Abstract
Background
Congential diaphragmatic herniae pose serious challenges in their management in this environment.Aim & Objective: To determine the pattern, as well as the diagnostic and management challenges of congenital diaphragmatic hernia in Dakar, Senegal.
Patients and Methods
This is a retrospective review of 14 children with congenital diaphragmatic hernia (CDH) managed within eleven years in Dakar, Senegal. Results: There were nine boys and five girls with the age range of one day to 22 months and a mean of 5 months. Respiratory signs (respiratory distress, cough, current pulmonary infection) were found in 13 patients and gastrointestinal symptoms (vomiting, Difficulty sucking, anorexia) in 6 patients. The thoracic-abdominal radiography was performed in all patients and revealed a Bochdalek hernia on the left in 10(71%) cases and 4(29%) were Morgagni hernia. Treatment was by repair of the diaphragmatic defect with non-absorbable sutures. The postoperative course was uneventful in 13 children while one patient died on the first postoperative day one.
Conclusion
Congenital diaphragmatic hernia presents mainly with postnatal respiratory features in this setting. Thoracic-abdominal radiography allows for early diagnosis, prompt and effective treatment with good outcome.Keywords: Congenital diaphragmatic hernia, Respiratory insufficiency, Radiological features, Good surgical outcome.
Keywords: Congenital diaphragmatic hernia, Respiratory insufficiency, Radiological features , Good surgical outcome
Introduction
Congenital diaphragmatic hernia (CDH) is characterized by a lack of closure of diaphragm associated with the development of some of the abdominal viscera into the thorax 1. This is a relatively uncommon malformation (1 in 3,000 to 5,000 births by the series) 2. Congenital diaphragmatic hernia can have two locations in the hernia defect: the hernia retro-costo-xyphoïdian or Morgagni hernia and posterolateral Bochdalek that is the most frequent responsible for 80% of the cases 3. Clinical diagnosis is difficult because of the absence of unique symptomatology pattern4, 5. The aim of our study was to report the diagnostic and therapeutic challenges in our service as well as compare the results with those from other workers elsewhere.
Reports
Patients and Methods
In the period January 2001 and December 2011, 14 children with congenital diaphragmatic hernia (CDH) were managed at the Department of Paediatric Surgery, Aristide Le Dantec Hospital in Dakar, Senegal. Their hospital records including demographics, clinical features, treatment offered and outcome were obtained retrospectively and entered in a proforma, and the data obtained were analyzed. We have excluded from this study all incomplete files of congenital diaphragmatichernia. ResultsThere were nine (64,2 %) boys and five (35,8 %) girls aged between one day and 22 months with a mean of 5 months. The main clinical features were respiratory and were found on 13 patients. They belonged to a respiratory distress type (6 cases), bronchus infections repeated (5cases) and cough (3cases). Digestif signs were found on 6 patients. It was about vomiting (6cases), anorexia (2cases) and transit disorders (2cases). Chest x-ray suggested the diagnosis in all patients as shown in Figure 1, showing intrathoracic intestines as well as a Bochdalek hernia all on the left side in 10 cases and Morgagni hernia in 4 cases.
Thoracic-abdominal ultrasound was performed in two children which identified the contents of the hernia. Barium swallow was performed in one patient and showed ascent of stomach in "E" shape as shown in Fig. 2. Dopplar echocardiography was done in one patient to exclude pericardial effusion. Two patients required preoperative resuscitation for 24 to 72 hours.
Surgical correction was done using the abdominal approach - transverse incision was used in 10 patients while upper midline incision was used in 4 patients. A hernia sac was present in ten children and absent in 4 children. The size of the diaphragmatic defect was 4cm - 13cm with a mean of 9cm as shown in Fig. 3. The colon alone was herniated in 4 cases, small intestine in 3 cases, liver in 1 case, and the spleen in 1 case. Multiple organs were herniated in 5 cases. The defect was repaired by interrupted suturing using non-absorbable suture in 12 patients and continuous suturing in 2. A chest tube with underwater seal drainage was necessary in 8 patients. In one patient, a ventral hernia was created on the abdomen in order to accommodate the reduced viscera and to prevent a compartment syndrome; the ventral hernia was repaired 18 months later. All patients were admitted to intensive care for 48 hours before being transferred to the general ward. In all, two patients needed mechanical ventilation to recover from cardio-respiratory insufficiency.
Chest tube was removed after 1-4 days. The postoperative course was uneventful in 13 patients and the hospital stay was 6-24 days with a mean of 10 days. A 2-day old baby died on the first postoperative day one from respiratory insufficiency.
Conclusions
Congenital diaphragmatic hernia presents mainly with postnatal respiratory features in this setting. Thoracic-abdominal radiography allows for early diagnosis, prompt and effective treatment with good outcome.
