Abstract
Hypothalamic leptin action promotes negative energy balance and modulates glucose homeostasis, as well as serving as a permissive signal to the neuroendocrine axes that control growth and reproduction. Since the initial discovery of leptin 20 years ago, we have learned a great deal about the molecular mechanisms of leptin action. An important aspect of this has been the dissection of the cellular mechanisms of leptin signaling, and how specific leptin signals influence physiology. Leptin acts via the long form of the leptin receptor, LepRb. LepRb activation and subsequent tyrosine phosphorylation recruits and activates multiple signaling pathways, including STAT transcription factors, SHP2 and ERK signaling, the IRS-protein/PI3Kinase pathway, and SH2B1. Each of these pathways controls specific aspects of leptin action and physiology. Important inhibitory pathways mediated by suppressor of cytokine signaling (SOCS) proteins and protein tyrosine phosphatases (PTPases) also limit physiologic leptin action. This review summarizes the signaling pathways engaged by LepRb and their effects on energy balance, glucose homeostasis, and reproduction. Particular emphasis is given to the multiple mouse models which have been used to elucidate these functions in vivo.
Obesity and its many comorbidities present a significant challenge to public health in the United States. The health care costs associated with obesity total more than $147 billion annually. In addition to the economic burden, obesity results in premature death and disability from stroke, cardiovascular disease, and type 2 diabetes mellitus (T2DM) (http://www.cdc.gov/obesity/data/adult.html accessed 6/29/14). Furthermore, the obesity epidemic is no longer confined to the United States. Worldwide, more than 1.4 billion adults were overweight or obese in 2008(Danaei, et al. 2011). Clearly the need for anti-obesity therapies is large and growing larger, yet no pharmacotherapies have achieved more than minimal success in promoting long-term weight loss.
At its most basic level, body weight is determined by the amount of energy taken in relative to energy expenditure(Schwartz, et al. 2000). If energy intake exceeds energy expenditure, excess energy accumulates in the form of triglycerides stored in adipose tissue, resulting in weight gain and obesity. The brain integrates signals of long-term energy stores with other physiologic inputs to modulate energy intake relative to energy expenditure, however. When adipose energy (fat) stores fall, hunger increases and energy expenditure decreases to defend body energy stores; conversely, the brain responds to nutritional surfeit by permitting increased energy expenditure and decreased feeding to maintain a constant body weight.
One of the most important and widely studied players in the control of energy balance is the hormone leptin (Elmquist, et al. 2005; Friedman and Halaas 1998). Leptin was discovered by Friedman and colleagues in 1994; defects in leptin production underlie the massive obesity observed in ob/ob mice(Zhang, et al. 1994). Leptin is produced in adipose tissue in proportion to triglyceride stores, and serves as a critical indicator of an organism's long-term energy status(Frederich, et al. 1995a; Maffei, et al. 1995). Leptin acts primarily in the brain, especially the hypothalamus, where its action is integrated with that of other adipokines, gastrokines, and other signals to coordinate energy homeostasis (Bates and Myers 2003; Friedman and Halaas 1998; Myers, et al. 2009; Ring and Zeltser 2010). In addition to leptin-deficient ob/ob mice, rare human mutations resulting in leptin deficiency have also been identified; leptin-deficient mice and humans display hyperphagia, decreased energy expenditure, and early-onset obesity(Farooqi, et al. 1999; Montague, et al. 1997). Leptin receptor deficient humans and db/db mice display a similar phenotype (Chua, et al. 1996; Tartaglia, et al. 1995). Numerous studies have elaborated the critical role for leptin in the modulation of energy balance: the lack of leptin, as in starvation or genetic leptin deficiency, increases hunger while promoting an energy-sparing program of neuroendocrine and autonomic changes, including decreased sympathetic nervous system tone, thyroid function, growth and reproduction(Ahima, et al. 1997). Leptin treatment largely reverses these changes (Farooqi et al. 1999; Farooqi, et al. 2002). Decreased leptin also promotes a variety of other behavioral and physiologic changes to respond appropriately to low energy stores(Liu, et al. 2010; Liu, et al. 2011; Lu, et al. 2006).
Despite the initial heralding of leptin as a potential cure for human obesity, most obese humans exhibit high circulating leptin concentrations(Maffei et al. 1995). Serum leptin increases in proportion to body fat percentage; obese patients secrete leptin at levels appropriate for their increased adipose mass and display elevated leptin concentrations (“hyperleptinemia”) relative to lean controls(Tobe, et al. 1999). Clearly, however, these high circulating leptin levels do not suffice to restore body adiposity to lean levels, as might be predicted based on the sensitivity of organisms to decreases in leptin signaling. Whether this inability of leptin to suppress feeding in the face of obesity results from an intrinsic or acquired defect in leptin action, or rather simply reflects the inability of homeostatic controls to overcome hedonic feeding drives remains a matter of debate. This controversy serves to underscore the importance of developing a more complete understanding of leptin signaling; its cellular effects; target neural pathways; and integration with other determinants of energy homeostasis.
Leptin and the leptin receptor
Leptin is a 146 amino acid protein produced in white adipose tissue in proportion to triglyceride stores(Frederich, et al. 1995b). Once secreted into the circulation, leptin travels to the brain, where it enters the CNS, presumably via the choroid plexus and circumventricular organs. In the brain, leptin acts by binding and activating the long form of leptin receptor (LepRb), which is expressed primarily on specialized subsets of neurons in certain hypothalamic and brainstem nuclei(Elias, et al. 2000; Patterson, et al. 2011; Scott, et al. 2009; Tartaglia 1997). Mutations that inactivate LepRb, as well as antagonists of LepRb activation, confirm that leptin binding to LepRb is required for its biological activity(Chen, et al. 1996; Shpilman, et al. 2011). While the Lepr gene encodes multiple isoforms (LepRa-f in rats), only LepRb contains the full intracellular domain necessary for the activation of critical second messenger pathways and normal leptin action (Chua et al. 1996; Chua, et al. 1997; Lee, et al. 1996; Tartaglia 1997). Many functions for the other (“short”) forms of the receptor have been hypothesized, including actions as a serum binding protein that functions in leptin stabilization or sequestration (Yang, et al. 2004; Zastrow, et al. 2003; Zhang and Scarpace 2009), or as a leptin transporter(Bjorbaek, et al. 1998b) (Kastin, et al. 1999),but LepRb alone suffices for the control of energy balance, glucose homeostasis, and other leptin effects, and LepRb thus constitutes the focus of this review.
Peripheral actions of leptin
Multiple studies have attempted to assess the role of leptin in the periphery. Mice with ablated hepatic leptin signaling had normal body weight and blood glucose levels, but were protected from high fat diet or age induced insulin intolerance. Mice in which LepRb was deleted from the pancreas using a Pdxcre or RIPcre also demonstrated improvements in glucose tolerance (Huynh, et al. 2010; Morioka, et al. 2007). Interpretation of these results is confounded by hypothalamic cre expression in both the Pdx and RIP models, however (Schwartz, et al. 2010; Wicksteed, et al. 2010). LepRb expression has also been demonstrated in perivascular intestinal cells, although the function of LepRb in these cells has not been determined (Rajala, et al. 2014). Studies examining the role of LepRb in the heart have been difficult to perform based on the negative effects of cre expression on cardiac function (Hall, et al. 2011). One model revealed an additive role for cardiac specific LepRb deletion in inducing cardiac failure, however, suggesting that LepRb may regulate the cardiovascular system through both central and peripheral mechanisms (Hall, et al. 2012).
