Abstract
Serum creatinine is a widely used marker in the assessment of renal function. Elevated creatinine levels suggest kidney dysfunction, prompting the need for further investigation. This report describes a case in which the consumption of the bodybuilding supplement creatine ethyl ester resulted in raised serum creatinine in the absence of true underlying kidney pathology. The abnormalities reversed after discontinuation of the supplement. A case of pseudo renal failure was recognised and kidney function was concluded to be normal. This report aims to address the mechanisms by which the ingestion of creatine ethyl ester can mimic the blood results expected in advanced renal failure, and confronts the problems faced when relying on serum creatinine as a diagnostic tool.
Background
The use of muscle enhancing supplements continues to increase in popularity in the world of body building and fitness. In particular, nutritional supplementation with creatine is believed to provide a genuine ergogenic advantage. Research comparing muscle power and mass in those who used strength training alone with those who combined training with creatine supplementation has supported such claims.1
The concentration of serum creatinine is a widely utilised measure of renal function. As a waste product of skeletal muscle metabolism, it is excreted almost entirely via the kidneys. The serum creatinine concentration is therefore used to form an estimate of the rate of glomerular filtration (eGFR). If elevated, emphasis is placed on recognising and treating renal failure promptly.2 Increasing reliance on serum creatinine as a marker can overlook situations in which levels are influenced by factors independent of true changes in kidney function. A high muscle mass alone has been correlated with elevated serum creatinine.3 Black men of a muscular build have been noted to have a particularly high serum creatinine, assumed to be due to race-related differences in muscle mass.4 Serum creatinine can also double 2–4 h after the ingestion of protein in the form of cooked meat.5 Several drugs, such as cimetidine, trimethoprim, corticosteroids, pyrimethamine, phenacemide, salicylates and active vitamin D metabolites, can also increase plasma creatinine without influencing glomerular filtration, thought to be through inhibition of creatinine secretion by the proximal tubule.6
In addition, certain chemicals can cause analytic interference of creatinine measurements. Ketoacids (such as occurring in diabetic ketoacidosis) and 5-aminolevulinic acid (sometimes administered for photodynamic therapy) interfere with the alkaline picrate (Jaffé) assay of creatinine, giving falsely high readings and the incorrect impression of kidney dysfunction. The issue does not arise with enzymatic creatinine measurements. Our laboratory measures creatinine using the Jaffé method.
The commonly abused anabolic steroid, boldenone, can cause an elevation of plasma creatinine either by increasing muscle mass and hence endogenous creatinine production, and more acutely (without decreasing renal creatinine excretion) by an unspecified mechanism.7
Finally, the ingestion of the bodybuilding supplement creatine ethyl ester has been associated with elevated serum creatinine levels.8 Its creatinine metabolite has a very short half-life9 consistent with the rapid normalisation of serum creatinine in this case report after discontinuing the supplement.
All scenarios demonstrate circumstances in which serum creatinine can be benignly elevated in the absence of kidney pathology. This could lead to problems if the serum creatinine concentration is interpreted as an accurate measure of renal function. Each scenario could result in an unnecessary referral to a specialist clinic, creating the possibility for early misdiagnosis if such circumstances are not recognised.
This report describes a case in which the ingestion of the bodybuilding supplement creatine ethyl ester led to a substantial increase in serum creatinine. The patient was informed that he could be experiencing renal failure. A picture of ‘pseudo’ renal failure was acknowledged when creatinine levels normalised on discontinuation of the product. This case highlights the importance of striving for more accurate diagnoses in the light of ambiguous test results in order to minimise patient anxiety and reduce early misdiagnosis.
