INTRODUCTION
We report a case of a young Chinese female who developed acute rhabdomyolysis with acute renal failure after a strenuous push-up exercise during a company motivation course. She managed to make full recovery after a period of outpatient treatment.
CASE REPORT
This is a case of a 33 years old Chinese lady who was previously healthy. Her lifestyle was sedentary (clerical job). Her weight was 60 kg and height 1.63 m (BMI 22.6 kg/m2). During a company motivation course she was instructed by the speaker to do 90 push-ups as a penalty for losing in one of the events. She admitted that it was tough but she managed to complete the push-ups over 5-10 minutes, urged on by her colleagues. She did the exercise at 2.00 pm and by 8.00 to 10.00 pm the same evening she complained of body aches and passed dark coloured urine. Following that, she had symptoms of lethargy, muscular weakness and nausea. She attributed it to ‘heat’ and did not seek medical attention. The aches were unbearable on the following night and she went to a nearby 24 hour clinic to obtain some analgesics. On the 4th day after the episode she decided to see her regular family physician. On consultation, her chief complains were lethargy, mild nausea and soreness of the arms, chest wall and abdomen. She brought with her a bottle of red coloured urine (Fig 1). She had no fever, frequency of urination or dysuria. She had her period well over a week before. She had not taken any drugs or alcohol prior to the episode. She gave no history of genetic disorders.
Figure 1.

Pigmenturia
Physical exam revealed bilateral tender and swollen arms, deep tenderness over the anterior chest wall and lower abdomen. The pulses of the upper limbs were all normal. Neurological examination was normal.
Urine dipstick test was positive 4+ for blood but the microscopic examination of the urine revealed less than 5 red blood cells per HPF. This laboratory finding suggested the presence of pigmenturia (haemoglobinuria or myoglobinuria). The clinical situation suggested the possibility of myoglobin in the urine. Blood sent for creatine kinase and renal function studies confirmed the clinical suspicion (Table1). Full blood count and urine cultures were normal.
Table 1. Serial laboratory test results.
| Day 4 | Day 7 | Day 10 | Day 13 | Day26 | Unit | Normal range | |
| CK | 134969 | 15537 | 2175 | 508 | NA | U/L | <201 |
| Sodium | 136 | 136 | 134 | 143 | 136 | mmol/L | 135-145 |
| Chloride | 103 | 99 | 98 | 99 | 100 | mmol/L | 95-110 |
| Potassium | 6.3 | 3.8 | NA | 3.8 | 3.8 | mmol/L | 3.5-5.1 |
| Urea | 7.1 | 6.6 | 6.1 | 3.6 | 3.8 | mmol/L | 2.5-6.4 |
| Creatinine | 192 | 154 | 119 | 99 | 78 | mmol/L | 40-80 |
| eGFR* | 28 | 36 | 48 | 60 | >60 | mL/min/1.73m2 | >60 |
NA, Not available
*MDRD study equation1
Table 1 shows the extremely elevated CK at presentation together with elevated levels of potassium, urea and creatinine. The estimates of glomerular filtration rate (eGFR) suggested that the renal function was significantly compromised at presentation. The subsequent changes of the laboratory parameters over time are also shown. With the clinical findings and the grossly elevated CK a diagnosis of acute rhabdomyolysis was made. The renal function studies suggest acute renal failure. She was advised to be admitted to hospital. Due to personal and family commitments she could not comply with inpatient treatment. However she agreed to see a private nephrologist and this was done only on the 7th day of the illness. In the interim period she was advised vigorous fluid intake and given a urinary alkaliniser. The parameters have improved when she saw the specialist such that hospitalization was unnecessary. She continued treatment on the ambulatory basis. She was treated with vigorous fluid intake and was prescribed sodium bicarbonate 2 g three times daily and frusemide 20 mg daily. The urinary pH was monitored and kept at > 7.0. The clinical and biochemical parameters gradually improved over the subsequent weeks. She made full recovery eventually.
DISCUSSION
Commercial urine dipstick tests are commonly used in the primary care office for the diagnosis of occult blood in the urine (haematuria) and other urinary disorders. It is based on the peroxidase-like activity of the heme moiety which catalyzes the reaction between an organic hydroperoxide and tetramethylbenzidine. Intact RBCs hemolyse on contact with the reagent pad and the haemoglobin reaction causes the appearance of a greenish ‘dot’. On the other hand, free haemoglobin or myoglobin results in a uniform colour on the reagent pad. However, the dipstick does not reliably distinguish between intact red blood cells and haemoglobin or myoglobin at high substrate concentrations (Fig 2 & 3). Thus pigmenturia (either hemoglobinuria or myoglobinuria) causes a false positive dipstick result for RBCs. The diagnosis of myoglobinuria is thus made in the appropriate clinical situation when there a positive dipstick test but the microscopy revealed a lack of RBCs in the sediment.
