Abstract
Background:
Paracetamol; a cyclooxygenase inhibitor; acts through the central nervous system as well as serotoninergic system as a nonopioid analgesic. A prospective, double-blinded, and randomized-controlled study was carried out to compare the efficacy of preoperative 1g intravenous (iv) paracetamol with placebo in providing postoperative analgesia in head-neck cancer surgery.
Materials and Methods:
From 2008 February to 2009 December, 80 patients for palliative head-neck cancer surgery were randomly divided into (F) and (P) Group receiving ivplacebo and iv paracetamol, respectively, 5 min before induction. Everybody received fentanyl before induction and IM diclofenac for pain relief at8 hourly for 24 h after surgery. Visual analogue scale (VAS) and amount of fentanyl were measured for postoperative pain assessment (24 h).
Results and Statistical analysis:
The mean VAS score in 1st, 2nd postoperative hour, and fentanyl requirement was less and the need for rescue analgesic was delayed in ivparacetamol group which were all statistically significant. Paracetamol group had a shorter surgical intensive care unit (SICU) and hospital stay which was also statistically significant.
Conclusion:
The study demonstrates the effectiveness of ivparacetamol as preemptive analgesic in the postoperative pain control after head-neck cancer surgery and earlier discharge from hospital.
Keywords: Intravenous paracetamol, postoperative analgesia, surgical intensive care unit
INTRODUCTION
Effective pain control in the postoperative period is essential for optimal recovery. Adequate postsurgical pain control increases patient satisfaction, improves sleep, results in a more rapid recovery and shorter hospital stay, and lowers the risks of postoperative complications, such as the development of a deep vein thrombosis (DVT) and pulmonary complications.[1,2] There are many different drugs that can be used to treat postoperative pain; each with its own risk and adverse effects. Throughout the decades, modalities to facilitate analgesia have been implemented with a variety of results. One of the most common ways of providing analgesia is with the use of opioids. Recently, it has been reported that the use of opioids has decreased in the postoperative setting due to unwanted side effects (e.g., respiratory depression, sedation, nausea and vomiting, and slowed gastrointestinal functioning) leading to longer postoperative stays and delayed recovery.[3,4] The use of nonopioid analgesics as adjuncts to opioids or as stand-alone agents in providing analgesia isbecoming feasible options, as more drugs with less adverse effects are being developed. Intravenous (iv) acetaminophen can be integrated into a multimodal approach to optimize pain management effectively. In November 2010, the FDA approved the use of IV acetaminophen for the management of mild to moderate pain, the management of moderate to severe pain with adjunctive opioid analgesics, and the reduction of fever.
Paracetamol (acetaminophen; N-acetyl-p-aminophenol) is an acetanilide derivative, safe, well tolerated drug with proven efficacy as analgesic. Its clinical effects arise most likely from central action and ivadministration provides rapid and predictable therapeutic plasma concentration. Ready to use paracetamol infusion has been available in India since the past few years.
Different types of pain control measures have been tried for a long time.[5,6] Valuable analgesic properties of opioids[7] like fentanyl[8] in the treatment of acute, intense postoperative pain are well-recognized. It has been found that routine treatment of opioids at the beginning of operation conferred significantly better pain control than opioids given at the end of surgery.[9] However, to reduce the opioid-related side effects and hasten recovery in head-neck cancer surgery drugs such as nonsteroidal anti-inflammatory drugs (NSAIDs), paracetamol, cyclooxygenase (COX)-2 inhibitors, local anesthetics, steroids, and so on are often used for their opioid-sparing action.[10,11]
The aim of this randomized study was to compare the analgesic efficacy of ivfentanyl alone versus ivfentanyl plus paracetamol for postoperative pain relief after head-neck cancer surgery as well as its impact on duration of hospital stay, if any.
