Abstract
Introduction:
Upper respiratory tract infection (URTI) is a common encounter in primary care and mostly viral in origin. Despite frequent reminders to primary care providers on judicious use of antibiotics for URTI, the practice is still rampant.
Methods:
As part of quality improvement initiative, an intervention was designed by distributing a profiling report on individual prescriber’s performance in comparison to colleagues on usage of antibiotic for URTI. The data were generated from electronic health record in three public primary care clinics in Malaysia and emailing monthly throughout 2011 to all providers.
Results:
There were 22,328 consultations for URTI in 2010 and 22,756 in 2011 with the incidence rates of URTI among overall consultations of 15.7% and 15.9% respectively. 60 doctors and medical assistants had performed consultations during the 2 year period. Following the intervention in 2011, the prescription rate of antibiotic for URTI is significantly reduced from 33.5% in 2010 to 23.3 % in 2011. Before intervention, individual prescription rate varies from 9.7% to 88.9% and reduced to 4.3% to 50.5% after intervention.
Conclusion:
Profiling report is a potential method of changing antibiotic prescribing habit among public primary care providers in Malaysia especially if the baseline adherence was poor and higher variation of prescribing rate.
Keywords: profiling, upper respiratory tract infection, antibiotic prescription
Introduction
Upper respiratory tract infection (URTI) is a common problem seen in primary care. It is generally believed that there is over-prescription of antibiotic for URTI in general practice and its usage varies among physicians in the same locality and between countries.1,2 Teng et al. found in 1999, antibiotic prescribing rate for URTI in Malaysian private primary care setting was higher at 68.4% as compared to public clinics, at 28.7%, in a study done a year later .3,4 A similar study done in 2008 showed the overall antibiotic prescribing rate for both Malaysian private and public primary care clinics was 33.8%.5 Most URTI, however, are primarily viral in origin, only 2.4% among unselected URTI and 14% of pharyngitis are bacterial in origin. 6,7 Multi-faceted interventions, where educational interventions are applied at various levels, are considered the most effective strategy in overcoming the problem of irrational and injudicious use of antibiotics but may involve greater effort and cost.8 Physician profiling, as part of auditing and giving feedback, has also been shown to be effective in changing practice patterns, especially if the baseline adherence was low. 9,10
American Academy of Family Physicians (AAFP) defines physician profiling as an analytical tool that, via epidemiological approaches, supplies physician groups with information on physician practice patterns across various quality of care dimensions.11 The desired benefit of profiling is that analysing and comparing patterns of care will raise provider awareness of quality and will help stimulate improvement by reducing the variation in performance among physicians through audit and feedback.12
The easily accessible data from Teleprimarycare® System (TPC), an electronic health record developed by Ministry of Health, Malaysia, presented an opportunity for using provider profiling report as an interventional method to improve the antibiotic prescription for URTI. There were 9 public primary care clinics with doctors in the State of Perlis, Malaysia, out of which 3 clinics were equipped with TPC. TPC was initiated in 2006 at Kangar Health Clinic (HC), which is the biggest clinic, followed by Beseri HC and Simpang Empat HC in 2008. By 2009; all three clinics used this system entirely for general outpatient consultation.
Methods
A before and after observational study was conducted to determine the effectiveness of profiling report in reducing the antibiotic prescription rate for URTI. Baseline data of year 2010 was considered as pre-intervention. The intervention was done through monitoring of antibiotic usage for URTI by the individual provider and emailing the profiling report monthly from January to December 2011 as shown in figures 1 and 2.
Figure 1:
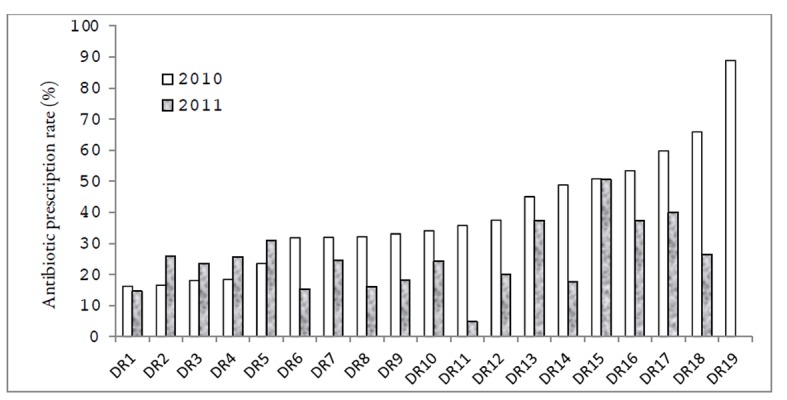
Profiling the individual doctor (DR) antibiotic prescription rate for URTIs in 2010 and 2011
Figure 2:

Profiling the individual Medical Assistant (MA) antibiotic prescription rate for URTIs in 2010 and 2011
Data was extracted from TPC system based on consultations with URTI diagnoses performed by individual provider. The diagnosis was coded using ICD-10 anatomical disease classification from acute rhinitis to laryngitis. All consultations generated via TPC system using a “careplan” module either by doctors or Medical Assistants were included in the study. They were also informed regarding the expected rate of antibiotic usage, at most of 10%, based on the prevalence of bacterial infection.6,7 Data were analysed using Microsoft Office Excel and VassarStats, an online statistical software.13
Results
Overall, there were 142,634 consultations recorded in 2010 and 143,351 in 2011. The number of consultations for URTI was 22,328 and 22,756 for 2010 and 2011, respectively; hence the incidence rate of URTI was 15.7% in 2010 and 15.9% in 2011. As shown in Table 1, children aged less than 12 years old contributed slightly more than a third of URTI visits with a slight male predominance.
