Abstract
Background:
Self-care plays an important role in diabetes management. One of the instruments used to evaluate self-care in patients with diabetes is the Summary of Diabetes Self-Care Activities (SDSCA) questionnaire. A validated instrument in the Malay language is used to assess self-care practice among children and adolescents with diabetes in Malaysia.
Objective:
To translate and evaluate the psychometric properties of the revised version of the SDSCA questionnaire in the Malay language.
Methods:
Forward and backward translations were performed. An expert panel reviewed all versions for conceptual and content equivalence. The final version was administered to paediatric patients with diabetes between August 2006 and September 2007. Reliability was analysed using Cronbach’s alpha and validity was assessed using exploratory factor analysis.
Results:
A total of 117 patients aged 10–18 years were enrolled from nine hospitals. The reliability of overall core items was 0.735 (with item 4) while the reliabilities of the four domains were in the range of 0.539–0.838. As core item number 4 was found to be problematic and it was subtituted by item 5a (from the expanded SDSCA) to suit local dietary education and practice; and the reliabilities of the overall core item (0.782) and the four domains (0.620 – 0.838) improved. Factor loadings of all the items were greater than 0.4, loaded into the original domains, and accounted for 73% of the total variance.
Conclusion:
The Malay translation of the revised English SDSCA is reliable and valid as a guide for Malaysian children and adolescents suffering from diabetes.
Keywords: Children, Adolescents Diabetes self-care, Malay-translated version of SDSCA
Introduction
The prevalence of Diabetes mellitus is rising rapidly and the number of people with diabetes is projected to increase from 285 million in 2010 to 439 million in 2030.1 Children and adolescents are not spared from this.1, 2 Of the estimated 479,600 children with type 1 diabetes worldwide, 24% are from Southeast Asian countries.3 Type 2 diabetes is also becoming more prevalent among adolescents in these countries. In Malaysia, the Diabetes in Children and Adolescents Registry (DiCARE) reported that among children and adolescents with diabetes in 2006–2007 17.5% had newly diagnosed type 2 diabetes.4
Self-care practices are considered a core component of diabetes care.5–9 Adequate self-care has been shown to improve blood glucose levels, glycosylated hemoglobin (HbA1c), and dietary habits10. A diabetes self-care activities measure, together with glycaemic control, can provide essential data for clinicians, diabetes educators, and patients to evaluate and modify treatment.11 In a busy diabetes clinic with inadequate support staff, it is essential to have a simple measure of diabetes self-care activities that is both valid and reliable.
The Summary of Self-Care Diabetes Activities (SDSCA) questionnaire11 is in the public domain and freely accessible. This self-report instrument measures levels of diabetes self-care across different components of the diabetes regimen over the previous seven days. The original SDSCA was a 12-item scale developed to assess four aspects of diabetes regimen: diet, exercise, glucose testing, and diabetes medications.12 The most recent revised version of the SDSCA questionnaire, based on seven studies, has been reduced to 11 items.11 The revised version added items on foot care and cigarette smoking, which may need to be modified or deleted for use in children with diabetes. It also provides 14 additional items that could be utilised to address specific self-care questions such as medication use. Respondents are asked to circle how many days in the past seven days they displayed a diabetes-specific behaviour. Response choices range from 0 to 7, with higher scores indicating better performance of self-care activities.
This instrument has been designed to measure diabetes self-care activities among type 1 and type 2 diabetes mellitus patients.12 Most previous studies involved adults with diabetes, although a large age range was included.11 The same questionnaire had been successfully adapted for adolescents as young as 12 years old with type 1 diabetes11. Its use in past studies indicated that the SDSCA is a multi-dimensional measure of diabetes self-management with adequate internal and test–retest reliability.
To date, there has been no reliable and validated instrument in Malay, which is the national language of Malaysia. Although it would have been ideal to develop a local instrument, due to resource constraints we opted to adapt, translate, and test the revised SDSCA instrument to measure diabetes self-care practices. This study was conducted to assess the cross-cultural adaptation and to validate the revised SDSCA questionnaire which had been translated into Malay.
