Abstract
Herbicide poisoning is most common method of suicide in India and it is associated with high morbidity and mortality. Among different herbicidal poisonings the most predominantly found poisonings are paraquat and glyphosate. These compounds are highly toxic and their poisonings require proper management techniques. High fatality is seen in these cases which are mainly due to its inherent toxicity and lack of effective treatment. Common symptoms of these poisonings includes gastrointestinal corrosive effects with mouth and throat, epigastric pain and dysphagia, acid-base imbalance, pulmonary edema, shock and arrhythmia. Long term health effects include pulmonary fibrosis, renal failure, hepatic failure, heart failure, multi-organ failure or death. No proven antidote exists for these poisonings. So the treatment is mainly supportive. Initially gastric lavage or whole-gut irrigation using adsorbents such as Fuller's earth, bentonite or activated charcoal is recommended. In case of renal failure hemodialysis or hemoperfusion may be considered. However novel approaches like treatment with N-acetylcysteine, vitamin C, vitamin E, cyclophosphamide may also be helpful.
Keywords: Glyphosate, herbicide, poisoning, paraquat, treatment
INTRODUCTION
Poisoning from pesticides and other agricultural chemicals is a major public health problem worldwide, especially in the developing countries. Among them, herbicides like paraquat and glyphospate are most common poisonings responsible for high morbidity and mortality. Paraquat (1, 1’-dimethyl-4, 4’-bipyridium dichloride) is non-selective contact herbicide that is relatively widely-used. It is a very dangerous pollutant of the environment, as it readily binds to both clay and organic matter in soil and is very slowly biodegraded.[1] This acute poisoning is common method of suicide in India.[2] Poisoning due to this chemical is observed because of the easy availability, improper storage methods and lack of awareness of the potential harm. As they are highly toxic compounds, management of these poisonings requires a great deal of skill and knowledge of proper management procedures.[3] Toxic effects of paraquat originate from the production of free radicals formed by the cyclic oxidation-reduction reactions of the compound in tissues.[4] The symptoms after ingestion are burning sensation in the mouth, throat, chest, upper abdomen, nausea, vomiting, abdominal pain and diarrhea. These gastrointestinal symptoms settle after 2-3 days if the patient survives. Ulceration of the mouth, acute renal failure and jaundice may follow a few days later. The early or delayed appearance of respiratory distress or failure is one of the characteristic feature of the condition.[5] Common symptoms of central nervous system (CNS) and other systems include giddiness, headache, fever, myalgia, lethargy and coma. High fatality is seen in these cases which are mainly due to its inherent toxicity and lack of effective treatment. For treatment of these poisoning there are no widely accepted guidelines.[6] To prevent systemic toxicity due to intoxication of these chemicals immediate treatment is necessary. In case of ingestion of herbicides like paraquat and glyphospate gastric lavage or whole-gut irrigation using adsorbents such as Fuller's earth, bentonite or activated charcoal is recommended.[7]
Glyphosate is an a non-selective herbicide. The mechanism by which glyphosate causes toxicity is complicated due to its composition. Common symptoms of this poisoning include gastrointestinal corrosive effects with mouth and throat, epigastric pain and dysphagia. In severe cases, impaired consciousness, arrhythmias, pulmonary edema, shock, renal failure requiring hemodialysis, hyperkalemia and metabolic acidosis are also seen. There is a sensible relationship between the amount of compound ingested and the effects caused by it.[8] There is no specific antidote for glyphosate and treatment is mainly supportive or activated charcoal and gastric lavage can be considered in patients who are admitted within one after ingestion of poison.[9]
Objectives
In the present study we aimed to study the demographics of patient, clinical characteristics and treatment pattern for herbicide poisoning in tertiary care hospital.
MATERIALS AND METHODS
A retrospective observational study was conducted on patients with herbicide poisoning admitted in emergency ward of tertiary care Hospital in South India between January 2004-2012. Sixty patients were included in the study. A detailed history had been taken from the patient records of medical record section. Demographic characteristics like age, sex, type of exposure, pre-hospitalization period, clinical features, type of compound along with treatment and outcome were obtained from the patient files. These were recorded using standardized data collection forms and were analyzed using SPSS 16.0 package.
