Abstract
Introduction: Ketamine is frequently abused nowadays as a recreational drug. Case reports are emerging since 2007 to describe a new clinical entity of severe bladder dysfunction associated with chronic abuse of street ketamine.
Clinical presentation: Severe lower urinary tract symptoms of urinary frequency and urgency which are refractory to conventional treatment. Quality of life is adversely affected as a consequence. Chronic kidney disease will develop in advanced cases.
Investigation findings: The urine is sterile on culture. Ultrasound will show reduced bladder capacity with thickened bladder wall. In advanced stage, hydronephrosis and renal impairment will develop.
Treatment: Patients should be advised to stop street ketamine use immediately. Anticholinergic medication could be tried to alleviate the symptoms. Refractory cases with dilatation of the upper urinary tract might need urinary diversion. Conclusion:
Awareness of this new condition is essential in diagnosis. Early intervention offers better treatment outcome.
Keywords: Ketamine, lower urinary tract symptoms, bladder dysfunction
INTRODUCTION
Ketamine, an N-methyl-D-aspartic acid receptor, is a commonly used anaesthetic agent in the operation theatre. However, it is also being abused as a recreational drug in parties, nightclubs, pubs and gatherings.1 There are several street name used for ketamine. These include: K, special K, super K, vitamin K, kit-kat, keets, super acid, jet and cat valiums.2 In recreational usage, ketamine is usually taken in powder form. It is smoked in a mixture of marijuana or tobacco, either taken intranasally2 or orally.3 The misuse of ketamine is widespread as there is a misconception that the drug is relatively safe compared to other illicit drugs such as morphine and heroin.4
There is now increasing news reports about smuggling of ketamine. The seizure of ketamine had multiplied from the usual 10-20 kg seized from air passengers to the current trend of hundred kilograms of ketamine being shipped through various sea ports in the country.5 Since 2007, case reports are appearing in the medical literature describing a form of severe haemorrhagic cystitis with debilitating bladder dysfunction which is linked to the abuse of ketamine. Among the first reported series were nine cases from Toronto, Canada.1 Chu PS et al from Hong Kong reported the largest series with 59 patients.6 In total, more than 70 cases had been reported to date (Table 1). In Malaysia, there had been anecdotal accounts of severe bladder dysfunction secondary to ketamine abuse among urological patients.
Table 1. Case reports on urinary tract dysfunction secondary to street ketamine abuse.
This review article aims to describe the clinical presentation and management of this new clinical entity. We also hope to create awareness among family physicians so that street ketamine associated bladder dysfunction could be considered in their differential diagnosis when faced with young patients who complain of lower urinary tract symptoms of frequency and urgency. A local Malaysian case will also be described to illustrate this clinical problem.
PSYCHOMOTOR MANIFESTATION OF KETAMINE ABUSE
The psychological effects of ketamine are brief, usually last for about 30 minutes.3 It can cause psychological dissociation, resulting in hallucinations and phenomena which may include subjective experiences of being out of the body or states similar to near death experience. Along with these ‘desired’ effects, users also commonly experienced confusion, anterograde amnesia and delirium.2 There may also be effects on movements. These include stereotypies (persistent repetition of acts or words), a severe loss of coordination, and pronounced analgesia.7 Many users also experienced an inability to speak, blurred vision and increased body temperature.8
Other effects include tachycardia, palpitation, hypertension and respiratory depression with apnoea.2 “Flashbacks” or visual disturbances can be experienced days or weeks after ingestion.9 Long term effects on frequent users include long-lasting impairments in episodic memory and aspects of retrieval from semantic memory.10 High doses of ketamine if being used for long term, also has the potential to interfere with learning and attentional mechanisms.11,12 These are due to blockade of the N-methy-D-aspartate receptor. Some chronic users may become addicted and exhibit severe withdrawal symptoms that require detoxification.2
UROLOGICAL MANIFESTATION OF KETAMINE ABUSE
Patients consistently present with severe lower urinary tract symptoms of urinary frequency and urgency. Some cases will have urge urinary incontinence, dysuria, gross haematuria and suprapubic pain.1,6 In advanced cases, the patients need to empty his/her bladder every 15 minutes. The quality of life is adversely affected with the patients being unable to continue with his/her daily activities. These urinary storage symptoms usually appear after long term ketamine abuse but could also appear in new ketamine abuser.13 There is equal distribution of cases between male and female in the reported literature (Table 1).