Case presentation
A 42-year-old Caucasian driving instructor attended his general practice clinic reporting a swollen left leg with an accompanying rash. These symptoms lasted for approximately 1 week and resolved spontaneously, but were followed by an episode of numbness in the right lower leg. He had never used anabolic steroids but consumed a high-protein diet (consisting of daily chicken and white fish), and took regular ‘muscle enhancing’ supplements including creatine ethyl ester, collagen and protein. He had been taking creatine ethyl ester for 4 months and used the supplement five times a week on training days. He took four tablets before and four tablets after training and each tablet contained 4 g of creatine ethyl ester. There was no history of ingestion of cimetidine, trimethoprim, corticosteroids, pyrimethamine, phenacemide, salicylates and active vitamin D metabolites, or and 5-aminolevulinic acid. The patient's medical history was otherwise unremarkable. He exercised regularly, mainly engaging in strength building activities, and occasionally took non-steroidal anti-inflammatories for muscle aches, but the use of non-steroidal anti-inflammatory drugs bore no temporal relationship to his presentation.
Investigations
Blood tests were arranged which revealed a serum creatinine of 198 µmol/L (normal range in men is 60–120 µmol/L) which corresponded to an estimated glomerular filtration rate (eGFR) of 33 mL/min. The blood test was repeated a week later and a serum creatinine level of 227 µmol/L was reported corresponding to an eGFR of 28 mL/min. Serum albumin level and blood count were normal, and there was no evidence of protein in the urine. Blood pressure was recorded to be 131/103 mm Hg.
Differential diagnosis
A middle-aged man presenting with an elevated serum creatinine corresponding to a low eGFR led to concerns of renal failure. The patient was referred to a specialist renal clinic for further assessment. He was advised to discontinue all bodybuilding supplements in the meantime which he was told could aggravate his potentially serious condition.
Outcome and follow-up
Two weeks later at the specialist appointment, physical examination revealed a very muscular appearance (weight 83 kg; height 1.79 m), consistent with his exercise orientated lifestyle. Blood pressure was recorded to be 127/78 mm Hg, heart and lung sounds were normal, examination of the abdomen was unremarkable and there was no visible skin rash. On testing, it became apparent that his creatinine levels had in fact returned to within normal range, at 104 µmol/L equating to an eGFR of 70 mL/min. A mildly elevated creatine kinase of 828 U/L was reported, again consistent with the patient's physique.
Three weeks later, he was reviewed again after remaining symptoms with discontinuing all bodybuilding supplements. Kidney function remained normal and home blood pressure readings were recorded at 125/60 mm Hg. It was concluded that the ingestion of creatine ethyl ester was responsible for the abnormalities in serum creatinine, and that the initial presentation of symptoms was unrelated and coincidental. The patient was advised that a bodybuilding supplement had caused a false reading in his kidney function test, falsely implying that he had acute kidney failure. Since there is no health evidence to support the use of these supplements, he was advised to discontinue them. The changes in the patient's serum creatinine from his first blood test at the GP to his third blood test in the renal clinic are demonstrated in figure 1.
Figure 1.
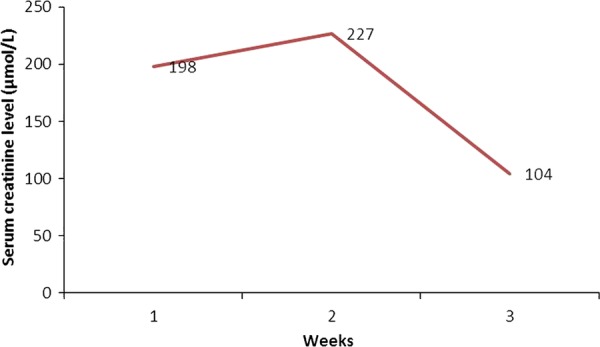
Graph demonstrating the change in serum creatinine over 4 weeks. A serum creatinine of 198 µmol/L corresponds to an estimated glomerular filtration rate (eGFR) of 33 mL/min, a serum creatinine of 227 µmol/L corresponds to an eGFR of 28 mL/min and a serum creatinine of 104 µmol/L corresponds to an eGFR of 70 mL/min. Note that patient stopped taking bodybuilding supplements at approximately 2 weeks, resulting in the decrease in serum creatinine, and the subsequent increase in eGFR.