Central actions of leptin
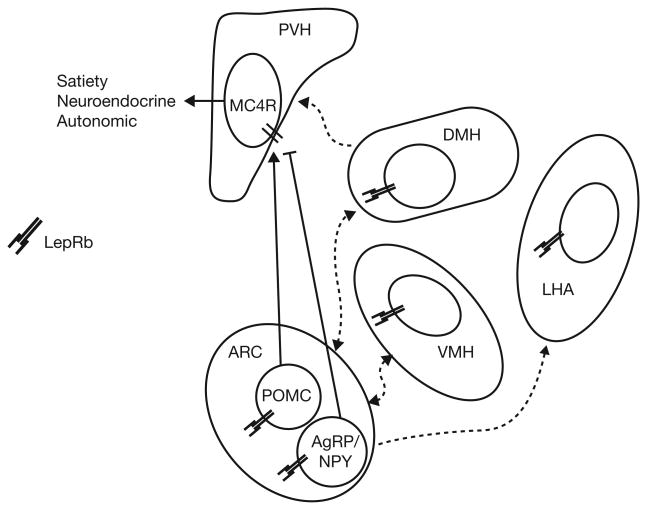
Within the brain, leptin acts on multiple populations of LepRb neurons- primarily in the hypothalamus and brainstem (Patterson et al. 2011; Scott et al. 2009). While leptin action in the nucleus of the solitary tract plays a role in modulating satiety, and ventral tegmental area LepRb contributes to the control of reward and aversion, hypothalamic LepRb appears to mediate the lion's share of leptin action on energy balance(Hayes, et al. 2010; Hommel, et al. 2006; Ring and Zeltser 2010). Within the hypothalamus, leptin acts on multiple populations of LepRb-expressing neurons, including those in the lateral hypothalamic area and the ventromedial, dorsomedial, ventral premammilary, and arcuate (ARC) nuclei (Patterson et al. 2011; Scott et al. 2009). Each of these sites contains multiple distinct types of LepRb cells, each of which contributes uniquely to leptin action. The most studied site of leptin action is the ARC, where leptin inhibits orexigenic agouti-related protein/neuropeptide Y-containing (AgRP/NPY) neurons, and stimulates anorexigenic proopiomelanocortin (POMC)-containing neurons. POMC neurons produce anorexigenic neuropeptides, while AgRP is a potent antagonist of the melanocortin system and NPY mediates additional orexigenic signals (Schwartz et al. 2000).
LepRb signaling
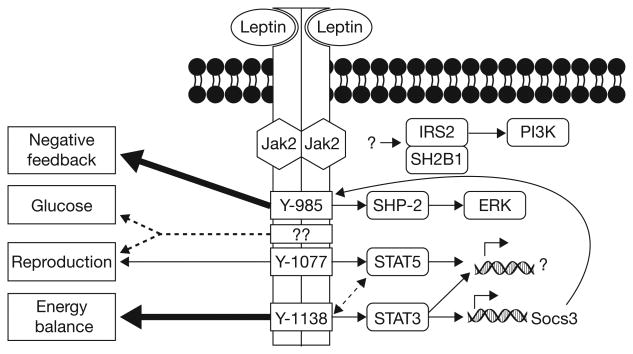
LepRb is an IL6-type class I cytokine receptor consisting of an extracellular leptin binding domain, a single-pass membrane spanning domain, and an intracellular tail that contains binding domains for multiple signaling proteins (Baumann, et al. 1996; Tartaglia et al. 1995). LepRb is present on the cell membrane as a mixture of monomers and dimers (Devos, et al. 1997). Unlike many other cytokine receptors, ligand binding does not appear to activate LepRb by promoting receptor dimerization, but rather promotes a conformational change that results in the autophosphorylation and activation of Janus kinase 2 (JAK2), which is constitutively bound to Box1 and Box2 motifs in the membrane-proximal portion of LepRb (Banks, et al. 2000; Kloek, et al. 2002). Activated JAK2 phosphorylates LepRb on three tyrosine residues in mice: Tyr985, Tyr1077, and Tyr1138 (Banks et al. 2000; Gong, et al. 2007). Each of these phosphorylated tyrosine (pY) residues represents a Src homology 2 (SH2) binding motif that recruits specific SH2-containing effector proteins to the receptor to mediate subsequent signaling.
Leptin binding to LepRb results in the activation of several major signaling pathways. Importantly, phosphorylation of Tyr1138 results in the recruitment of signal tranducer and activator of transcription 3 (STAT3) to LepRb, to permit its phosphorylation (pSTAT3) and activation by JAK2(Banks et al. 2000; White, et al. 1997). Activated pSTAT3 translocates to the nucleus, where it mediates changes in the expression of target genes, including Socs3 (which encodes a feedback inhibitor of LepRb signaling)(Bjorbaek, et al. 1999). Phosphorylation of Tyr985 recruits protein tyrosine phosphatase 2 (SHP2; PTPN1) to LepRb, contributing to the activation of the extracellular signal-regulated kinase (ERK) signaling pathway (Banks et al. 2000; Bjorbaek, et al. 2001). Tyr985 also serves as the binding site for SOCS3, and thus plays a prominent role in the feedback inhibition of LepRb (Bjorbaek, et al. 2000). Phosphorylated Tyr1077 promotes the recruitment and activation of STAT5; Tyr1138 may also contribute to STAT5 activation(Gong et al. 2007).
Another SH2 domain protein, SH2B1, also participates in LepRb signaling. In addition to increasing the amplitude of LepRb signaling via JAK2, SH2B1 may control specific downstream LepRb signals, including insulin receptor substrate (IRS)-proteins (Duan, et al. 2004; Ren, et al. 2005). IRS-proteins also participate in leptin action; they control the phosphatidylinositol 3-kinase (PI3K) pathway, and the subsequent regulation of Akt→FoxO1 and mTORC1 signaling (Kim, et al. 2006; Kitamura, et al. 2006; Niswender, et al. 2001). The mechanism(s) whereby LepRb modulates this pathway remains obscure; some data suggest a potential role for poorly-understood LepRb signaling that occurs independently of LepRb pY sites.
LepRb signaling & physiology
LepRb→STAT3 signaling
Multiple LepRb signaling pathways coordinate the regulation of energy homeostasis. Of these, the Tyr1138→pSTAT3 pathway plays an especially prominent role(Bates and Myers 2003). Mice containing a substitution mutation of LepRb Tyr1138 (which renders LepRb incapable of recruiting and activating STAT3; s/s mice) display hyperphagia and obesity approaching that of db/db animals (although linear growth, fertility, and glucose homeostasis are relatively protected in s/s relative to db/db mice)(Bates, et al. 2004; Bates, et al. 2005; Bates, et al. 2003). Furthermore, brain-specific STAT3 knockout mice (STAT3N-/-) exhibit severe obesity(Gao, et al. 2004). Mice in which STAT3 was deleted specifically in LepRb neurons (LepRbSTAT3-KO) similarly develop hyperphagic obesity with some preservation of glucose homeostasis (Piper, et al. 2007). These studies highlight the importance of LepRb Tyr1138→STAT3 signaling for the regulation of body weight, but suggest some regulation of growth, reproduction, and glucose homeostasis by leptin independently of this pathway.