MATERIALS AND METHODS
After takingethical committee approval, written and informed consent was obtained from all patients. Patients aged 30-70 years and American Society of Anesthesiologists (ASA) physical statuses I, II, or III scheduled for head-neck cancer surgery, were included in the study. Exclusion criteria included patient refusal, known allergy or hypersensitivity or contraindication to opioids or paracetamol, impaired liver function (transaminases > twice upper limit), renal dysfunction (creatinine >2.0 mg/dL), cardiopulmonary abnormality, alcoholism, uncontrolled chronic diseases, known or suspected history of alcohol, or drug abuse. Patients who were pregnant or breast-feeding mothers were excluded. Patients were also excluded if they had received NSAIDs within 8 h, any analgesic drug within 12 h, or corticosteroids within 7 days before administration of study medication. The patients were asked about history of drug allergy, previous operations, or prolonged drug treatment. General examination, systemic examinations, and assessment of the airway were done. Preoperative fasting of minimum 6 h was ensured before operation in all day care cases. Patients received oral premedication, 10 mg diazepam on the night before surgery and tablet ranitidine 150 mg in the previous night and on the morning of operation with sips of water.
The patients were randomly divided into two groups with 40 patients in each group. In the operating room, all standard monitoring techniques were used and crystalloid infusion was started. Patients in the fentanyl group (Group F) received 100 mLof normal saline and those in the fentanyl plus paracetamol group (Group P) received 100 mL of paracetamoliv 5 min before induction. All drugs were available in the hospital pharmacy. They were administered to the patients by qualified resident doctors who were not involved in the study. After preoxygenation for 5 min with 100% oxygen and premedication with glycopyrrolate (0.01 mg/kg) anesthesia was induced in both the group with iv etomidate (2 mg/kg), fentanyl (2 µg/kg), and vecuronium (0.1 mg/kg).
Anesthesia was maintained by 1%-2% isoflurane in nitrous oxide and oxygen (ratio 2:1). The lungs were mechanically ventilated and EtCO2 (End tidal CO2) was maintained between 35 and 40 mm Hg. Fentanyl was repeated in the dose of 1 µg/kg intraoperatively if both hazards ratio and NIBP (Non invasive blood pressure) increased >20% from baseline despite maintaining adequate depth of anesthesia.
After extubation, all patients were transferred to surgical intensive care unit (SICU). Postoperative pain was assessed using a visual analog scale (VAS; 0 = “no pain” and 10 = “worst pain imaginable”). Postoperative analgesia was provided routinely to all patients by intramuscular diclofenac at 8 h interval and ivfentanyl 1 µg/kg was administered as rescue analgesic when the VAS score exceeded 3.
Sedation was determined according to a sedation score ranging from 0 to 2 (0 = alert, 1 = drowsy but arousable to voice, and 2 = very drowsy, but arousable to shaking). The VAS scores and sedation scores were assessed at 1, 2, 4, 6, 8, 12, and 24 h after surgery. Total and incremental fentanyl consumption at these times for both the groups was also recorded. If nausea and/or vomiting occurred, the same was noted and 4 mg of ondansetron was given intravenously. The number of patients receiving antiemetics and their total dosages were noted. Patients were observed for the occurrence of any adverse effects during the first 24 h. After 24 h, patients were assessed for: (a) ability to mobilize and dress, (b) need for any analgesic, and (c) surgical complication, if any. When the patient scored yes on the former and no on the two latter questions, they were assessed ready for discharge from SICU. All measurements were recorded by the resident who was blinded to the study drugs.
A sample size of 35 patients by group was calculated to detect a significant difference of 20% or more in opioid consumption with a power of 80% and a significance level of 5%. Data were reported as mean ± standard deviation. Statistical assessment included analysis of variance (ANOVA) and student's t-test for continuous data and VAS pain data. Fisher's exact t-test and Chi-square test wereused to analyze nominal data; P < 0.05 was considered to be significant.
RESULTS
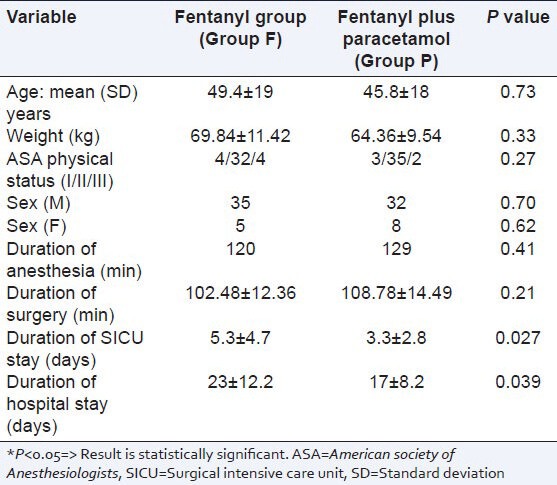
Both groups were similar in regard to age, weight, sex, ASA physical status, duration of anesthesia and surgery, and the duration of SICU as well as hospital stay [Table 1].
