Abstract
An 82-year-old man presented with progressive right frontal headaches. The patient's history was significant for benign polyps on surveillance colonoscopy 2 years prior, without high-grade dysplasia or carcinoma. MRI revealed an enhancing lesion arising within the superomedial aspect of the right orbit. Lesion biopsy demonstrated histological appearance and immunophenotype suggestive of colonic adenocarcinoma. Staging positron emission tomography/CT showed visceral metastases and diffuse activity in the posterior rectosigmoid, consistent with metastatic colon cancer. Treatment of the orbital lesion with external beam radiotherapy to 30 Gy resulted in significant palliation of the patient's headaches. The patient expired 2 months following treatment completion due to disease progression. Orbital metastasis as the initial presentation of an occult colorectal primary lesion is exceedingly rare, and occurred in this patient despite surveillance colonoscopy. Radiotherapy remains an efficacious modality for treatment of orbital metastases.
Background
Metastatic lesions in the orbit are uncommon, accounting for approximately 11% of orbital tumours.1 While a plurality of these lesions are derived from primary breast carcinomas, a diversity of primary malignancies have demonstrated capacity for orbital metastasis.1 2 Of note, only a handful of cases of colorectal primary lesions with orbital metastases have been described. We describe a case of primary colonic adenocarcinoma with orbital metastasis as the initial presentation. Given this patient's recent history of negative surveillance colonoscopy, this case highlights the potential for colonic malignancies ‘missed’ on colonoscopy to present in unusual ways. Furthermore, this case emphasises the important role of radiotherapy in treatment of orbital metastases.
Case presentation
An 82-year-old man presented with a 3-week history of progressively worsening right-sided frontal headaches, with radiation of pain to the right orbit. Relevant history includes benign polyp on surveillance colonoscopy 2 years prior to presentation with no high-grade dysplasia or carcinoma. The patient denied diplopia, visual impairment or gait disturbance; review of systems was otherwise negative, including changes in weight or bowel habits. Physical examination, including neurological, ophthalmological and otolaryngological examinations, revealed no abnormalities. Visual acuity and extraocular muscle function were grossly intact; no ptosis or gaze nystagmus was noted.
Investigations
To evaluate the aetiology of the patient's headaches, brain MRI (with and without gadolinium contrast) was performed, revealing a predominantly-homogenous enhancing lesion arising within the posterior superomedial aspect of the right orbit, involving the superior oblique muscle, measuring 1.1×2.1 cm (figure 1). Differential diagnosis of this orbital lesion included lymphoma, metastatic disease, nerve sheath tumour (ie, neurofibroma, schwannoma), plasmacytoma, meningioma, as well as less likely non-neoplastic aetiologies (including orbital pseudotumor). The patient underwent transnasal stereotactically-guided endoscopic biopsy of the intraorbital lesion. Pathological analysis demonstrated histological appearance and immunophenotype (cytokeratin-7 negative, cytokeratin-20 positive) consistent with colonic adenocarcinoma (figure 2). Staging positron emission tomography (PET)/CT showed hypermetabolic pulmonary, hepatic and mesenteric nodules, as well as diffuse activity in the posterior rectosigmoid corresponding to a likely primary site for metastatic colon carcinoma. Serum carcinoembryonic antigen (CEA) was measured once during staging at 13.4 ng/mL, suggestive of a primary colorectal malignancy, but serial CEA levels were not obtained.
Figure 1.