The role of STAT3 signaling in energy balance in discrete neural populations has been best characterized in the ARC. As might be expected, specific deletion of STAT3 from AgRP neurons results in moderate obesity, increased Npy expression, and decreased sensitivity to leptin (Gong, et al. 2008). STAT3 deletion from POMC neurons also increases adiposity, but the effect is milder than for the AgRP-specific knockout, suggesting a greater role for STAT3 in leptin action in AgRP neurons than in POMC cells(Xu, et al. 2007). In contrast to STAT3 deletion studies, the interpretation of studies in which a mutant, transcriptionally active, form of STAT3 (STAT3-C) is expressed in ARC neurons is more complicated. While STAT3-C expression in AgRP neurons promotes leanness, expression of STAT3-C in POMC neurons results in obesity(Ernst, et al. 2009; Mesaros, et al. 2008). Agrp expression is not altered in AgRPSTAT3-C mice, consistent with the notion that Agrp expression is more sensitive to modulation by PI3K than by STAT3 (see below) (Mesaros et al. 2008). It is possible that the mild obesity resulting from STAT3-C action in POMC neurons results from altered transcriptional activity of this isoform relative to native STAT3, but STAT3-C also promotes Socs3 expression, which could limit endogenous leptin action despite increased transcription mediated by STAT3-C. Interestingly, although the Pomc promoter contains known STAT3 binding sites(Munzberg, et al. 2003) and Pomc expression is decreased in s/s mice and animals with neuronal STAT3 ablation(Bates et al. 2003; Gao et al. 2004), Pomc expression is decreased in POMCSTAT3-C animals (Ernst et al. 2009), suggesting that while Socs3 represents a direct STAT3 target, the control of ARC Pomc expression may reflect the effects of additional and/or downstream LepRb signals, as well. Additionally, none of the phenotypes resulting from the modulation of LepRb→STAT3 signaling in POMC or AgRP neurons approach that of brain or hypothalamus-wide modulation, suggesting that LepRb→STAT3 signaling in other, non-ARC LepRb cells contributes to the control of energy balance during LepRb→STAT3 signaling.
Tyr985-dependent signaling, SOCS3, and SHP2
In contrast to the obese phenotype that results from disruption of LepRb→STAT3 signaling, mice with a mutation in Tyr985 display a lean phenotype (which is especially pronounced in females). These mice also display decreased hypothalamic Agrp expression, increased pSTAT3, exaggerated sensitivity to exogenous leptin, and resistance to DIO (Bjornholm, et al. 2007). These results are consistent with increased LepRb signaling due to decreased LepRb feedback inhibition via disruption of SOCS3 binding. Indeed, as for mice mutant for LepRb Tyr985, disruption of Socs3 in the brain decreases adiposity (more dramatically in female than in male mice) and increases the response to exogenous leptin (Mori, et al. 2004).
In addition to its role in feedback inhibition, Tyr985 may also coordinate energy homeostasis via SHP2/ERK signaling (Bjorbaek et al. 2001; Bjorbaek et al. 2000). As a tyrosine phosphatase, SHP2 was initially investigated as a potential negative regulator of leptin signaling. Deletion of Shp2 from the forebrain disrupts ERK signaling and promotes early onset obesity, however (Zhang, et al. 2004). Furthermore, deletion of Shp2 from POMC neurons results in mild obesity and increased susceptibility to DIO (Banno, et al. 2010). Similarly, female mice expressing a dominant active SHP2 mutant in the brain are resistant to DIO (He, et al. 2012). Thus, these data are consistent with the notion that LepRb→SHP2 signaling is important for leptin action and the control of energy homeostasis, rather than SHP2 mediating feedback inhibition on LepRb. While SHP2 plays an essential role in the control of energy homeostasis, however, the promiscuity of SHP2 (which plays roles in many signaling pathways), renders it difficult to assess the specificity of SHP2 effects for LepRb signaling.
Tyr1077 and STAT5
LepRb→STAT5 signaling appears to have little impact on energy balance. While brain-wide STAT5 knockout mice develop late-onset obesity, this phenotype is quite mild (Lee, et al. 2008). LepRb Tyr1077 mutants develop only mildly increased food intake and adiposity (Patterson, et al. 2012). Furthermore, a recent study deleting STAT5 specifically in LepRb neurons revealed no body weight phenotype; deleting both STAT3 and STAT5 did not produce a more robust phenotype than deleting STAT3 alone (Singireddy, et al. 2013). Also, Tyr1077 mutants enter puberty normally, but have a prolonged inter-estrus interval, suggesting mild subfertility in these animals. LepRSTAT5-KO animals display normal oestrus cycling and fertility, however. Altogether, these studies suggest that Tyr1077 plays a minor role in the control of feeding and reproductive function, but that STAT5 may not be the binding partner that mediates this effect.
Other LepRb signals
Although the tyrosine phosphorylation of LepRb is essential for the majority of leptin's actions, mice in which Tyr985,Tyr1077, and Tyr1138 have all been replaced with phenylalanine (LepRb3F) are less slightly less obese than db/db animals and display significant improvements in glucose homeostasis and fertility relative to db/db mice (Jiang, et al. 2008). In contrast, mice expressing a LepRb truncation mutant (LepRbΔ65) that retains JAK2 signaling and activity but lacks Tyr985,Tyr1077, and Tyr1138 phenocopy db/db animals, and do not appear to be significantly protected from the obesity, diabetes and infertility that are hallmarks of impaired leptin signaling (Robertson, et al. 2010). Thus the improved phenotype seen in LepRb3F mice relative to db/db animals does not result from JAK2 signaling alone, since the LepRbΔ65 model reveals that JAK2 signaling is not sufficient to mediate these improvements. The differing phenotypes between mice expressing LepRb3F and LepRbΔ65 thus suggests the existence of non-canonical signaling pathway which may emanate from a distal site on LepRb, independently of LepRb pY sites. Further work will be required to identify this presumptive pathway.
While SH2B1 and IRS-protein/PI3K signaling contribute to leptin action, the mechanism(s) of their activation by LepRb remain somewhat unclear- no LepRb pY site has been definitively shown to mediate their recruitment. Thus, it is possible that one or both of these pathways constitute the presumptive LepRb pY-independent signaling pathway. Furthermore, these pathways may overlap, since SH2B1 recruits the IRS-protein/PI3K pathway during leptin signaling in cultured cells(Duan et al. 2004) (Kim, et al. 2000). The SH2B1 and IRS-protein/PI3K pathways contribute to energy balance in vivo, however. SH2B1 null mice display severe early-onset obesity and hyperphagia (Ren et al. 2005). Furthermore, neuron-specific restoration of SH2B1 throughout the CNS rescues this phenotype, suggesting that CNS SH2B1 is crucial for the control of body weight (Morris, et al. 2010). Unfortunately, the critical role of SH2B1 in insulin signaling (which is also significantly impacted by this deletion) as well as in signaling by other receptor tyrosine kinases, renders it challenging to determine whether this phenotype results from only from the disruption of LepRb→SH2B1 signaling.
The roles for PI3K signaling in leptin action and the control of energy balance are also complicated. Leptin administration activates IRS-protein/PI3K signaling in the mediobasal hypothalamus, and ICV treatment with PI3K inhibitors inhibits leptin's anorexigenic effects (Niswender et al. 2001), along with the ability of exogenous leptin to suppress Agrp mRNA expression in fasted rats (Morrison, et al. 2005). Furthermore, deletion of IRS2 specifically in LepRb neurons results in obesity, (although it does not impact the ability of LepRb to stimulate pSTAT3)(Sadagurski, et al. 2012). Both in vitro and in vivo studies have also implicated PI3K signaling in the acute actions of leptin. Leptin treatment induces the depolarization of POMC neurons in slice recordings; these effects are abrogated by pretreatment with PI3K inhibitors (Hill, et al. 2008). This effect is also perturbed in mice lacking the PI3K regulatory subunits p85α and p85β in POMC neurons (Hill et al. 2008). While these mice do not display gross phenotypic abnormalities, leptin's ability to promote acute decreases in food intake is also disrupted. Studies in which the PI3K catalytic subunits p110α and p110β were deleted in AgRP or POMC neurons confirm these findings – mice lacking p110β in AgRP neurons are mildly lean, whereas mice lacking p110β in POMC neurons are more sensitive to DIO (Al-Qassab, et al. 2009). It is unclear however, whether these results emanate from disrupted LepRb-PI3K signaling, or from alternations in IR-PI3K signaling, especially in light of data that suggests that leptin and insulin activate non-overlapping populations of POMC neurons (Williams, et al. 2010). Together, these data suggest that leptin induced PI3K signaling has a limited effect on energy balance. However the importance of the LepRb-PI3K pathway for the glucoregulatory or reproductive functions of leptin is yet to be determined.
