-01. Cells were then stimulated with PMA for the indicated times, and cell surface was CXCR4 assayed as in A. Each point denotes the mean ± S.E.M. CXCR4 cell-surface level of SDF-1–treated as compared with unstimulated cells for three independent experiments. *Significantly different from unstimulated cells; P < 0.05. (C and D) UCN-01 does not block the ability of SDF-1 to decrease cell-surface CXCR4 on neuroblastoma cells. (C) Representative experiment in which SH-SY5Y cells were pretreated with UCN-01 as in B. Cells were then stimulated with either SDF-1 or PMA for 60 minutes, and cell-surface CXCR4 levels were measured as in Fig. 1. (D) Summary of multiple experiments as in C, in which cells were pretreated with either vehicle (DMSO) or UCN-01, then stimulated with SDF-1 for the indicated times. Each point denotes the mean ± S.E.M. CXCR4 cell-surface level of SDF-1–treated as compared with DMSO-treated cells for three independent experiments. (E) The PLC inhibitor U73122 fails to inhibit the ability of SDF-1 to decrease cell-surface CXCR4 on neuroblastoma cells. SH-SY5Y cells were pretreated with either vehicle (ethanol, EtOH) or U73122. Cells were then stimulated with SDF-1 for 60 minutes, and cell-surface CXCR4 was assayed as in A. A summary of multiple experiments is shown; bars denote the mean ± S.E.M. CXCR4 cell-surface level of SDF-1–treated as compared with unstimulated cells for three independent experiments. Results of cells treated with U73122 were not significantly different from control cells; P > 0.5. (F) Positive control for E, showing that U73122 pretreatment inhibits ERK activation in the Jurkat T cell line in response to SDF-1. Bars denote the mean ± S.E.M. ERK activation of three independent experiments. ***Significantly different from vehicle-treated cells; P < 0.001.
Fluorescently Tagged CXCR4 Can Be Overexpressed on the Surface of SH-SY5Y Cells, and Is Downregulated from the Cell Surface in Response to Treatment with SDF-1.
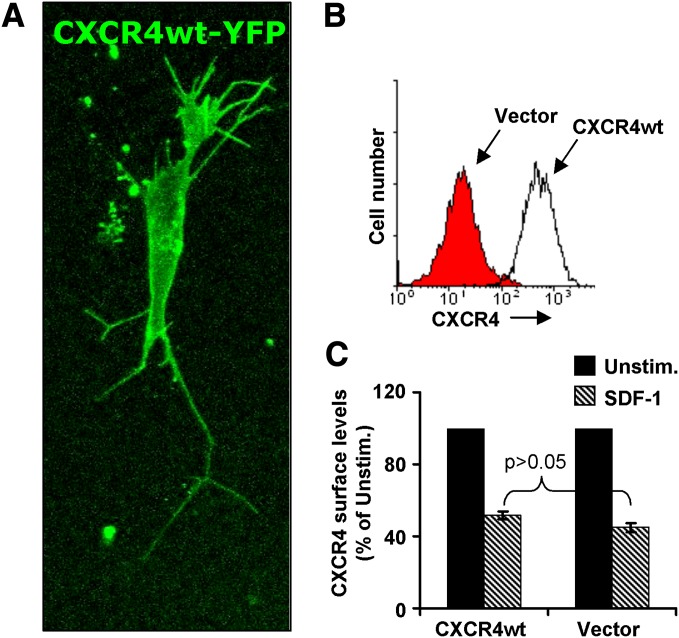
Surface expression of CXCR4 has been shown to be low in several neuroblastoma cell lines (Carlisle et al., 2009). Nevertheless, CXCR4 overexpression is an indicator of worse outcomes for patients with neuroblastoma (Russell et al., 2004) and is also associated with site-specific metastasis particularly to the bone marrow (Geminder et al., 2001; Meier et al., 2007; Ben-Baruch, 2009). To mimic neuroblastoma with elevated CXCR4, and to facilitate our structure/function studies of CXCR4 downregulation, we overexpressed CXCR4 in SH-SY5Y cells using transient transfection of an expression plasmid encoding wild-type CXCR4 tagged with fluorescent YFP (CXCR4wt). The YFP tag was used to facilitate detection of the transfected receptor. SH-SY5Y cells transiently transfected with CXCR4wt expressed CXCR4 that was easily detected by confocal fluorescence microscopy, with CXCR4wt (green) visualized both on the cell surface and within endosomal compartments of living cells (Fig. 3A). A fraction of endosomally located GPCR is expected, representing receptor biosynthetic processing and constitutive receptor recycling (Hanyaloglu and von Zastrow, 2008). Flow cytometric analysis of cell-surface CXCR4 confirmed that, compared with vector-transfected control cells that expressed only endogenous CXCR4, CXCR4wt-transfected SH-SY5Y cells expressed approximately 30-fold higher levels of cell-surface CXCR4 (Fig. 3B). SDF-1 treatment efficiently downregulated this transfected CXCR4wt-YFP from the cell surface (Fig. 3C). Comparing the overexpressed CXCR4wt with endogenous CXCR4 (in the vector-transfected cells), no statistically relevant difference was noted in the extent of CXCR4 downregulation in response to SDF-1 (P > 0.5). Thus, CXCR4 can be overexpressed in SH-SY5Y cells, and this overexpressed CXCR4 downregulates from the cell surface in a manner similar to endogenous CXCR4 when stimulated by SDF-1.
Fig. 3.
Fluorescently tagged CXCR4 can be overexpressed on the surface of SH-SY5Y cells, and is downregulated from the cell surface in response to treatment with SDF-1. To address the role of CXCR4 structural domains on CXCR4 endocytosis, we first tested the effects of overexpressing wild-type CXCR4 tagged with fluorescent YFP (CXCR4wt) in SH-SY5Y cells. (A) Typical confocal fluorescent microscopic image of a transfected SH-SY5Y cell, in which CXCR4wt (green) is seen localized to both the cell surface and within endosomal compartments. (B) SH-SY5Y cells were transiently transfected with plasmids encoding either YFP alone (vector control) or CXCR4wt-YFP. Cell-surface CXCR4 levels of YFP-expressing cells were assayed 24 hours later following CXCR4 staining as in Fig. 1; electronic gating of YFP+ cells was used to compare CXCR4 levels only on transfected cells. (C) SH-SY5Y cells transfected as in B were stimulated with SDF-1 for 60 minutes, then cell-surface CXCR4 levels on transfected cells were assayed by flow cytometry as in B. A summary of multiple experiments is shown; bars denote the mean ± S.E.M. CXCR4 cell-surface levels of SDF-1–treated as compared with unstimulated (Unstim.) cells for three independent experiments.
