Abstract
We experienced a case of vestibular schwannoma and metachronous schwannoma in the colon. A 59-year-old female presented with a 1-month history of hematochezia. She had undergone suboccipital craniectomy resulting in radical subtotal resection, followed by gamma knife radiosurgery for a large left vestibular schwannoma 4 years prior to admission. On preoperative colonoscopy, a huge mass through which the colonoscope could not be passed was detected. CT scans showed colo-colonic intussusception with a 4.8-cm-sized mass in the descending colon. PET/CT revealed hypermetabolism of the descending colon tumor and pericolic lymph nodes. We performed left hemicolectomy under the preoperative impression of colon cancer with intussusception. A pathological diagnosis of benign schwannoma of the colon was made in this patient.
Keywords: Colon neurilemmoma, Schwannoma, Craniectomy, Gamma knife radiosurgery
INTRODUCTION
Schwannoma is a benign tumor arising from Schwann cells that form the neural sheath [1,2,3,4,5,6,7]. Even though intracranial schwannoma is relatively common, primary schwannoma of the colon is rare [1,2,3,4,6] and a few cases of colonic schwannoma have been reported [2,3,4,5,6]. Herein, we report a case of vestibular schwannoma and metachronous schwannoma of the colon. To the best of our knowledge, this is the first case of schwannomas in the brain and colon.
CASE REPORT
A 59-year-old female patient was admitted with a 1-month history of hematochezia. She did not have any other gastrointestinal symptoms, such as change in bowel habit, constipation, weight loss etc. On physical examination, the abdomen was soft and flat, and bowel sounds were normo-active. There was no palpable mass or tenderness. On digital rectal examination, there were no abnormal findings. She had no history of smoking or drinking alcohol, and no past history of any medical disease, such as hypertension, diabetes mellitus, pulmonary tuberculosis, or hepatitis.
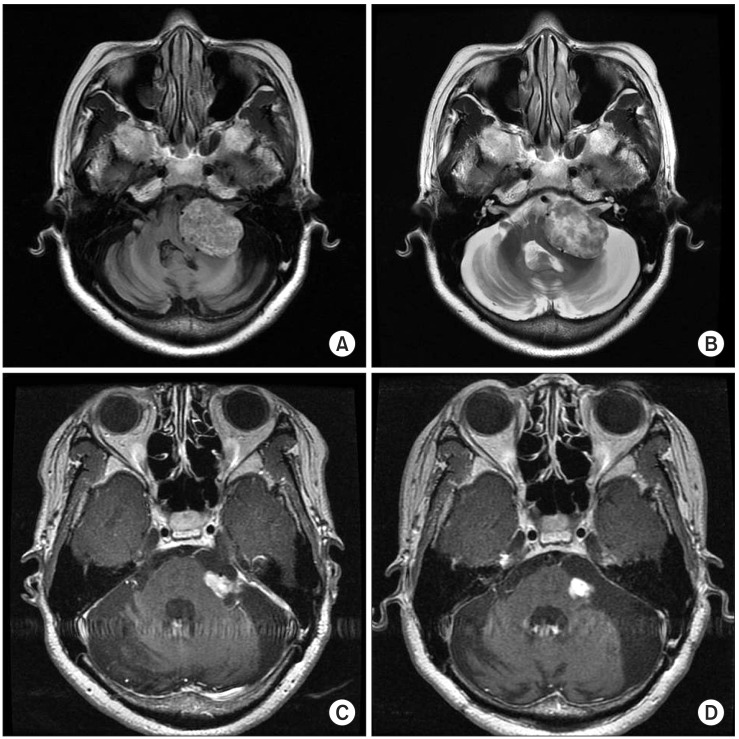
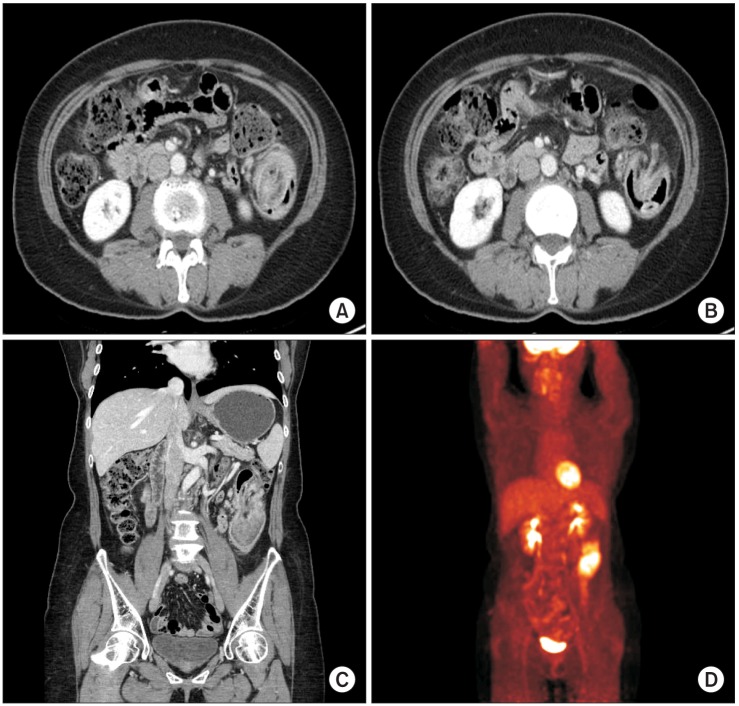
The past surgical history revealed that she had severe headache and dizziness for several years. There were progressive cranial neuropathies on the left side including hearing difficulty, tinnitus, and gait disturbance. A MRI study showed a 3.9-cm-sized, left cerebellopontine angle (CPA) tumor, which was extending into the internal auditory meatus and compressing the brain stem (Fig. 1). Lateral suboccipital craniotomy and radical subtotal tumor removal were performed by an