Negative regulation of leptin signaling
Multiple pathways and proteins inhibit LepRb. Given its role as an inhibitor of LepRb signaling, the mechanisms of action for SOCS3 have been a point of considerable interest. SOCS3 binds to LepRb Tyr985 and mediates negative feedback by directly inhibiting JAK2 activity and/or targeting the receptor-JAK2 complex for proteasomal degradation (Bjorbaek et al. 1999; Bjorbaek, et al. 1998a; Bjorbaek et al. 2000). Neuron-wide deletion of Socs3 using either nestin-cre (Socs3N-/-) or synapsin-cre confers significant resistance to diet-induced obesity (Mori et al. 2004). Socs3N-/- mice also display increased leptin sensitivity as measured by both leptin-induced food intake and STAT3 phosphorylation, as well as by increased PI3K activity. While Socs3 has not been disrupted specifically in LepRb neurons, overexpression of Socs3 in LepRb neurons (LepRbSocs3-OE) yields an unexpected phenotype of slightly increased leanness (Reed, et al. 2010). This may result from a compensatory increase of STAT3 at baseline and a corresponding increase in pSTAT3 levels after leptin treatment, although the mechanism for this is unclear and would seem to be a bit counter-intuitive. Clearly, however, the function of SOCS3 may not be as uniform or straightforward as initially thought.
Because high fat diet induces Socs3 expression in the ARC, ARC populations have been posited to be a major site of leptin resistance. As a result, the role of Socs3 in arcuate POMC and AgRP neurons has been extensively studied. As with Socs3N-/- mice, POMCSocs3-KO mice are resistant to DIO, but display normal body weight on chow diet (Kievit, et al. 2006). Interestingly, POMCSocs3-KO mice also have improved glucose homeostasis on a chow diet, suggesting that POMC neurons may be a critical site of LepRb/SOCS3 signaling in the control of peripheral blood glucose levels. Unlike LepRSocs3-OE mice, mice overexpressing Socs3 in POMC neurons develop mild obesity on a chow diet, and acute leptin resistance (as assessed by leptin induced inhibition of feeding) prior to any divergence in body weight (Reed et al. 2010). These animals also display a POMC neuron-restricted reduction in the pSTAT3 response to leptin, suggesting that potential compensatory mechanisms induced in the LepRbSocs3-OE model were not activated in this more restricted cell population. AgRPSocs3-OE mice also display early onset leptin resistance, and slightly abnormal glucose homeostasis, but no alterations in body weight (Olofsson, et al. 2013). Thus while decreasing Socs3 levels may prove protective against obesity, the modest body weight changes that occur with overexpression of Socs3 suggest that increased Socs3 levels may reflect hyperleptinemia and increased overall leptin signaling, rather than promoting obesity, per se.
Protein tyrosine phosphatases (PTPases) also modulate the amplitude and duration of LepRb signaling. Protein tyrosine phosphatase 1B (PTP1B) has been the most extensively studied of these, but other PTPs such as TCPTP and RPTPe also play critical roles in both leptin and insulin signaling (see review by Tsou & Bence, 2013). PTP1B is a promiscuous phosphatase that attenuates signaling by the receptor for insulin as well as other receptors, in addition to LepRb. In vitro, PTP1B dose-dependently suppresses the leptin-stimulated phosphorylation of Jak2 and pSTAT3 (Zabolotny, et al. 2002). In vivo, whole body PTP1B knockout (PTP1BTKO) results in a lean phenotype, resistance to DIO, and increased sensitivity to exogenous leptin, consistent with the interpretation that PTP1B is a negative regulator of LepRb signaling (Klaman, et al. 2000). Interpretation of the PTP1BTKO model is complicated by the promiscuity of PTP1B and its broad pattern of expression, however, provoking more focused studies of the sites and mechanisms of its action. Pan-neuronal deletion of PTP1B also induces a lean phenotype, whereas liver or muscle specific deletion has no effect, and adipose specific deletion actually causes weight gain (perhaps due to enhanced adipose insulin signaling) (Bence, et al. 2006). LepRb neuron-specific PTP1B deletion (LepRbPTP1B-KO) results in a leaner phenotype than that observed in the PTP1BTKO mice, suggesting that this model may have unmasked an even more important role for PTP1B in LepRb neurons that may have been opposed by other tissue (e.g., adipose) effects in the PTP1BTKO model (Tsou, et al. 2012). The specificity of PTP1B action on LepRb for the development of the lean phenotype is supported by the similar phenotypes of hypothalamic LepRb knockout and LepRb/PTP1B double-knockout mice, suggesting the LepRb-dependence of the lean phenotype of PTP1B null animals (Tsou, et al. 2014). Interestingly, heterozygous LepRbPTP1B+/- mice display as strong a phenotype as LepRbPTP1B-KO, underscoring the importance of appropriate levels of phosphatase action in the control of LepRb signaling (Tsou et al. 2012).
Future Directions: Leptin signaling and gene transcription
Despite the early identification of LepRb→STAT3 signaling as the primary mechanism for leptin's control of energy balance, LepRb→STAT3 target genes remain poorly defined. Currently, the list of genes known to be regulated by leptin in vivo is short: Socs3, Pomc, Cart, Agrp, and Npy. LepRb→STAT3 signaling is required for appropriate Socs3, Pomc, and Agrp gene expression, although (as noted above) Pomc and Agrp may represent indirect targets of STAT3 and/or may be partly controlled by other pathways; PI3K appears to play a role in the control of Agrp and Npy expression. Furthermore, of these five genes, only Socs3 is thought to be induced in multiple LepRb populations; Pomc, Agrp, Npy and Cart expression are restricted to circumscribed populations, and do not contribute to leptin action in the majority of LepRb neurons. This dearth of information about LepRb→STAT3 target genes can largely be attributed to the challenge of specifically isolating LepRb neurons from the hypothalamic milieu; LepRb neurons comprise approximately <5% of all hypothalamic neurons, making it challenging to identify cell-autonomous changes in gene transcription for any subset of neurons. Clearly more work will be necessary to identify the hypothalamic gene targets of LepRb and STAT3 signaling. These transcripts will be responsible for much of leptin action, and may represent potential targets for therapy, in addition to shedding light on the mechanisms of leptin action.
Figure 1. Leptin signaling and biological function.
Leptin binds to LepRb, activating the associated JAK2 tyrosine kinase. Activated JAK2 phosphorylates the intracellular tail of LepRb on 3 tyrosine residues. Phosphorylated Tyr985 recruits SHP2, which participates in ERK signaling; Tyr985 also serves as a binding site for the negative feedback regulator, SOCS3. Phosphorylated Tyr1077 partially mediates leptin's control of reproduction; while STAT5 binds this site, STAT5 does not appear to participate in this effect of leptin. Phosphorylated Tyr1138 engages the STAT3 transcription factor. LepRb→STAT3 signaling represents the primary mechanism by which leptin regulates energy balance, although the target genes of STAT3 in LepRb neurons remain undiscovered. Leptin also recruits the IRS2→PI3K and SH2B1 pathways, although the mechanism of their recruitment to LepRb remains unclear. Some glucoregulatory and reproductive actions of LepRb appear to be mediated by unknown signals that function independently of LepRb tyrosine phosphorylation sites.