Methods
This was a multicentre cross sectional study. A sub-study for test-retest and a follow-up was conducted two weeks after the baseline study. The revised SDSCA questionnaire was chosen for this study because it is simple, reliable, and valid.11 Permission to use and translate the questionnaire was obtained from the author. The study was conducted in three phases (see Figure 1 for study flow diagram) from August 2006 to September 2007. Phase 1 consisted of forward and backward translation of the revised English version to Malay; Phase 2 involved pre-testing the pre-final Malay version; and Phase 3 was the validation study. This study was approved by the University Malaya Medical Centre Ethics Committee, Hospital Universiti Sains Malaysia Ethics Committee and Ministry of Health’s Medical and Research Ethics Committee.
Figure 1.
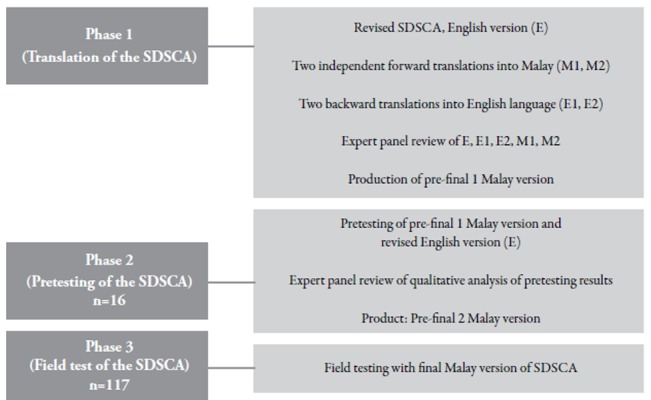
Overview of the study flow process of cross-cultural adaptation and validation of the (SDSCA) questionnaire
Phase 1 (Translation process)
The translation followed the EuroQoL translation guidelines,13 with the aim of preserving content and meaning. During this phase, two forward translations were completed: one by a clinician who was involved in diabetes care for the young (M1)(not blinded to the study) and the other by a certified translator (M2) from the Malaysia National Institute of Translation, (blinded to the study). Both the M1 and M2 versions were back-translated into English (E1 and E2) by a different clinician and a certified translator. orward and backward translations were done by the pairs independently. The researchers and the translators then formed the expert panel to review all five versions (the original, two forward translations, and two backward translations) to reconcile the discrepancies. The Malay version (either M1 or M2) that produced the back-translation (either E1 or E2) that was closest to the revised English version (E) was chosen as the pre-final 1 SDSCA Malay version. This version, together with the revised English version (E), was pretested on 16 patients.
Phase 2 (Pretest)
We performed a pretest of the pre-final 1 Malay version on July 3 (time 1) and July 17 (time 2), 2007, at the Pediatric Clinic, University Malaya Medical Centre. Seven adolescents with diabetes aged 11–18 years were involved; two had type 2 diabetes. All the patients passed a fluency test that required them to read a short passage from a local English daily and to translate it into Malay. During the pretest, each patient provided demographic data and completed two versions (prefinal 1 and original English version) of the SDSCA questionnaire. The Malay and English versions were administered in random sequence. This was followed by a focus group discussion to investigate the clarity, comprehensibility, and suitability of the text in the translated questionnaire.
To determine the stability of the pre-final 1 Malay version of SDSCA, we recruited another nine adolescents with diabetes from the same centre, who were fluent in both English and Malay. The questionnaires were administered to them on two occasions and two weeks apart. They completed both English (E) and Malay (pre-final 1) versions on the first occasion and only the Malay (pre-final 1) version on the second occasion. The outcome was then analysed by an expert panel, which generated the pre-final Malay version that later became the final version.
