Abstract
Introduction: Hypertension is a common co-morbidity in diabetes mellitus (DM) that may lead to serious complications if not adequately controlled.
Method: This is a descriptive study based on data from the Audit of Diabetes Control and Management (ADCM) registry. This audit assessed the treatment and standard of control of hypertension in diabetic patients aged 18 years and above. Data were analysed using STATA version 9.
Results: From a total of 20 646 cases, about two third of them, 13 417 (65%) were reported to have hypertension. 19 484 (94.4%) had their blood pressure (BP) recorded and out of these, 11 414 (58.5%) were found to have BP >130/80 mmHg. 13 601 cases (65.9%) of the total sample were on antihypertensive drugs. 64.1% of those on antihypertensive drugs were prescribed angiotensin-converting enzyme inhibitors (ACEI) or angiotensin II receptor blockers. 14.2% were on more than two types of antihypertensive drugs. Older patients and those with longer duration of DM were less likely to achieve the target BP of ≤130/80. In general, about 40% of diabetic cases registered in the ADCM project had their hypertension well controlled.
Keywords: Diabetes mellitus, hypertension, antihypertensives, primary care, registries
BACKGROUND
Hypertension is a common co-morbidity in 65% of patients with diabetes mellitus (DM).1-3 In type 2 diabetes (T2D), hypertension is often part of metabolic syndrome whereas in type 1 diabetes (T1D), hypertension often indicates the coexistence of diabetic nephropathy.4-7 Poorly controlled hypertension leads to heightened and accelerated nephropathy, cerebrovascular accidents, three-fold increase of atherosclerosis and heart diseases, retinopathy, poor quality of life and prematured death.8-13 Micro and macrovascular complications are more common in diabetic patients who also have hypertension. These patients have two-fold increased risk of cardiovascular mortality compared to patients with diabetes alone. Studies have shown that intensive blood pressure (BP) control has a beneficial effect in decreasing the rate of progression of these complications.14-16
The United Kingdom Prospective Diabetes Study (UKPDS 38) had shown that patients with good BP control (mean BP of 144/82 mmHg) had 25-50% less risk of developing cardiovascular complications compared to patients with not so well controlled BP (mean BP of 154/87 mmHg).15 Adequate BP control was reported to be the most cost-effective treatment to reduce cardiovascular complications in patients with DM. Current literature indicates that management of hypertension in diabetic patients is generally far from satisfactory.17-21
There are many evidence-based guidelines for management of hypertension in patients with DM. These guidelines emphasize on intensive BP control with combined drug therapy.14, 22,23 Renin-angiotensin system inhibitors are the preferred antihypertensive drugs of choice since a number of clinical trials have documented the benefits of these drugs in diabetic patients.14-16,22 Periodic audit and awareness of clinical performance in diabetic care is essential towards prevention of diabetic complications. This study assessed the control and treatment of hypertension in patients with diabetes from the database of Audit of Diabetes Control and Management (ADCM).
METHODS
AUDIT OF DIABETES CONTROL AND MANAGEMENT (ADCM) REGISTRY
ADCM is a multi-centred observational cohort study that was started in May 2008 in the state of Negeri Sembilan and will later include other states in Malaysia. The aim of this project is to gather information to monitor provision of diabetic care in Malaysia, to improve treatment outcomes, to help with budget planning, to facilitate research activities and to enhance health education for physicians and patients on the potential serious impacts of this chronic disease on the nation.24-27
All government health clinics and hospitals were invited to participate in this project. These clinics are mainly managed by medical officers and paramedics such as medical assistants, staff nurses, community nurses, nutritionists and physiotherapists.28 Some bigger health clinics are supervised by resident family medicine specialists and qualified pharmacists.28 Trained physicians and paramedical staff of these health clinics (termed as source data providers (SDP)) were briefed and instructed on how to register all newly diagnosed cases of DM of aged 18 years and above and how to enter follow-up information on the status of their diabetes. An online standard case record form (CRF) is available in the ADCM website. Information required includes demographic data, duration of diabetes, clinical examination findings including BP reading, treatment modalities, as well as various risk factors and diabetic complications. To maintain confidentiality, certain security procedures are required for SDP to gain access to the database.29
Diagnosis for new cases of DM is based on WHO criteria. Diagnosis for follow up cases is based on their current treatments that include lifestyle modification, oral hypoglycaemic drugs or insulin injections. Hypertension is diagnosed when there is persistent elevation of systolic BP >130 mmHg and/or diastolic BP >80 mmHg on two or more occasions as recommended in the National Clinical Practice Guidelines (CPG).30 BP readings that were recorded most recently were analysed in this study. Good BP control is considered as BP ≤130/80 mmHg. Data collected is analysed by a secretariat based at Clinical Research Centre (CRC), Hospital Kuala Lumpur with the use of Data Analysis and Statistical Software (Stata) version 9.