Discussion
In the case described, the ingestion of the body building supplement creatine ethyl ester caused serum creatinine concentration to markedly increase. These blood results were initially misconstrued as renal failure due to the correspondingly low eGFR. After discontinuation of the supplements, the serum creatinine concentration returned to within normal range and renal function was concluded to be normal. Despite the relieving outcome, the patient was subjected to anxiety and distress in light of the initial misdiagnosis. Creatine is a widely available product, with existing evidence supporting the fact that it potentiates muscle power and strength.1 It is legal, considered to be safe, and is not classified as a pharmaceutical agent.5 As an under recognised issue, the link between the consumption of such products and the blood results obtained could be easily overlooked during consultation. Fortunately, this initial misdiagnosis was rectified after acknowledging the reversal of results at the specialist renal review.
Velema and Ronde8 describe a similar case in which creatine ethyl ester was responsible for elevated serum creatinine in the absence of kidney pathology. Willis et al5 highlight a series of cases in which creatine supplementation was mistaken for kidney disease in patients who were HIV positive. It was suspected that the patients were experiencing kidney insufficiency secondary to their condition or as a result of their antiretroviral therapy. It was eventually recognised that creatine supplements were responsible, as their creatinine levels fell back to within normal range at times when the supplements were not used due to periods of illness. At these times the patients abstained from using creatine as they were not able to attend the gym. These documented cases highlight the importance of this as an issue. The likelihood of misdiagnosis can be minimised if all variables are taken into account and more reliable means of testing are utilised before jumping to conclusions that could cause unwarranted patient anxiety.
The National Institute for Health and Care Excellence (NICE) guidelines state that when a request for serum creatinine is made, clinical laboratories should make a corresponding estimate of the glomerular filtration rate. This serves to provide insight into how well the kidneys are functioning. The guidelines also state that in cases where there are extremes of muscle mass, for example in bodybuilders, the eGFR should be interpreted with caution due to the fact that increased muscle mass can lead to an underestimation of the GFR.10 It is therefore important for all clinicians to be aware of possible scenarios in which creatinine may be raised due to changes independent of true renal function. Although further investigation of a substantially raised serum creatinine is paramount, other explanations should be contemplated and discussed with the patient.
Creatinine is a chemical waste product formed by skeletal muscles in the process of creatine phosphate metabolism. It is produced at a fairly stable rate and it is almost entirely eliminated via renal excretion without being reabsorbed. The plasma creatinine concentration is equal to its rate of production divided by its rate of excretion, and on this basis it is used as a well-recognised marker of renal function.11 Clinicians can often assume by default that an elevated serum creatinine indicates that the kidneys are not clearing creatinine effectively. It is rarely considered that the body may in fact be producing creatinine in excess, which is demonstrated in the case discussed.
Creatine is a nitrogenous acid which is synthesised in the liver and to a lesser extent in the kidneys and the pancreas. It is made up of three amino acids, namely glycine, arginine and methionine.5 We also obtain creatine via our diets, particularly through protein rich foods such as red meat and fish. It is stored in skeletal muscle in the form of creatine phosphate where it serves to restore ATP from ADP after muscle contraction. It is then converted to creatinine by non-enzymatic dehydration.5 The reaction between creatine, creatine phosphate and creatinine is demonstrated in figure 2. Normal intake of creatine is approximately 1 g/day but can reach 25–30 g when consuming a protein rich diet combined with additional supplementation.5 It is believed that creatine supplementation can potentiate the ability of skeletal muscles to resynthesise ATP from ADP. As a result, recovery times shorten and muscle contractility is improved, allowing for longer and more intense training. This forms the principles behind the claimed ergogenic advantages of creatine use.
Figure 2.
