Abstract
Purpose: The purpose of this study was to assess the incidence of peritoneal adhesions leading to small intestinal obstruction after laparotomy in children in a tertiary paediatric surgical centre.
Methods: A retrospective review of 430 children aged <15 years who had trans-abdominal procedures over a 7 year period.
Results: Four hundred and fifty nine abdominal procedures were performed in 430 children during the study period. The follow up period ranged from 4 months – 7 years (Median 33 months). 22 (4.8%) had intra-operative confirmation of small intestinal obstruction. Their ages ranged from 21 days – 14 years (median 7 years). Postoperative adhesions due to laparotomy for typhoid perforation were the commonest, occurring in 10 (45%). Children undergoing emergency laparotomy were more likely to develop post operative small intestinal obstruction compared to elective laparotomy (p<0.025). Six (27.3%) children had bowel gangrene at laparotomy requiring bowel resection and anastomosis. Post-operative small intestinal obstruction developed in 6 (27.3%). One child died due to sepsis from intestinal gangrene. Conclusion: Small bowel obstruction due to adhesions requiring operative intervention in children in our setting is not un-common. Bowel gangrene is a common complication of postoperative small intestinal obstruction in children in our setting and should be suspected to avoid serious postoperative mortality and morbidity.
Keywords: Adhesions, Intestinal obstruction, children
Introduction
The risk of small bowel obstruction following laparotomy in infants and children has not been well investigated especially in developing countries. Laparotomy for various disease conditions is commonly done in children from developing countries. Ameh et al described adhesive intestinal obstruction in children from Zaria and noted that post-operative adhesions were the commonest cause of adhesion obstruction in children [1].This study aims to assess the incidence of intestinal obstruction due to post-operative peritoneal adhesions in a tertiary paediatric surgical centre
Reports
Patients and Methods
We reviewed the case notes of all children aged <15 years that had laparotomy for various intra-abdominal conditions between January 2001 and December, 2007 at Jos University Teaching Hospital (JUTH), Jos, Central Nigeria. A total of 459 intraabdominal procedures were performed in 430 children during the study period (excluding inguinal hernia repair).
Operative records were reviewed and the findings at re-operation for small intestinal obstruction were analyzed using simple statistical methods. Patients admitted for post-operative peritoneal adhesions but were not operated upon were excluded from the study. All children that had their initial laparotomy elsewhere and had re-operation for small intestinal obstruction in our hospital were also excluded. Information on children that had their initial laparotomy in our unit but had their re-operation for small intestinal obstruction elsewhere was not available. Adhesions were described as “single stranded” if there is only one band causing intestinal obstruction at surgery, “multiple adhesions” if there was more than one offending strand and “dense adhesions” if there was no identifiable interface between the offending strands. A total of 22 had intra-operative confirmation of small intestinal obstruction due to adhesions and form the basis of this report.
RESULTS
Small intestinal obstruction requiring re-operation occurred in 22 (4.8%); 16 (73%) boys and 6 (27%) girls. Two (9.1%) of the 22 had further adhesion related episodes requiring re-operation. Their ages at presentation ranged from 21 days-14 years (median 7 years). At the time of re-operation for small intestinal obstruction, 1 child was a neonate, 4 were infants <1 year, 3 were between 2-4 years; 6 between 5-10 years and 8 more than 10 years old (fig I). The follow-up period ranged from 4 months – 7 years (median 33 months). Ten (45%) of the children requiring laparatomy for small intestinal obstruction due to adhesions had perforated typhoid enteritis. There was a statistically significant difference between emergency and elective procedures (p<0.025), with emergency surgery causing 16 (72% of the post operative adhesive small intestinal obstruction (Table II). Table III shows the age at initial laparotomy and the incidence of small intestinal obstruction following laparotomy at this various age groups. Small intestinal obstruction occurred in greater proportion of neonates (6.1%) and infants within 1 year of age (3.4%) compared with children 1-4 years of age (1.6%). Children older than 4 years also had higher incidences of re-operation for small intestinal obstruction after laparotomy (5.8% in 4-10 years and 8.5% in 11-14 years). Adhesions were commonest within in the first year following surgery; by 6 months about 45% of adhesions had occurred and by 1 year 75% of the adhesions had occurred (Fig II).