Access to ACDM database for the purpose of writing this paper has received approval from Medical Research Ethics Committee (MREC), Ministry of Health, Malaysia.
RESULTS
Till 31st December 2008, there were a total of 81 health centres and hospitals that participated in this audit. Altogether there were 20 646 cases registered. About two third of them, 13 417 cases (65%) were reported to have hypertension. 19 484 (94.4%) had their BP recorded and out of these, 11 414 (58.5%) were found to have BP >130/80 mmHg.
Majority of cases (89.6%) were from Negeri Sembilan; 9.8% were from Selangor. Most of the cases registered (99.2%) were of T2D. 56.8% of cases were female; 56.6% were Malays, 19.5% were Chinese, 22.5% were Indians and 0.2% were of other races (Table 1). Mean age of patients was 58.0 years (SD 11.49); 76.9% of patients were aged 50 years and above. 82% of cases had body mass index (BMI) in the overweight category (BMI ≥23 kgm2); 42.3% in the obese category (BMI ≥27.5 kgm2). Mean age at diagnosis of diabetes was 54.8 years (SD 11.47) and mean duration of diabetes was 4.7 years (SD 4.20) (Table 2).
Table 1. Demographic profile of the T2D patients.
| Profile | Number (%) |
|---|---|
| Gender | 20 646 (100) |
| Male | 8687 (42.1) |
| Female | 11 722 (56.8) |
| Not stated | 237 (1.1) |
| Ethnicity | 20 646 (100) |
| Malay | 11 694 (56.6) |
| Chinese | 4026 (19.5) |
| Indian | 4637 (22.5) |
| Other Malaysian | 48 (0.2) |
| Non-Malaysian | 7 (0.03) |
| Not stated | 234 (1.1) |
| Age groups (years) | 20 646 (100) |
| <30 | 178 (0.9) |
| 30-49 | 4423 (21.4) |
| 50-69 | 12 424 (60.2) |
| ≥70 | 3456 (16.7) |
| Not stated | 165 (0.8) |
Table 2. Duration of T2D.
| Duration of diabetes | Number (%) |
|---|---|
| <5 years | 11 276 (54.6) |
| 5-10 years | 5672 (27.5) |
| >10 years | 3356 (16.3) |
| Not stated | 342 (1.7) |
| Total | 20 646 (100) |
Mean systolic and diastolic BP were 137.7 mmHg (SD 19.56) and 80.1 mmHg (SD 10.51) respectively. There were significant associations (Chi-square test, p<0.001) between each of these independent variables: ethnicity, age groups and duration of diabetes with target BP ≥130/80 mmHg. More Indians (45.9%) achieved target BP ≤130/80 mmHg as compared to the Malays (41.9%) and Chinese (34.8%). The older the patients, the lesser the percentage that achieved target BP ≤130/80 mmHg; 36.2% of age group ≥70 years achieved the target as compared to 42.3% and 59.3% of age groups 30-69 years and <30 years respectively (Table 3). Longer duration of diabetes corresponds to lesser percentage that achieved the target BP; 39.1% of cases with diabetes >10 years attained BP ≤130/80 mmHg as compared to 42.1% and 41.8% of those who have diabetes 5-10 years and <5 years respectively (Table 3). 13 601 cases (65.9%) of the total sample were on antihypertensive drugs. 64.1% of those on antihypertensive drugs were prescribed angiotensin-converting enzyme inhibitors (ACEI) or angiotensin II receptor blockers; 35.3% were on β-blockers and 34.3% were on calcium channel blockers (Table 4). 14.2% of cases were on more than two anti-hypertensive drugs (Figure 1).