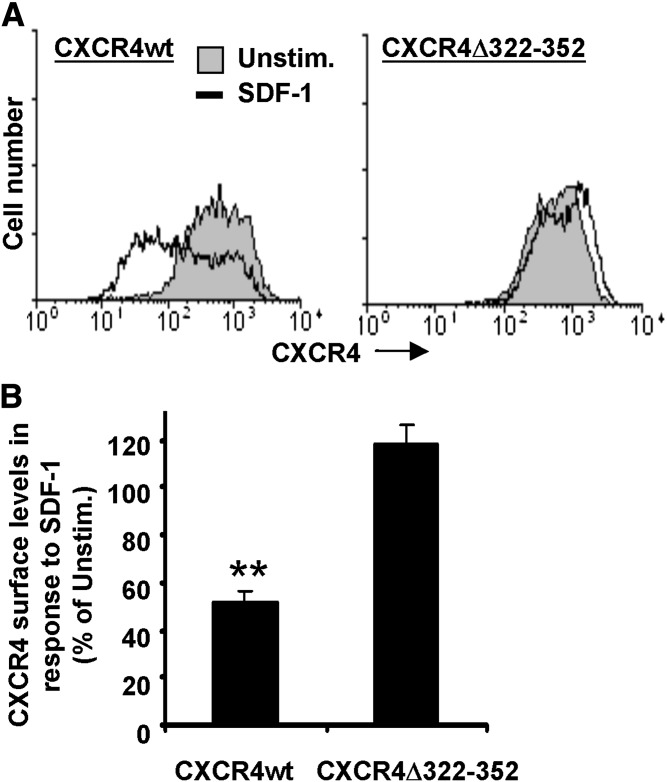
The Cytoplasmic “Tail” Domain of CXCR4 Consisting of the Carboxyl-Terminal Amino Acid Residues 323–352 Is Not Required for Cell-Surface Expression in SH-SY5Y Cells, but Is Required for SDF-1 Treatment to Downregulate CXCR4 from the Cell Surface.
To investigate the CXCR4 structures required for the SDF-1–mediated downregulation of cell-surface CXCR4 in neuroblastoma, we mutated CXCR4 prior to overexpressing it in SH-SY5Y cells. Our results indicate that deleting most of this cytoplasmic carboxyl-terminal “tail” domain of CXCR4 (by removing amino acid residues 323–352 to create CXCR4Δ322-352) had little effect on the ability of CXCR4 to be expressed on the cell surface of unstimulated cells (Fig. 4A, compare solid histograms). Yet unlike wild-type CXCR4, CXCR4Δ322-352 failed to detectably downregulate from the cell surface upon SDF-1 treatment (Fig. 4A). In multiple experiments, CXCR4Δ322-352 did not decrease on the cell surface following 60 minutes of SDF-1 treatment, in contrast to the wild-type CXCR4 (Fig. 4B). Similar results were seen with 60 minutes of PMA stimulation (Supplemental Fig. 1B). Thus, the CXCR4 tail domain is required for SDF-1 treatment to reduce cell-surface levels of CXCR4 in SH-SY5Y neuroblastoma cells.
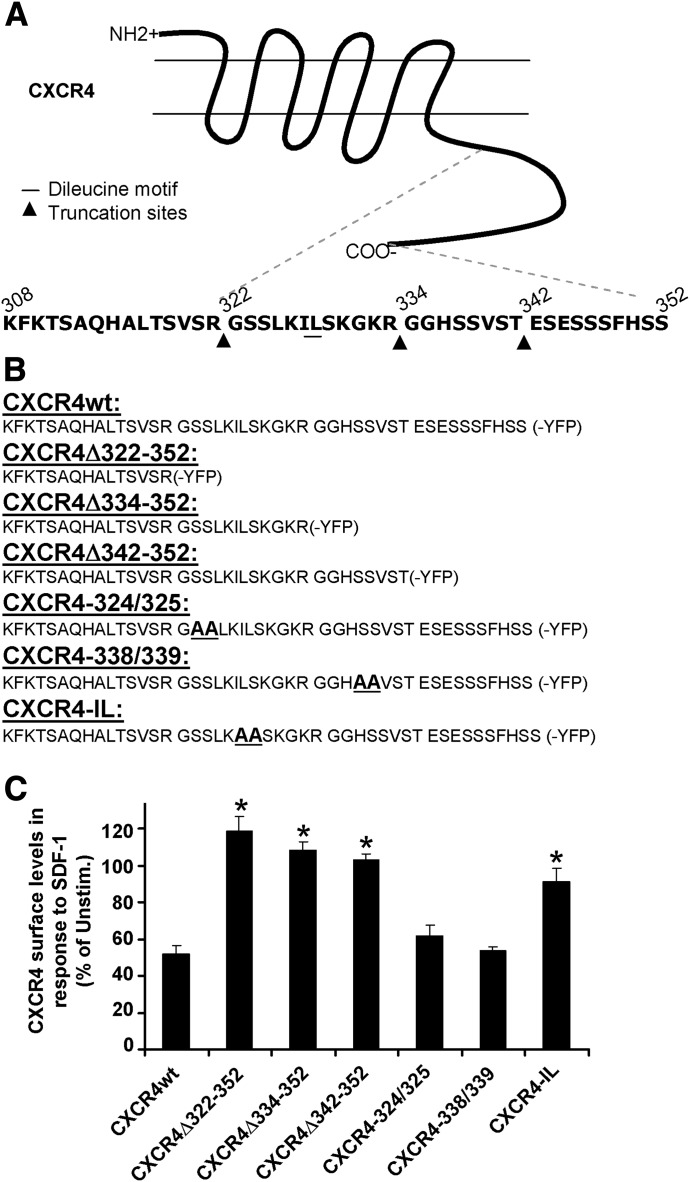
Fig. 5.
Two distinct regions of the CXCR4 “tail” are both required for SDF-1 treatment to downregulate CXCR4 cell-surface expression in SH-SY-5Y cells: the 343–352 region of CXCR4 and the CXCR4 IL motif. (A) Illustration of CXCR4 showing the amino acid residues of the 323–352 “tail” domain. Triangles denote the positions of CXCR4 deletion mutants; the IL motif at residues 328 and 329 is underlined. (B) The carboxyl-terminal amino acid residues of each CXCR4 mutant are shown. (C) SH-SY5Y cells were transiently transfected with plasmids encoding either YFP-tagged wild-type CXCR4 or the indicated YFP-tagged mutant CXCR4 construct. Twenty-four hours later, SDF-1–stimulated downregulation of YFP-tagged CXCR4 was assayed as in Fig. 3 (B and C). A summary of the results of multiple experiments is shown; each bar denotes the mean ± S.E.M. CXCR4 cell-surface levels of SDF-1–treated as compared with unstimulated cells expressing each CXCR4 construct for 3–5 independent experiments. *Significantly different from wild-type CXCR4; P < 0.05.
Fig. 4.
The cytoplasmic “tail” domain of CXCR4 consisting of the carboxyl-terminal amino acid residues 323–352 is not required for cell-surface expression in SH-SY5Y cells, but is required for SDF-1 treatment to downregulate CXCR4 from the cell surface. SH-SY5Y cells were transiently transfected with plasmids encoding either YFP-tagged wild-type (wt) CXCR4 or a YFP-tagged mutant version of CXCR4 that lacks the “tail” domain (Δ322-352). Twenty-four hours later, the cells were assayed as in Fig. 3, B and C, to determine if SDF-1 treatment can downregulate YFP-tagged CXCR4. (A) Results of a representative experiment indicating that 60 minutes of SDF-1 treatment downregulates cell-surface CXCR4wt but not CXCR4Δ322-352. (B) Summary of multiple experiments performed as in A; bars denote the mean ± S.E.M. CXCR4 cell-surface levels of SDF-1–treated as compared with unstimulated (Unstim.) cells for three independent experiments. **Significantly downregulated as compared with unstimulated cells; P < 0.01.
Two Distinct Regions of the CXCR4 “Tail” Are Both Required for SDF-1 Treatment to Downregulate CXCR4 Cell-Surface Expression in SH-SY5Y Cells: The 343–352 Region of CXCR4 and the CXCR4 IL Motif.