Table 1. Characteristics of patients with URTI in 2010 and 2011.
| Category | 2010 (%) n=22328 | 2011 (%) n=22756 | P value | |
|---|---|---|---|---|
| Age group | <12 | 8347(37.4) | 8361(36.7) | 0.16 |
| (years) | ≥12 | 13981(62.6) | 14395(63.3) | |
| Gender | Female | 10911(48.9) | 11120(48.9) | 1.00 |
| Male | 11417(51.1) | 11636(51.1) | ||
| Ethnicity | Chinese | 1124(5.0) | 1202(5.3) | 0.01 |
| Indian | 510(2.3) | 425(1.9) | ||
| Malay | 19983(89.5) | 20415(89.7) | ||
| Others | 711(3.2) | 714(3.1) | ||
| Diagnosis | Acute nasopharyngitis | 4862(21.8) | 4409(19.3) | <0.001 |
| Acute pharyngitis/laryngitis | 320(1.4) | 1047(4.6) | ||
| Acute sinusitis | 71(0.3) | 72(0.3) | ||
| Acute tonsillitis | 1984(8.9) | 1696(7.5) | ||
| URTI (unclassified) | 15091(67.6) | 15565(68.3) |
Almost 90% of patients with URTI were Malays in congruence with the population distribution for the state. Majority of cases diagnosed as URTI were unclassified and the number of cases diagnosed with acute pharyngitis/ laryngitis increased markedly in 2011 as compared to 2010.
Table 2 shows that antibiotics were prescribed for 33.5% of patients with URTI in 2010, but this was reduced to 23.3% in 2011. The greatest reduction of antibiotic usage was noted in Simpang Empat HC from 1,318 to 561 prescriptions or from 36.8% to only 14.8% of antibiotic prescription rate.
Table 2. Frequency of URTI and antibiotic prescribing among clinics.
| Clinics | Total URTI | Prescribed antibiotic | Antibiotic prescription rate (%) | P value | |||
|---|---|---|---|---|---|---|---|
| 2010 | 2011 | 2010 | 2011 | 2010 | 2011 | ||
| Beseri HC | 6720 | 5882 | 2061 | 1419 | 30.7 | 24.1 | <0.001 |
| Kangar HC | 12031 | 13080 | 4091 | 3317 | 34.0 | 25.4 | <0.001 |
| Simpang Empat HC | 3577 | 3794 | 1318 | 561 | 36.8 | 14.8 | <0.001 |
| Total | 22328 | 22756 | 7470 | 5297 | 33.5 | 23.3 | <0.001 |
A total of 60 doctors and Medical Assistants had managed cases of URTI in these clinics in 2010 and 2011 but only 19 doctors and 13 Medical Assistants worked continuously for both years. Slightly more than 70% of cases were managed by Medical Assistants and they prescribed much less antibiotic than the doctors.
The figures 1 and 2 illustrate the individual profiling report of doctors and Medical Assistants who worked continuously in the two consecutive years of 2010 and 2011. There were wide variations of individual practice in using antibiotic for the treatment of URTI.
Before intervention, individual prescription rate among doctors varies from 16.2% to 88.9% and reduced from 4.8% to 50.5% after intervention. For Medical Assistants, the rates were 9.7% to 65.7% in 2010 and from 4.3% to 44.4% following intervention in 2011.
Generally, the majority (75%) of the providers showed a reduction in their antibiotic prescribing rates during the intervention year. Only 19% (6) showed an increase while 6% (2) showed no change. A bigger proportion of doctors (21%) showed no reduction as compared to the Medical Assistants at 15%.
Median (IQR) = 34.1 (27.3) in 2010; Median (IQR) = 24.5 (19.6) in 2011
Median (IQR = 26.5 (12.3) in 2010; Median (IQR) = 20.1 (17.3) in 2011
Table 3 showed that the commonest antibiotic prescribed for URTIs was erythromycin while the least prescribed (< 0.5%) was penicillin V.