experienced neurosurgeon. Histopathologic examination of the CPA tumor specimen showed schwannoma. On special and immune staining, the tumor cells were negative for glial fibrillary acidic protein and diffusely positive for S-100 (Fig. 2). Meningitis with CSF rhinorrhea and House-Brackmann (HB) grade IV left facial palsy developed in the postoperative period. Meningitis improved with administration of antibiotics. For prevention of exposure keratitis associated with left facial palsy, upper blepharoplasty with gold weight implantation was performed. After one and a half years, gamma-knife radiosurgery was performed for the residual tumor of the left CPA measuring 1.7 cm × 1.2 cm in size (3.641 Gy/min for 23.6 minutes). The size of the residual tumor decreased slowly, and HB grade III facial palsy was noted. To date, there is no regrowth of the brain tumor (Fig. 1). For the evaluation of the colon, colonoscopy was performed. A fibrin covered, fungating huge mass was nearly obstructing the lumen of the sigmoid colon, and the scope could not pass through it. The biopsy result indicated only necrotic fibrinopurulent debris, and it did not provide a clear diagnosis (Fig. 3). On abdomino-pelvic CT, colo-colonic intussusception with a 4.8-cm-sized mass in the descending colon and enlarged pericolic lymph nodes were observed (Fig. 4). On PET/CT, a hypermetabolic mass in the descending colon with SUVmax 9.9 and hypermetabolic activity in the pericolic lymph nodes were observed (Fig. 4). These findings suggested that the mass was suspicious for colon cancer. Laboratory blood tests were within their normal ranges and the CEA level was 1.5 ng/mL (reference range, ~6.0 ng/mL).
Fig. 1.
Vestibular schwannoma on brain MRI. (A) T1 weighted image of vestibular schwannoma at the cerebello-pontine angle before neurosurgery. (B) T2 weighted image of vestibular schwannoma at the cerebello-pontine angle before neurosurgery. (C) T1 weighted image of residual vestibular schwannoma before Gamma-knife surgery. (D) T1 weighted image of residual vestibular schwannoma after Gamma-knife surgery.
Fig. 2.
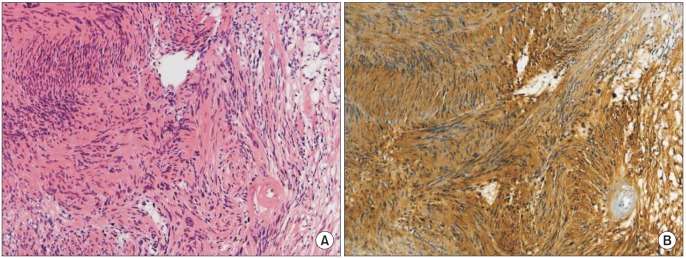
Pathologic findings of brain schwannoma. (A) The tumor shows typical microscopic appearance of a schwannoma. It is composed of spindle cells arranged in interlacing fascicles (Antoni A: cellular area, H&E: ×200) showing transition with loose meshwork of delicate collagen fibers (Antoni B: acellular area). (B) The tumor cells strongly and diffusely express the S-100 protein (×200).