Phase 3 (Validation)
The final Malay version of the SDSCA was field-tested in nine paediatric clinics of the Ministry of Health and in university hospitals throughout the country. All eligible patients who attended their routine diabetes clinic follow-up visits on the day the study was conducted were approached individually (face-to-face) by the investigator or research personnel and were given informational materials describing the study. Those who wanted to participate were recruited. The inclusion criteria were children and adolescents with diabetes mellitus aged 10–18 years who could read and write in Malay, irrespective of the duration and type of treatment received. Patients known to have cognitive impairment or severe psychosis were excluded.
For Phase 3, we calculated the sample size based on the rule of thumb for exploratory factor analysis. Gorsuch proposed minimum sample of 1:5 per item.14 Since SDSCA contained 10 items, the minimum sample size is 50 patients. We recruited more than 100 patients to accommodate drop out. Patients and their parent(s) gave written consent and each patient was given two self-administered questionnaires: (a) demographic survey, and (b) the final Malay version of the SDSCA which were completed within 15–20 minutes.
Data analysis
Phase 1 and 2: The cross cultural adaptation of the Malay translated version (M1 and M2) was on the basis of face validity, content validity, and test–retest reliability. Face validity was assessed via patient’s review; content validity was verified by an expert panel; and test–retest reliability was evaluated using the kappa agreement coefficient.
Phase 3. The internal consistency of the final Malay version of SDSCA was evaluated using Cronbach’s alpha, with values of more than 0.5 considered as acceptable and 0.7 or more considered good.15 For construct validity, exploratory factor analysis (EFA) was applied using the principal component analysis (PCA) extraction method with Varimax rotation. Kaiser-Meyer-Olkin values, communalities, total variance explained, and factor loadings were calculated to evaluate the factor solution. Factor loadings of 0.4 or more were considered a good fit.16 Statistical analyses were conducted using PASW 18.0 (version 18.0; Chicago, IL).
Results
Pretest (Phase 2)
In general, patients (n=16) agreed that the final Malay version was clearer and easier to comprehend. One patient had difficulty understanding item 5a (“membahagikan pengambilan,” which means “dividing the intake,” to be replaced with “mengambil,” which means “to take”). Patients commented that there were three questions which they believed were irrelevant to them: item 7a (not applicable to type 2 diabetes patients not on insulin), item 8a (not applicable to type 1 diabetes), and item 14a (not applicable to non-smokers). The expert panel decided to overrule all comments, as the initial translation of item 5a conveyed more accurate meaning or emphasis while items 7a, 8a, and 14a maintained the questionnaire’s original structure. The proportion agreement for each item between the English version and the pre-final 1 Malay version ranged from 77.8% to 97.8%. For test–retest reliability, the proportion agreement of each item of the Malay translated version on time 1 and time 2 ranged from 60.0% to 90.0%.
Phase 3
A total of 117 patients with a mean age of 13.9 (SD 2.7) years participated in the study. About one-third of the patients (35.0%) were 10-13 years. There were 55 (47.0%) male patients, with Malays being the majority (Table 1). Although the revised version of the SDSCA questionnaire was used for this study, reliability and validity were tested only on core items applicable to both type 1 and type 2 diabetes patients. The overall reliability was 0.735 with the reliabilities of the four domains ranging from 0.539 to 0.838 (Table 2).
Table 1. Demographic characteristics of patients.
| Profile characteristics | frequency (%) |
|---|---|
| Mean Age (in year)a | 13.9 (2.7) |
| Age group (yr) | |
| 10 – <13 | 41(35.0) |
| 13 – <16 | 41(35.0) |
| 16 – <19 | 35(30.0) |
| Gender | |
| Male | 55(47.0) |
| Female | 62(53.0) |
| Ethnicity | |
| Malay | 70(59.8) |
| Chinese | 27(23.1) |
| Indian | 15(12.8) |
| Other | 5(4.3) |
Table 2. Internal consistency of the final Malay version of the revised SDSCA questionnaire.