Figure 2. Hypothalamic leptin action.
Leptin acts on its receptor (LepRb) on neurons in a series of interconnected hypothalamic nuclei to regulate satiety, neuroendocrine function, and autonomic tone. In the arcuate nucleus, leptin controls the melanocortin system through its opposing actions on POMC and AgRP neurons. ARC, arcuate nucleus; VMH, ventromedial hypothalamic nucleus; DMH, dorsomedial hypothalamic nucleus; LHA, lateral hypothalamic area; PVH, paraventricular hypothalamic nucleus; MC4R, melanocortin 4 receptor; POMC, pro-opiomelanocortin; AgRP, agouti-related peptide.
Acknowledgments
Supported by the Michigan Diabetes Research Center (NIH Grant P30 DK020572) the NIH (DK056731, DK78056, DK098853), the American Diabetes Association, and the Marilyn H. Vincent Foundation to MGM, NIH DK097861 to MBA.
References
- Ahima RS, Dushay J, Flier SN, Prabakaran D, Flier JS. Leptin accelerates the onset of puberty in normal female mice. J Clin Invest. 1997;99:391–395. doi: 10.1172/JCI119172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Qassab H, Smith MA, Irvine EE, Guillermet-Guibert J, Claret M, Choudhury AI, Selman C, Piipari K, Clements M, Lingard S, et al. Dominant role of the p110beta isoform of PI3K over p110alpha in energy homeostasis regulation by POMC and AgRP neurons. Cell Metab. 2009;10:343–354. doi: 10.1016/j.cmet.2009.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banks AS, Davis SM, Bates SH, Myers MG., Jr Activation of downstream signals by the long form of the leptin receptor. J Biol Chem. 2000;275:14563–14572. doi: 10.1074/jbc.275.19.14563. [DOI] [PubMed] [Google Scholar]
- Banno R, Zimmer D, De Jonghe BC, Atienza M, Rak K, Yang W, Bence KK. PTP1B and SHP2 in POMC neurons reciprocally regulate energy balance in mice. J Clin Invest. 2010;120:720–734. doi: 10.1172/JCI39620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates SH, Dundon TA, Seifert m, Carlson M, Maratos-Flier E, Myers MG., Jr LRb-STAT3 signaling is required for the neuroendocrine regulation of energy expenditure by leptin. Diabetes. 2004;53:3067–3073. doi: 10.2337/diabetes.53.12.3067. [DOI] [PubMed] [Google Scholar]
- Bates SH, Kulkarni RN, Seifert m, Myers MG., Jr Roles for leptin receptor/STAT3-dependent and -independent signals in the regulation of glucose homeostasis. Cell Metabolism. 2005;1:169–178. doi: 10.1016/j.cmet.2005.02.001. [DOI] [PubMed] [Google Scholar]
- Bates SH, Myers MG., Jr The role of leptin receptor signaling in feeding and neuroendocrine function. Trends Endocrinol Metab. 2003;14:447–452. doi: 10.1016/j.tem.2003.10.003. [DOI] [PubMed] [Google Scholar]
- Bates SH, Stearns WH, Schubert M, Tso AWK, Wang Y, Banks AS, Dundon TA, Lavery HJ, Haq AK, Maratos-Flier E, et al. STAT3 signaling is required for leptin regulation of energy balance but not reproduction. Nature. 2003;421:856–859. doi: 10.1038/nature01388. [DOI] [PubMed] [Google Scholar]
- Baumann H, Morella KK, White DW, Dembski M, Bailon PS, Kim H, Lai CF, Tartaglia LA. The full-length leptin receptor has signaling capabilities of interleukin 6-type cytokine receptors. Proc Natl Acad Sci USA. 1996;93:8374–8378. doi: 10.1073/pnas.93.16.8374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bence KK, Delibegovic M, Xue B, Gorgun CZ, Hotamisligil GS, Neel BG, Kahn BB. Neuronal PTP1B regulates body weight, adiposity and leptin action. Nat Med. 2006;12:917–924. doi: 10.1038/nm1435. [DOI] [PubMed] [Google Scholar]
- Bjorbaek C, Buchholz RM, Davis SM, Bates SH, Pierroz DD, Gu H, Neel BG, Myers MG, Jr, Flier JS. Divergent roles of SHP-2 in ERK activation by leptin receptors. J Biol Chem. 2001;276:4747–4755. doi: 10.1074/jbc.M007439200. [DOI] [PubMed] [Google Scholar]
- Bjorbaek C, El Haschimi K, Frantz JD, Flier JS. The role of SOCS-3 in leptin signaling and leptin resistance. J Biol Chem. 1999;274:30059–30065. doi: 10.1074/jbc.274.42.30059. [DOI] [PubMed] [Google Scholar]
- Bjorbaek C, Elmquist JK, Frantz JD, Shoelson SE, Flier JS. Identification of SOCS-3 as a potential mediator of central leptin resistance. Molecular Cell. 1998a;1:619–625. doi: 10.1016/s1097-2765(00)80062-3. [DOI] [PubMed] [Google Scholar]
- Bjorbaek C, Elmquist JK, Michl P, Ahima RS, van Bueren A, McCall AL, Flier JS. Expression of leptin receptor isoforms in rat brain microvessels. Endocrinology. 1998b;139:3485–3491. doi: 10.1210/endo.139.8.6154. [DOI] [PubMed] [Google Scholar]
- Bjorbaek C, Lavery HJ, Bates SH, Olson RK, Davis SM, Flier JS, Myers MG., Jr SOCS3 mediates feedback inhibition of the leptin receptor via Tyr985. J Biol Chem. 2000;275:40649–40657. doi: 10.1074/jbc.M007577200. [DOI] [PubMed] [Google Scholar]
- Bjornholm M, Munzberg H, Leshan RL, Villanueva EC, Bates SH, Louis GW, Jones JC, Ishida-Takahashi R, Bjorbaek C, Myers MG., Jr Mice lacking inhibitory leptin receptor signals are lean with normal endocrine function. J Clin Invest. 2007;117:1354–1360. doi: 10.1172/JCI30688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H, Charlat O, Tartaglia LA, Woolf EA, Weng X, Ellis SJ, Lakey ND, Culpepper J, Moore KJ, Breitbart RE, et al. Evidence that the diabetes gene encodes the leptin receptor: identification of a mutation in the leptin receptor gene in db/db mice. Cell. 1996;84:491–495. doi: 10.1016/s0092-8674(00)81294-5. [DOI] [PubMed] [Google Scholar]
- Chua SC, Jr, Chung WK, Wu-Peng XS, Zhang Y, Liu SM, Tartaglia L, Leibel RL. Phenotypes of mouse diabetes and rat fatty due to mutations in the OB (leptin) receptor. Science. 1996;271:994–996. doi: 10.1126/science.271.5251.994. [DOI] [PubMed] [Google Scholar]
- Chua SC, Jr, Koutras IK, Han L, Liu SM, Kay J, Young SJ, Chung WK, Leibel RL. Fine structure of the murine leptin receptor gene: Splice site suppression is required to form two alternatively spliced transcripts. Genomics. 1997;45:264–270. doi: 10.1006/geno.1997.4962. [DOI] [PubMed] [Google Scholar]
- Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, Lin JK, Farzadfar F, Khang YH, Stevens GA, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378:31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- Devos R, Guisez Y, Van der Heyden J, White DW, Kalai M, Fountoulakis M, Plaetinck G. Ligand-independent dimerization of the extracellular domain of the leptin receptor and determination of the stoichiometry of leptin binding. Journal of Biological Chemistry. 1997;272:18304–18310. doi: 10.1074/jbc.272.29.18304. [DOI] [PubMed] [Google Scholar]