Presentation
The presenting features of the 22 children with post-operative small intestinal obstruction are shown in table IV. Abdominal distension was the commonest presenting feature occurring in 22 (100%) children, followed by vomiting in 20 (91%). Other presenting features included constipation 19 (86%) and abdominal pain 18 (82%). Six (27%) presented with fever and 5 of them were found to have intestinal gangrene at operation. The duration of symptoms before presentation ranged from 2-15 days (median 6 days).
Evaluation
The diagnosis of intestinal obstruction was mainly clinical, supported by radiological examination. All the children had plain abdominal radiographs that demonstrated multiple air-fluid levels and bowel distension. None had a contrast study of the gastrointestinal tract. All the patients were resuscitated by correcting urea, electrolytes and fluids derangements. Five children that were anaemic had blood transfusion before laparotomy.
Management
The initial management was non-operative for the first 24 hours hours except two children who had features of bowel gangrene at presentation. These two children had immediate laparotomy after initial resuscitation. The bowel gangrene was confirmed at laparotomy in these two children.
Most of the adhesions were multiple, occurring in 16 (72.3%) children. Single band adhesions occurred in 4 (18.2%) children and dense adhesions were found in only 2 (9.1%) children. Patients with single band adhesion had excision of the adhesive bands and patients with multiple adhesions had lysis of the adhesions after the offending bands had been excised. Six (27.3%) patients with bowel gangrene had excision of the gangrenous bowel and bowel continuity established by anastomosis. Postoperative morbidity occurred in 6(27.3%) children, one of them died. Superficial wound infection was the commonest occurring in 3 (18.2%) children (all 3 of them had had bowel resection and anastomosis for bowel gangrene) that healed after local wound care. One other patient had complete wound dehiscence and anastomotic breakdown that required re-operation. The same child later developed adhesion obstruction that required re-operation at a later date. One other child developed small intestinal obstruction again for which laparotomy was done. The only mortality in this series was a neonate that had laparotomy for bowel perforation due to necrotizing enterocolitis; developed SBO after 7 days of discharged but developed intra-abdominal abscesses after re-operation for small intestinal obstruction requiring laparotomy and drainage.
Conclusions
Surgeons should be careful and meticulous in handling of tissues and generous peritoneal lavage during lapartomy to minimize peritoneal injury to reduce postoperative small intestinal obstruction.
Discussion
Demographics
Adhesions occurring after injury to the peritoneal are results of biochemical and cellular responses that attempt to repair the peritoneum after such injury. While this process is beneficial, it could also have detrimental effects, one of which is SBO. The data on post-operative adhesions in children are few and so most of what we know about adhesions has been documentations from adult series. It has been estimated that over 93% of adults undergoing laparotomy eventually develop adhesions [2]. Grant et al reported that 1.1% of children younger than 16 years undergoing lower abdominal surgery would be admitted as a direct consequence of adhesions and 8.3% would have a readmission that may be related to adhesions after 4 years of initial surgery [3]. In this study the overall incidence of SBO requiring surgery is 4.8% which is high compared to a recent report by Young JY et al [4] who found an incidence of 2.8% readmission for adhesions among children; about 2% requiring laparotomy over a median follow-up period of 3.2 years. They however found a relatively higher incidence of adhesions amongst infants less than 1 year compared to older children. A similar report from UK found that 6% of neonates undergoing a transperitoneal procedure required laparotomy for small intestinal obstruction [5]. The high incidence of post operative small intestinal obstruction after laparotomy in this present study may be related to the indications for the initial surgery. Many of our patients had laprotomy for intra-abdominal septic conditions like typhoid perforation and perfortated appendicitis as shown in table 1. We had earlier noted that post-operative intestinal obstruction was a major late complication in this group of children.[6]. Ameh et al had noted high incidence of adhesions in children with typhoid enteritis [1]. Other authors have also noted a high incidence of adhesion following laparotomy for inflammatory processes and operations which require a lot of tissue handling by the surgeons.[5,7,8]. In another recent publication Grant et al found that operation on the ileum of children is followed by up to 25% readmission for adhesion related problems[9] which goes further to confirm our finding of high incidence of postoperative small intestinal obstruction in children with typhoid ileal perforation.