Table 1.
Patient data and characteristics (mean±SD)
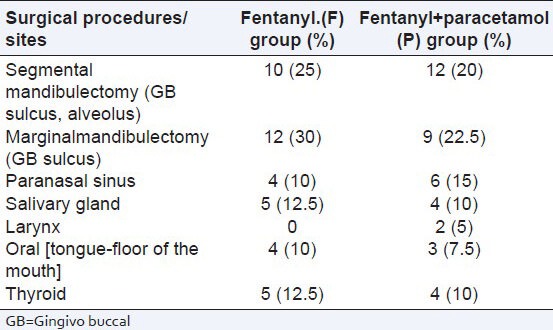
Nature and site of head-neck surgeries among two groups are quite comparable [Table 2].
Table 2.
Palliative surgeries for head-neck cancer for randomized patient groups
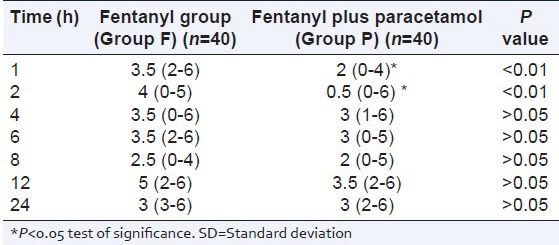
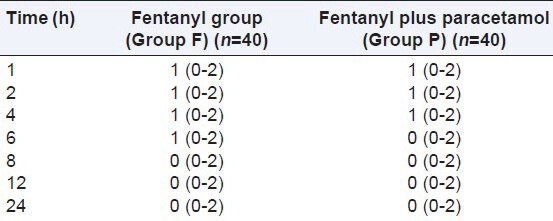
None of the patients in either group required fentanyl intraoperatively [Table 3]. The mean VAS pain score over the 24-h period was similar in both the groups [Table 3]; however, the mean VAS score at 1 and 2 h after surgery was lower in the Group P {2 (0-4) vs. 3.5 (2-6)}; {0.5 (0-6) vs. 4 (0-5)} respectively [Table 4].
Table 3.
Postoperative pain relief and side effects
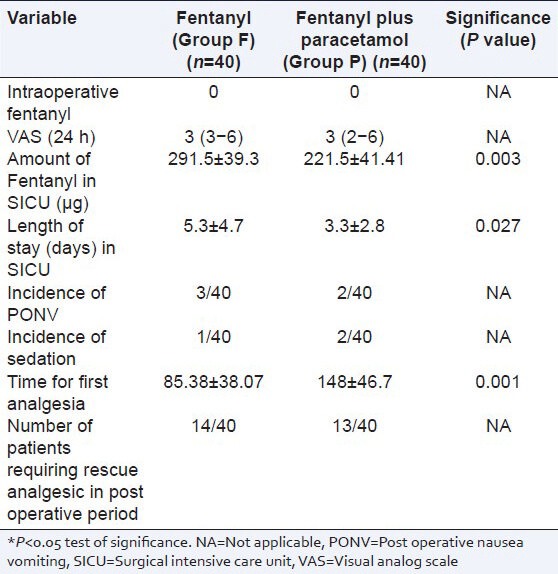
Table 4.
Pain scores (mean±SD)
The total use of fentanyl as rescue analgesic in SICU was significantly higher in Group F over Group P (291.5 ± 39.3 vs. 221.5 ± 41.41) µg, respectively [Table 3] and the time for the first dose of rescue analgesic in the SICU was significantly lower in Group F over Group P (85.38 ± 38.07 vs. 148 ± 46.7) min, respectively [Table 3]. However, the number of patients requiring rescue analgesic was similar in both the groups [Table 3].