Table 3. Proportion of patients controlled to target blood pressure according to age groups and duration of diabetes.
| Age group | BP≤130/80 mmHg, n(%) | Total, n(%) | |
|---|---|---|---|
| No | Yes | ||
| 15-19 | 2 (16.7) | 10 (83.3) | 12 (100) |
| 20-24 | 17 (42.5) | 23 (57.5) | 40 (100) |
| 25-29 | 49 (42.6) | 66 (57.4) | 115 (100) |
| 30-34 | 102 (42.0) | 141 (58.0) | 243 (100) |
| 35-39 | 258 (45.3) | 311 (54.7) | 569 (100) |
| 40-44 | 607 (49.3) | 623 (50.7) | 1230 (100) |
| 45-49 | 1129 (52.4) | 1027 (47.6) | 2156 (100) |
| 50-54 | 1745 (56.4) | 1350 (43.6) | 3095 (100) |
| 55-59 | 2156 (60.0) | 1439 (40.0) | 3595 (100) |
| 60-64 | 1771 (62.5) | 1063 (37.5) | 2834 (100) |
| 65-69 | 1525 (64.1) | 853 (35.9) | 2378 (100) |
| 70-74 | 1138 (64.3) | 633 (35.7) | 1771 (100) |
| 75-79 | 590 (63.6) | 338 (36.4) | 928 (100) |
| >80 | 325 (62.7) | 193 (37.3) | 518 (100) |
| Total | 11 414 (58.6) | 8070 (41.4) | 19 484 (100) |
| Duration of diabetes | No | Yes | Total |
| <5 years | 6331 (58.2) | 4541 (41.8) | 10 872 (100) |
| 5-10 years | 3089 (57.9) | 2248 (42.1) | 5337 (100) |
| >10 years | 1891 (60.9) | 1214 (39.1) | 3105 (100) |
| Total | 11 311 (58.6) | 8003 (41.4) | 19 314 (100) |
Table 4. Anti-hypertensives prescribed.
| Anti-hypertensive agent | n(%) |
|---|---|
| ACE inhibitor | 8456 (62.2) |
| ARB | 254 (1.9) |
| Centrally acting | 59 (0.4) |
| Alpha-blockers | 976 (7.2) |
| Calcium channel blocker | 4669 (34.3) |
| Diuretic | 2473 (18.2) |
| Beta-blocker | 4797 (35.3) |
| Others | 57 (0.4) |
| Total | 21 741 |
Figure 1.
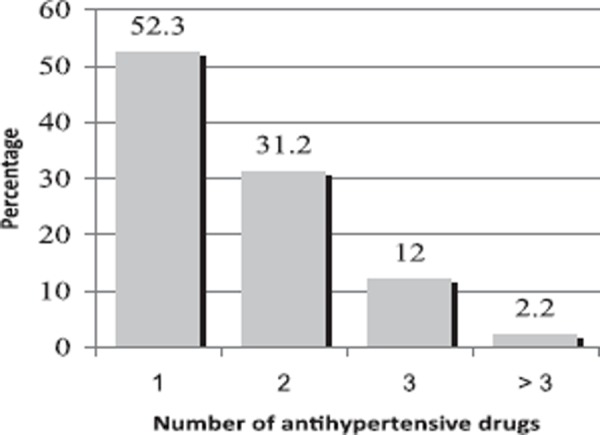
Percentage of number of anti-hypertensive prescribed
DISCUSSION
Majority of cases were from the public health clinics; the greatest number of cases came from the state of Negeri Sembilan. Predominance of female patients (57.2%) and retired elderly individuals in the registry (77.6% were > 50 years) reflects the day to day patient profiles of Malaysian public health care centres.27 However, the greater percentage of Indian as compared to Chinese patients recorded in the registry did not reflect the national ethnic representation. It was likely that this discrepancy was due to preference of Chinese patients seeking healthcare in the private sector31 or higher prevalence of DM among the Indians.
Similar to First Annual Report of National Eye database (2007) that stated 63.9% of diabetic patients were reported to have hypertension,32 the figure obtained in this study was 13 417 cases (65%). 19 484 cases (94.4%) had their BP readings recorded. It is a required routine for all diabetic patients to have their BP measured at the time of diagnosis and at each scheduled visit to the diabetic clinic.23 There could be accidental omission of BP readings for some cases in the registry.