Figure 2.
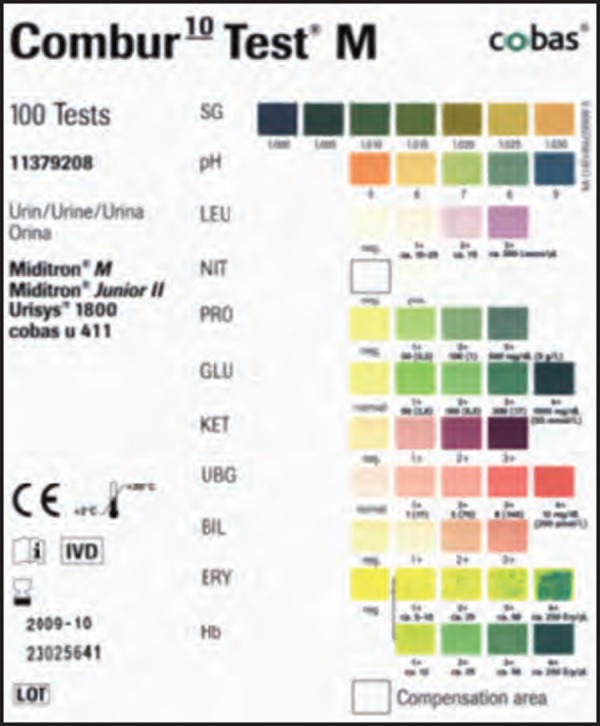
Typical dipstick panel
Figure 3.
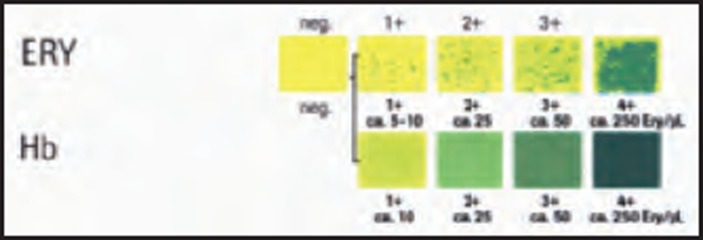
Occult blood panel (enlarged)
Rhabdomyolysis is defined as the dissolution or disintegration of skeletal muscles with the resultant release of intracellular contents into the circulation. The most important effects of these cellular by-products are electrolyte imbalance, acute renal failure respiratory distress syndrome and disseminated intravascular coagulation (DIC).2 Rhabdomyolysis can result from physical as well as nonphysical causes. Bywaters and colleagues were credited for their first description of traumatic rhabdomyolysis as a consequence of crush injuries at the time of the German blitz of London during World War 2.3 Nonphysical causes include infections (e.g. myositis due to influenza), toxins (e.g. snake venom) and drugs (e.g. statins). Exercise-induced rhabdomyolysis occurs when there is excessive muscular activity which may occur in situations like long distance running, military training and strenuous exertion in an untrained individual.4 The hallmark of exercise-induced rhabdomyolysis is the temporal relationship between the episode of strenuous and excessive muscular exertion and the occurrence of red or red-brown coloured pigmenturia, weakness, myalgia as well as a rapid elevation of the level of CK in the blood. The characteristic of ARF in rhabdomyolysis is the rate of rise of creatinine that is out of proportion to the rate of rise of blood urea nitrogen. The normal ratio of BUN:creatinine of 10:1 is lowered to less than 6:1 (calculated in mg%). This is due to the release of large quantities of creatine from damaged muscles and its subsequent conversion to creatinine.2,5 Elevations of the CK in exertional rhabdomyolysis may be quite remarkable.6
Exertional rhabdomyolysis with acute renal complication in a female worker is not commonly reported. Knochel described the complication of exhaustive exercise as ‘white collar rhabdomyolysis’ which he found to be a disease of working men.7 In a 5-year retrospective study in an emergency department, Sinert et al reported 35 cases of exercise-induced rhabdomyolysis. All the cases occurred in men.8 Lin et al reported 118 cases of exercise-induced rhabdomyolysis in students of both sexes after strenuous push-ups. However none of the cases developed acute renal complications.9 Typically, myoglobinuria occurs 2 to 4 days after a strenuous exertion. It is remarkable that the case reported had pigmenturia after a few hours after exercise. Perhaps it signifies the severity of the injury and the relatively deconditioned state of the musculature.