There was significant difference in the length of stay in SICU as well as in hospital. Group P was discharged earlier from SICU (3.3 ± 2.8 vs. 5.3 ± 4.7) days and from hospital (17 ± 8.2 vs. 23 ± 12.2) days, respectively [Table 3]. Incidence of PONV (post operative nausea vomiting) and sedation were similar among the two groups [Tables 3 and 5]. Sedation scores and nausea are similar among the groups. No other postoperative complications were reported from any of the groups.
Table 5.
Sedation scores
DISCUSSION
Inadequate pain management in the perioperative period specifically in cancer patients leads to both short- and long-termconsequences. Among these complications, basal atelectasis, pneumonia,[1,2] DVT, pulmonary embolism, psychological trauma which even may lead to posttraumatic stress disorder. With the help of excellent pain management protocol the anxiety, morbidity, cost, and length of hospital stay in the postoperative period can be decreased. Besides showing individual variation in intensity and duration, the pain is often unpredictable. It may remain severe throughout the first postoperative week in 18% of the patients.[12]
The complex nature of pain after head-neck cancer surgery suggests that effective analgesic treatment should be multimodal.[13,14]
In one study,[15] some authors observed a 9-year trend of opioid prescribing for cancer pain during the last 3 months of life. But long before that a persistent effort was there to avoid opioid and to administer NSAIDs for control of cancer pain.[16,17] Another study[18] showed that acetaminophen improved pain and well-being without major side effects in patients with cancer and persistent pain despite a strong opioid regimen. Efficacy and safety of single and repeated administration of 1 giv acetaminophen injection (paracetamol) for pain management after major orthopedic surgery was established by a repeated-dose, randomized, double-blind, placebo-controlled, three-parallel group study.[19]
In another study by Hein et al.,[20] of 60 patients undergoing a minor gynecological surgery, 8 mg of oral lornoxicam was given to one group and 1000 mg of oral paracetamol was given to another group 60 min before induction. It was observed that VAS pain scores at postoperative 30 and 60 min were similar in both the groups; however, the VAS score was higher in the control group (did not receive medicines).
In our study, we used ivparacetamol 1 g as preemptive analgesic and assessed its effects on intraoperative analgesic requirement, postoperative analgesic effectiveness, postoperative fentanyl consumption, frequency of side-effects, and duration of hospital stay.
The demographic profile between two groups which was statistically insignificant (P > 0.05) of our patients was quite similar with other research investigations and provided us the uniform platform to evenly compare the results obtained. A study conducted by Cakan et al.,[21] for evaluation of analgesic efficacy and opioid-sparing effect of ivparacetamol in a total of 40 patients undergoing lumbar laminectomy and discectomyyielded similar results. The mean duration of anaesthesia and surgery were almost comparable in both the groups with no significant statistical difference [Table 1].
From Table 2, it is quite evident that types of surgical procedures were almost similar in both the groups and has no statistical significance.
Our study showed that ivparacetamol when used as preemptive analgesic just before induction as part of multimodal analgesic regime has significant opioid sparing effect in perioperative period. This is consistent with the findings in various studies where opioid-sparing effects of NSAIDs, COX-2 inhibitors, and paracetamol have been found to be in the range of 20-30%.[22,23]
There are evidences from other surgical procedures to support clinically relevant analgesic effect of paracetamol with additives like opioids.[24] It has been reported[25] that the combinations of paracetamol and pregabalin, or paracetamol, pregabalin and dexamethasone did not reduce morphine consumption and pain score compared with paracetamol alone for patients undergoing abdominal hysterectomy.
As per European Society for Medical Oncology (ESMO) clinical practice guideline[26] paracetamol and/or a NSAID are effective for treating mild pain, again paracetamol and/or NSAID are effective for treating all intensities of pain, at least in the short term and unless contraindicated. Our study results are consistent with their findings in this regard. They[26] also stated that opioid is the first choice for moderate to severe pain. Here, we had also used iv fentanyl for postoperative rescue analgesia.