- Duan C, Li M, Rui L. SH2-B promotes insulin receptor substrate 1 (IRS1)- and IRS2-mediated activation of the phosphatidylinositol 3-kinase pathway in response to leptin. J Biol Chem. 2004;279:43684–43691. doi: 10.1074/jbc.M408495200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elias CF, Kelly JF, Lee CE, Ahima RS, Drucker DJ, Saper CB, Elmquist JK. Chemical characterization of leptin-activated neurons in the rat brain. J Comp Neurol. 2000;423:261–281. [PubMed] [Google Scholar]
- Elmquist JK, Coppari R, Balthasar N, Ichinose M, Lowell BB. Identifying hypothalamic pathways controlling food intake, body weight, and glucose homeostasis. J Comp Neurol. 2005;493:63–71. doi: 10.1002/cne.20786. [DOI] [PubMed] [Google Scholar]
- Ernst MB, Wunderlich CM, Hess S, Paehler M, Mesaros A, Koralov SB, Kleinridders A, Husch A, Munzberg H, Hampel B, et al. Enhanced Stat3 activation in POMC neurons provokes negative feedback inhibition of leptin and insulin signaling in obesity. J Neurosci. 2009;29:11582–11593. doi: 10.1523/JNEUROSCI.5712-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farooqi IS, Jebb SA, Langmack G, Lawrence E, Cheetham CH, Prentice AM, Hughes IA, McCamish MA, O'Rahilly S. Effects of recombinant leptin therapy in a child with congenital leptin deficiency. N Engl J Med. 1999;341:879–884. doi: 10.1056/NEJM199909163411204. [DOI] [PubMed] [Google Scholar]
- Farooqi IS, Matarese G, Lord GM, Keogh JM, Lawrence E, Agwu C, Sanna V, Jebb SA, Perna F, Fontana S, et al. Beneficial effects of leptin on obesity, T cell hyporesponsiveness, and neuroendocrine/metabolic dysfunction of human congenital leptin deficiency. J Clin Invest. 2002;110:1093–1103. doi: 10.1172/JCI15693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frederich RC, Hamann A, Anderson S, Lollmann B, Lowell BB, Flier JS. Leptin levels reflect body lipid content in mice: evidence for diet-induced resistance to leptin action. Nat Med. 1995a;1:1311–1314. doi: 10.1038/nm1295-1311. [DOI] [PubMed] [Google Scholar]
- Frederich RC, Lollmann B, Hamann A, Napolitano-Rosen A, Kahn BB, Lowell BB, Flier JS. Expression of ob mRNA and its encoded protein in rodents: Impact of nutrition and obesity. J Clin Invest. 1995b;96:1658–1663. doi: 10.1172/JCI118206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman JM, Halaas JL. Leptin and the regulation of body weight in mammals. Nature. 1998;395:763–770. doi: 10.1038/27376. [DOI] [PubMed] [Google Scholar]
- Gao Q, Wolfgang MJ, Neschen S, Morino K, Horvath TL, Shulman GI, Fu XY. Disruption of neural signal transducer and activator of transcription 3 causes obesity, diabetes, infertility, and thermal dysregulation. Proc Natl Acad Sci USA. 2004;101:4661–4666. doi: 10.1073/pnas.0303992101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong L, Yao F, Hockman K, Heng HH, Morton GJ, Takeda K, Akira S, Low MJ, Rubinstein M, MacKenzie RG. Signal transducer and activator of transcription-3 is required in hypothalamic agouti-related protein/neuropeptide Y neurons for normal energy homeostasis. Endocrinology. 2008;149:3346–3354. doi: 10.1210/en.2007-0945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong Y, Ishida-Takahashi R, Villanueva EC, Fingar DC, Munzberg H, Myers MG., Jr The long form of the leptin receptor regulates STAT5 and ribosomal protein S6 via alternate mechanisms. J Biol Chem. 2007;282:31019–31027. doi: 10.1074/jbc.M702838200. [DOI] [PubMed] [Google Scholar]
- Hall ME, Smith G, Hall JE, Stec DE. Systolic dysfunction in cardiac-specific ligand-inducible MerCreMer transgenic mice. Am J Physiol Heart Circ Physiol. 2011;301:H253–260. doi: 10.1152/ajpheart.00786.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall ME, Smith G, Hall JE, Stec DE. Cardiomyocyte-specific deletion of leptin receptors causes lethal heart failure in Cre-recombinase-mediated cardiotoxicity. Am J Physiol Regul Integr Comp Physiol. 2012;303:R1241–1250. doi: 10.1152/ajpregu.00292.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes MR, Skibicka KP, Leichner TM, Guarnieri DJ, DiLeone RJ, Bence KK, Grill HJ. Endogenous leptin signaling in the caudal nucleus tractus solitarius and area postrema is required for energy balance regulation. Cell Metab. 2010;11:77–83. doi: 10.1016/j.cmet.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He Z, Zhang SS, Meng Q, Li S, Zhu HH, Raquil MA, Alderson N, Zhang H, Wu J, Rui L, et al. Shp2 controls female body weight and energy balance by integrating leptin and estrogen signals. Mol Cell Biol. 2012;32:1867–1878. doi: 10.1128/MCB.06712-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill JW, Williams KW, Ye C, Luo J, Balthasar N, Coppari R, Cowley MA, Cantley LC, Lowell BB, Elmquist JK. Acute effects of leptin require PI3K signaling in hypothalamic proopiomelanocortin neurons in mice. J Clin Invest. 2008;118:1796–1805. doi: 10.1172/JCI32964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hommel JD, Trinko R, Sears RM, Georgescu D, Liu ZW, Gao XB, Thurmon JJ, Marinelli M, DiLeone RJ. Leptin receptor signaling in midbrain dopamine neurons regulates feeding. Neuron. 2006;51:801–810. doi: 10.1016/j.neuron.2006.08.023. [DOI] [PubMed] [Google Scholar]
- Huynh FK, Levi J, Denroche HC, Gray SL, Voshol PJ, Neumann UH, Speck M, Chua SC, Covey SD, Kieffer TJ. Disruption of hepatic leptin signaling protects mice from age- and diet-related glucose intolerance. Diabetes. 2010;59:3032–3040. doi: 10.2337/db10-0074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang L, You J, Yu X, Gonzalez L, Yu Y, Wang Q, Yang G, Li W, Li C, Liu Y. Tyrosine-dependent and - independent actions of leptin receptor in control of energy balance and glucose homeostasis. Proc Natl Acad Sci USA. 2008;105:18619–18624. doi: 10.1073/pnas.0804589105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kastin AJ, Pan W, Maness LM, Koletsky RJ, Ernsberger P. Decreased transport of leptin across the blood-brain barrier in rats lacking the short form of the leptin receptor. Peptides. 1999;20:1449–1453. doi: 10.1016/s0196-9781(99)00156-4. [DOI] [PubMed] [Google Scholar]
- Kievit P, Howard JK, Badman MK, Balthasar N, Coppari R, Mori H, Lee CE, Elmquist JK, Yoshimura A, Flier JS. Enhanced leptin sensitivity and improved glucose homeostasis in mice lacking suppressor of cytokine signaling-3 in POMC-expressing cells. Cell Metab. 2006;4:123–132. doi: 10.1016/j.cmet.2006.06.010. [DOI] [PubMed] [Google Scholar]
- Kim MS, Pak YK, Jang PG, Namkoong C, Choi YS, Won JC, Kim KS, Kim SW, Kim HS, Park JY, et al. Role of hypothalamic Foxo1 in the regulation of food intake and energy homeostasis. Nat Neurosci. 2006;9:901–906. doi: 10.1038/nn1731. [DOI] [PubMed] [Google Scholar]