Fig. 3.
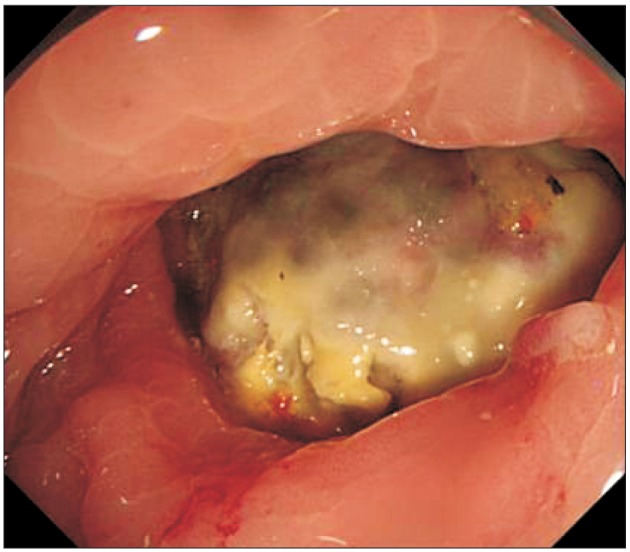
Intussuscepted tumor in the descending colon on preoperative colonoscopy.
Fig. 4.
Preoperative radiologic imaging (A-C, CT; D, PET).
Under the impression of colon cancer, left hemicolectomy was planned. With endotracheal intubation, a 7-cm midline incision was made and the intra-abdominal cavity was explored. There was no evidence of ascites, adhesion, peritoneal seeding, or liver metastasis. A tumor measuring 9 cm × 7 cm in size was located at the splenic flexure, and it intussuscepted into the sigmoid-descending colon junction. Pericolic lymph nodes were slightly enlarged, but frozen biopsy of lymph nodes around the inferior mesenteric vein did not show presence of a tumor. Then, left branches of the middle colic artery and left colic artery were securely ligated and the specimen was resected. End-to-end anastomosis was performed by the hand-sewn method. After saline irrigation, meticulous bleeding control was achieved and the operation was completed.
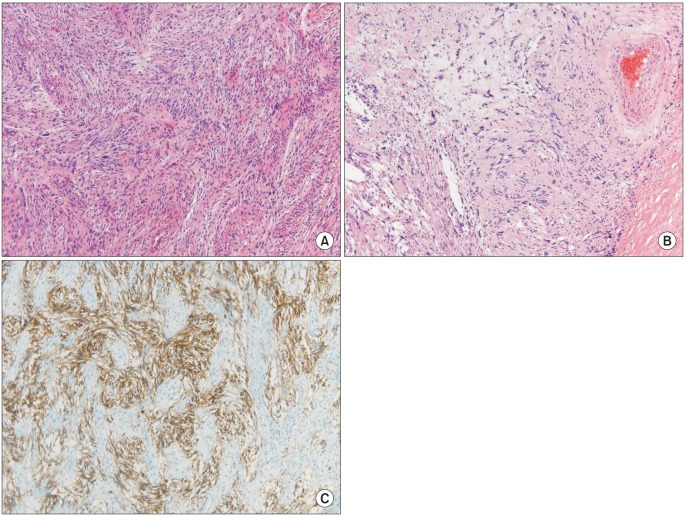
On histologic examination, the tumor size was 5.2 cm × 4.2 cm × 3.1 cm and the tumor extended from the mucosa to the subserosal soft tissue (Fig. 5). Mitotic activity was found in 1/10 high power field, the number of retrieved lymph nodes was 35 without metastasis, and there was no perineural or lymphovascular tumor cell invasion. Resection margins were free of tumor cells. Immunohistochemical staining showed S-100 (+), smooth muscle actin (-), and CD 34(-) (Fig. 6).
Fig. 5.
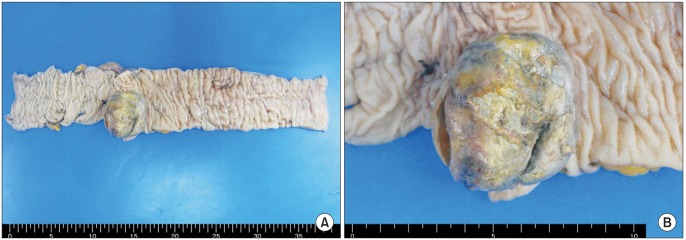
(A, B) Gross features of colonic schwannoma.