Table 3. Type of antibiotics prescribed and in 2010 and 2011.
| Antibiotic | 2010 (%) n=7470 | 2011 (%) n=5297 |
|---|---|---|
| Macrolides - Erythromycin | 61.2 | 59.8 |
| Penicillins - Amoxicillin | 20.2 | 22.2 |
| - Ampicillin | 12.2 | 13.1 |
| - Ampicillinclavulanate | 1.8 | 1.3 |
| - Penicillin V | 0.4 | 0.0 |
| - Cloxacillin | 1.6 | 1.2 |
| Cephalosphorins | 1.5 | 1.2 |
| Tetracylines | 1.1 | 1.2 |
Discussion
The incidence of URTI in these public primary care clinics of approximately 16% was comparable with the recent study by Mimi O et al which cited 16.5% for public primary care clinics but much higher at 34.4% in private primary care clinics. 14 This reflects the quality of TPC data as regards the completeness of diagnoses and “careplan” generated for URTI consultations.
The antibiotic prescription rate for URTI of 33.5% for the 2010 baseline was also comparable to other studies at public primary care clinics in Malaysia, ranging from 26% to 45.5% but much higher among private practices at 46.7% to 75.9%, with a reducing trend over the years.3-5,15,16 Studies from developed countries showed a similar reducing trend, for example, ranging from 58.6% in 1997 to 36.6% in 2006 in the United Kingdom.17
Following the intervention in this study, the overall rate was reduced to 23.3%, with the biggest reduction at Simpang Empat HC at 14.8%. These reductions were partly influenced by higher than expected baseline rates of 10% and wider inter provider variation. The variation in antibiotic prescribing practice could not be attributed to the morbidity pattern alone, as this was similar for both years. However, the variability among those 19 doctors who worked during the 2 year study period successively was reduced with the median (IQR) of 34.1 (27.3) in 2010 to 24.5 (19.6) in 2011. The highest antibiotic prescription rate for URTI among doctors was 88.9% before the intervention but was 50.5% after the intervention. The same pattern was seen among the Medical Assistants but at a much lower rate. The dissimilarity in antibiotic prescribing practice between these two groups of providers could be explained by the Ministry of Health’s formulary restriction of antibiotics for Medical Assistant who would then refer cases that they deem requiring antibiotics to the doctors.
The commonest antibiotics prescribed for URTI was erythromycin, followed by amoxicillin and ampicillin. In the National Medical Care Statistics (NMCS) 2010, a study on morbidity and prescription pattern in the primary care setting, both public and private, the most prescribed antibiotics for URTI were amoxicillin, cephalexin and erythromycin at rates of 35.0%, 15.1% and 12.0% respectively.18
Clinical audits and practice profiling have become popular tools in the attempt to change physician behavior and to improve quality of care especially in United States, where the American Medical Association’s survey in the 1990s showed that more than half of US physician are subjected to either clinical or economic profiling.19 Profiling on the other hand may be perceived negatively by providers as an attempt to limit costs at the expense of infringement of their clinical freedom. Additionally, the choice of indicators in individual provider profiling should be based on those within the provider’s control, should be non-punitive and preferably directly monitored by the immediate supervisor. Indicators beyond the individual’s jurisdiction to intervene are more appropriate for clinic or higher level profiling.
This study has demonstrated the feasibility of generating the individual profiling report from data generated from TPC. Provider coding practices could be tracked and any fraud on data entry, such as providers avoiding making a diagnosis of URTI, could be easily identified, provided electronic prescribing was strictly enforced.
However as this is not a control study, there might be other confounding factors besides profiling which may contribute to the reduction of antibiotic usage. The intervention in this study was carried out for a relatively short period of time and it is envisaged that over a prolonged duration of intensive feedback through the individual provider profiling report, the antibiotic prescribing rate could be further reduced to reach target. Fast turnover of staffs may influence the results whereby only 32 out of 60 staffs were present for both two consecutive years. The providers’ response to the profiling report has also not been studied to gauge its acceptability. Lastly, the quality of TPC data were based on providers coding practices whereby recording acute illnesses were less accurate than chronic condition and this has been described in our previous report.20
Acknowledgements
The authors wish to thank the Director General of Health Malaysia for his permission to publish this paper. Special thanks to Prof Dr CL Teng, International Medical University, Malaysia for giving input on writing this manuscript and to all personnel involved in this project especially from the three TPC clinics in Perlis.
