Abstract
Background
Ketamine is a common anaesthetic agent for surgical procedures in both paediatric and adult populations in our environment. In polytraumatised patients its cardio-stimulatory effects may be advantageous in supporting the cardiovascular system while awaiting the clinical effects of on-going resuscitative interventions. However, its clinical uses cause significant cardiovascular stimulations that may be deleterious in patients with cardiovascular diseases.
Aim & Objectives
To evaluate the stimulatory effects of ketamine on cardiovascular system following induction of anaesthesia with ketamine.
Study design
This was a prospective observational study of the haemodynamic responses of 52 consenting patients who underwent surgery surgeries under general anaesthesia with ketamine induction. The pulse rate and blood pressure were measured non-invasively and recorded every minute for ten minutes following ketamine induction.
Setting
University of Ilorin Teaching Hospital, Ilorin, Nigeria.
Materials & Methods
Following approval of the Institutional Ethical Review committee, 52 consenting adult patients scheduled for surgery under general anaesthesia were premedicated with 10mg oral diazepam 90 minutes before the ketamine (2mg/kg intravenously) was intravenously administered as induction of anaesthesia.
The pulse rate (PR) and mean arterial pressure (MAP) were measured non-invasively and recorded at 1 minute interval over 10 minutes after the induction of anaesthesia with intravenous ketamine 2mg/kg while the patients breathed 100% oxygen spontaneously.
Results
In the 52 patients studied, the values of pulse rate (PR), systolic blood pressure (SBP), diastolic blood pressure (DBP) and mean arterial pressure (MAP) were significantly elevated above the baseline values by 22±14bpm, 15±11mmHg, 19±15mmHg, and 12±10mmHg respectively, with p=0.0001.
Conclusion
Ketamine induction of general anaesthesia exerts beneficial stimulatory effects on the cardiovascular system.
Keywords: Ketamine, Cardiovascular stimulations at induction, Nigeria, Ilorin
Introduction
Ketamine, 2-(o-chlorophenyl)-2-(methylamine) cyclohexanone, a phencyclidine (PCP) and cyclohexamine derivative, was developed and introduced into clinical anaesthesia by Corssen and Domino in 19661. It is an intravenous induction agent producing a unique dissociative anaesthetic state characterized by a dissociation between the thalamocortical and limbic systems2. It produces profound analgesia, normal pharyngeal-laryngeal reflexes, normal or slightly enhanced skeletal tone, and respiratory stimulation and occasionally transient and minimal respiratory depression2.
Ketamine is a non-competitive antagonist of the N-Methyl-D-Aspartate receptor (NMDA receptor), a cation-gated channel receptor permeable primarily to calcium and to a lesser extent to sodium and potassium. This receptor is involved in sensory input at the spinal, thalamic, limbic, and cortical levels2.
Ketamine blocks sensory input and reuptake of catecholamines and impairs limbic functions. It stimulates opioid sigma receptors, alpha- and beta- adrenergic receptors and antagonizes muscarinic receptors of the central nervous system3. In recent time, ketamine is generating new interest with wide spectrum of applications in anaesthesia, pain management, and other clinical specialties4,5,6. It has a proven neuro-protection against ischaemic brain injury and glutamate-induced brain injury4. It is also considered a drug of choice for treating acute and chronic pain7,8 and management of depression7,8.
It is a common anaesthetic agent in our environment. In many private and general hospitals in Nigeria, surgical procedures are done under ketamine anaesthesia administered, in some cases, by non-anaesthetist9,10. Although ketamine has a reputation for easy administration and documented safety profile in the hands of non-anaesthetists,10,11 the drug is frequently misused, sometimes with disastrous cardiovascular consequences12,13. Ketamine causes a significant increase in heart rate and arterial blood pressure via central and peripheral mechanisms14 hence it is contraindicated in patients with raised intra-cranial pressure, hypertension, cardiac or coronary artery disease. Fatal heart failure and/or acute myocardial infarction may occur during the peri-operative period when ketamine is used in these patients15. Though ketamine causes some direct myocardial depression at higher doses, haemodynamic stability may be maintained in hypovolaemic patients due to its sympathomimetic actions15. Emergence and excitatory phenomena are important adverse effects experienced by patients after ketamine administration which are usually counteracted by benzodiazepines.
