Abstract
Background:
Snake bite is an important occupational and rural hazard because India has always been a land of Exotic snakes. In Maharashtra, common poisonous snakes are Cobra, Russell's Viper, Saw Scaled Viper, and Krait. It is a fact that inspite of heavy morbidity and mortality, very little attention is paid by the clinicians to this occupational hazard.
Aims:
To study the prevalence of poisonous and non-poisonous snake bites in part of Western Maharashtra with reference to age, sex, occupation, part of body bitten, time of bite and seasonal variation, and the types of poisonous snakes common in this locality and their clinical manifestations along with the systemic envenomation from various types of poisonous snakes and their effective management in reducing the mortality rate.
Materials and Methods:
This was a retrospective study conducted between May 2010 to May 2012 at a tertiary health care center in Maharashtra.
Result:
A total of 150 patients were studied in our hospital. Out of 150, 76 patients were of poisonous snake bite and 74 patients were of non-poisonous snake bite. Out of these 76 poisonous snake bites, 42 were viperine snake bites, 21 were neuroparalytic snake bites and 13 were locally toxic (LT) snake bites.
Conclusion:
Snake bite is a common life-threatening emergency in the study area. Delay in hospitalization is associated with poor prognosis and increased mortality rate due to consumptive coagulopathy, renal failure, and respiratory failure. Unusual complications like pulmonary edema, intracerebral hemorrhage, Disseminated intravascular coagulation (DIC) were observed in present study.
Keywords: Non-poisonous bite, neuroparalytic bite, poisonous bite, vasculotoxic bite
INTRODUCTION
In Maharashtra, common poisonous snakes are Cobra, Russell's Viper, Saw Scaled Viper, and Krait.[1] World mortality from snake bite is estimated as 50,000 to 1,00,000 annually (McNamee 2001) and the greatest number of reported snake bite death occurring in Indian subcontinent is 10,000 to 15,000 annually.[2] World Health Organization (WHO 1963) reports 40,000 annual deaths in tropical countries. Largest number of deaths reported in India are from Bengal, Uttar Pradesh (UP), Tamil Nadu, Bihar, and Maharashtra.[3] It is a fact that inspite of heavy morbidity and mortality, very little attention is paid by the clinicians to this occupational hazard.
MATERIALS AND METHODS
The present descriptive observational study was carried out in medicine wards of Krishna hospital, Karad, Satara, Maharashtra, India during May 2010 to May 2012. A total of 150 cases of snake bite were admitted in medicine wards during the study period. After obtaining consent, data was collected on pre-designed, pretested, and structured questionnaire by interviewing the study subjects who were hospitalized during the study period. A detailed information regarding demographic and epidemiological parameters such as age, sex, residence, occupation, site of bite and place of bite, type of snake if identified, etc., was obtained. Time interval to reach the health facility after snake bite and first aid received if any was asked to them. Thorough clinical examination was carried out in each case. For identification of type of snake bite (Vasculotoxic, VT, Neuroparalytic, and Non-poisonous) opinion from treating physician was taken. Subsequent information was collected on the day of discharge or death of the patient from the case paper of the patient.
RESULTS
A total of 150 patients were studied in our hospital. Out of 150, 76 patients were of poisonous snake bite and 74 patients were of non-poisonous snake bite. Out of these 76 poisonous snake bites, 42 were viperine snake bites, 21 were neuroparalytic snake bites, and 13 were locally toxic (LT) snake bites [Tables 1–18].
Table 1.
Age-wise prevalence of poisonous snake bites
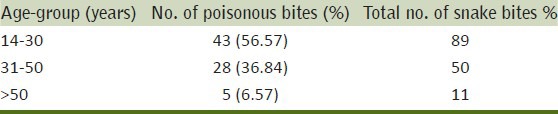
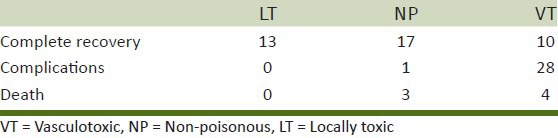
Table 18.