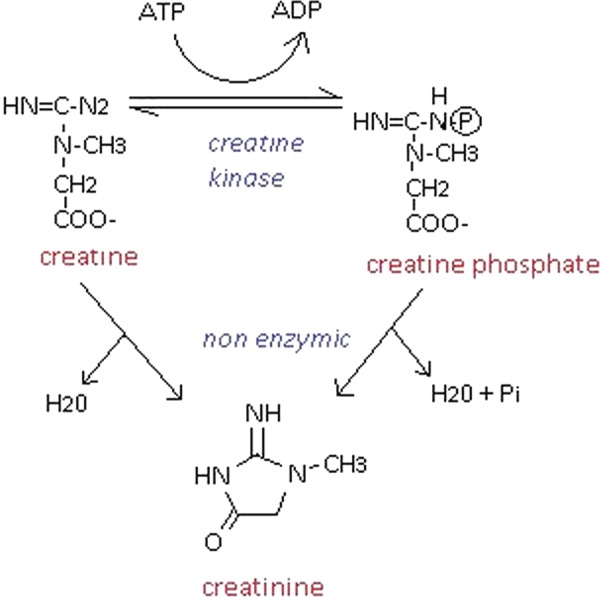
The reversible conversion of creatine to creatine phosphate by binding inorganic phosphate via the catalyst, creatine kinase. The reverse reaction produces ATP from ADP and the waste product, creatinine, which is excreted in urine.
Creatine supplements are available to be purchased in two forms: creatine monohydrate and creatine ethyl ester. Claims have suggested that creatine ethyl ester has a better solubility in lipids and therefore higher rates of absorption than creatine monohydrate.12 However, it has been found that under normal physiological conditions, creatine ethyl ester is very unstable and is largely converted into creatinine in the gastrointestinal tract, where it is also absorbed. Spillane et al13 demonstrate this in an experiment in which serum creatine and creatinine measurements were taken from healthy volunteers who either consumed creatine ethyl ester, creatine monohydrate or a placebo. It was found that serum creatinine levels approximately tripled after the ingestion of creatine ethyl ester, while serum creatine only marginally increased. The ingestion of creatine monohydrate caused serum creatine to increase significantly and only caused a marginal increase in serum creatinine. These findings suggest that it is highly likely that creatine ethyl ester supplementation provides little to no ergogenic advantage, by serving to only increase levels of the waste product, creatinine, which is then excreted via the kidneys. This explains how the consumption of creatinine ethyl ester can cause substantially elevated serum creatinine in the absence of true renal pathology. Creatinine has a half-life of 3.85 h, so you would expect it to decay to ¼ of its value within approximately 8 h of the consumption of creatine ethyl ester.14 This fully explains how serum creatinine had fallen to an acceptable value 2 weeks after discontinuing the supplements, yet it is also easy to imagine how these levels could build up over time through continued use.
It is important to remember that high muscle mass alone independently correlates with high levels of serum creatinine. This is due to increased supply and turnover of creatine phosphate. It is clear that this factor was not solely responsible for the initially raised serum creatinine, due to the reversal of the results on cessation of creatine ethyl ester supplementation.
Finally, it is also necessary to rule out the possibility that the findings in this case were actually caused by a reversible form of interstitial nephritis. Although temporary, this form of renal insufficiency would be of greater concern and has been associated with the ingestion of creatine. Koshy and Griswold15 report a case in which creatine use resulted in an allergic reaction in the form of interstitial nephritis. In the case described in this report, there was no eosinophilia, dipstick of urine was unremarkable and the abnormalities were quickly reversible, making this presentation unlikely to be due to a case of true allergic interstitial nephritis.
Learning points.
Ingestion of creatine ethyl ester can result in misleadingly raised serum creatinine. In general practice, increased awareness of the potential effects of bodybuilding supplements on apparent kidney function would be beneficial.
Elevated serum creatinine does not always indicate renal failure, and a normal serum creatinine level does not necessarily rule it out. Calculating the glomerular filtration rate solely from the serum creatinine concentration should be avoided, as this theoretical calculation can be influenced and deranged via a number of factors.
When in doubt, there are further measures that could be implemented to assess whether a high serum creatinine is due to reduced renal clearance. The creatinine clearance test could be used to compare the level of creatinine in the blood with the level of creatinine in the urine over 24 h. Isoptopic glomerular filtration rate (GFR) testing could also be performed. Alternatively, measuring cystatin C (a non-glycosylated 13 kDa protein) could be used to improve estimates of GFR as this measurement is thought to be less influenced by muscle mass or diet.16
The points made in this case can be extrapolated to other diagnostic scenarios. When considering ambiguous test results, if all relevant information is obtained and shared with the patient, it becomes possible to reduce unwarranted anxiety if an alternate explanation becomes plausible.