In our study, no differences were observed between the two groups in the adequacy of analgesia as assessed by VAS scores [Table 4, Figure 1]. However, the median pain scores were significantly lower in the paracetamol group (Group P) at two intervals particularly in immediate postoperative period and the time for first analgesic requirement was significantly lower in the fentanyl alone group (Group F). This may be because of the initial loading dose of paracetamol providing a higher plasma concentration. Piguet et al’.[27] had demonstrated the close correlation between plasma concentration and analgesic effect of paracetamol with ivdoses of up to 2 g in healthy volunteers. Juhl et al.,[28] had demonstrated that the extent and duration of pain relief following third molar surgery significantly improved after 2 g over 1 g of initial ivdose of paracetamol. Our results are consistent with these results.
Figure 1.
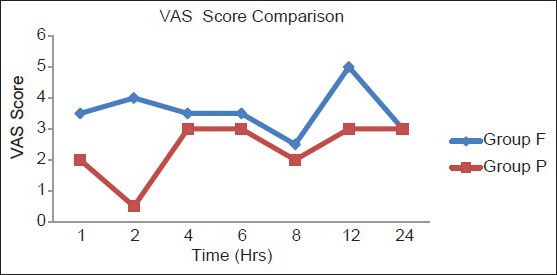
Comparison of visual analog scale score among Groups P and F
Our study did not find any reduction in the opioid related side-effects (PONV, sedation, etc.) in the paracetamol group (Group P) as might be expected because of the decrease in total fentanyl dose. This may be because of the lesser number of subjects in our study. Larger studies with adequate power to detect opioid-related side-effects would be able to demonstrate the reduction of dose- dependent side-effects of fentanyl, such as sedation, respiratory depression, urinary retention, or nausea. Our study demonstrated the additive effect of combining ivparacetamol with fentanyl on postoperative analgesia resulting in decreased opioid need and in slightly improved or similar pain relief. The different sites of action of these drugs in the nervous system may be the cause of better pain relief. Whereas the effect of paracetamol is due to the inhibition of prostaglandins and activation of descending serotonergic inhibitory pathways,[29,30] the analgesic effect of fentanyl is due to its agonist action in the opioid receptors of the central nervous system. The complimentary analgesic actions of.the two drugs make them an important component of multimodal pain therapy.
In 2009, a study[31] concluded that preemptively administered iv paracetamol 1 g in patients undergoing a total.abdominal.hysterectomy ensures an effective analgesia during.the postoperative period and thereby shortens the length of hospital stay. Our study also has a significant impact on SICU stay and hospital discharge program. Patients pretreated with ivparacetamol had less SICU stay and were discharged earlier from hospital.
However, our study had a few limitations. PCA pump was not used in the postoperative period. Both of these could have improved the results of our study but owing to technical reasons and limited availability it was not possible.
CONCLUSION
It can be concluded that iv paracetamol is an excellent preemptive analgesic which reduces postoperative pain, opioid consumption, and hastens discharge from hospital in palliative head-neck cancer surgery.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Lawrence VA, Hilsenbeck SG, Mulrow CD, Dhanda R, Sapp J, Page CP, et al. Incidence and hospital stay for cardiac and pulmonary complications after abdominal surgery. J Gen Intern Med. 1995;10:671–8. doi: 10.1007/BF02602761. [DOI] [PubMed] [Google Scholar]
- 2.Smetana GW. Postoperative pulmonary complications: An update on risk assessment and reduction. Cleve Clin J Med. 2009;76(Suppl 4):S60–5. doi: 10.3949/ccjm.76.s4.10. [DOI] [PubMed] [Google Scholar]