Thus, the known and re-emerging clinical uses of this anaesthetic agent impresses on the anaesthetist the need to establish the degree of stimulation of haemodynamic parameters following ketamine administration. This requires a sound understanding of its pharmacodynamic properties which will ensure the safety of patients.
This prospective observational study was carried at the University of Ilorin Teaching Hospital, Ilorin, Nigeria over a period of six months on 52 adult consenting patients who underwent surgical procedures under general anaethesia using ketamine as an induction agent.
Reports
PATIENTS AND METHODS
Following approval from Institutional Ethics Committee and study-specific informed consent, 68 ASA physical statuses I-II (18-60years) scheduled for elective general, plastic and gynaecologic surgical procedures under general anaesthesia at the University of Ilorin Teachng Hospital, Ilorin, Nigeria over a period of six months were enrolled into the study.
Exclusion criteria were: hypertensive patients, patients with raised intra-ocular and intra –cranial pressures, patients with psychiatric and endocrine problems, patients with seizure disorders and myocardial ischemia and/ or infarction. Others excluded from the study include patients in whom face mask ventilation was anticipated to be difficult, patients with ASA classification physical status greater than class II and patients who refused to participate in the study.
Patients were assessed the night before the operation and their resting pulse rate (PR), systolic blood pressure (SBP), diastolic blood pressure (DBP) and mean arterial pressure (MAP) values were recorded. Patients’ socio-demographic characteristics including the age, sex, height and weight were documented. Pharmacologic side effects of induction of anaesthesia with ketamine were explained to the patient. Informed consent was obtained from all patients. The subjects were given 10mg oral diazepam the night before the surgery, and then fasted overnight. On the morning of the surgery about 90 mins before induction, patients were pre-medicated with 10mg oral diazepam. All medications were served by a trained assistant who did not take further part in the administration of anaesthesia.
In the operating room, basic checks on the anaesthetic machine and equipment were done and the patients were connected to the multi-parameter patient monitor, Nellcor Puritan Bennett Model 4000, (Pleasanton, CA 94588, U.S.A). With the patients in supine position, the values of baseline PR, SBP, DBP, MAP and SPO2 were measured and recorded. Intravenous access was secured with an 18-gauge cannula on a forearm vein for drug and fluid administrations. Isotonic NaCl solution was infused at 20 drops per min for the first 10 minutes which constituted the study period. The patients were pre-oxygenated with 100% oxygen for five minutes and anaesthesia was induced with 2mg/kg of ketamine (50mg/ml, ketamine hydrochloride injection, ROTEXMEDICA, TRITTAU, GERMANY) and patients were allowed to breathe, spontaneously, 100% oxygen at flow rate of 8L/min via the face mask connected through a Bain’s breathing system to the anaesthetic machine. The HR, SBP, DBP, MAP and SPO2 values were monitored non-invasively using the multi parameter patient monitor every minute for ten minutes and this constituted the study period. The rest of the anaesthetic management was conducted according to our institution’s protocol of general anaesthetics with attention to patient safety.
Data generated from this study were expressed as absolute figures, percentages, means and standard deviations. The post induction haemodynamic values of PR, SBP, DBP and MAP were analyzed at 1 minute interval for 10 minutes. The computer software package, Epi-info version 2002 was used for statistical analysis of data. Continuous variables were compared using student t-test and a p-value of less than 0.05 was considered statistically significant.
RESULTS
A total number of 52 consenting patients were formed the basis of this study. Their age range was 18 – 60 years with a mean age of 40.6±12.1 years. Males constituted 42.3% of the total patients with a male to female ratio of 2.2:3.