Fig. 6.
Pathologic findings of colonic schwannoma. (A) The tumor is composed of compact spindle cells arranged in interlacing fascicles (Antoni A: H&E, ×100). (B) In the other part, more loosely arranged, delicate collagen fibers are noted (Antoni B: H&E, ×100). Ectatic vessel with surrounding hyalinization is also noted. (C) The tumor cells strongly and diffusely express the S-100 protein (×100).
Sips of water were started on postoperative day 4 and soft diet on day 5. She recovered without complications and was discharged on postoperative day 10. She did not show any recurrence of tumor until 1 year after colon surgery.
DISCUSSION
Schwannoma is a kind of benign tumor arising from Schwann cells that form the neural sheath [3,7]. Sixty percent of these tumors originate from cranial nerves [7], and the most common type is vestibular schwannoma [7]. Schwannomas of the brain represent approximately 8% of all intracranial tumors, for which the treatment of choice is complete surgical excision with tumor-free margins [7].
On the other hand, gastrointestinal schwannomas are rare [4,5]. They originate from Schwann cells in the neurons of the myenteric plexus in the digestive tract [5]. It has been estimated that schwannomas represent only 2%-6% of all stromal tumors of the gastrointestinal tract [5]. Stomach and small intestine are the most common sites for schwannomas [4,5,6], and primary schwannomas of the colon are extremely rare [2,4]. The most common location for schwannoma of the large intestine is cecum, followed by sigmoid colon, transverse colon, descending colon, and rectum [4]. The best treatment for these tumors is complete surgical excision with adequate surgical margins, which is similar to that for schwannomas in the brain [2,4].
Schwannomas are very difficult to diagnose preoperatively. For differential diagnosis, immunohistochemical staining is necessary, in particular for S-100 protein, CD117 (KIT), and CD34. In general, schwannomas are completely positive for S-100 protein, consistently negative for CD117, and usually negative for CD34. These special immunohistochemical staining methods could be helpful for discriminating schwannomas from other stromal tumors [5,6].
Although schwannomas are considered to be benign tumors, they have a tendency to recur locally and become malignant [3]. Also, the response of schwannomas to chemotherapy and radiotherapy remain uncertain. Therefore, complete surgical excision with tumor-free margins is very important for achieving an excellent long-term outcome [1,3].
The case presented here is interesting because the woman had a rare colonic schwannoma metachronously with a past history of vestibular schwannoma.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Di Cataldo A, Trombatore C, Cocuzza A, Latino R, Li Destri G, Petrillo G. Synchronous occurrence of colon adenocarcinoma and gastric schwannoma case report and review of the literature. Ann Ital Chir. 2013 Jul 2;84 [Epub] [PubMed] [Google Scholar]
- 2.Braumann C, Guenther N, Menenakos C, Junghans T. Schwannoma of the colon mimicking carcinoma: a case report and literature review. Int J Colorectal Dis. 2007;22:1547–1548. doi: 10.1007/s00384-006-0264-9. [DOI] [PubMed] [Google Scholar]
- 3.Fotiadis CI, Kouerinis IA, Papandreou I, Zografos GC, Agapitos G. Sigmoid schwannoma: a rare case. World J Gastroenterol. 2005;11:5079–5081. doi: 10.3748/wjg.v11.i32.5079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miettinen M, Shekitka KM, Sobin LH. Schwannomas in the colon and rectum: a clinicopathologic and immunohistochemical study of 20 cases. Am J Surg Pathol. 2001;25:846–855. doi: 10.1097/00000478-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Nonose R, Lahan AY, Santos Valenciano J, Martinez CA. Schwannoma of the colon. Case Rep Gastroenterol. 2009;3:293–299. doi: 10.1159/000237736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park KJ, Kim KH, Roh YH, Kim SH, Lee JH, Rha SH, et al. Isolated primary schwannoma arising on the colon: report of two cases and review of the literature. J Korean Surg Soc. 2011;80:367–372. doi: 10.4174/jkss.2011.80.5.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sanmillan JL, Plans G, Vidal N, Acebes JJ. Supratentorial brain schwannomas: an uncommon location for a common tumour. Br J Neurosurg. 2014;28:25–28. doi: 10.3109/02688697.2013.815320. [DOI] [PubMed] [Google Scholar]