- 3.Troidl H, Spangenberger W, Langen R, al-Jaziri A, Eypasch E, Neugebauer E, et al. Laparoscopic cholecystectomy: Technical performance, safety and patient's benefit. Endoscopy. 1992;24:252–61. doi: 10.1055/s-2007-1010477. [DOI] [PubMed] [Google Scholar]
- 4.Joshi GP, Ogunnaike BO. Consequences of inadequate postoperative pain relief and chronic persistent postoperative pain. Anesthesiol Clin North America. 2005;23:21–36. doi: 10.1016/j.atc.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 5.Lao L, Bergman S, Hamilton GR, Langenberg P, Berman B. Evaluation of acupuncture for pain control after oral surgery: A placebo-controlled trial. Arch Otolaryngol Head Neck Surg. 1999;125:567–72. doi: 10.1001/archotol.125.5.567. [DOI] [PubMed] [Google Scholar]
- 6.Gil Z, Smith DB, Marouani N, Khafif A, Fliss DM. Treatment of pain after head and neck surgeries: Control of acute pain after head and neck oncological surgeries. Otolaryngol Head Neck Surg. 2006;135:182–8. doi: 10.1016/j.otohns.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Oifa S, Sydoruk T, White I, Ekstein MP, Marouani N, Chazan S, et al. Effects of intravenous patient-controlled analgesia with buprenorphine and morphine alone and in combination during the first 12 postoperative hours: A randomized, double-blind, four-arm trial in adults undergoing abdominal surgery. Clin Ther. 2009;31:527–41. doi: 10.1016/j.clinthera.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 8.Practice guidelines for acute pain management in the perioperative setting: An updated report the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology. 2004;100:1573–81. doi: 10.1097/00000542-200406000-00033. [DOI] [PubMed] [Google Scholar]
- 9.Lane GE, Lathrop JC, Boysen DA, Lane RC. Effect of intramuscular intraoperative pain medication on narcotic usage after laparoscopic cholecystectomy. Am Surg. 1996;62:907–10. [PubMed] [Google Scholar]
- 10.McNicol E, Strassels S, Goudas L, Lau J, Carr D. Nonsteroidal anti-inflammatory drugs, alone or combined with opioids, for cancer pain: A systematic review. J Clin Oncol. 2004;22:1975–92. doi: 10.1200/JCO.2004.10.524. [DOI] [PubMed] [Google Scholar]
- 11.Marret E, Kurdi O, Zufferey P, Bonnet F. Effects of nonsteroidal anti-inflammatory drugs on patient-controlled analgesia side-effects: Meta-analysis of randomized controlled trials. Anesthesiology. 2005;102:1249–60. doi: 10.1097/00000542-200506000-00027. [DOI] [PubMed] [Google Scholar]
- 12.Bost P, Commun F, Albuisson E, Guichard C, Mom T, Eschalier A, et al. Postoperative pain assessment in head and neck cancer surgery: Benefit of patient controlled analgesia (PCA) Ann Otolaryngol Chir Cervicofac. 1999;116:154–61. [PubMed] [Google Scholar]
- 13.Guru K, Manoor UK, Supe SS. A comprehensive review of head and neck cancer rehabilitation: Physical therapy perspectives. Indian J Palliat Care. 2012;18:87–97. doi: 10.4103/0973-1075.100820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bernabei R, Gambassi G, Lapane K, Landi F, Gatsonis C, Dunlop R, et al. Management of pain in elderly patients with cancer. JAMA. 1998;279:1877–82. doi: 10.1001/jama.279.23.1877. [DOI] [PubMed] [Google Scholar]
- 15.Higginson IJ, Gao W. Opioid prescribing for cancer pain during the last 3 months of life: Associated factors and 9-year trends in a Nationwide United Kingdom Cohort Study. J Clin Oncol. 2012;30:4373–9. doi: 10.1200/JCO.2012.42.0919. [DOI] [PubMed] [Google Scholar]
- 16.Björkman R, Ullman A, Hedner J. Morphine-sparing effect of diclofenac in cancer pain. Eur J Clin Pharm. 1993;44:1–5. doi: 10.1007/BF00315271. [DOI] [PubMed] [Google Scholar]
- 17.Mercadante S, Sapio M, Caligara M, Serretta R, Dardanoni G, Barresi L. Opioid-sparing effect of diclofenac in cancer pain. J Pain Symptom Manage. 1997;14:15–20. doi: 10.1016/S0885-3924(97)00005-5. [DOI] [PubMed] [Google Scholar]