Discussion
The diagnosis of congenital diaphragmatic hernia can be done either prenatally by ultrasonography, or shortly after birth as a result of neonatal respiratory distress2, 6, 7, 8, 9, 10.Respiratory distress and recurrent pulmonary infections are the commonest presenting symptoms which are consistent with the findings of other workers11,12,13,14,15,16. In our series the chest x-rays were used to diagnose congenital diaphragmatic hernia. It’s often enough to make a diagnosis but in certain cases a scan, a digestive opacificatin or an echography can be necessary15, 16.The surgical treatment is the treatment of choice after ensuring cardio-respiratory stability. The surgical approach could be via laparotomy, laparoscopy or thoracoscopy 17,18,19. Currently thoracoscopic repair is the preferred choice of treatment with the best outcome with reduced morbidity 20 but in this series, laparostomy was performed for all the patients. The treatment included exploration of the abdominal cavity, reduction of the herniated viscera and repair of the diaphragmatic defect with non-absorbable sutures as is the practice with other reports in literature 21,22. Closure of the abdominal wall should be without tension 17,19,23. The treatment outcome was good in 13 of the children operated; one patient died on the first post-operative day as a result of respiratory insufficiency one death was noted on day 1 postoperatively. In the study by Coste et al 12, the postoperative course was uneventful in the first case but the other was complicated with intussusception which required reoperation. The same situation has been reported in the work of Sahnoun 14. Gischler et al 24 conducted a prospective longitudinal study in pediatric hospitals to compare long-term respiratory morbidity in children with congenital diaphragmatic hernia. Ten of the 20 patients with congenital diaphragmatic hernia in that study developed bronchopulmonary dysplasia. So it is important that the monitoring of respiratory system of patients even after repair of congenital diaphragmatic hernia should continue for up to one year after the repair.
Fig 1.
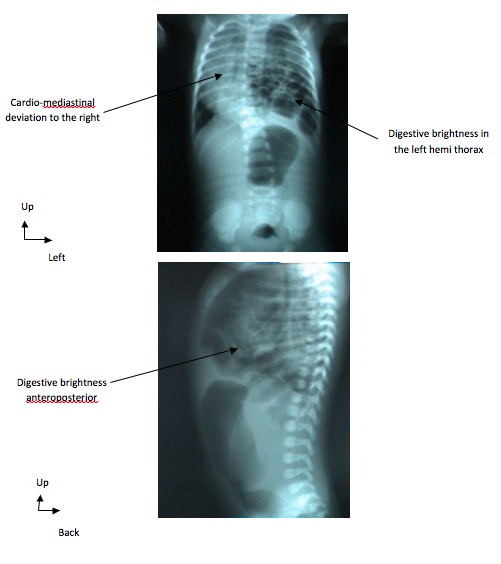
Thoraco-abdominal x-rays showing a left diaphragmatic hernia/ Radiographies thoraco-abdominales montrant une hernie diaphragmatique gauche
Fig 2.

Barium swallow showing diaphragmatic hernia/ Le transit baryté montrant une hernie diaphragmatique
Fig 3.

Preoperative image showing the herniated stomach and intestines/ Image per opératoire montrant l'estomac et des intestins herniés
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Grant support: None
References
- 1.Bargy F. Malformation of diaphragm. Handbook of Pediatric Surgery Paris. 1998. pp. 250–254..
- 2.Galifer RB. Treatment of hernia diaphragmatic dome.; Neonatal surgery visceral, eleventh national education seminar.Grenoble: 1992. pp. 257–264.. [Google Scholar]
- 3.Mitanchez D. Prenatal treatment of diaphragmatic hernia dome. Arch Pediatr. 2008;15:1320–1325. doi: 10.1016/j.arcped.2008.04.034. [DOI] [PubMed] [Google Scholar]
- 4.Chardot P, Montupet P. Encyclopedia medical-surgical (Elsevier SAS), Surgical Techniques Digestive. Paris: 2006. Diaphragmatic hernia child 2006. pp. 40–255.. [Google Scholar]
- 5.Saada J, Parat S, Delahaye S, Bourbon J, Benachi A. Dome diaphragmatic hernia. Encycl Med Chir (Scientific and Medical Publishing Elsevier SAS, Paris, all rights reserved) Gynaecology / Obstetrics. 2007;5:30–31. [Google Scholar]
- 6.Storme L, Pennaforte T, Raza T, Aubry E, Pennaforte T, Bonnevalle M. Medical care and postnatal by the congenital hernia of diaphragm. Arch Pediatr. 2010;17:85–92. [Google Scholar]
- 7.Vedel-werts F, Desandes R, Rouabah M, Bach PG, De Miscault J, Hascoet M, Hamon I. Right diaphragmatic hernia and neonatal sepsis secondary to Streptococcus β in a premature revelation. Arch Pediatr. 2007;14:897–899. doi: 10.1016/j.arcped.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 8.Garcia-Munoz F, Santana C, Reyes D, Wiehoff A, López-Pinto JM, García-Alix A. Early sepsis, obstructive jaundice and right-sided diaphragmatic hernia in the newborn. Acta Pediatr. 2001;90:96–98. [PubMed] [Google Scholar]