Comparative mortality in poisonous snake bite
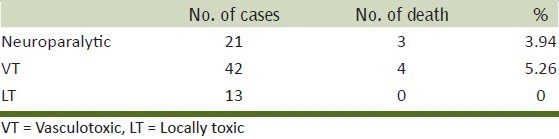
Table 2.
Occupational incidence of snake bites
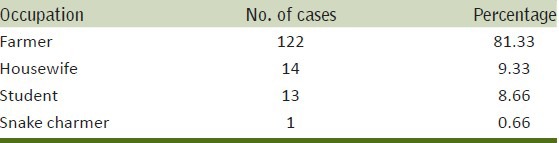
Table 3.
Sex incidence of snake bites
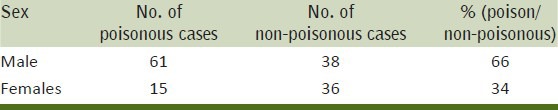
Table 4.
Incidence of snake bite with reference to site of bite
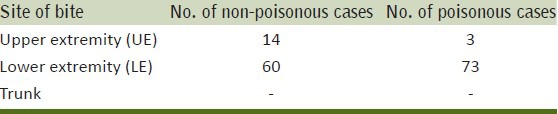
Table 5.
Relation of time with snake bite
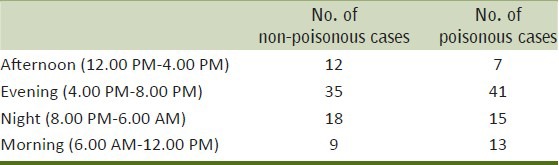
Table 6.
Seasonal incidence of snake bite
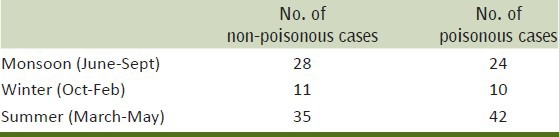
Table 7.
Incidence of snake seen and brought
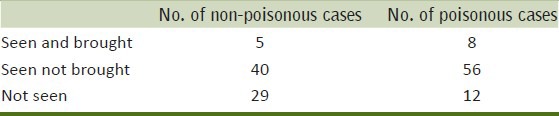
Table 8.
Incidence of poisonous snake bite with local toxicity
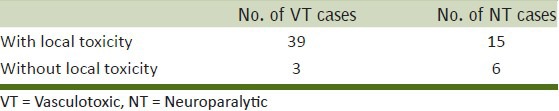
Table 9.
Loss of time from the bite till the admission
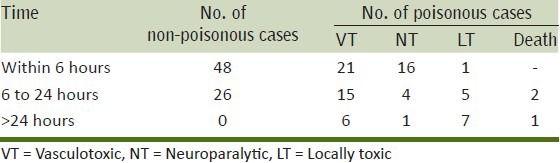
Table 10.
The no. of patients who received first-aid
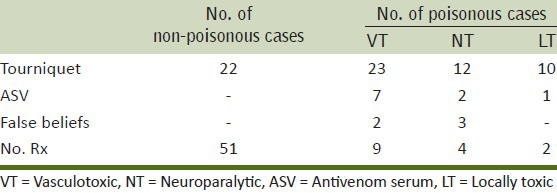
Table 11.
Incidence of local toxicity in poisonous snake bite
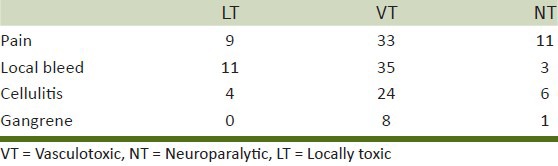
Table 12.
Incidence of symptomatology of neuro paralytic snake bite poisoning
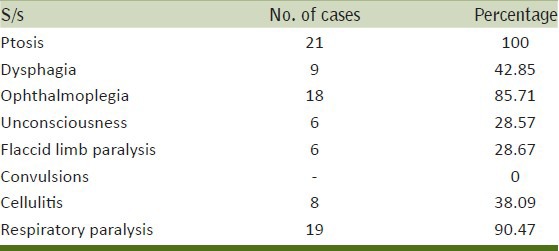
Table 13.
