Abstract
Patients with Wellen's syndrome often present with chest pain and found to have specific precordial T-wave changes on the electrocardiogram (ECG). They subsequently develop a large anterior wall myocardial infarction. These specific electrocardiographic abnormalities are associated with critical stenosis of the proximal left anterior descending coronary artery (LAD). This syndrome is often under-recognised and has fatal consequences; it is, therefore, also known as the widow maker. We highlight a case of a 39-year old gentleman who had a history of coronary artery disease and typical ECG characteristics of Wellen's syndrome.
Keywords: Wellen's syndrome, widow maker, myocardial infarction
Introduction
Wellen's syndrome occurs in a group of patients who have unstable angina presenting with chest pain and specific precordial T-wave changes. They are at risk of developing a large anterior wall myocardial infarction1. In most patients with Wellen's syndrome, the cardiac enzymes are not elevated.2
Recognising these ECG abnormalities is crucial because they signal a preinfarction stage of underlying coronary artery disease, which, if left untreated, often progresses to an anterior myocardial wall infarction. Previous studies have shown that the development of anterior myocardial infarction is rapid upon the onset of Wellen's syndrome.1 Unfortunately, medical management alone is not enough to halt the progression of this disease. Hence, Wellen's syndrome is also known as the “widow maker”.
This case report describes a patient with Wellen's syndrome. In view of the urgency of treating this syndrome and the potential fatality, it is important that frontline doctors, such as family and emergency physicians, recognise these and the ECG pattern when evaluating patients presenting with chest pain. Wellen's' syndrome and its characteristics, the criteria for diagnosis, and a discussion of its implications and medical management will be presented.
Case Report
A 39-year old Malay man presented to our ED with frequent chest pain of several weeks. He experienced chest pain while doing light work; sometimes the pain occurred even while he was resting. The patient had a past medical history of coronary artery disease (CAD), hypertension, and hyperlipidaemia which he received regular treatment. His previous ECG approximately done 3 months earlier showed a sinus rhythm, 78 beat per minute, normal axis with biphasic T wave at lead V1-V2. At lead aVL, V3 and V4, the T waves were inverted and symmetrical. He underwent exercise stress test (EST) a week later but the result was inconclusive as he was unable to complete the test due to lethargy. He was asked to undergo dobutamine stress test two months later but he didn't turn up.
During the physical examination, he was not experiencing chest pain. His vital signs and cardiovascular examination were normal. The ECG did not show significant changes (Figure 1) and the troponin T level was normal. The emergency physician diagnosed him to have Wellen's syndrome and was admitted to the ward. He refused angioplasty and further intervention due to financial constraint.
Figure 1.
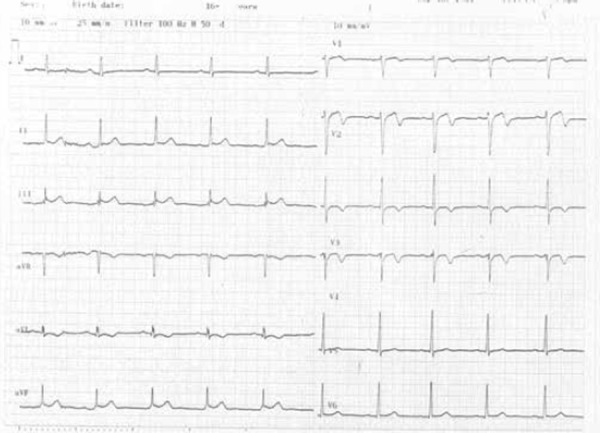
Showing the ECG abnormalities during admission (at rest and pain free)
Discussion
In 1982, Wellen and his colleagues first described a characteristic ECG pattern of T waves in the precordial leads that were associated with a critical stenosis of the proximal left anterior descending coronary artery.1 In Wellen's syndrome, T-wave changes usually occur during a pain-free interval when other evidence of ischaemia or unstable angina may be absent. Although these patients may initially respond well to medical treatment, they have poor prognosis with conservative therapy and often require aggressive treatment such as angioplasty or coronary artery bypass graft. The characteristics of Wellen's syndrome include:2
Recent history of chest pain
Little or no elevation of cardiac enzymes
Symmetric, deep T wave or biphasic T wave in V2-V5 or V6 during pain free period and
No precordial Q waves or loss of R waves
Minimal (<1mm) ST elevations
In Wellen's syndrome, a patient often presents with intermittent chest pain and there is a characteristic T-wave on the ECG during a pain-free period. It represents a critical stenosis of the LAD, a branch of left coronary artery that, if progressed to an occlusion, may result in an acute anterior wall myocardial infarction. The patient requires urgent angioplasty to reopen the occlusion.3 The LAD supplies the anterior wall of the heart, including both ventricles, as well as the septum. An occlusion in this vessel can result in serious ventricular dysfunction, thus placing the patient at risk of congestive heart failure and death. In Wellen's syndrome, the patients may not present with unstable angina; some may have symptoms mimicking chronic stable angina.
