A. Epidemiology, Clinical Diagnosis & General Principles of Management
Schizophrenia is a serious brain disease that alters an individual’s perception, thought, affect and behaviour. In a systematic review, the incidence rate was noted to be 15.2 per 100,000 (range of 7.7 to 43.0 per 100,000) and higher in males, urban and migrant population.
Although there is effective biopsychosocial treatment available, substantial number of people with schizophrenia remains undiagnosed and untreated. Duration of untreated psychosis (DUP) is described as the time period from onset of the first psychiatric symptom to initiation of antipsychotic treatment. In the National Mental Health Registry Report, the mean and median DUP was 28.7 months and 12 months respectively. Males had shorter DUP compared to female.
People who develop symptoms of schizophrenia should be diagnosed and treated early. The diagnostic criteria of schizophrenia, based on International Classification of Diseases-10 (ICD-10), are shown in Table 1.
Table 1: Diagnostic Criteria of Schizophrenia.
| • Distortions of thinking and perception | • The most important psychopathological phenomena include:
|
|
| • Inappropriate or blunted affects | ||
| • Clear consciousness and intellectual capacity maintained | ||
| • Certain cognitive deficits may evolve over time | ||
| The course of schizophrenic disorders can be either continuous, or episodic with progressive or stable deficit, or there can be one or more episodes with complete or incomplete remission. The following should be excluded: | ||
| • bipolar disorder | • drug intoxication or withdrawal | • overt brain disease |
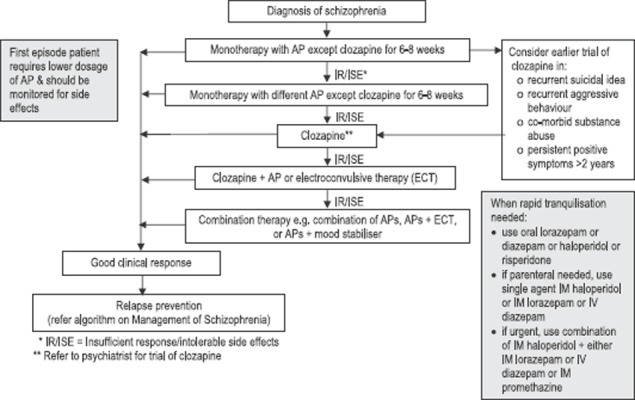
The management of schizophrenia should be a comprehensive package that includes individually-tailored medication, and appropriate psychosocial and service level interventions. This is illustrated in Algorithm 1. It may also be divided into acute phase, relapse prevention and stable phase. In the acute phase, positive symptoms (hallucinations, delusions and behavioural disturbances) will surface. With adequate treatment, the symptoms will disappear in most cases. However, negative symptoms (affective flattening, alogia and avolition) may persist. Although there are many patterns to the course of illness following this acute phase, majority of cases (75%) will have a chronic disease that causes some degree of disability. The associated deterioration may stop after ten years where cases may become stable with sign of improvement.
Algorithm 1:

Management of Schizophrenia
In 1996, integrated care of schizophrenia in primary health care services was implemented in Malaysia which includes mental health promotion, follow-up of stable cases, early detection and treatment, and psychosocial rehabilitation.
B. Pharmacological Treatment
Antipsychotics (APs) are the mainstay of pharmacological treatment in schizophrenia. Conventional APs should be used as a first option; most commonly used are haloperidol, perphenazine or sulpiride. As options, atypical APSs (AAPs) such as amisulpride (AMS) or olanzapine (OLZ) may also be considered (refer to Algorithm 2 and Table 3). Those taking AAPs should be monitored closely for emergence of metabolic syndrome.
Algorithm 2:
Medications of Schizophrenia
Table 3: Suggested AP Dosages and Adverse Effects.