- 9.Vachharajani AJ, Shah JK, Paes BA. Late-onset left diaphragmatic hernia aftergroup β streptococcal sepsis, an unusual presentation. J Pediatr Surg. 2002;37:932–933. doi: 10.1053/jpsu.2002.32918. [DOI] [PubMed] [Google Scholar]
- 10.Banagale RC, Watters JH. Delayed right-sided diaphragmatic hernia Following group β streptococcal infection: a focus icts of pathogenesis, with a review of the literature. Hum Pathol. 1983;14:67–69. doi: 10.1016/s0046-8177(83)80047-1. [DOI] [PubMed] [Google Scholar]
- 11.Handa N, Suita S, Shono T, Kukita J. Right-sided diaphragmatic hernia Following group β streptococcal pneumonia and sepsis. J Pediatr Surg. 1992;27:764–766. doi: 10.1016/s0022-3468(05)80112-5. [DOI] [PubMed] [Google Scholar]
- 12.Shima H, Ohshiro K, Taira Y, Miyazaki E, Oue T, Puri P. Antenatal dexamethasone Suppresses tumor necrosis factor-alpha Expression in hypoplastic development in nitrofen-induced diaphragmatic hernia in rats. Pediatr Res. 1999;46:633–637. doi: 10.1203/00006450-199911000-00023. [DOI] [PubMed] [Google Scholar]
- 13.Coste C, Jouvencel P, Debuch C, Argote C, Lavrand F, Feghali H. Congenital diaphragmatic hernia late onset: diagnostic difficulties (about two cases) Arch Pediatr. 2004;11:929–931. doi: 10.1016/j.arcped.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 14.Bonnet JP, Louis D. Intrathoracic volvulus of the spleen revealing left posterolateral diaphragmatic hernia. Arch Pediatr. 1996;3:701–704. doi: 10.1016/0929-693x(96)87094-1. [DOI] [PubMed] [Google Scholar]
- 15.Sahnoun L, Ksia A, Jouini R, Maazoun K, Mekki M, Krichene I. The rétrocosto-xiphoidiennes hernias in children: report of seven cases. Arch Pediatr. 2006;13:1316–1319. doi: 10.1016/j.arcped.2006.06.027. [DOI] [PubMed] [Google Scholar]
- 16.Wu CT, Huang JL, Hsia SH, Lin JJ, Lai SH. Late-presenting congenital diaphragmatic hernia in the pediatric emergency room: two case reports. EUR J Pediatr Surg. 2009;168:1013–1015. doi: 10.1007/s00431-008-0874-z. [DOI] [PubMed] [Google Scholar]
- 17.Laarif A. Congenital diaphragmatic hernia (About 15 cases). Thesis Medicine Rabat. 2007. pp. 40–40.
- 18.Bohn D. ongenital Diaphragmatic Hernia Bohn. Am J Respir and Crit Care Med. 2002;166:911–915. doi: 10.1164/rccm.200204-304CC. [DOI] [PubMed] [Google Scholar]
- 19.Moyer V, Moya F, Tibboel R, Losty P, Nagaya M, Lally KP. Late versus early surgical corrections for congenital diaphragmatic hernia in newborn infants. Cochrane database system rev. 2002;3:1695–1695. doi: 10.1002/14651858.CD001695. [DOI] [PubMed] [Google Scholar]
- 20.Dubois A, Storme L, Jaillard S, Truffert P, Riou Y, Rakza T. Domes of congenital diaphragmatic hernia. Retrospective study of 123 observations collected in neonatal medicine service you Lille University Hospital between 1985 and 1996th. Arch Pediatr. 2000;7:132–142. doi: 10.1016/s0929-693x(00)88082-3. [DOI] [PubMed] [Google Scholar]
- 21.Becmeur F, North M, Dhaoui R, De Billy B, Calvert JM, Lutz P. Videosurgery in children and diaphragmatic hernia. Memoirs of the National Academy of Surgery. 2008;7:50–54. [Google Scholar]
- 22.Favre JP, Hagry O, Chenel N. Encyclopedia medical-surgical Scientific and Medical Publishing Elsevier. Surgical techniques Digestive. Paris: 2002,. Rare surgical treatment of diaphragmatic hernia. pp. 240–247.. [Google Scholar]
- 23.Deprest J, Kohl T, Gembruchm U, Tchatchevam K, Schaible T. Current consequences of prenatal diagnosis of congenital diaphragmatic hernia. J Pediatr Surg. 2006;41:423–30.. doi: 10.1016/j.jpedsurg.2005.11.036. [DOI] [PubMed] [Google Scholar]
- 24.Gischler SJ, van der Cammen, van Zijp MH, Mazer P, Madern GC, Bax NM, de Jongste JC, van Dijk M. A prospective comparative assessment of persistent respiratory morbidity in esophageal atresia and congenital diaphragmatic hernia survivors. J Pediatr Surg. 2009;44:1683–1690. doi: 10.1016/j.jpedsurg.2008.12.019. [DOI] [PubMed] [Google Scholar]