Another finding in this study is that small intestinal obstruction varies among the different age groups. While the high incidence in neonatal period and early infancy agrees with other studies, the incidence in school age children is at variance with reports elswhere [4, 5]. The high incidence of adhesive SBO in children 4 years and above correlated with an earlier report of typhoid ileal perforation in children of this age group from our centre.[6]
Management
In developed countries, strategies to reduce post-operative adhesions like introduction of talc-free gloves, improved suture materials, better prosthetic materials and minimal access surgery are commonly available; the same may not be true for developing countries, where most of these new technologies are not readily available. It appears therefore that the burden of adhesions may be gradually shifting to developing countries where many open abdominal operations are being performed in children. This study therefore sets out to quantify the incidence of small intestinal obstruction due to adhesions after laparotomy in children in a developing country to raise awareness of this condition and to give an initial data for future work on adhesions in children in this part of the world. Majority of our patients presented with frank features of intestinal obstruction, though late (median duration of symptoms before presentation of 6 days). This may partly explain the high rate of bowel gangrene (27.3%) in this study. This is why the need for patient education after laparotomy to look out for symptoms of possible obstruction and report to hospital for immediate help cannot be overemphasized.
In this study, about three quarter of adhesions occurred within 12 months of surgery (fig II), a similar pattern has been observed elsewhere [2, 4]. Over 70% of the adhesions were multiple. This is not unusual as inflammatory process with multiple insults on the bowel was the main cause of adhesions in this study. Superficial wound infection were the main causes of post-operative morbidity in our patients which is similar to the finding from Zaria [1]. The recurrence rate of 9.1% in this study compares with other series [1, 4]. The only mortality in this study was in a neonate whose operation was complicated by intra-abdominal abscess.
It is pertinent to note here that our policy is to operate on children with postoperative adhesion obstruction if there are no signs of improvement after 24 hours of admission except those that have frank features of peritonitis who then undergo immediate operation after resuscitation. This is because most of our patients present late and to wait for the traditional 48-72 hours of conservative management may be detrimental in some of them that come in with already gangrenous bowel. This policy is supported by the finding in this study that more than a quarter of our patients have bowel gangrene at surgery. The implication of this policy is that most of the children we admit with postoperative small intestinal obstruction are operated upon. It has also been noted by other reports that most children admitted with postoperative small intestinal obstruction would need surgical intervention.[10,11]
Table I. Type of operation
| Type of operation | No | SBO | % |
| Elective | 237 | 6 | 2.5 |
| Emergency | 222 | 16 | 7.2 |
| Total | 459 | 22 | 4.8 |
| P<0.025 | |||
Table 2. Age at initial laparotomy and rate of adhesion obstruction in 22 children
| Age | No of Laparotomy | SIO | Percentage |
| 0-28 days | 66 | 4 | 6.1 |
| >28 days-1 year | 89 | 3 | 3.4 |
| 1-4 years | 123 | 2 | 1.6 |
| 5-10 years | 86 | 5 | 5.8 |
| 11-15 years | 95 | 8 | 8.4 |
| Total | 459 | 22 | 4.8 |
| SIO Small intestinal obstruction | |||
Fig I.