Incidence of symptomatology in viperine snake bite
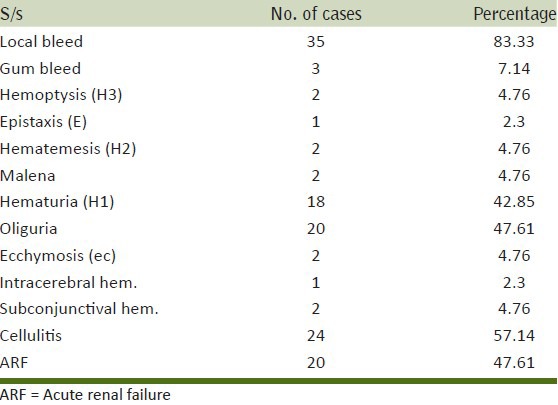
Table 14.
Incidence of complications of vasculotoxic snake bite
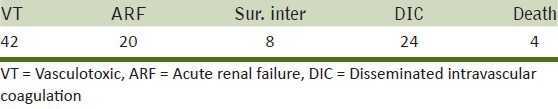
Table 15.
Type of treatment received in vasculotoxic snake bite
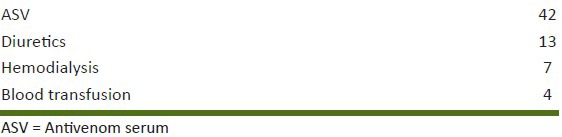
Table 16.
Duration of neuroparalytics on ventilator

Table 17.
Incidence in relation to condition at discharged
SUMMARY AND CONCLUSION
In all, 150 patients of snake bite were studied. Out of 150 patients, 74 patients had non-poisonous snake bites and 76 patients had poisonous snake bites. Maximum incidence of snake bite was found in farmers (81.33%) than in any other occupation. Males (66%) were bitten more than females (34%) among poisonous bites. Maximum incidence of snake bites was found in rural areas (85%) than urban areas (15%). Poisonous snake bites were more prevalent in rural than urban areas. Bites were commonly seen on the lower extremities 88.6% than upper (11.33%). Maximum bites were in the night (72.66%) than day time (27.33%) among which 73.68% were poisonous bites at night and 27% were poisonous bites at day time. Higher incidence of snake bites was found in summer (51.33%) i.e. March to May. In eight cases, the snakes were seen/identified. A total of 57.33% patients reported to medical help within 6 hours, among which 24.41% were VT and 18.60% were NT. Sixty-seven patients came with tourniquet application, out of which 45 had poisonous bite, out of which 9 patients had received ASV. Fifty-one cases did not receive any sort of medical help before admission. Five cases had received non-medical treatment. Time of onset of systemic manifestation was earlier in neuroparalytic snake bites than VT snake bite. VT snake bites (55.26%) were more common than neuroparalytic bites (27.63%). Commonest VT manifestation was local bleed (83.33%) and next on the list was cellulitis (57.14%). Hematuria (42.85%) was the commonest manifestation in those patients who developed ARF. Ptosis (100%) was the commonest and earliest manifestation of neuroparalytic snake bite. Out of VT snake bites, 20 were of ARF, 7 required hemodialysis. Four DIC patients received blood transfusion. Thirteen patients of ARF received diuretics and recovered completely. Thirteen cases were LT; out of them, 4 patients developed cellulitis. Nineteen patients with neuroparalytic bite required artificial ventilation. Seven patients died because they came late to seek medical treatment and by that time, complications were beyond control and were associated with systemic infection. Two patients developed anaphylactic reaction to ASV and were treated conservatively and recovered completely.
DISCUSSION
In India, it is believed that 2 lakh people are bitten by snakes and about 15,000-30,000 cases/year prove fatal.[2] In the present study, 150 cases of snake bites including poisonous and non-poisonous bites were studied in the medical wards of Krishna Hospital from 1st May 2010 to 31st May 2012. The number of poisonous cases were 76 and the number of non-poisonous cases were 74. Among the poisonous snake bites, the number of Viperine bites were 42, the number of neuroparalytic bites were 21 and the number of LT cases were 13. In the present study, maximum no. of patients bitten were between the age-group of 14-30 years of age. Next in order of frequency was the age-group 31-50 years. These observations go more in favor of the study of Russel et al. (1979)[4] and Hutchison et al. (1929). Among the group of 14-30 years, 43 patients had poisonous snake bite and in the age-group of 31-50 years, 28 patients had poisonous bites. In the age-group above 51, five bites were poisonous in nature.