| Domain | Items | Cronbach’s alpha |
|---|---|---|
| Overall | 1 – 10 | 0.735 |
| Diet | 1 – 4 | 0.539 |
| General diet | 1 – 2 | 0.903 |
| Specific diet | 3 – 4 | -0.094 |
| Exercise | 5 – 6 | 0.749 |
| Blood sugar | 7 – 8 | 0.838 |
| Foot care | 9 – 10 | 0.620 |
As the diabetes-specific diet subscale (items 3 and 4) was found to have a low Cronbach’s alpha (-0.094) value, we performed EFA, which showed that item 4 appeared to load into a different domain (i.e., glucose monitoring) with a factor loading of -0.427 (Table 3). To improve the factor solution and to suit local dietary education and practices, item 4 was substituted by item 5a from the expanded version. With this change, internal consistency improved for overall, diet, and diabetes-specific diet scales, from 0.735 to 0.782, from 0.539 to 0.742, and from -0.094 to 0.348, respectively (Table 5). By substituting item 5a for item 4, the item loaded into the original domain (diet) and the factor loading improved to 0.712. In addition, all the items were into their original domains and had factor loadings greater than 0.4. Overall, they accounted for 73% of the total variance (Table 4). Analysis of a subgroup of patients aged 10-13 years showed that the reliability and validity were consistent with the results of analysis using data from all patients (Tables 4 and 5). The similarities and differences between the revised Malay version (after substituting item 5a for item 4) and original revised English SDSCA is summarised in Table 6.
Table 3. Factor solution of the items in the final Malay version of the revised SDSCA.
| Items | Components | |||
|---|---|---|---|---|
| Diet | Sugar | Exercise | Foot care | |
| 2. Follow a healthy eating plan (on average per week, over the past month) | 0.919 | |||
| 1. Follow a healthy eating plan in the last week | 0.862 | |||
| 3. Eat five or more servings of fruits and vegetables | 0.537 | |||
| 8. Test your blood sugar according to the number of times recommended by your health care supervisor | 0.878 | |||
| 7. Test your blood sugar | 0.865 | |||
| 4. Eat high fat foods such as red meat or full-fat dairy products | -0.427 | |||
| 6. Participate in a specific exercise session | 0.879 | |||
| 5. Participate in a 30-minute exercise session | 0.858 | |||
| 10. Inspect the inside of your shoes | 0.806 | |||
| 9. Check your feet | 0.731 | |||
Table 5. Summary of exploratory factory analysis and reliability results of the final Malay version of the SDSCA questionnaire.
| With item 4 All patients | With item 5a All patients | With item 5a Subgroup(10–13 | |
|---|---|---|---|
| Exploratory Factor Analysis | |||
| KMO* | 0.67 (p<0.001) | 0.70 (p<0.001) | 0.63 (p<0.001) |
| Communalities | 0.493–0.893 | 0.602–0.944 | 0.709–0.918 |
| Total variance | |||
| Explained | 71% | 73% | 81% |
| Factor solution | Valid solution except item 4 | Valid solution | Valid solution |
| Reliability | |||
| Overall | 0.735 | 0.782 | 0.804 |
| Diet | 0.539 | 0.742 | 0.760 |
| General diet | 0.903 | 0.903 | 0.874 |
| Specific diet | -0.094 | 0.348 | 0.400 |
| Exercise | 0.749 | 0.749 | 0.809 |
| Blood sugar | 0.838 | 0.838 | 0.898 |
| Foot care | 0.620 | 0.620 | 0.686 |
* KMO = Kaiser-Meyer-Olkin; p value of Bartlett’s Test of Sphericity
Table 4. Factor loadings* of the items in the final Malay version of the revised SDSCA questionnaire among all patients and patients aged 10–13.