The crystal structure of CXCR4 showed that this receptor shares a similar structure with other GPCRs in that it consists of a tight bundle of seven transmembrane α helices; however, the carboxyl tail region of CXCR4 had no notable tertiary structural features (Wu et al., 2010). The CXCR4 carboxyl-terminal tail region does contain several defined phosphorylation and protein binding sites (Orsini et al., 2000). We therefore examined the effects of smaller mutations within the CXCR4 tail domain (Fig. 5, A and B). Two progressively smaller truncation mutants were studied in addition to CXCR4Δ322-352: CXCR4Δ334-352 and CXCR4Δ342-352. All three deletion mutants displayed dramatic inhibition of SDF-1–mediated receptor downregulation (Fig. 5C), indicating that the terminal 10 amino acid residues of CXCR4 (343–352) are minimally required for this downregulation. Additionally, several point mutants within the CXCR4 tail domain were studied. Specifically, two serines at a time, including the confirmed 324 and 338 phosphorylation sites (Orsini et al., 2000; Busillo et al., 2010), were mutated to alanine in the mutants CXCR4-324/325 and CXCR4-338/339. Mutation of these serines did not significantly alter the ability of CXCR4 to internalize in response to SDF-1 treatment (P > 0.5 as compared with CXCR4wt) (Fig. 5C). In contrast to the lack of effect of these serine mutations, dual mutation of CXCR4 I328 and L329 to alanines (creating CXCR4-IL) significantly reduced the ability of SDF-1 to downregulate the cell-surface levels of CXCR4 (Fig. 5C). This IL motif in CXCR4 was previously identified as homologous to the “dileucine motif” that regulates GPCR endocytosis in other cell types (Orsini et al., 2000; Fischer et al., 2011; Guo and Jose, 2011). Flow cytometric analysis indicated that these mutations did not inhibit the cell-surface expression of CXCR4, since the CXCR4 mutants studied were expressed on the cell surface at levels comparable to the wild-type CXCR4 construct (Supplemental Fig. 3, A and B). We also analyzed the ability of CXCR4 to undergo ligand-dependent downregulation from the cell surface using another human neuronal tumor cell line, NTera-2. The results show that, as in SH-SY5Y cells, wild-type CXCR4 internalized readily in response to SDF-1, whereas the CXCR4-IL and CXCR4-D322-352 mutants did not (Supplemental Fig. 2A) (n = 3, P < 0.05). Taken together, the results in Fig. 5 delineate two distinct regions of the CXCR4 tail domain that are both required for SDF-1 treatment to reduce cell-surface expression of CXCR4 in neuronal tumor cells: the 343–352 region of CXCR4, and the CXCR4 IL motif.
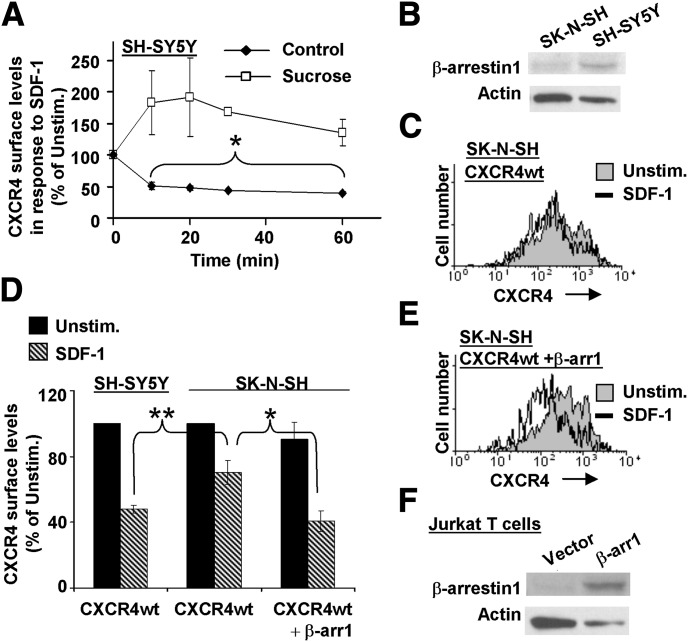
β-Arrestin1 Expression Is Required for SDF-1 Treatment to Efficiently Downregulate Cell-Surface CXCR4 in the Related SK-N-SH Neuroblastoma Cell Line.
The endocytosis of GPCRs can involve their clustering into clathrin-coated pits and clathrin-associated proteins including β-arrestins (Luttrell and Lefkowitz, 2002; Hanyaloglu and von Zastrow, 2008). To address the molecular and cellular mechanisms that mediate CXCR4 endocytosis in neuroblastoma, we first explored the role of clathrin using sucrose, which blocks clathrin-mediated receptor internalization (Heuser and Anderson, 1989; Hansen et al., 1993). We found that SDF-1–mediated downregulation of CXCR4 in SH-SY5Y cells was inhibited in the presence of sucrose (Fig. 6A), as was PMA-mediated CXCR4 downregulation (Supplemental Fig. 1A). These results suggest a role for clathrin in both processes. Next, we asked if this process also involves β-arrestin. We discovered that a related variant of SH-SY5Y, the SK-N-SH cell line, expresses relatively reduced levels of β-arrestin1 protein (Fig. 6B). We therefore determined if this low β-arrestin1 expression affected CXCR4 internalization. Because SK-N-SH cells express only very low levels of endogenous CXCR4 as compared with SH-SY5Y cells, we assayed CXCR4 downregulation in SK-N-SH versus SH-SY5Y cells after transfection of both cell lines with wild-type CXCR4. Significantly, the cell-surface CXCR4 was only poorly downregulated upon SDF-1 treatment of SK-N-SH cells (Fig. 6C), as compared with SH-SY5Y cells (Figs. 2–4). In multiple experiments, the SDF-1–stimulated CXCR4 downregulation was significantly impaired in SK-N-SH cells as compared with SH-SY5Y cells, with 70% ± 7.3% of CXCR4 still remaining on the surface of SDF-1–stimulated SK-N-SH cells as compared with 44% ± 4.1% for SH-SY5Y cells (n = 3–7 ± S.E.M., P < 0.01) (Fig. 6D). To determine if the relative deficiency of β-arrestin1 protein in SK-N-SH cells was responsible for the CXCR4 endocytosis defect in SK-N-SH cells, we transfected SK-N-SH cells with a β-arrestin1 expression plasmid. Adding β-arrestin1 significantly increased the efficiency of SDF-1–dependent downregulation of CXCR4 in SK-N-SH cells (Fig. 6E, compare with Fig. 6C). This result was significant; in multiple experiments, transfection of β-arrestin1 into SK-N-SH cells increased the downregulation of CXCR4 in response to SDF-1 from 70% ± 7.3% CXCR4 remaining on the cell surface after SDF-1 treatment to 41% ± 6.3% (n = 4 ± S.E.M., P < 0.05) (Fig. 6D). Indeed, the downregulation of CXCR4 in β-arrestin1–expressing SK-N-SH cells was not statistically different from SH-SY5Y cells (P > 0.05) (Fig. 6D). As a control, we demonstrated that the same β-arrestin1 expression plasmid efficiently increased expression of β-arrestin1 protein detectable by Western blotting after transfection into the Jurkat T-cell line (Fig. 6F). A similar Western blot could not be done on the transfected SK-N-SH cells due to the low transfection efficiency of these cells (data not shown). Nevertheless, the low transfection efficiency of SK-N-SH cells did not interfere with our flow cytometric assays of CXCR4 cell-surface levels on SK-N-SH cells because electronic gating permitted the selective analysis only of transfected cells. Together, these results indicate that β-arrestin1 expression is required for the efficient downregulation of CXCR4 cell-surface expression in these neuroblastoma cells in response to SDF-1 treatment.
Fig. 6.