Figure 1.

Ptosis in neuroparalytic snake bite
In the present study, 99 (66%) patients were male victims, whereas the female victims were 51 (34%) in number. All the previous reports mention the same findings. Ahuja and Singh[5] in 1954 reported the ratio as 4:1 (M: F). Bhat[6] et al. in 1974 reported the incidence as 7:3 (M: F).[6] Among male patients, 61 were poisonous, whereas in females, 15 were poisonous snake bites. In the present study, 122 were farmers, 13 were students, 14 were housewives, and 1 was a snake charmer. Studies undertaken by Bhat[6] et al. (1974), Saini[7] et al. in (1984), and Sarangi[8] et al. in (1977) showed the incidence in farmers to be 75%, 78%, and 72%, respectively. In the present study, rural prevalence of snake bite was 117 out of 150 cases. Among them, 69 were poisonous snake bites. The prevalence in urban area was 33 out of 150 cases, among which 7 were poisonous cases. Incidence of bites in present studies are as follows. In lower extremities bites are 133 (88.66%) and in upper extremities 17 (11.33%). Among them, upper extremity poisonous cases were 3 and lower extremity poisonous cases were 73. Reid[9] mentions that most of the bites in tropical countries are on lower extremities because the victims are bitten by treading on or near the snake, while in non-tropical countries most bites are on fingers and hands because the victim deliberately handles the snake. In the present study, the day was divided into four groups. Maximum number of cases were detected in the interval between 4.00 PM to 8.00 PM. The documented figure was 109 among 150 patients. Next on the list was the time interval between 8.00 PM to 6.00 AM where number of patients bitten was 41. These figures show close resemblance with the observation of Virmani and Dutt.[10] They have noted 12% cases during day time. In the present study, higher incidence was found in summer (March to May), 77 (51.33%) were total snake bites in summer, among them 42 were poisonous bites and 35 were non-poisonous bites. Next on the list was monsoon where the total number of snake bites was 52, among which 24 were poisonous bites and 28 were non-poisonous. Neuroparalytic snake bites were more at the end of summer and beginning of monsoon. Incidence of VT bites were comparatively more in winter. We defined summer as period of the year from March to May, winter period is between October to February, and Monsoon is June to September. Banerjee[11] (1978) noted incidence of 70-80% during May to October. In the present study, we have noted one case of a snake catcher from Satara district who was a professional. He had a neuroparalytic cobra bite. Remaining cases were all unprovoked.
In the present study, only eight patients had brought snakes along with them and they were identified in this hospital. Among them three were cobras, two vipers, one was Krait, and two were echis carinatus. In the present study, 86 (57.33%) patients were admitted within first 6 hrs. Among which 21 cases (24.41%) were VT and 16 (18.60%) were neuroparalytic. Seventy-six percent of neuroparalytic bites got admitted within the first 6 hrs. Fifty-two patients were admitted within the first 24 hrs but after 6 hrs, among which 15 were VT and 4 were NT. Two NT bites expired within 1 to 2 hrs after admission. In a series of 135 patient by Lahori et al., 85% patients were admitted in the first 24 hours after bite. Among 150 patients, 67 (44.66%) had applied tourniquet. Out of 67 patients, 45 were poisonous bites and 22 non-poisonous bites. Out of 45 cases of poisonous bites, 23 were VT, 12 were neuroparalytic, and 10 were LTbites. In a study conducted by George Watt[12] et al. (May 1988), tourniquet was applied in 94% patients, 4 were asymptomatic prior to release of their tourniquet, and in 11 patients symptoms worsened precipitously. In the present series, 53 (69.73%) patients had local pain. Among which 9 (16.98%) were LT, 33 (62.26%) were VT and 11 (20.75%) were neuroparalytic bites. In the present study, local edema was present in 64 (84.20%) patients of poisonous snake bite. Out of which 40 patients had VT snake bite, 11 patients had neuroparalytic snake bite, and 13 bites were LT. In VT bite 95.23% patients had local edema while in neuroparalytic snake bite 52.38% patients had local edema. Local cellulitis was seen in 24 (57.14%) patients of VT snake bite and 6 (28.57%) patients of neuroparalytic snake bites.