PATHOPHYSIOLOGY OF URINARY TRACT DAMAGE
The exact mechanism of ketamine causing urinary tract damage is unknown.6 However, it is believed to be caused by direct toxic effects of ketamine and its metabolites. This leads to submucosal oedema, inflammation, vascular ectasia and fibrosis of the detrusor muscles of the urinary bladder. It is postulated that intrinsic microcirculation of the subendothelium of the urinary tract is compromised as a result of ketamine abuse. Furthermore, an autoimmune reaction could also play a role in causing further damage to the urinary tract. In short, further investigation is needed to pinpoint the exact mechanism that leads to urinary tract damage by ketamine abuse.6
INVESTIGATION
The urine is sterile on culture.1 Imaging studies (ultrasound, CT scans or intravenous urogram) will show thickened bladder wall with small bladder capacity. There is also perivesical stranding signifying severe inflammatory changes of the bladder. In advanced cases, hydronephrosis will be present secondary to ureteric narrowing or strictures. Papillary necrosis of the kidneys had also been reported. Renal impairment with raised creatinine was observed in many of these cases.6
Urodynamic studies done in specialized urology centres revealed bladder detrusor muscles overactivity and decreased bladder compliance with or without vesico-ureteric reflux.6
Direct cystoscopic examination showed the picture of haemorrhagic cystitis with different degree of severity. Biopsies of the bladder revealed epithelial denudation and inflammation with eosinophilic infiltrate.1,6
MANAGEMENT
Effective management of this new condition remains elusive. The first thing the physician should do is to advise the patients to stop using ketamine. In patients with only short term ketamine exposure, where there is no permanent damage to the urinary tract, this simple measure is sufficed to alleviate the symptoms.13 For patients who failed to improve with cessation of ketamine abuse, anticholinergics could be used with the aim to reduce bladder detrusor muscle contraction. Common anticholinergics available are oxybutynin and tolterodine. However, in long term ketamine abusers, the symptomatic response to anticholinergics is disappointingly poor.6 Pentosan sulfate, a medication used to supplement the glycosaminoglycan layer of the urinary bladder, given intravesically had also been reported to be helpful in relieving the lower urinary tract symptoms.1
In advanced cases with upper urinary tract obstruction and renal impairment, temporizing measures to relieve the obstruction is indicated. This could be done either by double- J stenting of the obstructed ureter or percutaneous nephrostomy. Steroid had also been used to reduced the inflammation of the urinary tract.6
In cases refractory to the above measures, more drastic surgical procedures had been employed such as bladder augmentation6 or cystectomy with construction of neobladder.18 However, long term experience with these operative interventions is limited. One of the potential risks of incorporation of bowel into the urinary tract in such patients (in cases of bladder augmentation/clam cystoplasty or neobladder construction) might be reabsorption of ketamine or its metabolites. Should the patient continue to abuse ketamine after augmentation or construction of neobladder, reabsorption may lead to overdose. Multidisciplinary approach is essential in the management of patients with ketamine abuse. Failure to quit is often the reason for deterioration of the condition. Patient should be referred for counselling in order to properly deal with their drug addiction problem.
CASE ILLUSTRATION
A young gentleman, with renal failure (creatinine > 500 μmol/L) and deranged liver function test was admitted under the care of nephrologist and gastroenterologist. The urologist became involved when the ultrasound scan showed thickened bladder wall, bilateral hydronephrosis and hydroureter (Figure 1-Figure 3). He admitted to taking ‘K’. He was then stented and the creatinine normalised. On ultrasound scan, the hydronephrosis improved. The stents were removed after a few months and within a week the kidneys became hydronephrotic again. Therefore, the patient was stented again with long term stents.
Figure 1.
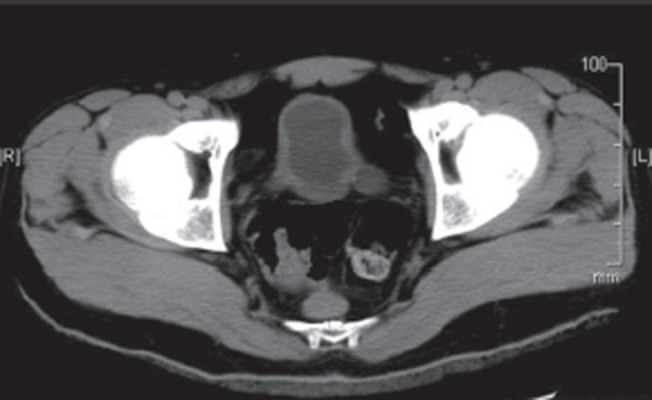
Thickened bladder wall with dilatation of the lower ureters.