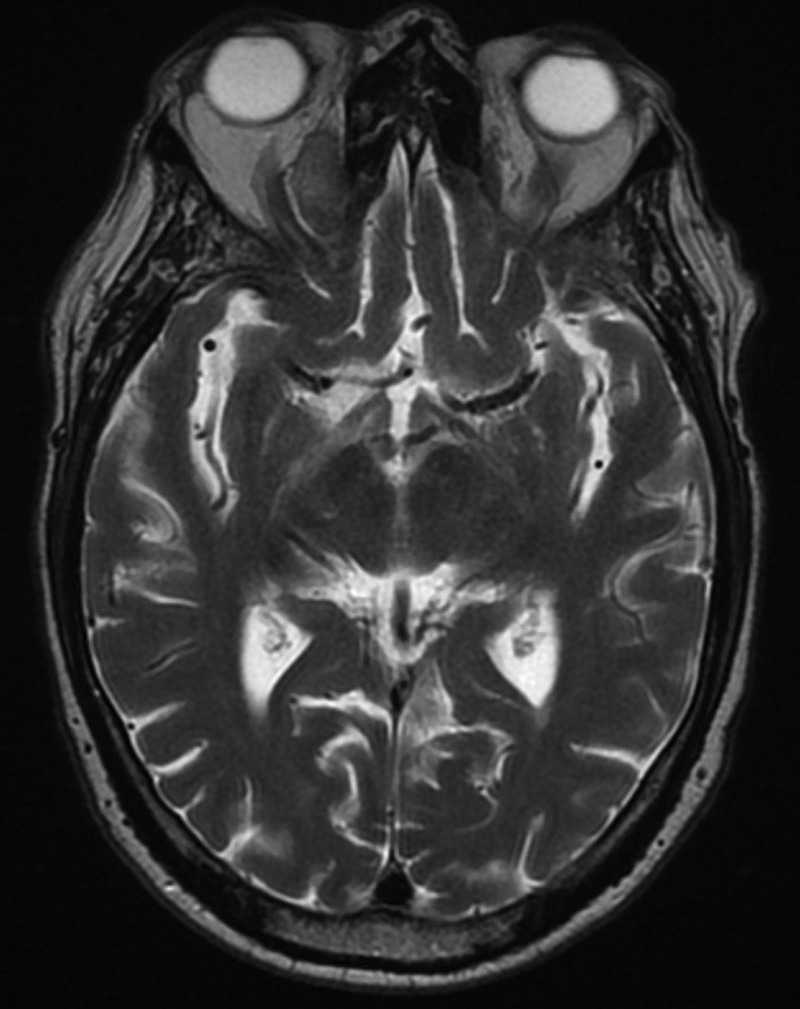
Axial T2-weighted MRI showing right orbital lesion, intrinsically involving the superior oblique muscle.
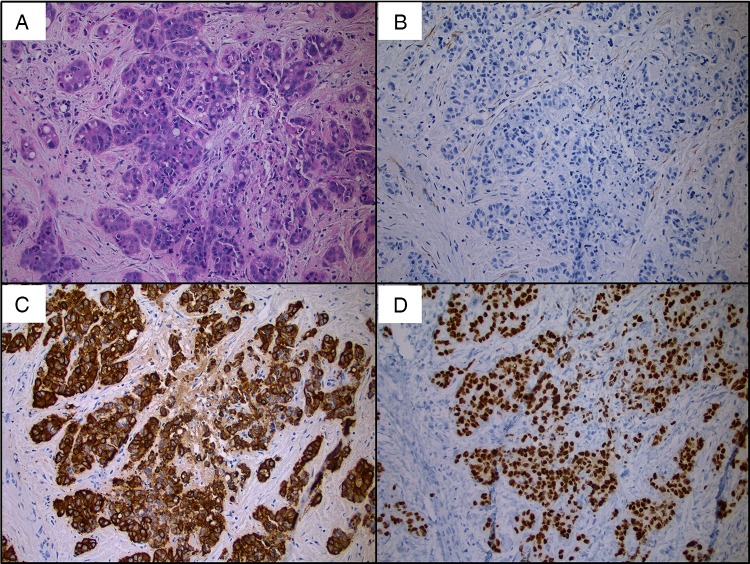
Figure 2.
Histopathology from orbital lesion biopsy: (A) H&E staining demonstrating adenocarcinoma. Immunohistochemistry consistent with colorectal primary: (B) cytokeratin-7 negative, (C) cytokeratin-20 positive, and (D) Cdx2 positive.
Treatment
The patient's symptomatic right orbital lesion was treated with external beam radiotherapy (EBRT) to 30 Gy over 10 fractions, using 3-field approach with customised multileaf collimator blocking to minimise dose to normal tissues (figure 3).
Figure 3.
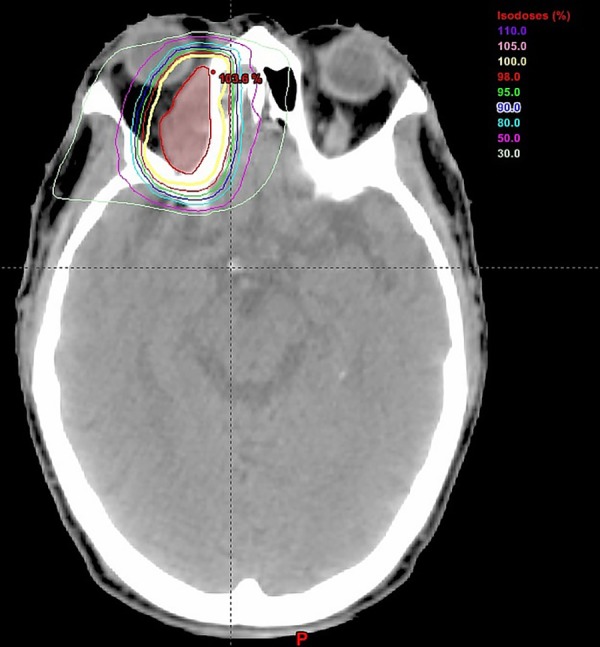
Axial CT during radiotherapy planning. Coloured isodose lines represent relative radiation doses delivered to lesion and surrounding tissues, scaled to 100% of target radiation dose (30 Gy total) to be delivered.