β-Arrestin expression is required for SDF-1 treatment to efficiently downregulate cell-surface CXCR4 in the related SK-N-SH neuroblastoma cell line. (A) SH-SY5Y cells were pretreated either with or without 0.6 M sucrose, then assayed for SDF-1–dependent downregulation of endogenous cell-surface CXCR4 as in Fig. 1. The results of three independent experiments are shown as means ± S.E.M. *Significantly different from untreated; P < 0.05. (B) Compared with SH-SY5Y cells, SK-N-SH cells are deficient in expression of β-arrestin1 protein. Top gel: Western blot of whole-cell lysates of SH-SY5Y cells and their variant neuroblastoma cell line SK-N-SH. As a control, the same blot was stripped and reblotted for actin (bottom gel). (C) Results of a representative experiment showing that SDF-1 treatment is defective in stimulating downregulation of cell-surface CXCR4 in SK-N-SH cells. (D) The indicated cell lines were transiently transfected, with either CXCR4wt alone or CXCR4wt plus a β-arrestin1 expression plasmid, as indicated. Twenty-four hours later, the SDF-1–stimulated downregulation of YFP-tagged CXCR4 was assayed as in Fig. 3, B and C. Bars denote the mean ± S.E.M. CXCR4 cell-surface levels of SDF-1–treated as compared with unstimulated (Unstim.) cells for three to seven independent experiments. A comparison of SDF-1–stimulated downregulation of cell-surface CXCR4 in SH-SY5Y and SK-N-SH cells is statistically different (**P < 0.01). Cotransfection with β-arrestin1 significantly enhanced the ability of SDF-1 treatment to downregulate cell-surface CXCR4 on SK-N-SH cells (*P < 0.05) and is not statistically different from SH-SY5Y cells transfected with YFP-tagged wt CXCR4 alone (P > 0.05). (E) Results of a representative experiment as in D for SK-N-SH cells transiently transfected with CXCRwt and β-arrestin1. (F) β-Arrestin1 protein is overexpressed 24 hours after transient transfection of the β-arrestin1 expression plasmid, shown using Jurkat T cell line and immunoblotting whole-cell lysates as in B (top gel). Control cells were transiently transfected with plasmid vector alone. The same blot was stripped and reblotted for actin as a control (bottom gel).
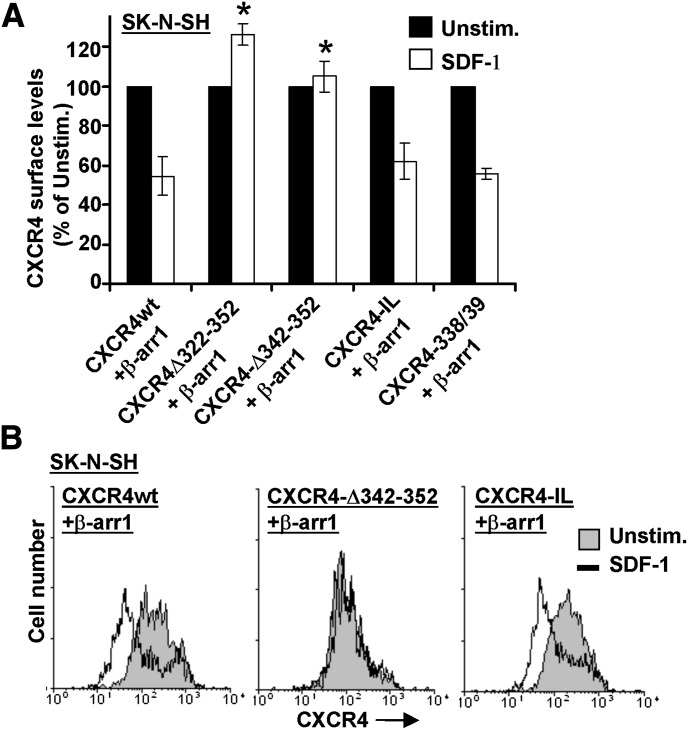
The 343–352 Region of CXCR4, but Not the CXCR4 IL Motif, Is Required for β-Arrestin1 to Regulate Cell-Surface Levels of CXCR4 in SK-N-SH Cells.
Since β-arrestins can bind directly to the CXCR4 tail domain (Orsini et al., 2000; Roland et al., 2003; Busillo et al., 2010), we asked if specific CXCR4 carboxyl region structure(s) were required for the mechanism by which β-arrestin1 expression enhances the down-modulation of CXCR4 from the cell surface of the neuroblastoma cell lines. First, we showed that, as for SH-SY5Y cells that are replete with endogenous β-arrestin1, the β-arrestin1–overexpressing SK-N-SH cells required the CXCR4 tail domain to downmodulate CXCR4 in response to SDF-1. This result was seen in multiple experiments and was statistically significant (Fig. 7A, compare CXCR4wt and CXCR4Δ322-352). Second, we showed that the more limited truncation mutant CXCR4Δ342-352 failed to be downregulated from the cell surface in response to SDF-1 when it was expressed in β-arrestin1–overexpressing SK-N-SH cells (Fig. 7, A and B). Thus, the ability of β-arrestin1 to enhance CXCR4 downmodulation requires the last 10 amino acid residues of CXCR4. Third, we showed that the CXCR4 serines 338 and 339 were not required for this response (Fig. 7A). The CXCR4 338 and 339 mutant was similarly deficient in causing internalization in SK-N-SH cells when compared with CXCR4 wild type (Fig. 6D) in the absence of β-arrestin1 (data not shown) (n = 3 ± S.E.M., P > 0.5). Fourth, and in contrast to its behavior in SH-SY5Y cells, we found that the CXCR4-IL mutant expressed in β-arrestin1–transfected SK-N-SH cells was able to permit the downregulation of cell-surface CXCR4 in response to SDF-1, and that this occurred to an extent that was not significantly different from the behavior of CXCR4wt-YFP (n = 3 ± S.E.M., P > 0.5) (Fig. 7A). Together, these results indicate that the 343–352 region of CXCR4 is necessary for SDF-1 treatment to mediate the downmodulation of cell-surface CXCR4 in neuroblastoma cells via a mechanism requiring β-arrestin1, whereas the CXCR4 IL motif is required for CXCR4 downregulation in SH-SY5Y cells for a distinct reason.
Fig. 7.
The 343–352 region of CXCR4, but not the CXCR4 IL motif, is required for β-arrestin to regulate cell-surface levels of CXCR4 in SK-N-SH cells. SK-N-SH cells were transiently transfected with β-arrestin1 plus either YFP-tagged wild-type or mutant CXCR4. Twenty-four hours later, the SDF-1–stimulated downregulation of YFP-tagged CXCR4 was assayed as in Fig. 3C. (A) Summary of multiple experiments as in B. Bars denote the mean ± S.E.M. CXCR4 cell-surface levels of SDF-1–treated as compared with unstimulated (Unstim.) cells for three independent experiments. Deletion of either the entire tail domain (Δ322–352) or the final 10 amino acid residues (Δ342–352) significantly inhibited the downregulation of CXCR4 associated with β-arrestin1. *Significantly different from CXCR4wt (P < 0.05). (B) Results of a representative experiment performed as in A.