- 18.Stockler M, Vardy J, Pillai A, Warr D. Acetaminophen (paracetamol) improves pain and well-being in people with advanced cancer already receiving a strong opioid regimen: A randomized, double-blind, placebo-controlled cross-over trial. JCO. 2004;22:3389–94. doi: 10.1200/JCO.2004.09.122. [DOI] [PubMed] [Google Scholar]
- 19.Sinatra RS, Jahr JS, Reynolds LW, Viscusi ER, Groudine SB, Payen-Champenois C. Efficacy and safety of single and repeated administration of 1 gram intravenous acetaminophen injection (Paracetamol) for pain management after major orthopedic surgery. Anesthesiology. 2005;102:822–83. doi: 10.1097/00000542-200504000-00019. [DOI] [PubMed] [Google Scholar]
- 20.Hein A, Norlander C, Blom L, Jakobsson J. Is pain prophylaxis in minor gynaecological surgery of clinical value? A double blind placebo controlled study of Paracetamol 1 gm versus lornoxicam 8 mg given orally. Ambul Surg. 2001;9:91–4. doi: 10.1016/s0966-6532(01)00078-6. [DOI] [PubMed] [Google Scholar]
- 21.Cakan T, Inan N, Culhaoglu S, Bakkal K, Başar H. Intravenous paracetamol improves the quality of postoperative analgesia but does not decrease narcotic requirements. J Neurosurg Anesthesiol. 2008;20:169–73. doi: 10.1097/ANA.0b013e3181705cfb. [DOI] [PubMed] [Google Scholar]
- 22.Fayaz MK, Abel RJ, Pugh SC, Hall JE, Djaiani G, Mecklenburgh JS. Opioid sparing effects of diclofenac and Paracetamol lead to improved outcomes after cardiac surgery. J Cardiothorac Vasc Anaesth. 2004;18:742–7. doi: 10.1053/j.jvca.2004.08.012. [DOI] [PubMed] [Google Scholar]
- 23.Hyllested M, Jones S, Pedersen JL, Kehlet H. Comparative effect of Paracetamol, NSAIDs or their combination in post-operative pain management: A qualitative review. Br J Anaesth. 2002;88:199–214. doi: 10.1093/bja/88.2.199. [DOI] [PubMed] [Google Scholar]
- 24.Remy C, Marret E, Bonnet F. Effects of acetaminophen on morphine side-effects and consumption after major surgery: Meta-analysis of randomized controlled trials. Br J Anaesth. 2005;94:505–13. doi: 10.1093/bja/aei085. [DOI] [PubMed] [Google Scholar]
- 25.Mathiesen O, Rasmussen ML, Dierking G, Lech K, Hilsted KL, Fomsgaard JS, et al. Pregabalin and dexamethasone in combination with paracetamol for postoperative pain control after abdominal hysterectomy. A randomized clinical trial. Acta Anaesthesiol Scand. 2009;53:227–35. doi: 10.1111/j.1399-6576.2008.01821.x. [DOI] [PubMed] [Google Scholar]
- 26.Ripamonti CI, Santini D, Maranzano E, Berti M, Rolia F, et al. Management of cancer pain: ESMO Clinical Practice Guidelines. Ann Oncol. 2012;23(suppl 7):139–54. doi: 10.1093/annonc/mds233. [DOI] [PubMed] [Google Scholar]
- 27.Piguet V, Desmeules J, Dayer P. Lack of acetaminophen ceiling effect on R-III nociceptive flexion reflex. Eur J Clin Pharmacol. 1998;53:321–4. doi: 10.1007/s002280050386. [DOI] [PubMed] [Google Scholar]
- 28.Juhl GI, Norholt SE, Tonnese E, Hiesse-Provost O, Jensen TS. Analgesic efficacy and safety of intravenous Paracetamol (acetaminophen) administered as a 2 g starting dose following 3rd molar surgery. Eur J Pain. 2006;10:371–7. doi: 10.1016/j.ejpain.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 29.Anderson BJ. Paracetamol (Acetaminophen): Mechanisms of action. Paediatr Anaesth. 2008;18:915–21. doi: 10.1111/j.1460-9592.2008.02764.x. [DOI] [PubMed] [Google Scholar]
- 30.Graham GG, Scott KF. Mechanism of action of paracetamol. Am J Ther. 2005;12:46–55. doi: 10.1097/00045391-200501000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Arici S, Gurbet A, Türker G, Yavaşcaoğlu B, Sahin S. Preemptive analgesic effects of intravenous paracetamol in total abdominal hysterectomy. AĞRI. 2009;21:54–61. [PubMed] [Google Scholar]