Outcome and follow-up
Radiotherapy to the right orbital lesion resulted in significant palliation of the patient's orbital symptoms, with complete headache resolution. The patient experienced mild tearing in the treated eye during and following EBRT, but otherwise had no periorbital erythema, scleral injection or other acute radiation toxicities. Following completion of radiation therapy, the patient was scheduled to undergo flexible sigmoidoscopy to assess extent of colonic obstruction. However, the patient experienced worsening performance status and expired secondary to disease progression approximately 2 months following orbital EBRT completion, and 6 months following initial presentation.
Discussion
Gastrointestinal primary tumours account for a small percentage of orbital metastases, ranging from 1% to 5%.1–3 Only 10 other cases reporting colorectal malignancies metastatic to the orbit have been described in the literature; these cases are tabulated in table 1.4–13 Of these, three described orbital symptoms as the initial presentation.9 12 13 This report represents the fourth such case. The uniqueness of this case is compounded by the fact that this patient had an extensive history of screening colonoscopies without suspicious findings. Prior analyses have determined that approximately 1.8/1000 patients undergoing screening colonoscopy will develop a ‘missed’ colorectal carcinoma within 5 years of colonoscopy.14 Given the patient's colonoscopy 2 years prior to presentation, this case may represent one such example of a ‘missed’ malignancy on screening. Of note, the benign polyp identified on prior colonoscopy was re-reviewed by a board-certified pathologist in preparation of this case report and confirmed to be free of high-grade dysplasia or carcinoma.
Table 1.
Tabulation of published cases of orbital metastases from primary colorectal malignancies
| Authors | Publication year | Citation | Histology | Orbital symptoms as presentation of malignancy | Number of patients | Treatment of orbital lesion |
|---|---|---|---|---|---|---|
| Rush et al | 1980 | 4 | Carcinoid | No | 1 | Radioactive Cobalt |
| Shetty and Tyers | 1992 | 5 | Adenocarcinoma | No | 1 | External beam radiotherapy |
| Caliandro et al | 1994 | 6 | Adenocarcinoma | Unknown | 1 | Unknown |
| Dizdar et al | 2005 | 7 | Adenocarcinoma | No | 1 | Eye enucleation |
| Hisham et al | 2006 | 8 | Mucinous adenocarcinoma | No | 1 | None |
| Chen et al | 2011 | 9 | Adenocarcinoma | Yes | 1 | Systemic FOLFOX chemotherapy |
| Charles et al | 2012 | 10 | Signet cell adenocarcinoma | No | 1 | Unknown |
| Garcia-Fernandez et al | 2012 | 11 | Unknown | No | 1 | Systemic corticosteroids |
| Chekrine et al | 2013 | 12 | Mucinous adenocarcinoma | Yes | 1 | Unknown |
| Cherif et al | 2014 | 13 | Adenocarcinoma | Yes | 1 | Systemic corticosteroids |
| Ludmir et al | 2014 | NA | Adenocarcinoma | Yes | 1 | External beam radiotherapy |
NA, not applicable.
In view of the unusual features in this case, occult colorectal carcinoma with symptomatic orbital metastasis would be less likely in the differential for this patient at the time of presentation. However, standard investigations facilitated this unlikely diagnosis with minimal unnecessary testing. Imaging followed by biopsy establishes diagnosis in the majority (>70%) of orbital space-occupying lesions in older patients, as in this case.15 Once biopsy suggested metastatic tumour of colonic origin, PET/CT allowed for prompt assessment of disease stage, confirming likely primary tumour origin as well as widespread metastases. By following previously published recommendations for orbital lesion evaluation, these studies facilitated determination of this highly unusual aetiology of the patient's presentation.3 15 16
Prognosis in patients with orbital metastases is poor, with one report describing a median survival of 1.3 years.16 This patient's course was consistent with this observation, with death secondary to disease progression 6 months following presentation. However, this case highlights the important role of palliative radiotherapy in orbital lesions. Radiotherapy is widely considered the most efficacious treatment modality for orbital metastasis, with symptomatic improvement observed in >70% of cases.2 17 18 As utilised in this case, standard radiotherapy courses for orbital metastases typically range from 30 to 40 Gy total dose divided over approximately 10–20 fractions, depending on histology.2 3 The complete resolution of this patient's headaches following radiotherapy underscores the radiosensitivity of these lesions, irrespective of primary neoplasm.2
Learning points.