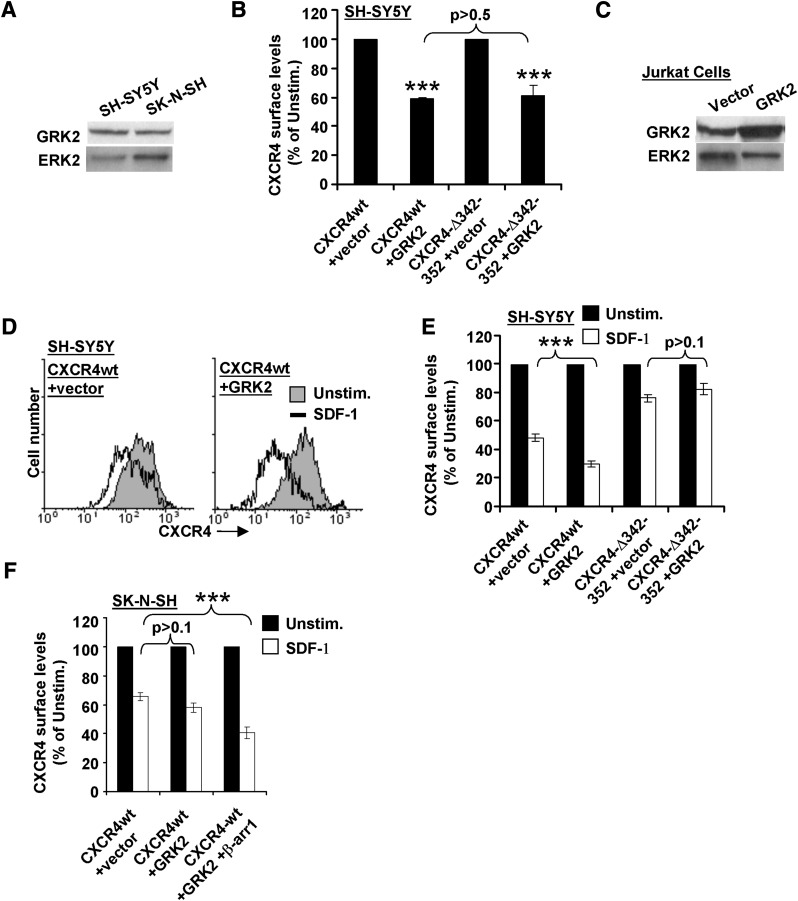
GRK2 Participates in Regulating CXCR4 Cell-Surface Levels and Internalization.
Since several reports suggest that β-arrestins associate with GRKs, and that these proteins function together to regulate GPCRs (Willets et al., 2001; Busillo et al., 2010; Morris et al., 2011), we asked if GRK2 also participates in regulating β-arrestin1–dependent CXCR4 internalization in neuroblastoma cells. GRK2 was endogenously expressed in both SH-SY5Y and SK-N-SH cells (Fig. 8A). Interestingly, overexpressing GRK2 in SH-SY5Y cells via transient transfection of an expression plasmid (Fig. 8C) significantly reduced the cell-surface levels of CXCR4 even in unstimulated neuroblastoma cells. Moreover, this effect of GRK2 was not detectably different when comparing CXCR4wt versus CXCR4-D342-352 (Fig. 8B) (compare 59% ± 0.8% versus 61% ± 7.7%, P > 0.5, n = 3). In contrast to this effect of overexpressing GRK2, overexpressing β-arrestin1 did not alter the levels of unstimulated CXCR4 on these cells (Fig. 6D). Despite the differences in CXCR4 cell-surface levels on unstimulated cells, it is clear that the SDF-1–mediated internalization of wild-type CXCR4 is significantly more complete when GRK2 was overexpressed (Fig. 8, D and E) (n = 3 ± S.E.M., P < 0.05). Figure 8D shows an example of a typical experiment, and Fig. 8E shows the mean results of multiple such experiments. Moreover, GRK2 overexpression did not detectably increase the internalization of the CXCR4Δ342-352 mutant (Fig. 8E) (n = 3 ± S.E.M., P > 0.1), suggesting that this effect of GRK2 also requires β-arrestin1 expression. Consistent with this idea, we found that GRK2 overexpression in the β-arrestin1–deficient SK-N-SH cell line failed to significantly increase the internalization of wild-type CXCR4 unless β-arrestin1 was also expressed (Fig. 8F). In addition, overexpressing a point-mutated, kinase-inactive GRK2 (Willets et al., 2001) in SH-SY5Y cells had no effect on either CXCR4 cell-surface levels of unstimulated cells or SDF-1–induced CXCR4 internalization, indicating that these effects of GRK2 require its kinase activity (Supplemental Fig. 4). Thus, the carboxyl-terminal 343–352 residues of CXCR4 and β-arrestin1 are required for GRK2 to enhance the ligand-dependent internalization of CXCR4 in neuroblastoma cells.
Fig. 8.
GRK2 participates in regulating CXCR4 cell-surface levels and internalization. (A) Western blot of whole-cell lysates of SH-SY5Y cells and their variant neuroblastoma cell line SK-N-SH showing endogenous GRK2 expression levels as compared with ERK2 control. (B) The indicated cell lines were transiently transfected with either CXCR4wt alone or CXCR4wt plus a GRK2 expression plasmid or CXCR4Δ342–352 alone or CXCR4Δ342–352 plus a GRK2 expression plasmid, as indicated. Including the GRK2 expression plasmid significantly reduced CXCR4 surface levels regardless of CXCR4 construct. Bars denote the mean ± S.E.M. CXCR4 cell-surface levels as compared with unstimulated (Unstim.) without GRK2 addition for three independent experiments. ***P < 0.001. (C) Positive control Western blot of whole-cell lysates of Jurkat T cells transfected with the GRK2 expression plasmid. (D) Representative flow cytometric data from one experiment, showing that the decrease in cell-surface CXCR4 levels on SH-SY5Y cells following 60-minute treatment with SDF-1 is enhanced by GRK2 overexpression. (E) Pooled data as in D; bars denote the mean ± S.E.M. CXCR4 cell-surface levels of SDF-1–treated cells as compared with unstimulated cells for three independent experiments. ***P < 0.001. (F) SK-N-SH cells were transiently transfected with YFP-tagged CXCR4wt and either GRK2 or GRK2 and β-arrestin1 expression plasmids. Twenty-four hours later, the SDF-1–stimulated downregulation of YFP-tagged CXCR4 was assayed as in Fig. 3C. Downregulation of YFP-tagged CXCR4 was not significantly different from GRK2-transfected cells; P > 0.1. ***Downregulation of YFP-tagged CXCR4 was significantly different from GRK2- and β-arrestin1–transfected cells; P < 0.001.
Discussion
Here, we characterize two distinct structural regions of CXCR4 that are both necessary for SDF-1 to modulate the cell-surface levels of CXCR4 in neuroblastoma cells. In addition, we show that one of these CXCR4 structural regions (encompassing the CXCR4 amino acid residues 343–352) is further regulated by expression of the β-arrestin1 scaffold protein and GRK2 kinase in these cells, whereas the other CXCR4 structural region (the IL motif) regulates CXCR4 cell-surface levels in neuroblastoma cells via an independent mechanism. Moreover, we showed that ligand-dependent internalization of CXCR4 in these cells does not require activity of PTX-sensitive G proteins. In addition, we showed that activation of an endogenous kinase, PKC, potently downregulates CXCR4 cell-surface levels in neuroblastoma cells in the absence of SDF-1. Finally, and in contrast to previous reports in other cell types (Kremer et al., 2011), we found that CXCR4 cell-surface regulation in neuroblastoma was unaffected by either a PLC inhibitor drug or mutation of several specific CXCR4 serine residues.