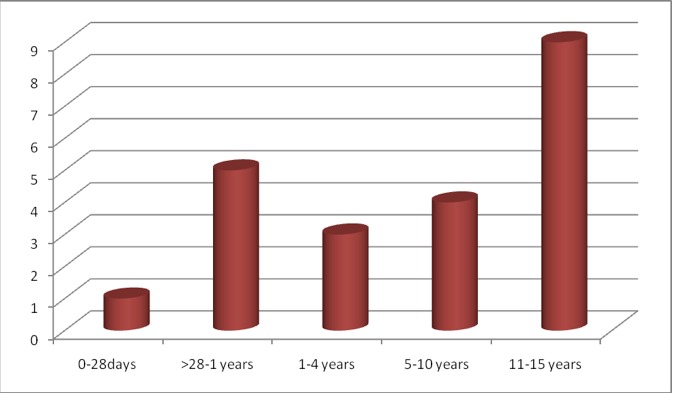
Age at re-operation for small intestinal obstruction
Fig. II.

Time from operation to development of SBO
References
- 1.Grant HW, Parker MC, Wilson MS, Menzies D, Sunderland G, Thompson JN Clark,, Knight AD, Crowe AM, Ellis H. Population-based analysis of the risk of adhesion-related re-admissions after abdominal surgery in children. J Pediatr Surg. 2006;41:1453–1456. doi: 10.1016/j.jpedsurg.2006.04.023. [DOI] [PubMed] [Google Scholar]
- 2.Ameh EA, Nmadu PT. Adhesion obstruction in children in northern Nigeria. Trop Doct . 2004;34:104–6. doi: 10.1177/004947550403400219. [DOI] [PubMed] [Google Scholar]
- 3.Menzies D, Ellis H. Intestinal obstruction from adhesions: how big is the problem? . Ann R Coll Surg Engl. 1990;72:60–63. [PMC free article] [PubMed] [Google Scholar]
- 4.Young JY, Kim DS, Muratore CS, Kurkchubasche AG, Tracy TF(Jr), Luks FI. High incidence of postoerative bowel obstruction in newborns and infants. J Pediatr Surg . 2007;42:962–965. doi: 10.1016/j.jpedsurg.2007.01.030. [DOI] [PubMed] [Google Scholar]
- 5.Choudhry MS, Grant HW. Small bowel obstruction due to adhesions following neonatal laparotomy. Pediatr Surg Int . 2006;22:729–732. doi: 10.1007/s00383-006-1719-3. [DOI] [PubMed] [Google Scholar]
- 6.Uba AF, Chirdan LB, Ituen AM, Mohammed AM. Typhoid intestinal perforation in children: a continuing scourge in a developing country. Pediatr Surg Int. 2007;23:33–39. doi: 10.1007/s00383-006-1796-3. [DOI] [PubMed] [Google Scholar]
- 7.Parker MC, Ellis H, Moran BJ, Thompson JN, Wilson MS, Menzies D, McGuire A, Lower AM, Hawthorn RJ, O’Brien F, Buchan S, Crowe AM. Postoperative adhesion: ten year follow-up of 12584 patients undergoing lower abdominal surgery. Dis Colon Rectum. 2001;44:822–830. doi: 10.1007/BF02234701. [DOI] [PubMed] [Google Scholar]
- 8.Grant HW, Parker MC, Wilson MS, Menzies D, Sunderland G, Thompson JN, Clark DN, Knight AD, Crowe AM, Ellis H. Adhesions after abdominal surgery in children . J Pediatr Surg. 2008;43:152–157. doi: 10.1016/j.jpedsurg.2007.09.038. [DOI] [PubMed] [Google Scholar]
- 9.Akgur FM, Tanyel FC, Buyukpamukcu HI. Adhesive small bowel obstruction in children: the place and predictors of success for conservative treatment. J Pediatr Surg . 1991;26:37–41. doi: 10.1016/0022-3468(91)90422-p. [DOI] [PubMed] [Google Scholar]
- 10.Vijay K, Anindya C, Bhanu P, Mohan M, Rao PL. Adhesive small bowel obstruction (ASBO) in children-role of conservative management. Med J Malaysia. 2005;60:81–4. [PubMed] [Google Scholar]
- 11.Fazio VW, Ziv Y, Church JM, Oakley JR, Lavery IC, Milsom JW, Shroeder TK. Ileal pouch-anal anastomosis complications and function in 1005 patients. Ann Surg. 1995;222(2):120–127. doi: 10.1097/00000658-199508000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]