RESULTS
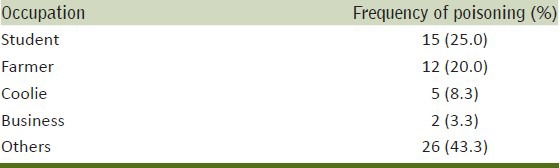
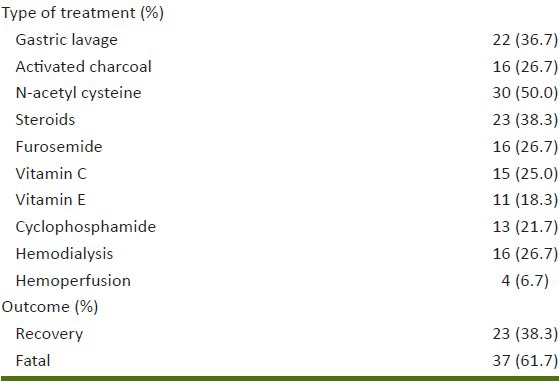
During the study period, 60 patients of Herbicide poisoning were admitted to the emergency ward of tertiary care Hospital in South India. Gender wise distribution showed that majority of them were males which constitute 60% of the study population. There were 36 male and 24 female patients and the male/female ratio was almost 3:2. The median age of the study population was found to be 25.38 ± 9.136 yrs. Majority of poisoning were intentional (95%). The median pre-hospitalization period was found to be 3.50 (9.25) hrs. The clinical characteristics of herbicide poisoning patients mainly includes incidence of vomiting 41 (68.3%), oral ulcers 19 (31.7%), throat discomfort 16 (26.7%), abdominal pain 14 (23.3%), dysphagia 10 (16.7%) and dyspnea 6 (10.0%). Among the study population, 6.7% (n = 4) of patients had psychiatric illness. Table 1 presents the basic demographic details of paraquat poisoning patients. Different herbicide compounds consumed are paraquat 47 (78.3%) and glyphosate 13 (21.7%). Herbicide compounds consumed by the patients are given in Table 2. Among the study population majority of them were students n = 15 (25.0%)) followed by farmers (n = 12 (20.0%). Details are given in the Table 3. Among the different treatment approaches majority of the patients 22 (36.7%) received gastric lavage and 16 (26.7%) patients received activated charcoal at initial stage of therapy. Among 60, 30 (50.0%) patients received N-acetylcysteine (NAC), 23 (38.3%) patients received steroids, furosemide16 (26.7%), vitaminC15 (25.0%), cyclophosphamide 13 (21.7%) and Vitamin E11 (18.3%). A total of 16 (26.7%) patients underwent hemodialysis and hemoperfusion was done only in 4 (6.7%). The outcome analysis of herbicide poisoning cases admitted during study period, 23 (38.3%) of them recovered, 37 (61.7%) of them were expired.
Table 1.
Demographical and clinical characteristics of herbicide poisoning
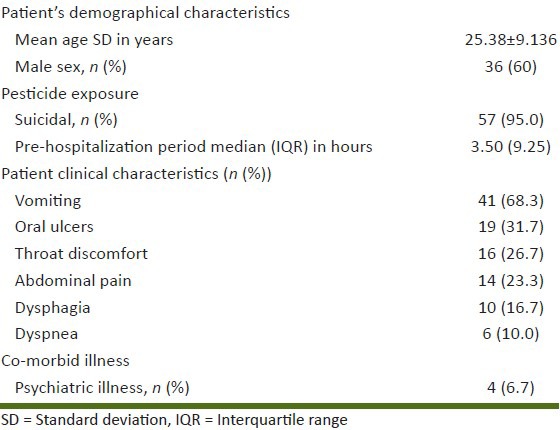
Table 2.
Percentage of different herbicide poisoning

Table 3.
Occupation and Herbicide poisoning
Details regarding treatment and outcome are given in Table 4.
Table 4.