β-Arrestin proteins bind to various regions of GPCR cytoplasmic tail domains and regulate endocytosis, frequently in response to GRK-mediated receptor phosphorylation (Luttrell and Lefkowitz, 2002; Kelly et al., 2008; Busillo et al., 2010). Interestingly, we found that β-arrestin1 expression varied significantly between the SH-SY5Y and SK-N-SH neuroblastoma cell lines. Moreover, we found that the lack of β-arrestin1 expression in SK-N-SH cells contributed significantly to the failure of SDF-1 to downmodulate CXCR4 cell-surface levels in these cells. We further showed that CXCR4 cell-surface regulation in SK-N-SH cells was rescued by introduction of β-arrestin1, that β-arrestin1 regulation of CXCR4 levels in both SH-SY5Y and SK-N-SH cells requires the 343–352 region of CXCR4, and that GRK2 overexpression further enhanced ligand-dependent CXCR4 internalization via a mechanism similarly requiring the 343–352 region. This 343–352 CXCR4 region may bind directly to β-arrestin1 in neuronal cells, since it is contained within a larger CXCR4 tail region previously characterized as a β-arrestin binding site in epithelial cells (Cheng et al., 2000; Roland et al., 2003). In further support of our results, both β-arrestin1 and 2 were previously shown to conditionally associate with the CXCR4 tail region upon SDF-1 stimulation of HEK293 cells, and did so via a mechanism requiring a similar carboxyl-terminal region of CXCR4 (Busillo et al., 2010). In contrast, our results suggest that another β-arrestin binding site reportedly located within the third intracellular loop of CXCR4 (Roland et al., 2003), which was intact in all our CXCR4 mutants, either does not bind β-arrestin1 in neuroblastoma cells or plays no role in regulating CXCR4 endocytosis in these cells.
Our results significantly improve understanding of CXCR4 regulation in neuroblastoma, and may lead to better therapies for this disease. All known effects of CXCR4 require its expression on the cell surface, which is required for CXCR4 to bind SDF-1 and initiate signal transduction. Yet until now, the molecular mechanisms involved in regulating the cell-surface levels of CXCR4 and other GPCRs, which typically vary among different cell types, have mainly been studied in cell types other than neuroblastoma (Bhandari et al., 2007; Kelly et al., 2008; Holman et al., 2011). Here, we focused on characterizing the molecular mechanisms responsible for the SDF-1–dependent modulation of CXCR4 cell-surface expression in neuroblastoma cells, since this type of CXCR4 down-modulation has been shown to functionally lower cellular responses to SDF-1 (Kumar et al., 2011), and since aggressiveness and poor prognosis in neuroblastoma correlate with SDF-1/CXCR4 signaling in these cells (Geminder et al., 2001; Domanska et al., 2013).
Our results indicate that CXCR4 cell-surface regulation in neuroblastoma may involve some mechanisms that are relatively tissue-specific, which may be helpful for designing future therapies for this disease. For example, we found no role for the CXCR4 phosphorylation sites 324 and 338 in regulating CXCR4 cell-surface levels in neuroblastoma cells, in contrast with previous reports on epithelial cells (Orsini et al., 2000). In another example, we found evidence that neuroblastoma cells and lymphocytes differ significantly in phosphoinositide pathway regulation of cell-surface CXCR4. We showed that a PLC inhibitor drug which impairs SDF-1–dependent downmodulation of CXCR4 in T lymphocytes (Kremer et al., 2011) had no effect on CXCR4 cell-surface regulation in neuroblastoma. This latter result is particularly interesting because it suggests that there may be a way to therapeutically modulate CXCR4 in neuroblastoma without disrupting normal immune functions. We identified a critical role for β-arrestin1 as a required modulator of CXCR4 cell-surface levels in neuroblastoma cells that may also be relatively specific for this cell type. β-Arrestin1 was previously reported to be dispensable for ligand-dependent CXCR4 internalization in epithelial cells, with this process requiring β-arrestin2 instead (Orsini et al., 2000; Bhandari et al., 2007). Thus, future therapies designed to specifically enhance expression of β-arrestin1 may be able to selectively inhibit CXCR4 cell-surface expression and function in neuroblastoma. Our results additionally suggest that β-arrestin1 expression, together with GRK2, may serve as useful markers in combination with CXCR4 for predicting metastatic risk in neuroblastoma, helping to regulate the migration, proliferation, invasion, and metastasis of neuroblastoma that is dependent on CXCR4 (Raffaghello et al., 2009; Liberman et al., 2012). Other β-arrestin1 binding proteins might also modulate CXCR4 expression and function in neuroblastoma, for example, ESCRT-0, STAM-1, and/or AIP-4 (Bhandari et al., 2007; Malik and Marchese, 2010).
Neuroblastoma derives from the neural crest (Verissimo et al., 2011), and neuroblastoma cell lines including SH-SY5Y have been used as models for studying the molecular pathways involved in neural development and degeneration, such as Parkinson’s disease, Alzheimer’s disease, and multiple sclerosis (Cheung et al., 2009; Agholme et al., 2010; Emanuelsson and Norlin, 2012). Neural crest cells, which migrate via CXCR4, differentiate into Schwann cells, melanocytes, enteric neurons, and chromaffin cells (Verissimo et al., 2011), and can be disregulated to form other neuroectodermal tumors, such as melanoma and small-cell lung cancer (Raffaghello et al., 2009). SDF-1 and CXCR4 have been implicated in the development, proliferation, and migration of neuronal and glial precursors (Bajetto et al., 2001; Stumm and Hollt, 2007) and the etiology and recovery of the nervous system during disease (Carbajal et al., 2011). Yet the molecular regulation of CXCR4 is still poorly understood in these diseases. Our results describing the roles of β-arrestin1, GRK2, and specific CXCR4 structural elements may also be relevant for these related neuroectodermal cells, tumors, and diseases.
Supplementary Material
Acknowledgments
The authors thank Dr. Allan Bieber (Mayo Clinic, Rochester, MN) for help in the critique and editing of this manuscript.
Abbreviations
- CXCR
CXC chemokine receptor
- DMEM
Dulbecco’s modified Eagle’s medium
- ERK
extracellular signal-regulated kinase
- FACS
fluorescence-activated cell sorter
- GPCR
G protein–coupled receptor
- GRK
G protein–coupled receptor kinase
- HEK293
human embryonic kidney 293
- IL
isoleucine-leucine
- PKC
protein kinase C
- PLC
phospholipase C
- PMA
phorbol 12-myristate 13-acetate
- PTX
pertussis toxin
- SDF-1
stromal derived factor-1, also known as chemokine ligand 12
- U73122
1-[6-[[(17β)-3-methoxyestra-1,3,5(10)-trien-17-yl]amino]hexyl]-1H-pyrrole-2,5-dione
- UCN-01
7-hydroxystaurosporine
- wt
wild-type
- YFP
yellow fluorescent protein
Authorship Contributions
Participated in research design: Clift, Bamidele, Kremer, Hedin.
Conducted experiments: Clift, Rodriguez-Ramirez, Bamidele.
Contributed new reagents or analytic tools: Clift, Bamidele, Kremer, Hedin.
Performed data analysis: Clift, Rodriguez-Ramirez, Kremer, Hedin.
Wrote or contributed to the writing of the manuscript: Clift, Hedin.
Footnotes
This work was supported by a National Multiple Sclerosis Society Collaborative Research Center Award (to Mayo Clinic and K.E.H.); the Alma B. Stevenson Endowment Fund for Medical Research (to K.E.H.); and the Mayo Clinic Robert D. and Patricia E. Kern Predoctoral Fellowship for Neuroscience Research (to I.C.C.).
 This article has supplemental material available at molpharm.aspetjournals.org.
This article has supplemental material available at molpharm.aspetjournals.org.