| Items | Components | |||
|---|---|---|---|---|
| Diet | Sugar | Exercise | Foot care | |
| 2. Follow a healthy eating plan (on | 0.870 | |||
| average per week, over the past month) | 0.874 | |||
| 1. Follow a healthy eating plan in the | 0.813 | |||
| last week | 0.646 | |||
| 5a Space carbohydrates evenly | 0.712 | |||
| through the day | 0.607 | |||
| 3. Eat five or more servings of fruits | 0.449 | |||
| and vegetables | 0.794 | |||
| 7. Test your blood sugar | 0.902 | |||
| 0.912 | ||||
| 8. Test your blood sugar according to | 0.877 | |||
| the number of times recommended | 0.905 | |||
| by your health care supervisor | ||||
| 6. Participate in a specific exercise | 0.892 | |||
| session | 0.852 | |||
| 5. Participate in a 30-minute exercise | 0.848 | |||
| session | 0.884 | |||
| 10. Inspect the inside of your shoes | 0.875 | |||
| 0.887 | ||||
| 9. Check your feet | 0.759 | |||
| 0.738 | ||||
* Factor loadings without italic = overall. Factor loading in italic = children aged 10–13
Table 6. Comparison of the original English, revised English and revised Malay SDSCA questionnaire.
| Domain/Item | Original English SDSCA | Revised English SDSCA | Revised Malay version |
|---|---|---|---|
| 1. General diet | |||
| 1. Follow healthy | Y | Y | Y |
| diet/Recommended diet (last 7 days) | |||
| 2. Limited-calorie diet for diabetics | Y | N | N |
| 3. Fruits and veg. (fiber) (last 7 days) | Y | Y | Y |
| 4. High-fat food (fatty food)(last 7 days) | Y | Y | N (replaced with item 5a) |
| 5. Sweet food | Y | N | N |
| 6. Follow healthy diet plan (past 1 month) | N | Y | Y |
| 2. Exercise | |||
| 1. 20 mins (last 7 days) | Y | N | N |
| 2. 30 mins (last 7 days) | Y (%) | Y (number of days) | Y |
| 3. Specific exercise session (last 7 days) | Y | Y | Y |
| 3. Blood glucose testing | |||
| 1 Test blood (last 7 days) | Y | Y | Y |
| 2. Test blood per recommendation (last 7 days) | Y | Y | Y |
| 4. Medication | (moved to Additional Items) | (moved to Additional Items) | |
| 1. Taking diabetes medication (last 7 days) | N | Y | Y |
| 2. Taking insulin injection (last 7 days) | Y | Y | Y |
| 3. Taking diabetes pills (last 7 days) | Y | Y | Y |
| 6. Foot care | |||
| 1. Inspect feet (last 7 days) | N | Y | Y |
| 2. Inspect inside of shoes (last 7 days) | N | Y | Y |
| 7. Smoking | |||
| 1. Smoke (last 7 days) | N | Y | N (unsuitable for children) |
| Additional items (extended version) | |||
| 1a. Advice on diet | Y | Y | |
| 2a. Advice on exercise | Y | Y | |
| 3a. Advice on blood testing | Y | Y | |
| 4a. Advice on medication | |||
| 5a. Diet – balancing | Y | Y | |
| carbohydrate intake (last 7 days) | Y | Y (replace item 4) | |
| 6a. Medication – as above | |||
| 7a. Medication – as above | Y | Y | |
| 8a. Medication – as above | Y | Y | |
| 9a. Foot care – wash feet (last 7 days) | Y | Y | |
| 10a. Foot care – soak feet (last 7 days) | |||
| 11a. Foot care – dry in between toes after wash (last 7 days) | Y | Y | |
| 12a. Smoking – asked about smoking | Y | N (not suitable for children) | |
| 13a. Smoking – advice to stop smoking | Y | N (not suitable for | |
| 14a. Smoking – the last time smoking | Y | N (not suitable for children) |
* Y=Yes, N=No
Discussion
The Malay version (translated) was found to be equivalent to the revised English version. We did not face major challenges in translating and adapting the English SDSCA into the Malay language as we had the support and cooperation of the expert panel and the patients. During the pre-test, the patients felt that the Malay-translated version of the SDSCA was easier to understand. However, a few issues were raised about the suitability of the words (one item) and the appropriateness of items related to their type of diabetes (three items). These concerns were overruled by the expert panel, which deemed all items to be appropriately translated with conceptual content similar to the revised English version. By testing this questionnaire on bilingual patients, the proportion agreement for the revised English version and the pre-final 1 Malay version for each item demonstrated good agreement.