The baseline values of PR, SBP, DBP and MAP were significantly increased when compared with their corresponding resting values (93±13 vs 86±8, p<0.003), (130±1 vs 124±10, p<0.009), (82±8 vs78±7, p<0.008), and (98±8 vs 93±7, p<0.005) respectively as shown in Table 1. These increases were noticed at every succeeding minute and peaked by the fifth minutes followed by a progressive decline.
The values of the haemodynamic parameters measured at 5 minutes post induction of anaesthesia were not statistically different when compared with the baseline values as shown in Tables 2. However, there was a statistically significant elevation in the value of mean arterial pressure (MAP) 10 minutes post induction when compared with the corresponding baseline value (p<0.02) as shown in Table 3 .
The absolute degree of changes of the PR, SBP, DBP and MAP values from the baseline were 22±14bpm, 19±15mmHg, 12±10mmHg and 15±11mmHg respectively as shown in Table 4. The values of peak MAP and PR were 120±13mmHg and 125±17bpm, increases of 22mmHg (23%) and 32bpm (34%) above their baseline values respectively.
The values of mean % changes from baseline of PR, SBP, DBP, and MAP increased steadily from 1 to 4 min after ketamine induction in all the patients as shown in Figures 1 – 4 above. The RPP value in the study population was 17259±3201.
Conclusions
This study showed that a significant cardiovascular stimulation occurred within a few minutes following ketamine induction of anaesthesia. In view of this, the use of an anaesthetic adjunct that can antagonize this effect in susceptible patients is recommended to prevent the deleterious effects of ketamine.
Discussion
The average peak increases of 34% in the pulse rate (PR), 22% in the systolic blood pressure (SBP), 24% in the diastolic blood pressure (DBP) and 23% in the mean arterial pressure (MAP) are the main findings in this study. These findings are comparable with the report of Virtue et al 16 in which 34% increase in PR and 23% elevation in the MAP after induction of anaesthesia with 2.2mg/kg in adults were reported.
Kreuscher et al 17 on the other hand, reported increased PR of 38%, SBP of 26%, DBP of 33% and 30% increase in MAP from the baseline when adult patients were induced with 1.5mg/kg ketamine while Wilson et al 18 found increases in PR of 20%, SBP of 26%, DBP of 30% and MAP of 29% when 1mg/kg of ketamine was used in the paediatrics patients. The data obtained by these authors agree with the findings in our study. Though they both used lower induction doses of ketamine compared to our study, their patients also received anticholinergic agents (0.5mg/kg, 0.4mg/kg of atropine and 0.1mg/kg of scopolamine respectively) to prevent salivatory effects of ketamine. The anticholinergic agent employed for premedication by these two authors may have contributed to the slightly higher elevations in the haemodynamic variables they observed in their works when compared with the values in our study, where no anticholinergic drug was used. Glycopyrrolate, an anticholinergic that has little or no cardiac effect but effective secretion-drying property, could have been administered to patients in our study to prevent ketamine-induced secretions which if aspirated by the patients could affect gas exchange when the quantity is significant. Interestingly, the values of most of the haemodynamic parameters obtained in our study are higher than the data observed by Traber and associates19 who induced anaesthesia in dogs with 5mg/kg of ketamine. They found significant cardiovascular stimulations of 36% PR, 10% SBP, 17% DBP and 14% MAP above baseline values. This is in support of their opinions that ketamine was seen to have consistently produced a greater pressor response in humans than was observed in animals.
Similarly, our findings are consistent with the findings of Marlow et al20 who reported a 25% high incidence of adverse haemodynamic response to intubation in patients with high baseline BP (MAP ≥ 100mmHg) and Ramsubramanian et al21 who detected significant increases in PR and MAP. The two researchers premedicated their patients with iv midazolam before ketamine induction as was done in our study.
The calculated RPP obtained (17259±3201) is well above the acceptable value of <15,000 that is generally considered safe for patients with ischaemic heart disease for surgical procedures under general anaesthesia. This high value further asserts the stimulations of cardiovascular system following induction of anaesthesia using ketamine.