Majority (76%) of the patients with Wellen's syndrome have typical ECG (type I) features showing deep, symmetrical T-wave inversions in precordial leads V2 and V3. It often involves leads V1 and V4 and occasionally leads V5 and V6.4,5 One third of Wellen's syndrome presents with biphasic T waves in leads V2 and V3 (type II).4
The diagnosis is difficult as most patients with Wellen's syndrome do not have chest pain during the visit, have normal or minimally elevated cardiac enzymes and “non-specific” ECG findings.6
The patient in this case report had typical type II ECG features suggestive of Wellen's syndrome and they were recorded while the patient was resting and pain free. The patient was asked to undergo EST to establish the diagnosis but, fortunately, the procedure was abandoned due to his poor effort tolerance. Tandy and colleagues4 reported a patient of Wellen's syndrome who, after undergoing an EST, developed an ST-elevation anterior myocardial infarction resulting in death. His death was attributed to cardiogenic shock and arrhythmia despite early administration of fibrinolytic therapy.
The ECG features of Wellen's syndrome show sensitivity, specificity and positive predictive value of 69%, 89% and 86% respectively.1 Urgent angiography is the investigation of choice and it helps to determine the extent of the disease and assist the cardiologist in making decisions whether the patient will need percutaneous coronary intervention, coronary artery bypass graft, or medical management.4,8
Summary
The ECG characteristic of Wellen's syndrome is highly specific for LAD stenosis. Primary care physicians should not focus solely on the ST segment in ECG interpretation of ischemia, but also take into account any T wave changes in a patient with chest pain and history of coronary arterty disease. It is, therefore, important to compare current and previous ECGs as this might provide clues to the diagnosis. Referral for EST or dobutamine stress test is contraindicated in Wellen's syndrome as they precipitate an acute myocardial infarction. The recommended treatment for patients with Wellen's syndrome is early intervention with either angioplasty or coronary artery bypass surgery.7
References
- 1.De Zwaan C, Bar FW, Janssen JH. et al. Angiographic and clinical characteristics of patients with unstable angina showing an ECG pattern indicating critical narrowing of the proximal LAD coronary artery. Am Heart J. Mar. 1989;117((3)):657–65. doi: 10.1016/0002-8703(89)90742-4. [DOI] [PubMed] [Google Scholar]
- 2.Nicole E Mead, Keally P O'Keefe. Wellen's Syndrome: An ominous EKG pattern. Journal of Emergencies, Trauma and Shock. Sept-Dec 2009;2((3)):206–208. doi: 10.4103/0974-2700.55347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moore KL, Dalley AF. Thorax. In:Clinically Oriented Anatomy. 4th ed. Baltimore, Maryland: Lippincott Williams & Wilkins; 1999. 135 pp. [Google Scholar]
- 4.Tandy TK, Bottomy DP, Lewis JG. Wellen's' syndrome. Ann Emerg Med. Mar. 1999;33((3)):347–51. doi: 10.1016/s0196-0644(99)70373-2. [DOI] [PubMed] [Google Scholar]
- 5.Aufderheide TP, Gibler WB, Rosen P, Barkin R. Emergency medicine: concepts and clinical practice. 4th edn. St Louis: Mosby–Year Book; 1998. Acute ischemic coronary syndromes; pp. 1688–91. [Google Scholar]
- 6.Haines DE, Raabe DS, Gundel WD, Wackers T. Anatomic and prognostic significance of new T-wave inversion in unstable angina. Am J Cardiol. 1983;52:14–8. doi: 10.1016/0002-9149(83)90061-9. [DOI] [PubMed] [Google Scholar]
- 7.John R. Kapoor. et al. Isolated Disease of the Proximal Left Anterior Descending Artery; Comparing the Effectiveness of Percutaneous Coronary Interventions and Coronary Artery Bypass Surgery. J Am Coll Cardiol Intv. 2008;1((5)):483–491. doi: 10.1016/j.jcin.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 8.Tatli E, Aktoz M, Buyuklu M, Altun A. Wellen's' syndrome: the lectrocardiographic finding that is seen as unimportant. Cardiol J. 2009;16((1)):73–5. [PubMed] [Google Scholar]