For test–retest reliability, the proportion agreement in this study was higher than in previous study11, indicating stability of responses across the two time intervals. This may be explained by the shorter time interval in our study (two-weeks), compared with the three-month interval in previous studies11. The shorter interval may have resulted in less variation in self-care practices and lifestyle. Given its face validity and stability, no changes were made, and the prefinal Malay version was subjected to field testing (Phase 3).
The internal consistency of all domains in the final Malay version of the SDSCA questionnaire was acceptable. However, we discovered that the diabetes-specific diet subscale was not reliable and performed poorly in factor analysis. This domain was also found to be the least reliable item in the original English SDSCA version as well as the Spanish version.10, 12 Item 4 (“On how many of the last SEVEN DAYS did you eat high-fat foods such as red meat or full-fat dairy products?”) appeared problematic, probably because of the poor understanding of the concept of high-fat food among these patients. Item 4 is reverse coded according to the SDSCA scoring guidelines12, but the Cronbach’s alpha remained negative despite reverse scoring. To improve internal consistency of the diet scales, item 5a (“On how many times in the last SEVEN DAYS did you space carbohydrates evenly through the day?”) from the expanded version was substituted for item 4, which resulted in the improvement of the reliability for overall and diet domains in the revised Malay version. This was similarly observed in the Spanish version.10 Item 4, therefore, may need a separate assessment with a more-detailed questionnaire addressing specific types of high-fat food and the frequency of intake.
Factor analysis performed on the revised Malay version found that all items were loaded in their original domains, providing strong evidence that the questionnaire is constructively valid. Similar results were found when analysis was limited to younger patients, aged 10–13 years. These findings indicate that the revised Malay version of SDSCA may be used in younger children between ages 10–13 years, even though the original/revised English SDSCA questionnaire was validated in patients aged 12 years and older. To our knowledge, this is the first study where translation and validation of the English SDSCA into any language was performed exclusively among children and adolescents, aged 10-18 years with both type 1 and type 2 diabetes.
Based on the above findings we decided to substitute item 4 with item 5a for clinical use and future studies. This version, which we have named revised Malay version of SDSCA, will be made widely available in clinics for future use. However, we admit that this revised Malay version may not be suitable for some patients whose primary language is not Malay, especially children who attend the vernacular schools (i.e., Indian or Chinese primary schools) and whose main languages are Tamil and Mandarin respectively. Hence, these children may have difficulty understanding either the revised Malay or revised English SDSCA version. There are some children who are more proficient in English, and may find the revised English version more appealing than the revised Malay version.
This questionnaire is potentially very useful during an outpatient visit as a quick assessment of diabetes self-care to identify areas for improvement. This questionnaire may also be used to monitor changes in a patient’s self-care activities over time. Regular monitoring of self-care practice is likely to promote compliance in diabetes management and consistency in self-care.
We recommend that this questionnaire be used for children older than 10 years who are fluent in Malay, and that future research should validate this Malay version of SDSCA questionnaire among adult Malaysian patients. In addition, prospective studies to evaluate the impact of regular usage of this questionnaire on the metabolic outcome of children and adolescents with diabetes should be conducted.
In summary, the Malay-translated version of the revised SDSCA questionnaire is highly reliable and valid, and may come in handy for Malaysian children aged 10–18 years and adolescents with diabetes.