A total of 32.66% of the patients in the present study had local bleeding. Out of which 11 patients had LT bite, 35 patients had VT bite and 3 patients had neuroparalytic snake bites. In the present study, 3 (7.14%) patients had gum bleeding but Purohit (1944) described gum bleeding as the commonest manifestation of viperine bite. Corkill[13] (1956) described hematuria as the commonest manifestation but in the present study, 18 (42.85%) patients had hematuria. Ecchymosis was present in 2 (4.75%) patients in the present study but Bhat (1974) described ecchymosis in 43% of patients. Hematemesis was present in 2 (4.75%) patients in the present study, whereas Bhat[6] showed that 37 patients among 310 patients had hematemesis. In the present study, 2 (4.75%) patients had haemoptysis and 1 (2.3%) patient had epistaxis. Fundal hemorrhage was seen in one patient (2.3%) who expired within 2 days. Reid[14] et al. in his study of 281 cases of viper bite had not found a single case with fundal haemorrhage. Saini[7] and Sharma et al. (1984) in their study of 200 cases of poisonous bite do not report about fundal hemorrhage. In the present study, 100% patients developed ptosis among 21 cases of Neuroparalytic bite. Ophthalmoplegia was seen in 18 (85.71%) patients of Neuroparalytic bite. Six (28.57%) patients became unconscious, 6 (28.57%) patients with flaccid limb paralysis, 19 (90.47%) patients developed respiratory paralysis, among which 15 patients needed respirator.
ARF was seen in 20/42, 47.61% of patients of VT bite. In all the cases of ARF except one, DIC was the cause for it. Basu et al. (1977) observed ARF in 27 cases of viper bite and attributed it to circulatory collapse and shock in 5 cases, direct nephrotoxicity in 4 cases. In the present study, 7 patients died of poisonous snake bites out of which 3 (3.94%) were neuroparalytic bite patients and 4 were VT bite patients. Among neuroparalytic bites, mortality rate (14.28%) was higher than in VT bite (9.52%). All 3 patients died because of delay in receiving respiratory assistance. Among four deaths of VT bites, three patients died of acute renal failure, and one patient died of DIC and intracerebral hemorrhage. Lahori[14] et al. (1981) showed mortality rate to be 2% and 3 deaths were due to central nervous system (CNS) involvement.
Bleeding time, clotting time was raised in all patients of VT snake bites. Similar incidence has been reported by Saini[7] et al. and Lahori et al. in their studies. BT, CT, PT gradually returned to normal within 3-4 days after full dose of ASV and blood transfusion in present study. Prothrombin time was abnormal in almost all the VT bites. In the present study, thrombocytopenia was noted in 24/41 patients of VT bite with coagulation defects. Saini[7] et al. (1981) noted thrombocytopenia in only 5% patients and Reid[9] tioned that platelet count may be depressed but is often normal in viperine bites.
In the present study, two patients developed anaphylaxis for ASV and they were treated with steroids and adrenaline. In the present study, 76/150 (50.66%) patients received ASV. According to Reid et al., ASV is not very effective against local effects of venom. In the present study, 69/76 reversed completely. Three deaths in neuroparalytics were because of delay in administration of ASV producing respiratory paralysis and delay in ventilatory support who were transferred from other hospital to our hospital. In the present study, four (9.52%) patients of viperine snake bites received blood transfusions. Saini[7] et al. (1984) and Reid et al. feel that blood transfusion is not required routinely. In the present series, neostigmine with atropine was given to 13 patients out of 21 patients of neuroparalytic snake bite. Most of the patients responded to it within 4-6 hours. In these patients, first to improve was respiratory paralysis, then ophthalmoplegia and lastly ptosis. Dubay[15] et al. (1981), Banerjee[16] et al., Dash[17] et al. (1976) are strong supporters of this regime but Reid[9] had doubts about the benefits of this mode of therapy.
