INTRODUCTION
Mediastinal shift (upper and lower) is a clinical and radiological marker of significant importance, which at times helps to determine the aetiological cause of the underlying pathology. Tracheal shift is an indicator of upper mediastinal shift, while a shift in the position of the heart indicates a lower mediastinal shift. Since the pleural cavity is confined by the rib cage, in case of a moderately large pleural effusion, the structures in the thoracic cavity normally get ‘pushed’ to the opposite side resulting in a shift of the upper and lower mediastinum. This is clinically and radiologically detected by a shift in the trachea and heart to the side opposite to the pleural effusion. This is commonly seen in pleural effusions resulting from tuberculosis or other infections. However, in some cases even a large pleural effusion fails to shift the mediastinum to the opposite side. In fact, in some cases, the trachea and heart are observed to be central or even shifted to the same side as the effusion. This finding is of immense importance as it is a clinical indicator of a more serious condition which needs prompt diagnosis and urgent management. We report here, one such case of a middle-aged man who presented to the emergency department with complaints of increasing breathlessness and whose clinical and radiological examination revealed a moderately large right-sided pleural effusion with the trachea and heart also shifted to the right side.
CASE REPORT
A 55-year-old man came to the Acccident and Emergency department with complaints of rapidly increasing breathlessness and right-sided chest pain since 10 days. He was a smoker, smoking 30 cigarettes per day for the past 28 years. He worked in a consultancy firm as an officer. There was no history of cough, haemoptysis, fever or loss of appetite. However, the patient claimed that he had lost 12 kg weight in the last three months.
On examination, the patient appeared to be underweight and breathless. His accessory muscles of respiration were active. His pulse rate was 92 beats per minute and the respiratory rate was 26 breaths per minute. His blood pressure (BP) was 132/86 mmHg. He was not cyanosed. His finger nails showed nicotine staining, however, there was no clubbing. Cervical and axillary lymph nodes were not palpable. On systemic examination of his chest, the trachea was slightly deviated to the right side. The apex beat was palpable in the fifth left intercostal space, 1 cm medial to the mid-clavicular line. On palpation, there was chest wall tenderness over the right side. Chest wall movements were significantly reduced on the right side and tactile fremitus was absent below the third intercostal space on the right side. On percussion, a stony dull note was heard below the right inframammary region and in the right infrascapular region. On auscultation, air entry was diminished in the right infraclavicular and interscapular regions while it was completely absent below the right inframammary region anteriorly and in the right infrascapular region. Tubular bronchial breath sounds were heard in the right interscapular region. Vocal resonance was absent in the inframammary and infrascapular regions on the right side while it was increased in the right interscapular region. A right- sided pleural effusion was suspected. However, the medical officer on duty wondered why the trachea was deviated to the same side as the pleural effusion (right side) and the cardiac apex was not shifted outwards (left side).
A chest radiograph, PA view, was done. On viewing, the chest radiograph appeared to be fairly well-centralised. It showed the presence of a moderately large pleural effusion on the right side (Figure 1, single large black arrow) with lateral upward sloping of a meniscus-shaped contour. The fluid obliterated the right hemi-diaphragmatic contour. The trachea was also slightly deviated to the right side (Figure 1, small black arrows). It appeared to be a moderately large pleural effusion as the fluid occupied between 25-50% of the hemithorax.1 When the consultant physician saw the patient, a discussion ensued regarding the conflicting position of the trachea and lower mediastinum (heart), vis-à-vis the pleural effusion.
Figure 1:
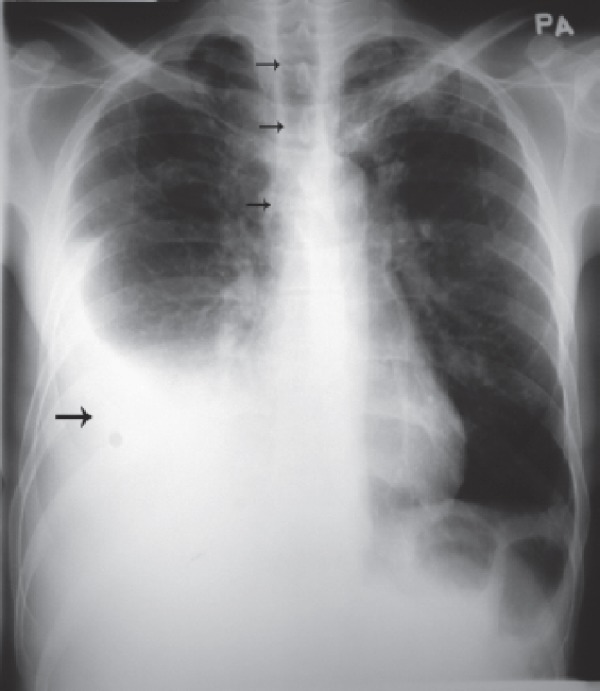
Chest radiograph of a patient with a right-sided pleural effusion. The pleural fluid is seen as opacity (single large black arrow) with lateral upward sloping of a meniscus- shaped contour. The right diaphragmatic contour is also completely obliterated, indicating presence of fluid in the right pleural space. In spite of a moderately large right pleural effusion, the trachea appears to be slightly shifted to the right side (as depicted by small black arrows), and the heart also does not appear to be shifted to the left side, thereby indicating an underlying lung pathology on the right side. A right lower lobe collapse was subsequently diagnosed on high resolution computed tomography (HRCT) chest scan, as a consequence of right lung carcinoma.