Footnotes
Contributors: DN gathered the data for the case as he was the renal specialist that the patient was referred to LW and DN constructed the design of the actual report and discussed how to interpret the issues and results addressed in the case. LW drafted the article, and DN revised the article and helped make necessary adjustments. All authors have read and approved the final version.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Bemben M, Lamont H. Creatine supplementation and exercise performance: recent findings. Sports Med 2005;35:107–25 [DOI] [PubMed] [Google Scholar]
- 2.Perrone RD, Madias NE, Levey AS. Serum creatinine as an index of renal function: new insights into old concepts. Clin Chem 1992;38:1933–53 [PubMed] [Google Scholar]
- 3.Baxmann AC, Ahmed MS, Heilberg IP. Influence of muscle mass and physical activity on serum and urinary creatinine and serum cystatin C. Clin J Am Soc Nephrol 2008;3:348–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hsu J, Johansen KL, Hsu CY, et al. Higher serum creatinine concentrations in black patients with chronic kidney disease: beyond nutritional status and body composition. Clin J Am Soc Nephrol 2008;3:992–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Willis J, Jones R, Nwokolo N, et al. Protein and creatine supplements and misdiagnosis of kidney disease. BMJ 2010;340:b5027. [DOI] [PubMed] [Google Scholar]
- 6.Andreev E, Koopman M, Arisz L. A rise in plasma creatinine that is not a sign of renal failure: which drugs can be responsible? J Intern Med 1999;246: 247–52 [DOI] [PubMed] [Google Scholar]
- 7.Winnett G, Cranfield L, Almond M. Apparent renal disease due to elevated creatinine levels associated with the use of boldenone. Nephrol Dial Transplant 2011;26:744–7 [DOI] [PubMed] [Google Scholar]
- 8.Velema MS, Ronde W. Elevated plasma creatinine due to creatine ethyl ester use. Neth J Med 2011;69:79–81 [PubMed] [Google Scholar]
- 9.Katseres NS, Reading DW, Shayya L, et al. Non-enzymatic hydrolysis of creatine ethyl ester. Biochem Biophys Res Commun 2009;386:363–7 [DOI] [PubMed] [Google Scholar]
- 10.Chronic kidney disease: early identification and management of chronic kidney disease in adults in primary and secondary care. Cg73. National Institute for Health and Care Excellence, 2008
- 11.Wyss M, Kaddurah DR. Creatine and creatinine metabolism. Physiol Rev 2000;80:1107–213 [DOI] [PubMed] [Google Scholar]
- 12.Jager R, Purpura M, Shao A, et al. Analysis of the efficacy, safety, and regulatory status of novel forms of creatine. Amino Acids 2011;40:1369–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spillane M, Schoch R, Cookel M, et al. The effects of creatine ethyl ester supplementation combined with heavy resistance training on body composition, muscle performance, and serum and muscle creatine levels. J Int Soc Sports Nutr 2009;6:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chiou WL, Hsu FH. Pharmacokinetics of creatinine in man and its implications in the monitoring of renal function and in dosage regimen modifications in patients with renal insufficiency. J Clin Pharmacol 1975;15:427–34 [DOI] [PubMed] [Google Scholar]
- 15.Koshy KM, Griswold E. Interstitial nephritis in a patient taking creatine. N Engl J Med 1999;340:814–15 [DOI] [PubMed] [Google Scholar]
- 16.Stevens LA, Coresh J, Schmid CH, et al. Estimating GFR using serum cystatin C alone and in combination with serum creatinine: a pooled analysis of 3,418 individuals with CKD. Am J Kidney Dis 2008;5:395–406 [DOI] [PMC free article] [PubMed] [Google Scholar]


