Abstract
Human herpes virus 6 (HHV-6) infections are frequently detected in patients with immunosuppressed transplant; however, reactivation in an immunocompetent patient is rarely reported. The author reports the case of a 65-year-old woman presenting with status epilepticus with foci in the temporal and occipital lobe and MRI suggestive of encephalitis in the parietal, occipital and temporal regions. The cerebrospinal fluid (CSF) analysis showed normal cell counts, protein and glucose levels and hence viral aetiologies were considered. The patient's workup returned positive for HHV-6 in serum as well as CSF. The patient responded well to a 21-day course of antivirals with complete resolution of her symptoms. This case highlights the importance of considering HHV-6 encephalitis even among immunocompetent patients presenting with encephalitis and having signs of temporal lobe involvement.
Background
Human herpes virus 6 (HHV-6) is the sixth member of the herpes virus family to infect humans. A member of the Roseolovirus genus, HHV-6 is the causal agent of roseola infantum (also known as sixth disease), which is a childhood illness characterised by fever and rash. HHV-6 infection is frequently detected in patients with immunosuppressed transplant; however, reactivation in an immunocompetent patient is rarely reported.
Case presentation
The author reports of a 65-year-old woman, brought to the emergency centre (EC) by her family, with a 1-day history of confusion. The family mentioned that the patient had reported of a right temporal headache for the past day followed by an acute episode of confusion where she was disoriented in time and space. This was followed by left-sided weakness in the upper and lower extremities and some fasciculation, observed by the family, in the left upper extremity. This acute change in her baseline got the family worried and they brought the patient to the EC. The family denied any fever or chills in the patient and explained that this was the first episode of such symptoms in the patient.
The patient was relatively healthy with well-controlled hypertension on lisinopril and hydrochlorthiazide. The family denied any sick contact or any other known person with such presentation. They denied any recent travel, dietary change, insect or tick bites or any illicit drug use for the patient.
On presentation the patient was afebrile and haemodynamically stable. She was somnolent and was not able to follow commands, however, she opened her eyes to verbal stimuli. There were fine muscle twitchings observed in her left upper extremity. The remainder of her examination was benign.
Investigations
Initial laboratory investigation revealed normal complete blood count, liver function and renal function tests. Owing to concerns of a cerebrovascular event in the patient, she underwent a CT scan of the brain, which did not reveal any intracranial pathology. Further, there were concerns of complex partial seizures in the patient due to confusion and muscle twitching and jerking in her upper extremity. She underwent an EEG that revealed right hemisphere dysfunction, maximum in the posterior head region (occipital/temporal) with electrographic seizure.
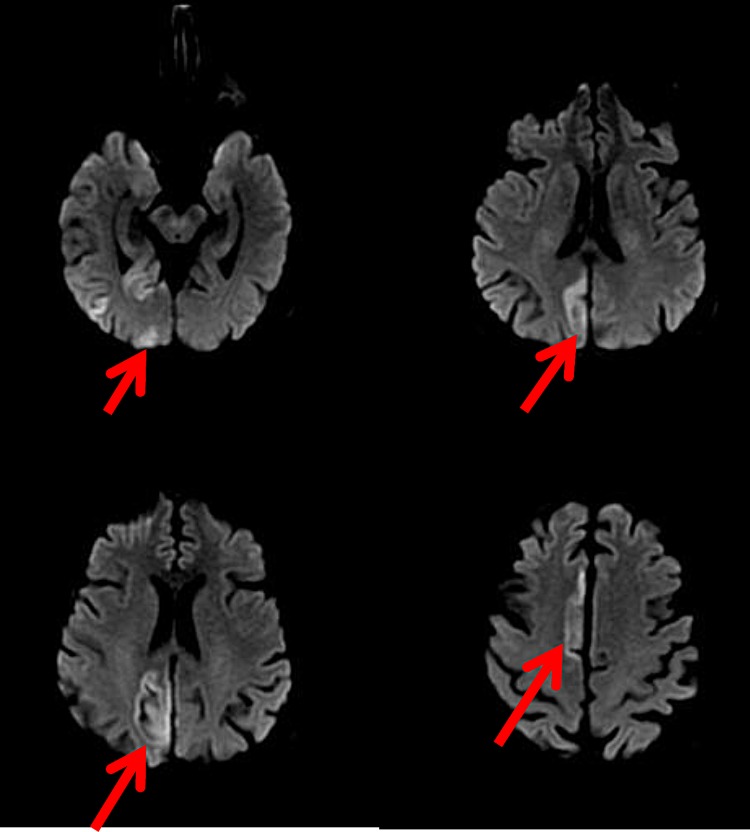
This was followed by an MRI of the brain with contrast, which showed multifocal areas of hyperintensities on the T2-weighted image, fluid-attenuated inversion recovery pulse image and diffusion-weighted imaging, primarily involving cortical grey matter of the right cingulate gyrus, right parietal, occipital and temporal regions (figures 1 and 2). The clinical and radiological picture was concerning for encephalitis and hence the patient underwent a lumbar puncture. The cerebrospinal fluid (CSF) fluid analysis showed normal cell counts, protein and glucose levels.