DISCUSSION
It was apparent both clinically and radiologically that the patient had a moderately large pleural effusion on the right side as the fluid occupied between 25-50% of the hemithorax.1However, the trachea and lower mediastinum (heart) appeared to be shifted to the same side as the effusion.
To understand the mechanism behind the tracheal and cardiac shift to the same side as the effusion, it is at first important to determine the potential cause of the effusion. In view of the history of chronic heavy smoking, significant weight loss in a relatively short duration of time accompanied by breathlessness, chest pain and chest wall tenderness, it was likely that the patient had a malignant pleural effusion. Normally, in case of a pleural effusion, the trachea (upper mediastinum) and the heart (lower mediastinum) shift to the opposite side, as the fluid in the pleural space causes a ‘push’ to the opposite side. In such cases, it must be remembered that even though the fluid causes some amount of ‘compression collapse’ of the underlying lung (which would technically cause a ‘pull’ of the mediastinum to the same side), the ‘push’ by the fluid within the enclosed pleural cavity overcomes that, and overall there is a shift of the upper and lower mediastinum to the opposite side. This is commonly seen in case of tuberculous pleural effusion and effusion due to other infective causes.
However, in case the trachea and heart are found to be central or shifted to the same side as the fluid both clinically and radiologically, a malignant pleural effusion’ must be suspected. Paradoxically, in malignant pleural effusions it has been observed that even though the effusion is usually large, the upper and lower mediastinum (as represented by the trachea and heart, respectively) are not significantly shifted to the opposite side. In fact, in many cases the mediastinum is either central or shifted to the same side as the fluid.
The mechanism for this is as follows:
In case of a primary lung malignancy with an underlying effusion, a central tumour mass obstructing a bronchus causes a significant lung collapse distal to the site of obstruction. This results in a significant pull on the mediastinum (upper and lower) to the same side as the lesion. This pull, caused by the collapsed lung, is so great that it ‘overcomes’ the push caused by the underlying fluid, resulting in a net shift of the mediastinum to the same side as the fluid (effusion). Hence, in these cases, the trachea and heart either remain central or get shifted to the same side as the effusion.
CONCLUSION
In conclusion, it can be surmised that the tracheal and lower mediastinal (heart) shift is an important clinical and radiological marker in the diagnosis of a suspected malignant pleural effusion. If, clinically and radiologically there is a large amount of fluid in the pleural cavity and inspite of that the trachea and heart are not significantly shifted to the opposite side, or are in fact central or shifted to the same side as the effusion, a significant underlying lung collapse must be suspected. This can usually only occur if there is a tumour mass obstructing a bronchus, thereby causing a significant lung collapse distal to the site of obstruction.
Consequently, it would be useful for hospital doctors and family physicians to be aware of this important clinical and radiological sign, as they would then be able to suspect the presence of an underlying malignancy early on, when the patient first presents with symptoms and signs suggestive of a pleural effusion.
An ultrasonography and HRCT chest scan were subsequently done which confirmed the presence of a moderately large pleural effusion (approximately 2000 ml) with a tumour mass underlying it, which was obstructing the right lower lobe bronchus resulting in a significant right lower lobe collapse. Further investigations including pleural fluid aspiration and tumour biopsy confirmed the presence of a primary lung malignancy.
REFERENCE
- Light RW, Rogers JT, Cheng DS. et al. Large pleural effusions occurring after coronary artery bypass grafting. Cardiovascular Surgery Associates, PC. Ann Intern Med. 1999;130((11)):891–6. doi: 10.7326/0003-4819-130-11-199906010-00004. [DOI] [PubMed] [Google Scholar]