Nevertheless, ketamine-induced cardiac stimulations could be advantageous in the management of severely-ill or septic shock patients as an anaesthetic as well as sedative agent due to its ability to elevate haemodynamic parameters and the suggested tendency to exert a protective anti-inflammatory effect against the sepsis process itself.22 However, the stimulations of cardiovascular system following ketamine induction of anaesthesia in haemodynamically-stable patient could cause transient hypertensive crisis that may lead to stroke, blindness, renal impairment, myocardial ischaemia or cardiac failure peri-operatively, thereby predisposing patients to high anaesthetic morbidity and mortality when used in susceptible patients.
This study revealed that stimulations of cardiovascular system, following ketamine induction of anaesthesia, occurred within the first four minutes. Thus the use of an anaesthetic adjunct that exerts antagonizing effects on the cardiovascular system may be necessary in the susceptible patients in whom ketamine induction of anaesthesia is being anticipated. In doing this, it is logical to administer an adjunct which its onset and duration of actions will be comparable to that of ketamine or whose terminal part of its duration of action will extend into the earlier part of ketamine onset of action, the critical period. Some drugs like propranolol and clonidine have demonstrated pharmacologic properties of reducing the heart rates and can therefore be safely used as anaesthetic adjuncts during ketamine anaesthesia to obtund the ketamine-induced cardiovascular stimulation.
There are some limitations encountered while conducting this study and these included the induction of anaesthesia, in few of the patients, more than 90 minutes after the oral clonidine premedication due to delays resulting from logistics. Another challenge was the frequent one-minute interval recordings of the haemodynamic parameters for ten minutes.
Table 1. Changes in haemodynamic parameters with ketamine induction of anaesthesia
| Parameters | Resting | At induction (baseline) | % change | t-test | p value |
| PR | 86.4 (8.1) | 93.4 (12.5) | 8 | 3.19 | 0.003 |
| SBP | 123.5 (10.1) | 129.6 (10.6) | 5 | 2.57 | 0.009 |
| DBP | 77.9 (6.6) | 82.1 (8.0) | 5 | 3.40 | 0.008 |
| MAP | 93.1 (7.0) | 97.8 (8.3) | 5 | 2.83 | 0.005 |
| Values are expressed as mean ± SD |
Table 2. Comparison of haemodynamic parameters before and at 5minutes post ketamine induction
| Parameters | Mean at Baseline | Mean at 5 mins | t-test | p value |
| HRSBPDBPMAP | 93.4 (12.5)129.6 (10.6)82.1 (8.05)97.8 (8.3) | 125.4 (16.8)154.8 (21.5)95.6 (11.3)115.2 (13.6) | 1.620.881.310.84 | 0.190.640.250.67 |
| Values are expressed as mean ± SD |
Table 3. Comparison of haemodynamic parameters before and at10 minutes post ketamine induction
| Parameters | Mean at Baseline | Mean at 10 mins | t-test | p value |
| HRSBPDBPMAP | 93.4 (12.5)129.6 (10.6)82.1 (8.05)97.8 (8.3) | 107.7 (14.0)139.5 (17.5)87.1 (12.1)104.6 (12.7) | 1.391.841.542.38 | 0.230.080.150.02 |
| Values are expressed as mean ± SD |
Table 4. Comparison of haemodynamic parameters over a 10-minute post induction
| Parameters | Baseline | Degree of change from baseline | % change |
| PR | 93.1 (12.5) | 22(14) | 24 |
| SBP | 126.6 (10.6) | 19(15) | 15 |
| DBP | 82.1 (8.0) | 12(10) | 15 |
| MAP | 97.8 (8.3) | 15(11) | 15 |
| Values are expressed as mean ± SD and percentages |
Figure 1.

Change in mean pulse rate over a 10 minutes period following induction of anaesthesia with ketamine
Figure 2.