Different treatment pattern in herbicide poisoning
DISCUSSION
In the present study the Herbicide poisoning cases included were of paraquat (78.3%) and glyphosate (21.7%). Gender wise distribution of study population showed that males (60%) predominated over females (40%). The male to female ratio was 1.5:1 with mean age of 25.38 ± 9.136 years. A similar study conducted in Soonchunhyang Hospital (SCH) in Cheonan, Korea by Kim et al., 2009 showed similar results with male to female ratio of 1.3:1 with mean age 26.58 ± 9.473 years in males and mean age of 23.58 ± 8.480 years in females.[10] In the present study, mean pre-hospitalization period was found to be 11.250 ± 19.96 hrs. In a study conducted by Hong et al., 2000, the mean pre-hospitalization period was found to be 15.6 ± 30.8 in survivors and 1.7 ± 2.1 in non-survivors.[11] This indicates that the mortality rate not only depends on pre-hospitalization period but also depends on other factors like type and amount of compound consumed. In another study conducted by Kim et al., 2009, the mean pre-hospitalization period was found to be 15.93 ± 26.03.[10]
Among the total pesticide exposures herbicides accounts for 29% according to British pesticide exposure survey by the UK National Poisons Information Service in 2005. Glyphosate was the fourth most common exposure, and the third most common implicated in self-harm cases.[12] Among the total acute pesticide poisonings, the majority of deaths were from intentional self-poisoning with paraquat, organophosphorus pesticides (OP) and aluminium phosphide.[13] In pesticide poisoning the fatality rate is between 18% and 23% with highest fatality rates in case of paraquat.[14,15,16,17] In the present study majority of the herbicide poisonings were due to deliberate self-harm (95%) with high mortality rate 61.7%.
The common clinical features of herbicide poisoning as observed in our study are as follows: Vomiting (68.3%), oral ulcers (31.7%), throat discomfort (26.7%), abdominal pain (23.3%), dysphagia (16.7%) and dyspnea (10%). As per study conducted by Sandhu et al., 2003 the common symptoms for paraquat poisoning were vomiting (100%) followed by oral ulceration (59%), dysphagia (53%) and dyspnea (41%).[18] For glyphosate poisoning the clinical manifestations include corrosive effects on the gastrointestinal tract, Tachy- and brady-arrhythmias, renal failure, elevated liver enzymes, hyperkalemia and metabolic acidosis.[19]
Out of 60 patients 4 (6.7%) patients had psychiatric illness. It is one of the risk factor for the intentional self-harm. According Eddleston and Phillips psychiatric illness is the one of the major risk factor for self-poisoning. By prophylactic medical management it is possible to reduce the incidences of self harm.[20] Due to its inherent toxicity and the lack of effective treatment paraquat has high mortality rate. The treatment varies from supportive care alone to various combinations of immune-modulation, antioxidant therapy, hemoperfusion and hemodialysis as there are no widely accepted guidelines.[6]
In the present study treatment pattern analysis showed that 22 (36.7%) patients were treated with gastric lavage and 16 (26.7%) patients were treated with activated charcoal at the initial stage of therapy. Inducing emesis is not recommended instead gastric lavage might be helpful when performed within 1 hour of ingestion, although it may be useful up to 24 hours after ingestion.[9,21] Hemodialysis and Hemoperfusion were performed in 16 (26.7%) and 4 (6.7%) respectively. In our study out of 60 patients 17 patients had developed acute renal failure and 8 of these patients were given dialysis for acute renal failure (Hemodialysis in six and Hemoperfusion in two). A study conducted by Koo et al., supports that the accumulated paraquat elimination from lungs depends minimally on plasma concentration. An uncontrolled study conducted by Koo et al., showed that number of survival days were prolonged but there was no difference in mortality when hemoperfusion is given along with continued venovenous hemofiltration (CVVH) when compared to hemoperfusion alone in a group of 80 patients with paraquat self poisoning and mortality between these two groups was found to be 63.6% versus 66.7%.[22,23]
The major event of free radical injury primarily affects the lungs therefore the use of anti-oxidants was supported by some groups (Vitamin C 4000 mg/day and Vitamin E 250 mg/day) even though their efficacy is unproven.[24,25] In the present study vitamin C was given in 15 (25%) and vitamin E in 11 (18.3%). There were very few studies carried out to evaluate the role of vitamin C and vitamin E in paraquat poisoning. An observational study conducted by Yasaka et al., 1986 in nine patients showed that the mortality rate was 78% in patients who received vitamin E[26] and observational study in five patients conducted by Hong et al., 2002 showed that the mortality rate was 0% in patients who received vitamin C.[27]
The effectiveness of pulse therapy using steroids and cyclophosphamide in preventing pulmonary fibrosis was supported by some authors.[28,29] Assessment of therapy in our study showed that 23 (38.3%) were given steroids and 13 (21.7%) were given cyclophosphamide.