References
- Agholme L, Lindström T, Kågedal K, Marcusson J, Hallbeck M. (2010) An in vitro model for neuroscience: differentiation of SH-SY5Y cells into cells with morphological and biochemical characteristics of mature neurons. J Alzheimers Dis 20:1069–1082 [DOI] [PubMed] [Google Scholar]
- Bach TL, Chen QM, Kerr WT, Wang Y, Lian L, Choi JK, Wu D, Kazanietz MG, Koretzky GA, Zigmond S, et al. (2007) Phospholipase cbeta is critical for T cell chemotaxis. J Immunol 179:2223–2227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baird AM, Gerstein RM, Berg LJ. (1999) The role of cytokine receptor signaling in lymphocyte development. Curr Opin Immunol 11:157–166 [DOI] [PubMed] [Google Scholar]
- Bajetto A, Bonavia R, Barbero S, Florio T, Schettini G. (2001) Chemokines and their receptors in the central nervous system. Front Neuroendocrinol 22:147–184 [DOI] [PubMed] [Google Scholar]
- Bardi G, Sengupta R, Khan MZ, Patel JP, Meucci O. (2006) Human immunodeficiency virus gp120-induced apoptosis of human neuroblastoma cells in the absence of CXCR4 internalization. J Neurovirol 12:211–218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker BL, Benovic JL. (2011) G protein-coupled receptor kinase 5 phosphorylation of hip regulates internalization of the chemokine receptor CXCR4. Biochemistry 50:6933–6941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Baruch A. (2009) Site-specific metastasis formation: chemokines as regulators of tumor cell adhesion, motility and invasion. Cell Adhes Migr 3:328–333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhandari D, Trejo J, Benovic JL, Marchese A. (2007) Arrestin-2 interacts with the ubiquitin-protein isopeptide ligase atrophin-interacting protein 4 and mediates endosomal sorting of the chemokine receptor CXCR4. J Biol Chem 282:36971–36979 [DOI] [PubMed] [Google Scholar]
- Biedler JL, Spengler BA. (1976) A novel chromosome abnormality in human neuroblastoma and antifolate-resistant Chinese hamster cell lives in culture. J Natl Cancer Inst 57:683–695 [DOI] [PubMed] [Google Scholar]
- Busillo JM, Armando S, Sengupta R, Meucci O, Bouvier M, Benovic JL. (2010) Site-specific phosphorylation of CXCR4 is dynamically regulated by multiple kinases and results in differential modulation of CXCR4 signaling. J Biol Chem 285:7805–7817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carbajal KS, Miranda JL, Tsukamoto MR, Lane TE. (2011) CXCR4 signaling regulates remyelination by endogenous oligodendrocyte progenitor cells in a viral model of demyelination. Glia 59:1813–1821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlin CR, Andrews PW. (1985) Human embryonal carcinoma cells express low levels of functional receptor for epidermal growth factor. Exp Cell Res 159:17–26 [DOI] [PubMed] [Google Scholar]
- Carlisle AJ, Lyttle CA, Carlisle RY, Maris JM. (2009) CXCR4 expression heterogeneity in neuroblastoma cells due to ligand-independent regulation. Mol Cancer 8:126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng ZJ, Zhao J, Sun Y, Hu W, Wu YL, Cen B, Wu GX, Pei G. (2000) beta-arrestin differentially regulates the chemokine receptor CXCR4-mediated signaling and receptor internalization, and this implicates multiple interaction sites between beta-arrestin and CXCR4. J Biol Chem 275:2479–2485 [DOI] [PubMed] [Google Scholar]
- Cheung YT, Lau WK, Yu MS, Lai CS, Yeung SC, So KF, Chang RC. (2009) Effects of all-trans-retinoic acid on human SH-SY5Y neuroblastoma as in vitro model in neurotoxicity research. Neurotoxicology 30:127–135 [DOI] [PubMed] [Google Scholar]
- Davidoff AM. (2012) Neuroblastoma. Semin Pediatr Surg 21:2–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Clercq E. (2009) The AMD3100 story: the path to the discovery of a stem cell mobilizer (Mozobil). Biochem Pharmacol 77:1655–1664 [DOI] [PubMed] [Google Scholar]
- Domanska UM, Kruizinga RC, Nagengast WB, Timmer-Bosscha H, Huls G, de Vries EG, Walenkamp AM. (2013) A review on CXCR4/CXCL12 axis in oncology: no place to hide. Eur J Cancer 49:219–230 [DOI] [PubMed] [Google Scholar]
- Dziembowska M, Tham TN, Lau P, Vitry S, Lazarini F, Dubois-Dalcq M. (2005) A role for CXCR4 signaling in survival and migration of neural and oligodendrocyte precursors. Glia 50:258–269 [DOI] [PubMed] [Google Scholar]
- Emanuelsson I, Norlin M. (2012) Protective effects of 27- and 24-hydroxycholesterol against staurosporine-induced cell death in undifferentiated neuroblastoma SH-SY5Y cells. Neurosci Lett 525:44–48 [DOI] [PubMed] [Google Scholar]
- Fischer R, Maier O, Naumer M, Krippner-Heidenreich A, Scheurich P, Pfizenmaier K. (2011) Ligand-induced internalization of TNF receptor 2 mediated by a di-leucin motif is dispensable for activation of the NFκB pathway. Cell Signal 23:161–170 [DOI] [PubMed] [Google Scholar]
- Geisler C. (2004) TCR trafficking in resting and stimulated T cells. Crit Rev Immunol 24:67–86 [DOI] [PubMed] [Google Scholar]
- Geminder H, Sagi-Assif O, Goldberg L, Meshel T, Rechavi G, Witz IP, Ben-Baruch A. (2001) A possible role for CXCR4 and its ligand, the CXC chemokine stromal cell-derived factor-1, in the development of bone marrow metastases in neuroblastoma. J Immunol 167:4747–4757 [DOI] [PubMed] [Google Scholar]
- Guo Y, Jose PA. (2011) C-terminal di-leucine motif of dopamine D₁ receptor plays an important role in its plasma membrane trafficking. PLoS ONE 6:e29204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen SH, Sandvig K, van Deurs B. (1993) Clathrin and HA2 adaptors: effects of potassium depletion, hypertonic medium, and cytosol acidification. J Cell Biol 121:61–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanyaloglu AC, von Zastrow M. (2008) Regulation of GPCRs by endocytic membrane trafficking and its potential implications. Annu Rev Pharmacol Toxicol 48:537–568 [DOI] [PubMed] [Google Scholar]
- Haribabu B, Richardson RM, Fisher I, Sozzani S, Peiper SC, Horuk R, Ali H, Snyderman R. (1997) Regulation of human chemokine receptors CXCR4. Role of phosphorylation in desensitization and internalization. J Biol Chem 272:28726–28731 [DOI] [PubMed] [Google Scholar]
- Heuser JE, Anderson RG. (1989) Hypertonic media inhibit receptor-mediated endocytosis by blocking clathrin-coated pit formation. J Cell Biol 108:389–400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holman DW, Klein RS, Ransohoff RM. (2011) The blood-brain barrier, chemokines and multiple sclerosis. Biochim Biophys Acta 1812:220–230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang R, Cheung NK, Vider J, Cheung IY, Gerald WL, Tickoo SK, Holland EC, Blasberg RG. (2011) MYCN and MYC regulate tumor proliferation and tumorigenesis directly through BMI1 in human neuroblastomas. FASEB J 25:4138–4149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang JI, Kim HS, Lee JR, Kim E, Ryu SH, Suh PG. (2005) The interaction of phospholipase C-beta3 with Shank2 regulates mGluR-mediated calcium signal. J Biol Chem 280:12467–12473 [DOI] [PubMed] [Google Scholar]