13 601 cases (65.9%) were taking antihypertensive drugs, a figure slightly higher than the 65% of cases that were reported to have hypertension. It could be that antihypertensive drugs were prescribed solely for renoprotection and cardioprotection rather than for hypertension, or cases with controlled hypertension were considered as normotensive and not included in the report. 8070 cases (41.4%) or 39.1% if calculation were to be based on total number of 20 646 cases, achieved target BP of ?130/80 mmHg (Table 3). This figure was comparable to those of Thailand cohort33 and slightly higher than the Swedish cohort (2003).34
Out of all cases on antihypertensive treatment in the ADCM registry, 52.3% were receiving monotherapy. Only 14.2% were receiving three or more antihypertensive drugs, a figure less than the 21.6% of Thailand cohort that received combined drug therapy.35 UKPDS 38 showed that diabetic patients with hypertension generally require three and more antihypertensive drugs after having the disease for more than nine years.15 ACEI that have been proven to confer significant renal and cardiac protection for high risk diabetic patients, were the most prescribed antihypertensive drugs.36,37 Previous study conducted in Melaka Tengah district in year 2003 indicated that the most commonly used antihypertensive was a beta blocker, metoprolol.38 This shows that there is greater awareness among healthcare providers of the usefulness of ACEI for diabetic patients. Angiotensin II receptor blocker is not widely prescribed because of its higher cost and prescribing is restricted only to medical specialists.
Phenomenon of therapeutic inertia (TI) was well-reported by Okonofua EC et al. in United States using the Hypertension Initiative database. It was found that TI could account for a 19% variance in BP control; patients who experienced higher TI score had systolic BP increased in their last visit when compared to first clinic visit and vice versa.39 Poor achievement of target BP of ≤130/80 mmHg in ADCM could be partly due to this phenomenon of TI in view of decreasing percentage of achievement of target BP corresponding to increasing age groups and increasing duration of diabetes. Other factors for failure to achieve target BP include budget constraints, degree of patient adherence to medication and limited number of qualified Family Medicine Specialists.
Limitation of this audit was the retrospective retrieval of data from patient records by physicians not involved in the clinical care of these diabetic cases. Information recorded may be inaccurate or incomplete. Hopefully with improved training and good teamwork, these unfavourable factors may be overcomed.
To improve the outcome of this national audit of such a massive scale, we recommend that:
A steering committee to be established to look after timely reports and publications.
A team of bio-medical statisticians to analyse database and to provide expert advice.
Regular on-site training and support for SDP.
CONCLUSION
Hypertension is prevalent among patients with DM. Less than 50% of diabetic cases registered in the ADCM achieved good control of BP to the target level of ≤130/80 mmHg. Antihypertensive treatments were mainly monotherapy. Most commonly prescribed antihypertensive drug was ACEI. Prescribing skills of physicians for management of hypertension in patients with DM requires further improvements.
ACKNOWLEDGEMENT
We would like to acknowledge the Director General of Health for his support and approval in using these data from public health clinics for this study. We would like to express our thanks to Dr Jamaiyah Haniff of Clinical Research Centre (CRC), Hospital Kuala Lumpur, for facilitating access to the registry database and to CRC staff, Noor Akma Hassim and Tee Chin Kim. Special thanks to Ms Lena Yeap from ClinResearch Sdn Bhd for her support in the statistical analysis of data.
Footnotes
Funding
This project was supported by Ministry of Health, Malaysia.
Contributor Information
BH Chew, MFamMed.
I Mastura, MFamMed.
AT Cheong, MFamMed.
SAR Syed Alwi, MFamMed.