An observational study in five patients conducted by Agarwal et al., 2006 showed that the mortality rate was 60% in patients who received steroids and cyclophosphamide.[30] In our study NAC was administered to 30 (50%) patients. NAC is an excellent source of sulfhydryl groups acting directly as a free radical scavenger thus having potentially beneficial effects in paraquat poisoning but it has been minimally studied in human paraquat poisoning.[31] In our study furosemide was given in 16 (26.7%) patients.
CONCLUSION
This study showed that poisoning with herbicides is associated with high morbidity and mortality. Clinical signs and symptoms may vary widely depending upon the type and amount of compound ingested, pre-hospitalization period etc., Very limited data is available in the literature with respect to treatment pattern of herbicide poisoning. However novel approaches like treatment with NAC, vitamin C, vitamin E, cyclophosphamide, hemodialysis and hemoperfusion may be useful in reduction of high mortality rate. Controlled trials with different treatment modalities may help in giving beneficial information in these patients.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Shopova VL, Dancheva VY, Salovsky PT, Stoyanova AM, Lukano TH. Protective effect of U-74389G on paraquat induced pneumotoxicity in rats. Environ Toxicol Pharmacol. 2002;24:167–73. doi: 10.1016/j.etap.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 2.Gururaj G, Isaac MK, Subbakrishna DK, Ranjani R. Risk factors for completed suicides: A case-control study from Bangalore, India. In Control Saf Promot. 2004;11:183–91. doi: 10.1080/156609704/233/289706. [DOI] [PubMed] [Google Scholar]
- 3.Vale JA, Meredith TJ, Buckley BM. Paraquat poisoning: Clinical features and immediate general management. Hum Toxicol. 1987;6:41–7. doi: 10.1177/096032718700600107. [DOI] [PubMed] [Google Scholar]
- 4.Fung TK, Huang TY, Chan JT. A case of paraquat poisoning. Hong Kong Pract. 1999;21:317–9. [Google Scholar]
- 5.Hoffman S, Jedeikin R, Korzets Z, Shapiro AL, Kaplan R, Bernheim J. Successful management of severe paraquat poisoning. Chest. 1983;84:107–9. doi: 10.1378/chest.84.1.107. [DOI] [PubMed] [Google Scholar]
- 6.Gawarammana IB, Buckley NA. Medical management of paraquat ingestion. Br J Clin Pharmacol. 2011;72:745–57. doi: 10.1111/j.1365-2125.2011.04026.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dasta JF. Paraquat poisoning: A review. Am J Health Syst Pharm. 1978;35:1368–72. [PubMed] [Google Scholar]
- 8.Bradberry SM, Proudfoot AT, Vale JA. Glyphosate poisoning. Toxicol Rev. 2004;23:159–67. doi: 10.2165/00139709-200423030-00003. [DOI] [PubMed] [Google Scholar]
- 9.Beswick E, Millo J. Fatal poisoning with glyphosate-surfactant herbicide. J Iran Chem Soc. 2011;12:37–9. [Google Scholar]
- 10.Kim SJ, Gil HW, Yang JO, Lee EY, Hong SY. The clinical features of acute kidney injury in patients with acute paraquat intoxication. Nephrol Dial Transplant. 2009;24:1226–32. doi: 10.1093/ndt/gfn615. [DOI] [PubMed] [Google Scholar]
- 11.Hong SY, Yang DH, Hwang KY. Associations between laboratory parameters and outcome of paraquat poisoning. Toxicol Lett. 2000;118:53–9. doi: 10.1016/s0378-4274(00)00264-2. [DOI] [PubMed] [Google Scholar]
- 12.Adams RD, Good AM, Bateman DN. UK: 2005. Aug, Pesticide Exposure Monitoring Using NPIS Resources. NPIS, Edinburgh. [Google Scholar]
- 13.Gupta PK. Pesticide exposure-Indian scene. Toxicology. 2004;198:83–90. doi: 10.1016/j.tox.2004.01.021. [DOI] [PubMed] [Google Scholar]
- 14.Sheu JJ, Wang JD, Wu YK. Determinants of lethality from suicidal pesticide poisoning in metropolitan HsinChu. Vet Hum Toxicol. 1998;40:332–6. [PubMed] [Google Scholar]
- 15.van der Hoek W, Konradsen F. Risk factors for acute pesticide poisoning in Sri Lanka. Trop Med Int Health. 2005;10:589–96. doi: 10.1111/j.1365-3156.2005.01416.x. [DOI] [PubMed] [Google Scholar]
- 16.Srinivas Rao Ch, Venkateswarlu V, Surender T, Eddleston M, Buckley NA. Pesticide poisoning in south India: Opportunities for prevention and improved medical management. Trop Med Int Health. 2005;10:581–8. doi: 10.1111/j.1365-3156.2005.01412.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nagami H, Nishigaki Y, Matsushima S, Matsushita T, Asanuma S, Yajima N, et al. Hospital-based survey of pesticide poisoning in Japan, 1998-2002. Int J Occup Environ Health. 2005;11:180–4. doi: 10.1179/oeh.2005.11.2.180. [DOI] [PubMed] [Google Scholar]
- 18.Sandhu JS, Dhiman A, Mahajan R, Sandhu P. Outcome of paraquat poisoning- a five year study. Indian J Nephrol. 2003;13:64–8. [Google Scholar]
- 19.National Pesticide Information Center. Zinc Phosphide [internet] 2010. [Last accessed on 2013 Apr 15]. Available from: npic.orst.edu/ingred/zp.html .