In the present series, ARF was observed in 20 patients among 42 (47.61%) patients of VT snake bite. Eleven patients were treated conservatively with diuretics, renal diet, and fluid restriction. Seven patients needed hemodialysis. Three patients died of renal failure among which 2 patients died after hemodialysis and one died because of acute renal failure. Saini[7] et al. reported 8 cases of ARF and 7 cases recovered with conservative treatment. In the present study, among 21 patients of neuroparalytic bite (71.42%), 15 needed ventilatory support and 4 (19.04%) patients needed only intubation. Among which 3 patients died. Total duration of ventilator was less than 24 hrs for most of the patients except one. Not a single patient needed tracheostomy. In the present study, 9 patients required surgical intervention, out of which 8 patients had viper bite and one patient had Elapid bite. Reid[17] et al. recommends early surgical intervention to prevent extension of infection and development of gangrene.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Warell DA. Injuries, envenoming, poisoning and allergic reactions caused by animals. Oxford Textbook of Med 1984. 1984:635–640. [Google Scholar]
- 2.Vol. 10. WHO bulletin; 1954. Swaroop and Grab. Snake bite Mortality in world; p. 35. [PMC free article] [PubMed] [Google Scholar]
- 3.Manson Bahr Poisonous snakes, Manson's Tropical Diseases. 1968;(Ch XL VII):749–60. [Google Scholar]
- 4.Russell FE, Emery CA. Effects of corticosteroids on lethality of Ancistrodon contortrix venon. Am J Med Sci. 1961;241:507–11. doi: 10.1097/00000441-196104000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Ahuja MM. Progress in clinical medicine in India. Second Series. 1978:136–77. [Google Scholar]
- 6.Bhat RN. Viperine snake poisoning in Jammu. J Indian Med Assoc. 1974;63:383–92. [PubMed] [Google Scholar]
- 7.Saini RK, Sharma S, Singhs, Pathania NS. Snake bite poisoning: A preliminary report. J Assoc Physicians India. 1984;32:195–7. [PubMed] [Google Scholar]
- 8.Sarangi A, Jana I, Das JP. Clinical profile of snake bite poisoning. J Assoc Physicians India. 1977;25:55–60. [PubMed] [Google Scholar]
- 9.Reid HA, Theakston RD. The management of snake bite. Bull WHO. 1983;61:885–95. [PMC free article] [PubMed] [Google Scholar]
- 10.Virmani SK, Dutt OP. A profile of snake bite poisoning in Jammu region. J Indian Med Assoc. 1987;85:132–4. [PubMed] [Google Scholar]
- 11.Banerjee RN. Poisonous snakes of India, progress in, clinical medicine’ in India. In: Ahuja MS, editor. 1st ed. 1987. pp. 136–177. [Google Scholar]
- 12.Watt G, Padre L, Tuazon ML, Theakston RD, Laughlin LW. Tourniquet application after cobra bite: Delay in the onset of neurotoxicity and the dangers of sudden release. Am J Trop Med Hyg. 1988;38:618–22. doi: 10.4269/ajtmh.1988.38.618. [DOI] [PubMed] [Google Scholar]
- 13.Corkill NL, Venoms EE, Euckley, Porges N. Washington D.C: 1956. p. 331. [Google Scholar]
- 14.Reid HA, Thean PC, Martin WJ. Specific antivenin and prednisolone in viper bite poisoning. Br Med J. 1963:1378–80. doi: 10.1136/bmj.2.5369.1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dubey GK, Joglekar VK, Chaubey BS, Kalamkar RB. Neostigmine in the treatment of snake bite. J Assoc Physicians India. 1981;29:229–31. [PubMed] [Google Scholar]
- 16.Banerjee RN, Siddiqui ZA. Proc. 5th international symposium on Animal plant and Microbial Toxins, Toxico; 1976. Therapeutic advance in the treatment of snake venom poisoning. [Google Scholar]
- 17.Dash SC, Ghosh SK, Mathur DC, Jha GN, Prasad U, Grewal KS. Neurotoxic snake bite-dramatic recovery following neostigmine therapy. J Assoc Physicians India. 1976;24:535–7. [PubMed] [Google Scholar]