Figure 1.
MRI of the brain showing multifocal areas of T2 fluid-attenuated inversion recovery hyperintensities, primarily involving cortical grey matter of the right parietal, occipital and temporal regions.
Figure 2.
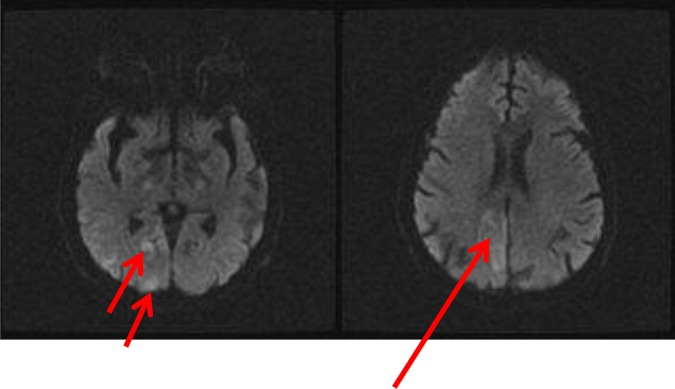
Hyperintensities on diffusion-weighted imaging seen in the cortical grey matter of the right parietal, occipital and temporal regions.
Differential diagnosis
The differentials at this time included an infectious versus a non-infectious cause for the patient's encephalitis. The Gram stain did not show any organisms and the aerobic, anaerobic, fungal and acid-fast bacilli cultures as well as CSF Venereal Disease Research Laboratory test were negative. Non-infectious causes such as paraneoplastic and N-methyl-d-aspartate receptor encephalitis were considered, however, the work up was negative. Viral aetiologies such as herpes simplex virus (HSV), cytomegalovirus (CMV), varicella zoster virus (VZV), HHV-6, Epstein-Barr virus and John Cunningham virus were considered.
Treatment
The patient was started on intravenous foscarnet after the CSF fluid analysis showed normal cell counts, protein and glucose levels and rapid quantitative real-time PCR for HSV were negative. Intravenous foscarnet was started instead of acyclovir to cover for viral aetiologies such as VZV, CMV and HHV-6, as acyclovir would not treat CMV and HHV-6. The patient continued to have seizures with multiple EEG recordings demonstrating right hemisphere dysfunction and electrographic seizures in the posterior head region for the first 48 h of admission. The patient was intubated and mechanically ventilated and required lorazepam, phenytoin, valproic acid and phenobarbital initially to stop the seizures and later required continuation of the anti-epileptics along with midazolam to prevent her from having seizures over the next 4 days in the intensive care unit.
Outcome and follow-up
The patient's viral workup came back positive for HHV-6 B DNA with 148 387 copies/mL in the serum and 16 189 copies/mL in the CSF. Foscarnet was changed to ganciclovir because of acute kidney injury on foscarnet, and the patient was treated for 21 days. Antiepileptic agents were tapered to valproic acid and phenytoin, and the patient was maintained and followed up on this regimen for the next year, during which period she was seizure free.