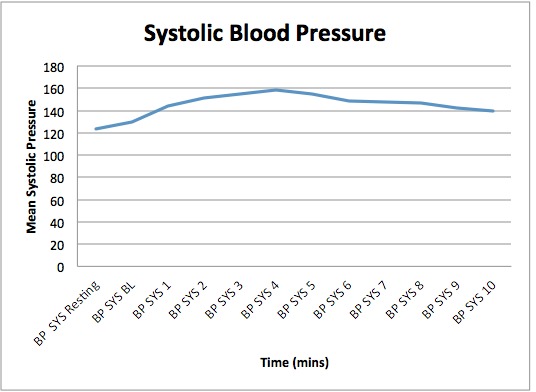
Change in mean systolic blood pressure over a 10 minute period after induction of anaesthesia with ketamine
Figure 3.
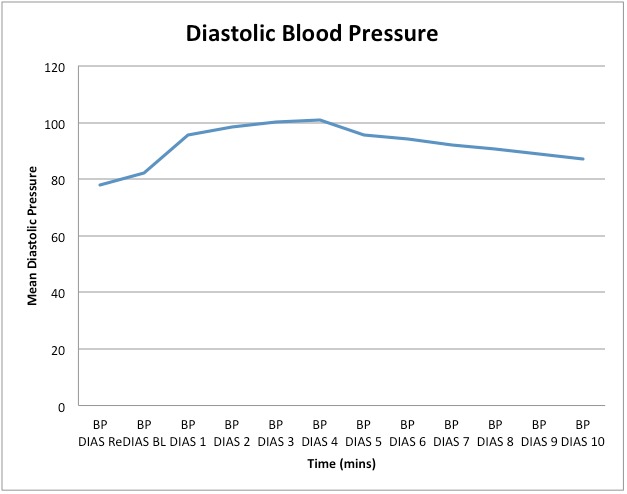
Change in mean diastolic blood pressure over a 10-minute period following induction of anaesthesia with ketamine
Figure 4.
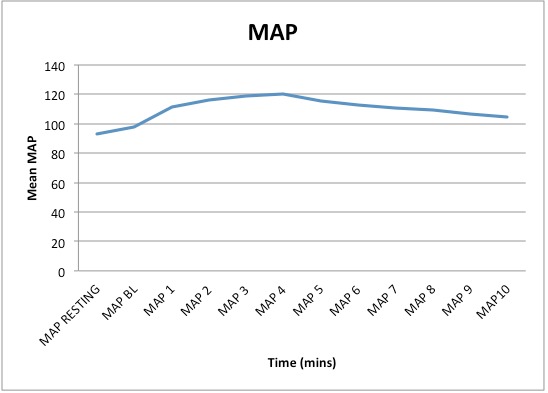
Change in mean arterial pressure over a 10-minute period following induction of anaesthesia with ketamine
Acknowledgment
We wish to thank Dr A.A. Nasir for critiquing the manuscript before submission for publication. Also worthy of acknowledgement are the residents and other staff of the Dept of Anaesthesia, University of Ilorin Teaching Hospital, Ilorin.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Grant support: None
References
- 1.Kolawole IK. "Ketamine Hydrochloride: A Useful but Frequently Misused Drug". Niger J of Surg Res . 2001; 3:118–125.. [Google Scholar]
- 2.Yoon Seok. Concerns of the anaesthesiologist: anaesthetic induction in severe sepsis or septic shock patients. Korean J Anesthesiol . 2012; 63(1):3–10. doi: 10.4097/kjae.2012.63.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adesunkanmi ARK. "Ketamine anaesthesia". Niger J of Surg Sci. 1993;;3:36–38. [Google Scholar]
- 4.Colligride GL, Singer W. "Excitatory amino acid receptors and synaptic plasticity.". Trends Pharmacol Sci. 1990;11:290–296. doi: 10.1016/0165-6147(90)90011-v. [DOI] [PubMed] [Google Scholar]
- 5.Kolawole IK. "Misuse of Ketamine : Report of two cases". Niger J of Surg Res. 2001;;3::175–180. [Google Scholar]
- 6.Megafu U. "Short-acting agents for minor surgery for a single-handed Gynaecologist". West Afr J. Med. 1985;5:235–238. [Google Scholar]
- 7.Corssen G, Domino EF. Dissociative anaesthesia: Further Pharmacologic studies and first clinical experience with the phencyclidine derivative C1-581. Curr Res Anesth Analg. 1966;45:29–29. [PubMed] [Google Scholar]
- 8.Stewart AB. "Ketamine: Review of Its Pharmacology and Its Use in Paediatric Anaesthesia". Anaesth Prog. 1999;46:10–20. [PMC free article] [PubMed] [Google Scholar]
- 9.Shibuta S, Varathan S, Mashimo T. "Ketamine and thiopental sodium: individual and combined neuroprotective effects on cortical cultures exposed to NMDA or nitric oxide". Br J Anaesth. 2006;97:517–524. doi: 10.1093/bja/ael192. [DOI] [PubMed] [Google Scholar]
- 10.Elia N, Tramer M. "Ketamine and postoperative pain- a quantitative systematic review of randomized trials". Pain. 2005;;113:61–70.. doi: 10.1016/j.pain.2004.09.036. [DOI] [PubMed] [Google Scholar]