In view of the risks of electrolyte imbalance and cardiac arrest complicated cases of acute rhabdomyolysis would require hospitalization. Treatment options include vigorous intravenous hydration, pushing oral fluid intake, urinary alkalinizaton, intravenous mannitol and diuretics. In severe cases haemodialysis may be required. Our case in question opted for outpatient treatment against medical advice.
Muscle damage and soreness after exercise principally results from eccentric exercise, a form of activity in which a muscle is forcefully lengthened while it contracts. Force can be generated within a muscle via concentric or eccentric exercise. An example of concentric exercise is lifting a dumbbell in the hand (concentric biceps contraction). Lowering the dumbbell would be an example of an eccentric exercise, the biceps muscle being forcefully lengthened while contracting. Similarly the negative phase of a push-up involves eccentric muscular activity of the triceps muscle.10 Severe muscle injury can thus be produced by strenuous push-ups.
How many push-ups in an individual could result in serious skeletal muscle injury? It would depend on the load factor (ones own weight), the condition of the muscle (training reduces risks) and the environmental condition (heat and humidity increases risk). Lin et al described rhabdomyolysis in students after 120 push-ups in 5 minutes in cold weather.9 Our patient developed rhabdomyolysis and renal complications after 90 push-ups in equivalent time in normal office condition.
In conclusion, rhabdomyolysis due to excessive muscular activity in untrained individuals can be prevented. Suspicion should be heightened in the right clinical situation. Physical trainers should be aware of this condition and be extremely careful when prescribing exercise to untrained individuals.
Red yeast rice reduces cholesterol level
Becker DJ, Gordon RY, Halbert SC, et al. Red yeast rice for dyslipidemia in statin-intolerant patients: a randomized trial. Ann Intern Med. 2009; 150(12):830-9
62 patients with dyslipidemia and history of discontinuation of statin therapy due to myalgias were randomized to receive red yeast rice, 1800 mg or placebo twice daily for 24 weeks. All patients were concomitantly enrolled in a 12-week therapeutic lifestyle change program. Low-density lipoprotein cholesterol level was significantly lower in the red yeast rice group than in the placebo group at both weeks 12 and 24.
REFERENCES
- 1.Levey AS, Bosch JP, Lewis JB. et al. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of diet in renal disease study group. Ann Intern Med. 1999;130((6)):461–70. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 2.Huerta-Alardin AL, Varon J, Marik PE. Bench-to-bedside review: Rhabdomyolysis - an overview for clinicians. Crit Care. 2005;9((2)):158–69. doi: 10.1186/cc2978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bywaters E, Beall D. Crush injuries with impairment of renal function. BMJ. 1941;1:427–32. doi: 10.1136/bmj.1.4185.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Teitjen DP, Guzzi LM. Exertional rhabdomyolysis and acute renal failure following the Army Physical Fitness Test. Mil Med. 1989;154((1)):23–5. [PubMed] [Google Scholar]
- 5.Schrier RW. Lippincot: Williams & Wilkins; 2007. Diseases of the kidney and urinary tract; p. 1190. [Google Scholar]
- 6.Casares P, Marull J. Over a million creatine kinase due to a heavy work-out: a case report. Cases J. 2008;1((1)):173. doi: 10.1186/1757-1626-1-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Knochel JP. Catastrophic medical events with exhaustive exercise: “white collar rhabdomyolysis”. Kidney Int. 1990;38((4)):709–19. doi: 10.1038/ki.1990.263. [DOI] [PubMed] [Google Scholar]
- 8.Sinert R, Kohl L, Rainone T. et al. Exercise induced rhabdomyolysis. Ann Emerg Med. 1994;23((6)):1301–6. doi: 10.1016/s0196-0644(94)70356-6. [DOI] [PubMed] [Google Scholar]
- 9.Lin AC, Lin CM, Wang TL. et al. Rhabdomyolysis in 119 students after repetitive exercise. Br J Sports Med. 2005;39((1)):e3. doi: 10.1136/bjsm.2004.013235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Proske U, Morgan DL. Muscle damage from eccentric exercise: mechanism, mechanical signs, adaptation and clinical applications. J Physiol. 2001;537((pt 2)):333–45. doi: 10.1111/j.1469-7793.2001.00333.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