- 20.Eddleston M, Phillips MR. Self poisoning with pesticides. BMJ. 2004;328:42–4. doi: 10.1136/bmj.328.7430.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vale JA, Kulig K. American Academy of Clinical Toxicology, European Association of Poisons Centres and Clinical Toxicologists. Position paper: Gastric lavage. J Toxicol Clin Toxicol. 2004;42:933–43. doi: 10.1081/clt-200045006. [DOI] [PubMed] [Google Scholar]
- 22.Koo JR, Kim JC, Yoon JW, Kim GH, Jeon RW, Kim HJ, et al. Failure of continuous venovenous hemofiltration to prevent death in paraquat poisoning. Am J Kidney Dis. 2002;39:55–9. doi: 10.1053/ajkd.2002.29880. [DOI] [PubMed] [Google Scholar]
- 23.Van de Vyver FL, Giuliano RA, Paulus GJ, Verpooten GA, Franke JP, De Zeeuw RA, et al. Hemoperfusion-hemodialysis ineffective for paraquat removal in life-threatening poisoning? J Toxicol Clin Toxicol. 1985;23:117–31. doi: 10.3109/15563658508990622. [DOI] [PubMed] [Google Scholar]
- 24.Bismuth C, Garnier R, Baud FJ, Muszynski J, Keyes C. Paraquat poisoning: An overview of the current status. Drug Saf. 1990;5:243–51. doi: 10.2165/00002018-199005040-00002. [DOI] [PubMed] [Google Scholar]
- 25.Bateman DN. Pharmacological treatments of paraquat poisoning. Hum Toxicol. 1987;6:57–62. doi: 10.1177/096032718700600109. [DOI] [PubMed] [Google Scholar]
- 26.Yasaka T, Okudaira K, Fujito H, Matsumoto J, Ohya I, Miyamoto Y. Further studies of lipid peroxidation in human paraquat poisoning. Arch Intern Med. 1986;146:681–5. [PubMed] [Google Scholar]
- 27.Hong SY, Hwang KY, Lee EY, Eun SW, Cho SR, Han CS, et al. Effect of vitamin C on plasma total antioxidant status in patients with paraquat intoxication. Toxicol Lett. 2002;126:51–9. doi: 10.1016/s0378-4274(01)00431-3. [DOI] [PubMed] [Google Scholar]
- 28.Lin JL, Leu ML, Liu YC, Chen GH. A prospective clinical trial of pulse therapy with glucocorticoids and cyclophosphamide in moderate to severe paraquat poisoned patients. Am J Respir Crit Care Med. 1999;159:357–60. doi: 10.1164/ajrccm.159.2.9803089. [DOI] [PubMed] [Google Scholar]
- 29.Buckley NA, Lin JL. Pulse corticosteroids and cyclophosphamide in paraquat poisoning. Am J Respir Crit Care Med. 2001;163:585. doi: 10.1164/ajrccm.163.2.16310a. [DOI] [PubMed] [Google Scholar]
- 30.Agarwal R, Srinivas R, Aggarwal AN, Gupta D. Experience with paraquat poisoning in a respiratory intensive care unit in North India. Singapore Med J. 2006;47:1033–7. [PubMed] [Google Scholar]
- 31.Moldeus P, Cotgreave IA, Berggren M. Lung protection by a thiol containing antioxidant: N acetylcysteine. Respiration. 1986;50:31–42. doi: 10.1159/000195086. [DOI] [PubMed] [Google Scholar]