- 11.Saito O, Aoe T, Kozikowski A, Sarva J, Neale J, Yamamoto T. "Ketamine and N-acetyl aspartyl glutamate peptidase inhibitor exert analgesia in bone cancer pain". Can J Anaesth. 2006;;53:891–898. doi: 10.1007/BF03022832. [DOI] [PubMed] [Google Scholar]
- 12.Correll GE, Futter GE. Two case studies of patient with major depressive disorder given low dose (sub-anaesthetic) ketamine infusions. Pain Med . 2006;7:92–95. doi: 10.1111/j.1526-4637.2006.00101.x. [DOI] [PubMed] [Google Scholar]
- 13.Berman R. Antidepressant effects of ketamine in depressed patients. Biol Psychiatry. 2000;;47:351–354. doi: 10.1016/s0006-3223(99)00230-9. [DOI] [PubMed] [Google Scholar]
- 14.Soliman MG, Brinale GF, Kuster G. "Response to hypercarbia under ketamine anaesthesia". Can Anaesth Soc J. 1975;22:486–486. doi: 10.1007/BF03004864. [DOI] [PubMed] [Google Scholar]
- 15.White PF, Way WL, Trevor AJ. "Ketamine: its pharmacological and therapeutic uses.". Anesthesiology. 1982;56::119–136. doi: 10.1097/00000542-198202000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Russel C. In: Avoiding Common Paediatric Errors. Lippincott and Williams: 2008. "Give ketamine in patients with significant cardiac disease or sepsis". [Google Scholar]
- 17.Virtue RW, Alanis JM, Mori M, La-Fargue RT, Vosel JH, Metcalf DR. "An Anaesthetic Agent: 2-(0-chloropyhenyl)-2-(methylamino) cyclohexanone Hcl (CI581) Anesthesiology. 1967;28:823–823. doi: 10.1097/00000542-196709000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Kreuscher H, Gauch H. "Die Wirkung des phencyclidin derivates ketamine (CI 581) auf des cardiovasculaere system des Menschen.". Anaesthetist. 1967;16:229–229. [PubMed] [Google Scholar]
- 19.Wilson RD, Traber DL, McCoy NR. "Cardiopulmonary effects of CI-581, The New Dissociative Anaesthetic". Southern Med. J. 1968;;61:692–692. doi: 10.1097/00007611-196807000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Traber DL, Wilson RD, Priano LL. "Differentiation of the cardiovascular effects of C1-581". Anesth Analg. 1968;47:769–777.. [PubMed] [Google Scholar]
- 21.Marlow R, Reich DL, Neustein S, Silvary G. "Haemodynamic responses to induction of anaesthesia with ketamine/midazodam". Can J Anaesth. 1991;;33:844–848. doi: 10.1007/BF03036958. [DOI] [PubMed] [Google Scholar]
- 22.Ramsubramanian R, Rawle PR, Verma R. "Attenuation of psychological effects of ketamine anaesthesia by midazodam: a dose response study". Anaesth Analg. 1989;68:231–231. [Google Scholar]