References
- 1.Epstein M, Sowers JR. Diabetes mellitus and hypertension. Hypertension. 1992;19((5)):403–18. doi: 10.1161/01.hyp.19.5.403. [DOI] [PubMed] [Google Scholar]
- 2.Williams B. Insulin resistance; the shape of things to come. Lancet. 1994;344((8921)):521–4. doi: 10.1016/s0140-6736(94)91904-6. [DOI] [PubMed] [Google Scholar]
- 3.Williams G. In: Pickup J, Williams G, editors. London: Blackwell Scientific Publications; 1991. Hypertension in diabetes; pp. 719–32. Textbook of diabetes. [Google Scholar]
- 4.DeFronzo RA, Ferrannini E. Insulin resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care. 1991;14((3)):173–94. doi: 10.2337/diacare.14.3.173. [DOI] [PubMed] [Google Scholar]
- 5.Nishimura R, LaPorte RE, Dorman JS. et al. Mortality trends in type 1 diabetes. The Allegheny County (Pennsylvania) Registry 1965-1999. Diabetes Care. 2001;24((5)):823–7. doi: 10.2337/diacare.24.5.823. [DOI] [PubMed] [Google Scholar]
- 6.Cowie CC, Harris MI. 2nd ed. Washington DC: U.S. Govt. Printing Office; 1995. Physical and metabolic characteristics of patients with diabetes. In: Diabetes in America. National Diabetes Data Group; pp. 117–64. [Google Scholar]
- 7.Mathiesen ER, Ronn B, Jensen T. et al. Relationship between blood pressure and urinary albumin excretion in development of microalbuminuria. Diabetes. 1990;39((2)):245–9. doi: 10.2337/diab.39.2.245. [DOI] [PubMed] [Google Scholar]
- 8.Kuala Lumpur: The National Renal Registry, Malaysian Society of Nephrology; 2009. 16th Report of the Malaysian Dialysis and Transplant Registry 2008. [Google Scholar]
- 9.Agmon Y, Khandheria BK, Meissner I. et al. Independent association of high blood pressure and aortic atherosclerosis: a population-based study. Circulation. 2000;102((17)):2087–93. doi: 10.1161/01.cir.102.17.2087. [DOI] [PubMed] [Google Scholar]
- 10.Stamler J, Vaccaro O, Neaton JD. et al. Diabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care. 1993;16((2)):434–44. doi: 10.2337/diacare.16.2.434. [DOI] [PubMed] [Google Scholar]
- 11.Stratton IM, Kohner EM, Aldington SJ. et al. UKPDS 50: risk factors for incidence and progression of retinopathy in Type II diabetes over 6 years from diagnosis. Diabetologia. 2001;44((2)):156–63. doi: 10.1007/s001250051594. [DOI] [PubMed] [Google Scholar]
- 12.Garcia MJ, McNamara PM, Gordon T. et al. Morbidity and mortality in diabetics in the Framingham population. Sixteen year follow-up study. Diabetes. 1974;23((2)):105–11. doi: 10.2337/diab.23.2.105. [DOI] [PubMed] [Google Scholar]
- 13.Alexandria VA: American Diabetes Association; 2001. American Diabetes Association. Diabetes 2001 Vital Statistics. [Google Scholar]
- 14.Chobanian AV, Bakris GL, Black HR. et al. The Seventh Report of the Joint National Committee on Prevention, Detection,Evaluation, and Treatment of High Blood Pressure: JAMA. 2003;289((19)):2560–72. doi: 10.1001/jama.289.19.2560. the JNC 7 report. [DOI] [PubMed] [Google Scholar]
- 15.Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes. BMJ. 1998;317((7160)):703–13. UKPDS 38. UK Prospective Diabetes Study Group. [PMC free article] [PubMed] [Google Scholar]
- 16.Hansson L, Zanchetti A, Carruthers SG. et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: Lancet. 1998;351((9118)):1755–62. doi: 10.1016/s0140-6736(98)04311-6. principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. [DOI] [PubMed] [Google Scholar]
- 17.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988-2000. JAMA. 2003;290((2)):199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 18.Wolf-Maier K, Cooper RS, Kramer H. et al. Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension. 2004;43((1)):10–7. doi: 10.1161/01.HYP.0000103630.72812.10. [DOI] [PubMed] [Google Scholar]