Discussion
HHV-6 reactivation is common in immunosuppressed patients and has been associated with cases of encephalitis in these patients. Status epilepticus associated with HHV-6 encephalitis has been previously reported in the first month after allogeneic stem cell transplantation.1 HHV-6 encephalitis in immunocompetent patients is rare, and has not been reported as presenting with status epilepticus. Among the previous studies evaluating the cause of encephalitis in immunocompetent patients, HHV-6 has been identified but the incidence of the same is low. In the two studies using CSF HHV-6 PCR for diagnosis, HHV-6 was positive in 4 out of the 1000 patients (California Encephalitis Project)2 and 9 of 138 patients presenting with signs of focal encephalitis.3
Previous case reports and series have commented that the majority of immunocompetent patients with HHV-6–induced encephalitis present with an altered level of consciousness associated with seizures and focal neurological signs. The majority of these patients have lesions detected on brain imaging.3–5 Classic neuroimaging findings reported in these patients include signal abnormalities in the medial temporal lobe involving the hippocampal formation and amygdala.6 HHV-6 encephalitis is known to manifest with symptoms of limbic encephalitis, with temporal lobe seizures and neuropsychiatric symptoms such as psychosis and behavioural disturbances and recognition of this neuroanatomic distribution aids in the diagnosis of HHV-6 encephalitis.7 Ganciclovir and foscarnet have been known to be effective against HHV-6 and previous case reports have demonstrated good clinical outcomes with both drugs. Foscarnet was used in our patient and later as the patient developed acute kidney injury in the hospital, foscarnet was switched to ganciclovir to complete a 21 day regimen.
This case highlights the importance of considering HHV-6 encephalitis even among immunocompetent patients presenting with encephalitis and having signs of temporal lobe involvement.
Learning points.
Human herpes virus 6 (HHV-6) reactivation is common in immunosuppressed patients and has been associated with cases of encephalitis.
HHV-6 encephalitis is known to manifest with symptoms of limbic encephalitis, with temporal lobe seizures and neuropsychiatric symptoms such as psychosis and behavioural disturbances.
Neuroimaging findings in HHV-6 encephalitis include signal abnormalities in the medial temporal lobe involving the hippocampus and amygdale.
Ganciclovir and foscarnet have been known to be effective against HHV-6.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Chordia P, Chandrasekar P. Status epilepticus due to severe HHV-6 encephalitis in an allogeneic stem cell transplant recipient. Mediterr J Hematol Infect Dis 2014;6:e2014008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Isaacson E, Glaser CA, Forghani B, et al. Evidence of human herpesvirus 6 in 4 immunocompetent patients with encephalitis. Clin Infect Dis 2005;40:890–3 [DOI] [PubMed] [Google Scholar]
- 3.McCullers JA, Lakeman FD, Whitley RJ. Human herpesvirus 6 is associated with focal encephalitis. Clin Infect Dis 1995;21:571–6 [DOI] [PubMed] [Google Scholar]
- 4.Patnaik M, Peter JB. Intrathecal synthesis of antibodies to human herpes virus 6 early antigen in patients with meningitis/encephalitis. Clin Infect Dis 1995;21:715–16 [DOI] [PubMed] [Google Scholar]
- 5.Birnbaum T, Padovan CS, Sporer B, et al. Severe meningoencephalitis caused by human herpesvirus 6 type B in an immunocompetent woman treated with ganciclovir. Clin Infect Dis 2005;40:887–9 [DOI] [PubMed] [Google Scholar]
- 6.Provenzale JM, vanLandingham KE, Lewis DV, et al. Extrahippocampal involvement in human herpesvirus 6 encephalitis depicted at MR imaging. Radiology 2008;249:955–63 [DOI] [PubMed] [Google Scholar]
- 7.De Simone M, Muccio CF, Megna AS, et al. Human herpes virus 6encephalitis in immunocompetent patient: an unusual neuroradiological presentation. Clin Neurol Neurosurg 2013;115:2219–22 [DOI] [PubMed] [Google Scholar]