- Kim YB, Uotani S, Pierroz DD, Flier JS, Kahn BB. In vivo administration of leptin activates signal transduction directly in insulin-sensitive tissues: overlapping but distinct pathways from insulin. Endocrinology. 2000;141:2328–2339. doi: 10.1210/endo.141.7.7536. [DOI] [PubMed] [Google Scholar]
- Kitamura T, Feng Y, Ido KY, Chua SC, Xu AW, Barsh GS, Rossetti L, Accili D. Forkhead protein FoxO1 mediates Agrp-dependent effects of leptin on food intake. Nat Med. 2006;12:534–540. doi: 10.1038/nm1392. [DOI] [PubMed] [Google Scholar]
- Klaman LD, Boss O, Peroni OD, Kim JK, Martino JL, Zabolotny JM, Moghal N, Lubkin M, Kim YB, Sharpe AH, et al. Increased energy expenditure, decreased adiposity, and tissue-specific insulin sensitivity in protein-tyrosine phosphatase 1B-deficient mice. Mol Cell Biol. 2000;20:5479–5489. doi: 10.1128/mcb.20.15.5479-5489.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kloek C, Haq AK, Dunn SL, Lavery HJ, Banks AS, Myers MG., Jr Regulation of Jak kinases by intracellular leptin receptor sequences. J Biol Chem. 2002;277:41547–41555. doi: 10.1074/jbc.M205148200. [DOI] [PubMed] [Google Scholar]
- Lee GH, Proenca R, Montez JM, Carroll KM, Darvishzadeh JG, Lee JI, Friedman JM. Abnormal splicing of the leptin receptor in diabetic mice. Nature. 1996;379:632–635. doi: 10.1038/379632a0. [DOI] [PubMed] [Google Scholar]
- Lee JY, Muenzberg H, Gavrilova O, Reed JA, Berryman D, Villanueva EC, Louis GW, Leinninger GM, Bertuzzi S, Seeley RJ, et al. Loss of Cytokine-STAT5 Signaling in the CNS and Pituitary Gland Alters Energy Balance and Leads to Obesity. PLoS ONE. 2008;3:e1639. doi: 10.1371/journal.pone.0001639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J, Garza JC, Bronner J, Kim CS, Zhang W, Lu XY. Acute administration of leptin produces anxiolytic-like effects: a comparison with fluoxetine. Psychopharmacology (Berl) 2010;207:535–545. doi: 10.1007/s00213-009-1684-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J, Perez SM, Zhang W, Lodge DJ, Lu XY. Selective deletion of the leptin receptor in dopamine neurons produces anxiogenic-like behavior and increases dopaminergic activity in amygdala. Mol Psychiatry. 2011 doi: 10.1038/mp.2011.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu XY, Kim CS, Frazer A, Zhang W. Leptin: a potential novel antidepressant. Proc Natl Acad Sci USA. 2006;103:1593–1598. doi: 10.1073/pnas.0508901103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maffei M, Halaas J, Ravussin E, Pratley RE, Lee GH, Zhang Y, Fei H, Kim S, Lallone R, Ranganathan S, et al. Leptin levels in human and rodent: Measurement of plasma leptin and ob RNA in obese and weight-reduced subjects. Nature Medicine. 1995;1:1155–1161. doi: 10.1038/nm1195-1155. [DOI] [PubMed] [Google Scholar]
- Mesaros A, Koralov SB, Rother E, Wunderlich FT, Ernst MB, Barsh GS, Rajewsky K, Bruning JC. Activation of Stat3 signaling in AgRP neurons promotes locomotor activity. Cell Metab. 2008;7:236–248. doi: 10.1016/j.cmet.2008.01.007. [DOI] [PubMed] [Google Scholar]
- Montague CT, Farooqi IS, Whitehead JP, Soos MS, Rau H, Wareham NJ, Sewter CP, Digby JE, Mohammed SN, Hurst JA, et al. Congenital leptin deficiency is associated with severe early onset obesity in humans. Nature. 1997;387:903–908. doi: 10.1038/43185. [DOI] [PubMed] [Google Scholar]
- Mori H, Hanada R, Hanada T, Aki D, Mashima R, Nishinakamura H, Torisu T, Chien KR, Yasukawa H, Yoshimura A. Socs3 deficiency in the brain elevates leptin sensitivity and confers resistance to diet-induced obesity. Nat Med. 2004 doi: 10.1038/nm1071. [DOI] [PubMed] [Google Scholar]
- Morioka T, Asilmaz E, Hu J, Dishinger JF, Kurpad AJ, Elias CF, Li H, Elmquist JK, Kennedy RT, Kulkarni RN. Disruption of leptin receptor expression in the pancreas directly affects beta cell growth and function in mice. J Clin Invest. 2007;117:2860–2868. doi: 10.1172/JCI30910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris DL, Cho KW, Rui L. Critical role of the Src homology 2 (SH2) domain of neuronal SH2B1 in the regulation of body weight and glucose homeostasis in mice. Endocrinology. 2010;151:3643–3651. doi: 10.1210/en.2010-0254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison CD, Morton GJ, Niswender KD, Gelling RW, Schwartz MW. Leptin inhibits hypothalamic Npy and Agrp gene expression via a mechanism that requires phosphatidylinositol 3-OH-kinase signaling. Am J Physiol Endocrinol Metab. 2005;289:E1051–E1057. doi: 10.1152/ajpendo.00094.2005. [DOI] [PubMed] [Google Scholar]
- Munzberg H, Huo L, Nillni EA, Hollenberg AN, Bjorbaek C. Role of signal transducer and activator of transcription 3 in regulation of hypothalamic proopiomelanocortin gene expression by leptin. Endocrinology. 2003;144:2121–2131. doi: 10.1210/en.2002-221037. [DOI] [PubMed] [Google Scholar]
- Myers MG, Jr, Munzberg H, Leinninger GM, Leshan RL. The geometry of leptin action in the brain: more complicated than a simple ARC. Cell Metab. 2009;9:117–123. doi: 10.1016/j.cmet.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niswender KD, Morton GJ, Stearns WH, Rhodes CJ, Myers MG, Jr, Schwartz MW. Intracellular signallingKey enzyme in leptin-induced anorexia. Nature. 2001;413:794–795. doi: 10.1038/35101657. [DOI] [PubMed] [Google Scholar]
- Olofsson LE, Unger EK, Cheung CC, Xu AW. Modulation of AgRP-neuronal function by SOCS3 as an initiating event in diet-induced hypothalamic leptin resistance. Proc Natl Acad Sci U S A. 2013;110:E697–706. doi: 10.1073/pnas.1218284110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson CM, Leshan RL, Jones JC, Myers MG., Jr Molecular mapping of mouse brain regions innervated by leptin receptor-expressing cells. Brain Res. 2011 doi: 10.1016/j.brainres.2011.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson CM, Villanueva EC, Greenwald-Yarnell M, Rajala M, Gonzalez IE, Saini N, Jones J, Myers MG., Jr Leptin action via LepR-b Tyr1077 contributes to the control of energy balance and female reproduction. Mol Metab. 2012;1:61–69. doi: 10.1016/j.molmet.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper ML, Unger EK, Myers MG, Jr, Xu AW. Specific physiological roles for Stat3 in leptin receptor-expressing neurons. Mol Endocrinol. 2007 doi: 10.1210/me.2007-0389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajala MW, Patterson CM, Opp JS, Foltin SK, Young VB, Myers MG., Jr Leptin acts independently of food intake to modulate gut microbial composition in male mice. Endocrinology. 2014;155:748–757. doi: 10.1210/en.2013-1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed AS, Unger EK, Olofsson LE, Piper ML, Myers MG, Jr, Xu AW. Functional role of suppressor of cytokine signaling 3 upregulation in hypothalamic leptin resistance and long-term energy homeostasis. Diabetes. 2010;59:894–906. doi: 10.2337/db09-1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren D, Li M, Duan C, Rui L. Identification of SH2-B as a key regulator of leptin sensitivity, energy balance, and body weight in mice. Cell Metab. 2005;2:95–104. doi: 10.1016/j.cmet.2005.07.004. [DOI] [PubMed] [Google Scholar]