- 19.Geiss LS, Rolka DB, Engelgau MM. Elevated blood pressure among U.S. adults with diabetes, 1988-1994. Am J Prev Med. 2002;22((1)):42–8. doi: 10.1016/s0749-3797(01)00399-3. [DOI] [PubMed] [Google Scholar]
- 20.Donnelly R, Molyneaux L, McGill M. et al. Detection and treatment of hypertension in patients with non-insulin-dependent diabetes mellitus: does the “rule of halves” apply to a diabetic population? Diabetes Res Clin Pract. 1997;37((1)):35–40. doi: 10.1016/s0168-8227(97)00062-4. [DOI] [PubMed] [Google Scholar]
- 21.Berlowitz DR, Ash AS, Hickey EC. et al. Hypertension management in patients with diabetes: the need for more aggressive therapy. Diabetes Care. 2003;26((2)):355–9. doi: 10.2337/diacare.26.2.355. [DOI] [PubMed] [Google Scholar]
- 22.American Diabetes Association. Standard of medical care in diabetes - 2006. Diabetes Care. 2006;29(Suppl 1):4–42. [Google Scholar]
- 23.4th ed. Malaysia: Ministry of Health; 2009. Clinical Practice Guidelines: Management of Type 2 Diabetes Mellitus. [Google Scholar]
- 24.ADCM User Manual (version 1.0) [Online]
- 25.Kuala Lumpur: Clinical Research Centre; Diabetes Malaysia Registry. About DRM-ADCM. [Google Scholar]
- 26.Economic consequences of diabetes mellitus in the U.S. in 1997. American Diabetes Association. Diabetes Care. 1998;21((2)):296–309. doi: 10.2337/diacare.21.2.296. [DOI] [PubMed] [Google Scholar]
- 27.Malaysia: Ministry of Health; 2006. National Health Morbidity Survey III. [Google Scholar]
- 28.Noor Ghani S, Yadav H. Kuala Lumpur: University of Malaya Press; 2008. Health Care in Malaysia. [Google Scholar]
- 29.Mastura I, Zanariah H, Fatanah I. et al. An Audit of Diabetes Control and Management (ADCM) Med J Malaysia. 2008;63(suppl C):76–7. [PubMed] [Google Scholar]
- 30.3rd ed. Malaysia: Ministry of Health; 2008. Clinical Practice Guidelines: Management of Hypertension. [Google Scholar]
- 31.Toh MP, Heng BH, Sum CF. et al. Measuring the quality of care of diabetic patients at the specialist outpatient clinics in public hospitals in Singapore. Ann Acad Med Singapore. 2007;36((12)):980–6. [PubMed] [Google Scholar]
- 32.Goh PP Elias H Mariam I et al. The First Annual Report of the National Eye Database 2007. [Online]
- 33.Kosachunhanun N, Benjasuratwong Y, Mongkolsomlit S. et al. Thailand diabetes registry project: glycemic control in Thai type 2 diabetes and its relation to hypoglycemic agent usage. J Med Assoc Thai. 2006;89(Suppl 1):66–71. [PubMed] [Google Scholar]
- 34.Eliasson B, Cederholm J, Nilsson p. et al. The gap between guidelines and reality: Type 2 diabetes in a National Diabetes Register 1996-2003. Diabet Med. 2005;22((10)):1420–6. doi: 10.1111/j.1464-5491.2005.01648.x. [DOI] [PubMed] [Google Scholar]
- 35.Bunnag P, Plengvidhya N, Deerochanawong C. et al. Thailand diabetes registry project. prevalence of hypertension, treatment and control of blood pressure in hypertensive adults with type 2 diabetes. J Med Assoc Thai. 2006;89(Suppl 1):72–7. [PubMed] [Google Scholar]
- 36.Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus. results of the HOPE study and MICRO-HOPE substudy. Heart Outcomes Prevention Evaluation Study Investigators. Lancet. 2000;355((9200)):253–9. [PubMed] [Google Scholar]
- 37.Yusuf S, Sleight P, Pogue J. et al. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med. 2000;342:145–53. doi: 10.1056/NEJM200001203420301. [DOI] [PubMed] [Google Scholar]
- 38.Chan GC. Type 2 diabetes mellitus with hypertension at primary healthcare level in Malaysia: are they managed according to guidelines? Singapore Med J. 2005;46((3)):127–31. [PubMed] [Google Scholar]
- 39.Okonofua EC, Simpson KN, Jesri A. et al. Therapeutic inertia is an impediment to achieving the healthy people 2010 blood pressure control goals. Hypertension. 2006;47((3)):345–51. doi: 10.1161/01.HYP.0000200702.76436.4b. [DOI] [PubMed] [Google Scholar]