Primary colorectal adenocarcinomas rarely metastasise to the orbit, but should be considered in the differential diagnosis of orbital metastases.
While negative screening evaluations make certain diagnoses less likely, direct evaluation of space-occupying orbital lesions via imaging and biopsy can pinpoint underlying aetiologies of these lesions.
Orbital metastases tend to be radiosensitive, irrespective of primary tumour origin, and radiotherapy can provide significant palliation.
Acknowledgments
The authors thank the patient’s family for allowing this case to be submitted for publication.
Footnotes
Contributors: All authors were involved in the preparation and writing of this manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions: the 2002 Montgomery Lecture, part 1. Ophthalmology 2004;111:997–1008 [DOI] [PubMed] [Google Scholar]
- 2.Goldberg RA, Rootman J, Cline RA. Tumors metastatic to the orbit: a changing picture. Surv Ophthalmol 1990;35:1–24 [DOI] [PubMed] [Google Scholar]
- 3.Shields JA, Shields CL, Brotman HK, et al. Cancer metastatic to the orbit: the 2000 Robert M. Curts Lecture. Ophthal Plast Reconstr Surg 2001;17:346–54 [DOI] [PubMed] [Google Scholar]
- 4.Rush JA, Waller RR, Campbell RJ. Orbital carcinoid tumor metastatic from the colon. Am J Ophthalmol 1980;89:636–40 [DOI] [PubMed] [Google Scholar]
- 5.Shetty B, Tyers AG. Metastatic carcinoma in the orbit. A case report. Indian J Ophthalmol 1992;40:29–30 [PubMed] [Google Scholar]
- 6.Caliandro R, Souquet PJ, El Khoury MT, et al. Ptosis revealing an orbital metastasis of a rectal adenocarcinoma. Presse Med 1994;23:138. [PubMed] [Google Scholar]
- 7.Dizdar O, Aksoy S, Kilickap S, et al. Orbital metastasis from adenocarcinoma of colon. South Med J 2005;98:846–7 [DOI] [PubMed] [Google Scholar]
- 8.Hisham RB, Thuaibah H, Gul YA. Mucinous adenocarcinoma of the rectum with breast and ocular metastases. Asian J Surg 2006;29:95–7 [DOI] [PubMed] [Google Scholar]
- 9.Chen SF, Yii CY, Chou JW. Colon cancer with orbital metastasis. Clin Gastroenterol Hepatol 2011;9:e76–7 [DOI] [PubMed] [Google Scholar]
- 10.Charles NC, Ng DD, Zoumalan CI. Signet cell adenocarcinoma of the rectum metastatic to the orbit. Ophthal Plast Reconstr Surg 2012;28:e1–2 [DOI] [PubMed] [Google Scholar]
- 11.Garcia-Fernandez M, Castro-Navarro J, Saiz-Ayalab A, et al. Orbital metastases in colorectal cancer: a case report. Arch Soc Esp Oftalmol 2012;87:216–19 [DOI] [PubMed] [Google Scholar]
- 12.Chekrine T, Hassouni A, Hatime M, et al. Orbital metastasis from mucinous adenocarcinoma of the rectum. J Fr Ophtalmol 2013;36:e73–5 [DOI] [PubMed] [Google Scholar]
- 13.Cherif E, Ben Hassine L, Azzabi S, et al. Orbital metastasis as the inaugural presentation of occult rectal cancer. BMJ Case Rep 2014;2014:pii: bcr2013201428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pohl H, Robertson DJ. Colorectal cancers detected after colonoscopy frequently result from missed lesions. Clin Gastroenterol Hepatol 2010;8:858–64 [DOI] [PubMed] [Google Scholar]
- 15.Demirci H, Shields CL, Shields JA, et al. Orbital tumors in the older adult population. Ophthalmology 2002;109:243–8 [DOI] [PubMed] [Google Scholar]
- 16.Char DH, Miller T, Kroll S. Orbital metastases: diagnosis and course. Br J Ophthalmol 1997;81:386–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glassburn JR, Klionsky M, Brady LW. Radiation therapy for metastatic disease involving the orbit. Am J Clin Oncol 1984;7:145–8 [DOI] [PubMed] [Google Scholar]
- 18.Huh SH, Nisce LZ, Simpson LD, et al. Value of radiation therapy in the treatment of orbital metastasis. Am J Roentgenol Radium Ther Nucl Med 1974;120:589–94 [DOI] [PubMed] [Google Scholar]