Figure 3.
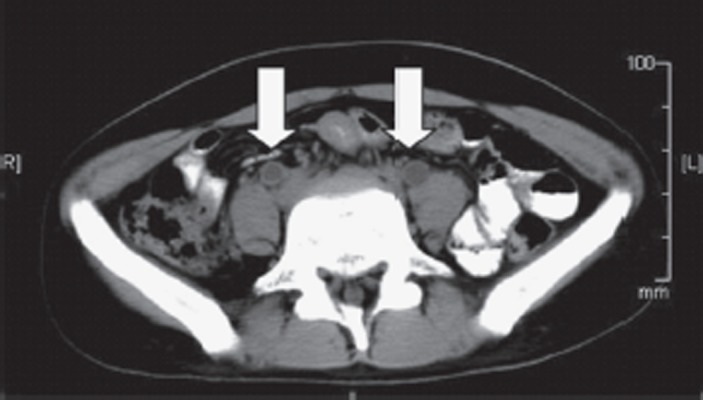
Bilateral hydroureter (white arrows).
Figure 2.
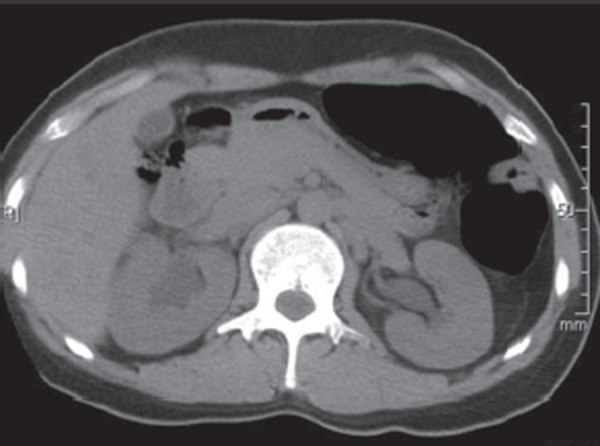
Bilateral hydronephrosis.
CONCLUSION
As abuse of ketamine becomes more rampant, as reflected by increase seizures of illicit ketamine by the police, the incidence of “ketamine bladder” will increase. Therefore, it is important for the frontline physicians to be aware of this new clinical entity. Diagnosing this condition early holds the key to satisfactory treatment outcome as current available treatment modalities are relatively ineffective in patients with established urinary tract damage. Multidisciplinary approach is essential in the management of patients with ketamine abuse. Patient should be referred for counselling in order to properly deal with their drug addiction problem and early referral to the urologist could facilitate the treatment of this debilitating condition.
ACKNOWLEDGEMENT
We would like to thank Dr Robert J Stewart for providing the information on the male:female distribution in his case series.1
Footnotes
Conflicts Of Interest
None
Source of funding
None
Two RCTs on PSA screening with conflicting results
PLCO trial failed to show mortality benefit of PSA screening
Andriole GL, Crawford ED, Grubb RL III, et al. Mortality results from a randomized prostate-cancer screening trial. N Engl J Med. 2009;360(13):1310-9
Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial: 76,693 men at 10 U.S. study centres to receive either annual screening PSA (with digital rectal exam) or usual care as the control. After 7 years of follow-up, more prostate cancers are detected in the screened group (RR=1.22; 95%CI 1.16 to 1.29) but the death rate in both similar is not statistically different (RR=1.13; 95%CI 0.75 to 1.70).
ERSPC trial showed mortality benefit of PSA screening
Schroder FH, Hugosson J, Roobol MJ,et al. Screening and prostate-cancer mortality in a randomized European study. N Engl J Med. 2009;360(13):1320-8
European Randomized Study of Screening for Prostate Cancer (ERSPC): 182,000 men in seven European countries was offered PSA screening 4-yearly or no screening. The predefined core age group for this study included 162,243 men between the ages of 55 and 69 years. During a median follow-up of 9 years, more prostate cancers are detected in the screened group (RR=0.80, 95%CI 0.65 to 0.98) and the death rate is also reduced in the screened group (RR=0.73, 95%CI 0.56 to 0.90).