| Drug | Starting Dose | Target Dose or Range | Antipsychotic Schedule | Side Effects |
| Amisulpride (Solian) | 50 mg/day | 50-300 mg for negative symptoms, 400-800 mg for positive symptoms | Once daily. If more than 400 mg, twice daily | Insomnia, anxiety, agitation, somnolence, nausea, dry mouth, acute dystonia, galactorrhoea |
| Aripiprazole (Abilify) Generic available | 10-15 mg/day | 10-30 mg/day | Once daily | Agitation, constipation, EPS, insomnia, nausea, somnolence |
| Olanzapine (Zyprexa) | 5-10 mg/day | 10-20 mg/day | Once daily | Constipation, dizziness, dry mouth, impaired glucose tolerance (IGT), hyperlipidaemia, increased appetite, sedation, weight gain |
| Quetiapine (Seroquel) | 50 mg/day | 300-800 mg/day | Twice daily | Dry mouth, IGT, headache, hyperlipidaemia, increased appetite and weight, orthostatic hypotension, sedation |
| Paliperidone (Invega) | 3 mg/day | 6-12 mg/day | Once in the morning | EPS, IGT, galactorrhoea, hyperlipidaemia, menstrual irregularity, orthostatichypotension, prolactin elevation, sedation, sexual dysfunction, tardive dyskinesia, weight gain |
| Risperidone (Risperdal) Generic available | 1-2 mg/day | 2-6 mg/day | Once daily | |
| Risperidone microspheres long-acting injection (Consta) | 25 mg/2 weeks | 25-50 mg every 2 weeks | Once every 2 weeks | |
| Clozapine (Clozaril) Generic available | 12.5 mg/day | 300-900 mg/day (serum level for doses >600 mg/day) | Twice daily | Agranulocytosis, excess salivation, fever, IGT, hyperlipidaemia, increased appetite, myocarditis, orthostatic hypotension, sedation, seizures, tachycardia, weight gain |
| Chlorpromazine (CPZ) | 50-100 mg/day | 300-1000 mg/day | 3 times daily | Constipation, dry mouth, EPS, orthostatic hypotension, photosensitivity, sedation, tachycardia, tardive dyskinesia |
| Perphenazine | 4-8 mg/day | 16-64 mg/day | 3 times daily | |
| Fluphenazine depot (Modecate) Generic available | 12.5-25 mg IM/ 1-3 weeks | 6.25-50 mg IM every 2-4 weeks | Every 1-3 weeks | |
| Flupenthixol decanoate (Fluanxol) | 10-20 mg IM/ 1-3 weeks | 10-40 mg IM every 2-4 weeks | Every 1-3 weeks | |
| Haloperidol | 2-5 mg/day | 2-20 mg/day | 1-3 times daily | |
| Sulpiride Generic available | 200-400 mg daily | 400-800 mg daily | Twice daily | |
| Zuclopenthixol acetate (Acuphase) | 50-100 mg IM/ 2-3 days | 50-200 mg/3 days | - | |
| Zuclopenthixol decanoate (Clopixol depot) | 100-200 mg IM/ 1-3 weeks | 100-400 mg/ 1-3 weeks | Every 1-3 weeks |
C. Psychosocial Intervention
Psychosocial interventions aim to improve the individual’s ability to handle stressful life events, increase adherence to medication, help with illness self-management, promote better communication and coping skills, enhance quality of life and promote recovery and reintegration Effective psychosocial interventions for schizophrenia include family intervention, psychoeducation, social skills training and cognitive remediation therapy.
D. Service Level Intervention
Service Level Intervention is important as Malaysia is currently in the process of developing more comprehensive hospital-based community psychiatric services and mental health services at the primary care level. It is essential that the following services be considered for every person with schizophrenia i.e. community mental health team to prevent relapse and readmissions, assertive community treatment for more difficult cases, supported employment for all who want to work and crisis intervention and home treatment as alternative to acute inpatient care.
Criteria for referral and admission are shown in Table 2 below:-
Table 2: Criteria for referral and admission.
| Criteria for Early Referral to Specialist Care | Criteria for Hospitalisation |
|---|---|
| • Prodromal or attenuated symptoms | • Risk of harm/neglect to self or others |
| • Unclear diagnosis | • Deterioration in psychosocial functioning |
| • Treatment adherence issues | • Serious/life-threatening drug reactions |
| • Poor response to treatment | |
| • Potential violent behaviour to self or others | |
| • Drug-related complications | |
| • Plan for psychosocial rehabilitation | |
| • o-morbid substance abuse | |
| • Special group such as pregnancy, paediatric and geriatric age |
ACKNOWLEDGEMENT
List of other members for the Development Group Clinical Practice Guidelines Management of Schizophrenia in Adults: Ahmad Zabidin Zakaria, Anil Kalsom Musa, Cathy Suhaila Abdullah, Cheah Yee Chuang, Mohd Fadzillah Abdul Razak, Muhammah Najib Mohd Alwi, Nor Asmawati Mohamad Ali Abdul Rahman, Nurulwafa Hussain, Ruzanna Zamzam, Shamini Rama and Sheamini Sivasampu.
Details of the evidence supporting these recommendations can be found in the CPG on Management of Schizophrenia in Adults, available on the following websites: Ministry of Health Malaysia: http://www.moh.gov.my and Academy of Medicine: http://www.acadmed.org.my. Corresponding organisation: CPG Secretariat, Health Technology Assessment Section, Medical Development Division, Ministry of Health Malaysia & contactable at htamalaysia@moh.gov.my