Acknowledgements
We extend our appreciation to the Director General of Health for permission to publish this work and convey our deepest gratitude to the National Institute of Health, Ministry of Health, Malaysia for grant conferment. We also thank Dr. Deborah Toobert, the author of the English original version of SDSCA, for permission to use and translate the questionnaire. We are grateful to the dedicated research assistants, Azdayanti Muslim, Gunavathy Selvaraj, Norwani Rosli, and Nurul Husna Mohammad Patel, for their tireless effort in managing the project. We are also indebted to the doctors and nurses at the Paediatric Institute of Kuala Lumpur Hospital, and the various paediatrics and medical clinics in the University Malaya Medical Centre, Putrajaya Hospital, Raja Permaisuri Bainun Hospital in Ipoh, Sultanah Nur Zahirah Hospital in Kuala Terengganu, Melaka Hospital in Melaka, Sultanah Aminah Hospital in Johor Bharu, Sultanah Bahiyah Hospital in Alor Setar, and Universiti Sains Malaysia Hospital in Kota Bharu.
References
- 1.The Diabetes Atlas. 4th. Brussels: International Diabetes Federation; 2009. International Diabetes Federation. [Google Scholar]
- 2.The Diabetes Atlas. 3rd. Brussels: International Diabetes Federation; 2006. International Diabetes Federation. [Google Scholar]
- 3.Low LCK. The epidemic of type 2 diabetes mellitus in the Asia-Pacific region. Pediatric Diabetes. 2010;11:212–5. doi: 10.1111/j.1399-5448.2010.00682.x. [DOI] [PubMed] [Google Scholar]
- 4.Fuziah MZ, Hong JYH, Zanariah H. et al. A national database on children and adolescent with diabetes (e-DiCARE): results from April 2006 to June 2007. Med J Malaysia. 2008;63 (Suppl. C):37–40. [PubMed] [Google Scholar]
- 5.Goodall TA, Halford WK. Selfmanagement of diabetes mellitus: a critical review. Health Psychol. 1991;10:1–8. doi: 10.1037//0278-6133.10.1.1. [DOI] [PubMed] [Google Scholar]
- 6.Johnson SB. Health behavior and health status: concepts, methods and applications. J Pediatr Psychol. 1994;19:129–41. doi: 10.1093/jpepsy/19.2.129. [DOI] [PubMed] [Google Scholar]
- 7.Johnson SB. Psychosocial factors in juvenile diabetes: a review. J Behav Med. 1980;3:95–116. doi: 10.1007/BF00844916. [DOI] [PubMed] [Google Scholar]
- 8.McNabb WL, Quinn MT, Murphy DM, Thorp FK, Cook S. Increasing children’s responsibility for diabetes self-care: the In Control study. The Diabetes Educator. 1994;20:121–4. doi: 10.1177/014572179402000206. [DOI] [PubMed] [Google Scholar]
- 9.McNabb WL. Adherence in diabetes: Can we define it and can we measure it? Diabetes Care. 1997;20:215–8. doi: 10.2337/diacare.20.2.215. [DOI] [PubMed] [Google Scholar]
- 10.Vincent D, McEwen MM, Pasvogel A. The validity and reliability of a Spanish version of the Summary of Diabetes Self-Care Activities questionnaire. Nurs Res. 2008;57:101–6. doi: 10.1097/01.NNR.0000313484.18670.ab. [DOI] [PubMed] [Google Scholar]
- 11.Toobert D, Hampson S, Glasgow RE. The Summary of Diabetes Self-Care Activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23:943–50. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 12.Toobert DJ, Glasgow RE, Bradley C. Handbook of Psychology and Diabetes. Chur, Switzerland: Harwood Academic; 1994. Assessing diabetes self-management: the Summary of Diabetes Self-Care Activities questionnaire; pp. 351–75. [Google Scholar]
- 13.EuroQol Group. Translation guidelines. 2003. [accessed 2005 Sept 8]. Available from: www.euroqol.org/web/files/Translation_guidelines.pdf. [Google Scholar]
- 14.Gorsuch R.L. 2nd. Hillsdale, NJ: Erlbaum; 1983. Factor analysis. [Google Scholar]
- 15.Nunnally JC. 2nd. New York: McGraw Hill; 1978. Psychometric theory. [Google Scholar]
- 16.Raubenheimer JE. An item selection procedure to maximize scale reliability and validity. S Afr J Industrial Psychol. 2004;30:59–64. [Google Scholar]