- Ring LE, Zeltser LM. Disruption of hypothalamic leptin signaling in mice leads to early-onset obesity, but physiological adaptations in mature animals stabilize adiposity levels. J Clin Invest. 2010;120:2931–2941. doi: 10.1172/JCI41985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson S, Ishida-Takahashi R, Tawara I, Hu J, Patterson CM, Jones JC, Kulkarni RN, Myers MG., Jr Insufficiency of Janus kinase 2-autonomous leptin receptor signals for most physiologic leptin actions. Diabetes. 2010;59:782–790. doi: 10.2337/db09-1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadagurski M, Leshan RL, Patterson C, Rozzo A, Kuznetsova A, Skorupski J, Jones JC, Depinho RA, Myers MG, Jr, White MF. IRS2 Signaling in LepR-b Neurons Suppresses FoxO1 to Control Energy Balance Independently of Leptin Action. Cell Metab. 2012;15:703–712. doi: 10.1016/j.cmet.2012.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz MW, Guyenet SJ, Cirulli V. The hypothalamus and ss-cell connection in the gene-targeting era. Diabetes. 2010;59:2991–2993. doi: 10.2337/db10-1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz MW, Woods SC, Porte D, Jr, Seeley RJ, Baskin DG. Central nervous system control of food intake. Nature. 2000;404:661–671. doi: 10.1038/35007534. [DOI] [PubMed] [Google Scholar]
- Scott MM, Lachey JL, Sternson SM, Lee CE, Elias CF, Friedman JM, Elmquist JK. Leptin targets in the mouse brain. J Comp Neurol. 2009;514:518–532. doi: 10.1002/cne.22025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shpilman M, Niv-Spector L, Katz M, Varol C, Solomon G, Ayalon-Soffer M, Boder E, Halpern Z, Elinav E, Gertler A. Development and characterization of high affinity leptins and leptin antagonists. J Biol Chem. 2011;286:4429–4442. doi: 10.1074/jbc.M110.196402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singireddy AV, Inglis MA, Zuure WA, Kim JS, Anderson GM. Neither signal transducer and activator of transcription 3 (STAT3) or STAT5 signaling pathways are required for leptin's effects on fertility in mice. Endocrinology. 2013;154:2434–2445. doi: 10.1210/en.2013-1109. [DOI] [PubMed] [Google Scholar]
- Tartaglia LA. The leptin receptor. Journal of Biological Chemistry. 1997;272:6093–6096. doi: 10.1074/jbc.272.10.6093. [DOI] [PubMed] [Google Scholar]
- Tartaglia LA, Dembski M, Weng X, Deng N, Culpepper J, Devos R, Richards GJ, Campfield LA, Clark FT, Deeds J, et al. Identification and expression cloning of a leptin receptor, OB-R. Cell. 1995;83:1263–1271. doi: 10.1016/0092-8674(95)90151-5. [DOI] [PubMed] [Google Scholar]
- Tobe K, Ogura T, Tsukamoto C, Imai A, Matsuura K, Iwasaki Y, Shimomura H, Higashi T, Tsuji T. Relationship between serum leptin and fatty liver in Japanese male adolescent university students. Am J Gastroenterol. 1999;94:3328–3335. doi: 10.1111/j.1572-0241.1999.01549.x. [DOI] [PubMed] [Google Scholar]
- Tsou RC, Rak KS, Zimmer DJ, Bence KK. Improved metabolic phenotype of hypothalamic PTP1B-deficiency is dependent upon the leptin receptor. Mol Metab. 2014;3:301–312. doi: 10.1016/j.molmet.2014.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsou RC, Zimmer DJ, De Jonghe BC, Bence KK. Deficiency of PTP1B in leptin receptor-expressing neurons leads to decreased body weight and adiposity in mice. Endocrinology. 2012;153:4227–4237. doi: 10.1210/en.2012-1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White DW, Kuropatwinski KK, Devos R, Baumann H, Tartaglia LA. Leptin receptor (OB-R) signaling. Cytoplasmic domain mutational analysis and evidence for receptor homo-oligomerization. J Biol Chem. 1997;272:4065–4071. doi: 10.1074/jbc.272.7.4065. [DOI] [PubMed] [Google Scholar]
- Wicksteed B, Brissova M, Yan W, Opland DM, Plank JL, Reinert RB, Dickson LM, Tamarina NA, Philipson LH, Shostak A, et al. Conditional gene targeting in mouse pancreatic ss-Cells: analysis of ectopic Cre transgene expression in the brain. Diabetes. 2010;59:3090–3098. doi: 10.2337/db10-0624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams KW, Margatho LO, Lee CE, Choi M, Lee S, Scott MM, Elias CF, Elmquist JK. Segregation of acute leptin and insulin effects in distinct populations of arcuate proopiomelanocortin neurons. J Neurosci. 2010;30:2472–2479. doi: 10.1523/JNEUROSCI.3118-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu AW, Ste-Marie L, Kaelin CB, Barsh GS. Inactivation of signal transducer and activator of transcription 3 in proopiomelanocortin (Pomc) neurons causes decreased pomc expression, mild obesity, and defects in compensatory refeeding. Endocrinology. 2007;148:72–80. doi: 10.1210/en.2006-1119. [DOI] [PubMed] [Google Scholar]
- Yang G, Ge H, Boucher A, Yu X, Li C. Modulation of direct leptin signaling by soluble leptin receptor. Mol Endocrinol. 2004;18:1354–1362. doi: 10.1210/me.2004-0027. [DOI] [PubMed] [Google Scholar]
- Zabolotny JM, Bence-Hanulec KK, Stricker-Krongrad A, Haj F, Wang Y, Minokoshi Y, Kim YB, Elmquist JK, Tartaglia LA, Kahn BB, et al. PTP1B regulates leptin signal transduction in vivo. Dev Cell. 2002;2:489–495. doi: 10.1016/s1534-5807(02)00148-x. [DOI] [PubMed] [Google Scholar]
- Zastrow O, Seidel B, Kiess W, Thiery J, Keller E, Bottner A, Kratzsch J. The soluble leptin receptor is crucial for leptin action: evidence from clinical and experimental data. Int J Obes Relat Metab Disord. 2003;27:1472–1478. doi: 10.1038/sj.ijo.0802432. [DOI] [PubMed] [Google Scholar]
- Zhang EE, Chapeau E, Hagihara K, Feng GS. Neuronal Shp2 tyrosine phosphatase controls energy balance and metabolism. Proc Natl Acad Sci U S A. 2004;101:16064–16069. doi: 10.1073/pnas.0405041101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Scarpace PJ. The soluble leptin receptor neutralizes leptin-mediated STAT3 signalling and anorexic responses in vivo. Br J Pharmacol. 2009;158:475–482. doi: 10.1111/j.1476-5381.2009.00246.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994;372:425–432. doi: 10.1038/372425a0. [DOI] [PubMed] [Google Scholar]