- Kelly E, Bailey CP, Henderson G. (2008) Agonist-selective mechanisms of GPCR desensitization. Br J Pharmacol 153 (Suppl 1):S379–S388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kremer KN, Clift IC, Miamen AG, Bamidele AO, Qian NX, Humphreys TD, Hedin KE. (2011) Stromal cell-derived factor-1 signaling via the CXCR4-TCR heterodimer requires phospholipase C-β3 and phospholipase C-γ1 for distinct cellular responses. J Immunol 187:1440–1447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kremer KN, Peterson KL, Schneider PA, Meng XW, Dai H, Hess AD, Smith BD, Rodriguez-Ramirez C, Karp JE, Kaufmann SH, et al. (2013) CXCR4 chemokine receptor signaling induces apoptosis in acute myeloid leukemia cells via regulation of the Bcl-2 family members Bcl-XL, Noxa, and Bak. J Biol Chem 288:22899–22914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar A, Humphreys TD, Kremer KN, Bramati PS, Bradfield L, Edgar CE, Hedin KE. (2006) CXCR4 physically associates with the T cell receptor to signal in T cells. Immunity 25:213–224 [DOI] [PubMed] [Google Scholar]
- Kumar A, Kremer KN, Dominguez D, Tadi M, Hedin KE. (2011) Gα13 and Rho mediate endosomal trafficking of CXCR4 into Rab11+ vesicles upon stromal cell-derived factor-1 stimulation. J Immunol 186:951–958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z, Jiang H, Xie W, Zhang Z, Smrcka AV, Wu D. (2000) Roles of PLC-beta2 and -beta3 and PI3Kgamma in chemoattractant-mediated signal transduction. Science 287:1046–1049 [DOI] [PubMed] [Google Scholar]
- Liberman J, Sartelet H, Flahaut M, Mühlethaler-Mottet A, Coulon A, Nyalendo C, Vassal G, Joseph JM, Gross N. (2012) Involvement of the CXCR7/CXCR4/CXCL12 axis in the malignant progression of human neuroblastoma. PLoS ONE 7:e43665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Ji R, Li J, Gu Q, Zhao X, Sun T, Wang J, Li J, Du Q, Sun B. (2010) Correlation effect of EGFR and CXCR4 and CCR7 chemokine receptors in predicting breast cancer metastasis and prognosis. J Exp Clin Cancer Res 29:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luttrell LM, Lefkowitz RJ. (2002) The role of beta-arrestins in the termination and transduction of G-protein-coupled receptor signals. J Cell Sci 115:455–465 [DOI] [PubMed] [Google Scholar]
- Malik R, Marchese A. (2010) Arrestin-2 interacts with the endosomal sorting complex required for transport machinery to modulate endosomal sorting of CXCR4. Mol Biol Cell 21:2529–2541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier R, Mühlethaler-Mottet A, Flahaut M, Coulon A, Fusco C, Louache F, Auderset K, Bourloud KB, Daudigeos E, Ruegg C, et al. (2007) The chemokine receptor CXCR4 strongly promotes neuroblastoma primary tumour and metastatic growth, but not invasion. PLoS ONE 2:e1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modak S, Cheung IY, Kushner BH, Kramer K, Reich L, Cheung NK. (2012) Plerixafor plus granulocyte-colony stimulating factor for autologous hematopoietic stem cell mobilization in patients with metastatic neuroblastoma. Pediatr Blood Cancer 58:469–471 [DOI] [PubMed] [Google Scholar]
- Morris GE, Nelson CP, Everitt D, Brighton PJ, Standen NB, Challiss RA, Willets JM. (2011) G protein-coupled receptor kinase 2 and arrestin2 regulate arterial smooth muscle P2Y-purinoceptor signalling. Cardiovasc Res 89:193–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orsini MJ, Parent JL, Mundell SJ, Marchese A, Benovic JL. (2000) Trafficking of the HIV coreceptor CXCR4: role of arrestins and identification of residues in the C-terminal tail that mediate receptor internalization. J Biol Chem 275:25876. [DOI] [PubMed] [Google Scholar]
- Raffaghello L, Cocco C, Corrias MV, Airoldi I, Pistoia V. (2009) Chemokines in neuroectodermal tumour progression and metastasis. Semin Cancer Biol 19:97–102 [DOI] [PubMed] [Google Scholar]
- Roland J, Murphy BJ, Ahr B, Robert-Hebmann V, Delauzun V, Nye KE, Devaux C, Biard-Piechaczyk M. (2003) Role of the intracellular domains of CXCR4 in SDF-1-mediated signaling. Blood 101:399–406 [DOI] [PubMed] [Google Scholar]
- Russell HV, Hicks J, Okcu MF, Nuchtern JG. (2004) CXCR4 expression in neuroblastoma primary tumors is associated with clinical presentation of bone and bone marrow metastases. J Pediatr Surg 39:1506–1511 [DOI] [PubMed] [Google Scholar]
- Shim H, Oishi S, Fujii N. (2009) Chemokine receptor CXCR4 as a therapeutic target for neuroectodermal tumors. Semin Cancer Biol 19:123–134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stumm R, Höllt V. (2007) CXC chemokine receptor 4 regulates neuronal migration and axonal pathfinding in the developing nervous system: implications for neuronal regeneration in the adult brain. J Mol Endocrinol 38:377–382 [DOI] [PubMed] [Google Scholar]
- Tachibana K, Hirota S, Iizasa H, Yoshida H, Kawabata K, Kataoka Y, Kitamura Y, Matsushima K, Yoshida N, Nishikawa S, et al. (1998) The chemokine receptor CXCR4 is essential for vascularization of the gastrointestinal tract. Nature 393:591–594 [DOI] [PubMed] [Google Scholar]
- Vasudevan SA, Nuchtern JG, Shohet JM. (2005) Gene profiling of high risk neuroblastoma. World J Surg 29:317–324 [DOI] [PubMed] [Google Scholar]
- Verissimo CS, Molenaar JJ, Fitzsimons CP, Vreugdenhil E. (2011) Neuroblastoma therapy: what is in the pipeline? Endocr Relat Cancer 18:R213–R231 [DOI] [PubMed] [Google Scholar]
- Willets JM, Challiss RA, Kelly E, Nahorski SR. (2001) G protein-coupled receptor kinases 3 and 6 use different pathways to desensitize the endogenous M3 muscarinic acetylcholine receptor in human SH-SY5Y cells. Mol Pharmacol 60:321–330 [DOI] [PubMed] [Google Scholar]
- Wu B, Chien EY, Mol CD, Fenalti G, Liu W, Katritch V, Abagyan R, Brooun A, Wells P, Bi FC, et al. (2010) Structures of the CXCR4 chemokine GPCR with small-molecule and cyclic peptide antagonists. Science 330:1066–1071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu XS, Lonsdorf AS, Hwang ST. (2009) Cutaneous T-cell lymphoma: roles for chemokines and chemokine receptors. J Invest Dermatol 129:1115–1119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yusuf M, Leung K, Morris KJ, Volpi EV. (2013) Comprehensive cytogenomic profile of the in vitro neuronal model SH-SY5Y. Neurogenetics 14:63–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao H, Cai W, Li S, Da Z, Sun H, Ma L, Lin Y, Zhi D. (2012) Establishment and characterization of xenograft models of human neuroblastoma bone metastasis. Childs Nerv Syst 28:2047–2054 [DOI] [PubMed] [Google Scholar]
- Zlotnik A, Yoshie O. (2012) The chemokine superfamily revisited. Immunity 36:705–716 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.