References
- 1.Wrigley T. Age- and sex-specific antibiotic prescribing patterns in general practice in England and Wales 1994–1998. Health Stat Q. 2002;14:14–20. [Google Scholar]
- 2.Cars O, Molstad S, Melander A. Variation in antibiotic use in the European Union. Lancet. 2001;357((9271)):1851–1853. doi: 10.1016/S0140-6736(00)04972-2. [DOI] [PubMed] [Google Scholar]
- 3.Teng CL, Leong KC, Aljunid SM, Cheah M. Antibiotic prescription in upper respiratory tract infections. Asia Pacific Family Medicine. 2004;3((1-2)):38–45. [Google Scholar]
- 4.Teng CL, Nurjahan MI, Hashim NA. et al. Upper respiratory tract infections: to what extent is the management evidence-based? Med J Malaysia. 2003;58:159–66. [PubMed] [Google Scholar]
- 5.Teng CL, Tong SF, Khoo EM, Lee V, Zailinawati AH, Mimi O, Chen WS, Nordin S. Antibiotics for URTI and UTI - prescribing in Malaysian primary care settings. Aust Fam Physician. 2011;40((5)):325–9. [PubMed] [Google Scholar]
- 6.Hong CY, Lin RT, Tan ES. et al. Acute respiratory symptoms in adults in general practice. Fam Pract. 2004;21:317–23. doi: 10.1093/fampra/cmh319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Foong HBB, Yassim M, Chia YC. et al. Streptococcal pharyngitis in a primary care clinic. Singapore Med J. 1992;33:597–9. [PubMed] [Google Scholar]
- 8.Arnold SR, Straus SE. Interventions to improve antibiotic prescribing practices in ambulatory care. Cochrane Database Syst Rev. 2005;4:CD003539 doi: 10.1002/14651858.CD003539.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Balas EA, Boren SA, Brown GD, Ewigman BG, Mitchell JA, Perkoff GT. Effect of physician profiling on utilization. Meta-analysis of randomized clinical trials. J Gen Intern Med. 1996;11((10)):584–90. doi: 10.1007/BF02599025. [DOI] [PubMed] [Google Scholar]
- 10.Jamtvedt G, Young JM, Kristoffersen DT, O’Brien MA, Oxman AD. Audit and feedback: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2006;2:CD000259 doi: 10.1002/14651858.CD000259.pub2. [DOI] [PubMed] [Google Scholar]
- 11.American Academy of Family Physicians. Physician Profiling, Guiding Principles. [Accessed November 26]. 2011. http://www.aafp.org/online/en/home/policy/policies/p/physicianprofiling.html . [Google Scholar]
- 12.Goldfield N, Gnani S, Majeed A. Primary care in the United States. Profiling performance in primary care in the United States BMJ. 2003;326((7392)):744–747. doi: 10.1136/bmj.326.7392.744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.VassarStats: Website for Statistical Computation. http://vassarstats.net/index.html . [Google Scholar]
- 14.Mimi O, Tong SF, Nordin S, Teng CL, Khoo EM, Abdul-Rahman A, Zailinawati AH, Lee VKM, Chen WS, Shihabudin WM, Noridah MS, Fauziah ZE. A Comparison of morbidity patterns in public and private primary care clinics in Malaysia. Malaysian Family Physician. 2011;6:19–25. [PMC free article] [PubMed] [Google Scholar]
- 15.Teng CL, Achike FI, Phua KL, Norhayati Y, Nurjahan MI, Nor AH, Koh CN. General and URTI-specific antibiotic prescription rates in a Malaysian primary care setting. Int J Antimicrob Agents. 2004;24((5)):496–501. doi: 10.1016/j.ijantimicag.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 16.Aljunid S. Paper presented in Annual Scientific Meeting, Academy of Medicine. Malaysia on 24th March: 1996. Management of upper respiratory tract infections by public and private sector doctors in a rural district of Malaysia. [Google Scholar]
- 17.Gulliford M, Latinovic R, Charlton J, Little P, van Staa T, Ashworth M. Selective decrease in consultations and antibiotic prescribing for acute respiratory tract infections in UK primary care up to 2006. J Public Health (Oxf) 2009;31((4)):512–20. doi: 10.1093/pubmed/fdp081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sivasampu S. Paper presented in Annual Scientific Meeting on Antimicrobial Resistance. Putrajaya, Malaysia: 2012. Antibiotic Utilisation Pattern in Primary Care, National Medical Care Survey (NMCS) 2010. [Google Scholar]
- 19.Emmons DW, Wozniak GD. Chicago, Ill: American Medical Association; 1994. Profiles and feedback: who measures physician performance? In: Gonzalez ML, ed. Socioeconomic Characteristics of Medical Practice, 1994. [Google Scholar]
- 20.Mohd Fozi K, Kamaliah MN, Safurah J. Morbidity Profiles at Three Primary Care Clinics in Perlis, Malaysia. Med J Malaysia. 2012;67((4)):363–368. [PubMed] [Google Scholar]