References
- 1.Shahani R, Streutker C, Dickson B. et al. Ketamine-associated ulcerative cystitis: a new clinical entity. Urology. 2007;69((5)):810–2. doi: 10.1016/j.urology.2007.01.038. [DOI] [PubMed] [Google Scholar]
- 2.Gahlinger PM. Club drugs: MDMA, gamma-hydroxybutyrate (GHB), Rohypnol, and ketamine. Am Fam Physician. 2004;69((11)):2619–26. [PubMed] [Google Scholar]
- 3.Jansen KL. Non-medical use of ketamine. BMJ. 1993;306((6878)):601–2. doi: 10.1136/bmj.306.6878.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Patterns and trends of amphetamine-type stimulants (ATS) and other drugs of abuse in East Asia and the Pacific 2006. United Nations Office on Drugs and Crime Regional Centre for East Asia and the Pacific. 200793 [Google Scholar]
- 5. Bid to ship 100kg of ketamine to Malaysia foiled. The Star Online, 2009 March 1;Sect. News (col. Nation)
- 6.Chu PS, Ma WK, Wong SC. et al. The destruction of the lower urinary tract by ketamine abuse: a new syndrome? BJU Int. 2008;102((11)):1616–22. doi: 10.1111/j.1464-410X.2008.07920.x. [DOI] [PubMed] [Google Scholar]
- 7.White PF, Way WL, Trevor AJ. Ketamine‒its pharmacology and therapeutic uses. Anesthesiology. 1982;56((2)):119–36. doi: 10.1097/00000542-198202000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Dillon P, Copeland J, Jansen K. Patterns of use and harms associated with non-medical ketamine use. Drug Alcohol Depend. 2003;69((1)):23–8. doi: 10.1016/s0376-8716(02)00243-0. [DOI] [PubMed] [Google Scholar]
- 9.Freese TE, Miotto K, Reback CJ. The effects and consequences of selected club drugs. J Subst Abuse Treat. 2002;23((2)):151–6. doi: 10.1016/s0740-5472(02)00267-2. [DOI] [PubMed] [Google Scholar]
- 10.Curran HV, Monaghan L. In and out of the K-hole: a comparison of the acute and residual effects of ketamine in frequent and infrequent ketamine users. Addiction. 2001;96((5)):749–60. doi: 10.1046/j.1360-0443.2001.96574910.x. [DOI] [PubMed] [Google Scholar]
- 11.Jansen KL. Ketamine-can chronic use impair memory? Int J Addict. 1990;25((2)):133–9. doi: 10.3109/10826089009056204. [DOI] [PubMed] [Google Scholar]
- 12.Cotman CW, Monaghan DT, Ganong AH. Excitatory amino acid neurotransmission: NMDA receptors and Hebb-type synaptic plasticity. Annu Rev Neurosci. 1988;11:61–80. doi: 10.1146/annurev.ne.11.030188.000425. [DOI] [PubMed] [Google Scholar]
- 13.Tsai JH, Tsai KB, Jang MY. Ulcerative cystitis associated with ketamine. Am J Addict. 2008;17((5)):453. doi: 10.1080/10550490802266243. [DOI] [PubMed] [Google Scholar]
- 14.Chu PS, Kwok SC, Lam KM. et al. ‘Street ketamine’-associated bladder dysfunction: a report of ten cases. Hong Kong. Med J. 2007;13((4)):311–3. [PubMed] [Google Scholar]
- 15.Chen KT, Foo NP, Lin HJ. Frequent visits with urinary symptoms: subtle signs of ketamine abuse. Am J Emerg Med. 2008;26((9)):1061–2. doi: 10.1016/j.ajem.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 16.Colebunders B, Van Erps P. Cystitis due to the use of ketamine as a recreational drug: a case report. J Med Case. Reports. 2008;2:219. doi: 10.1186/1752-1947-2-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoskins R. Ketamine associated cystitis - A case report. Int Emerg Nurs. 2009;17((1)):69–71. doi: 10.1016/j.ienj.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 18.Cottrell A, Gillatt D. Ketamine-associated urinary tract pathology: the tip of the iceberg for urologist? British Journal of Medical & Surgical Urology. 2008;1((3)):136–8. [Google Scholar]


