Abstract
Purpose
The aim of this retrospective study was to evaluate the feasibility of single incision laparoscopic surgery (SILS), and to compare the short-term surgical outcomes with those of conventional laparoscopic surgery for colorectal cancer.
Methods
Forty-four patients who underwent SILS were compared with 263 patients who underwent conventional laparoscopic surgery for colorectal adenocarcinoma between November 2011 and September 2012.
Results
In the SILS group, eleven cases (25.0%) of right hemicolectomy, 15 (34.1%) anterior resections, and 18 (40.9%) low anterior resections were performed. Additional ports were required in 10 rectal patients during SILS operation. In the 32 patients with rectosigmoid and rectal cancer in the SILS group, patients with mid and lower rectal cancers had a tendency to require a longer operation time (168.2 minutes vs. 223.8 minutes, P = 0.002), additional ports or multiport conversion (P = 0.007), than those with rectosigmoid and upper rectal cancer. Both SILS and conventional groups had similar perioperative outcomes. Operation time was longer in the SILS group than in the conventional laparoscopic surgery group (185.0 minutes vs. 139.2 minutes, P < 0.001). More diverting stoma were performed in the SILS group (64.7% vs. 24.2%, P = 0.011). Multivariate analysis showed that tumor location in the rectum (95% confidence interval [CI], 1.858-10.560; P = 0.001), SILS (95% CI, 3.450-20.233; P < 0.001), diverting stoma (95% CI, 1.606-9.288; P = 0.003), and transfusion (95% CI, 1.092-7.854; P = 0.033) were independent risk factors for long operation time (>180 minutes).
Conclusion
SILS is a feasible, not inferior treatment option for colorectal cancer, and appears to have similar results as standard conventional multiport laparoscopic colectomy, despite the longer operative time.
Keywords: Single incision, Laparoscopic surgery, Colorectal neoplasms
INTRODUCTION
Laparoscopic surgery has gained wide acceptance in colon cancer treatment, and its oncologic outcomes have been shown to be at least equivalent to those of conventional open surgery. Moreover, the safety and feasibility of laparoscopic resection of rectal cancer have also been shown to be equivalent to open surgery, thus application has been extended to rectal cancer.
Previous multicenter prospective randomized controlled trials reported that laparoscopy has benefits in the short-term outcomes, including early postoperative recovery, decreased postoperative pain, shorter hospital stay [1,2,3], and safe oncologic outcomes in colon and rectal cancer [4,5,6].
Recently, single incision laparoscopic surgery (SILS) for reducing laparoscopic ports and minimizing the potential risks of trocar related complications has emerged as a novel technique, and has been applied to colorectal surgery [7,8,9,10,11,12].
The aim of our study was to compare the short-term surgical outcomes of SILS with conventional laparoscopic colectomy for colorectal cancer.
METHODS
Three hundred and ninety-seven patients with colorectal cancer underwent laparoscopic colectomy as an elective operation at our institute in the Department of Colon and Rectal Surgery between October 2011 and August 2012.
Perioperative data of 44 consecutively enrolled patients in the SILS group were prospectively collected, and were compared with those of 263 patients in the conventional laparoscopic surgery group, retrospectively.
Each procedure was performed by three board-certified colorectal surgeons. This study was approved by the Institutional Review Board of Chonnam National University Hwasun Hospital, and written informed consent for the operation was received from all patients.
The following were the inclusion criteria for the present study: (1) patients aged over 18 years; (2) histologically confirmed colon or rectal adenocarcinoma; (3) patients planning to undergo elective laparoscopic colectomy; and (4) patients interested in SILS after gaining informed consent for both SILS and conventional techniques, with counseling for the potential of requiring additional ports and conversion to open surgery. The exclusion criteria were as follows: (1) patients with a bulky large tumor (size greater than 7 cm on preoperative radiologic examination); (2) unresectable distant solid organ metastasis; (3) operations conducted in an emergency setting; and (4) subtotal colectomy with familial adenomatous polyposis or synchronous multiple colorectal cancers.
Rectal cancer was defined as an adenocarcinoma located within 15 cm of the anal verge upon rigid sigmoidoscopy or digital rectal examination, and was classified according to tumor location in the distal margin of the tumor. Tumors located 10-15 cm from the anal verge were classified as upper rectal cancer, while those within 10 cm of the anal verge were classified as mid and lower rectal cancer.
Every patient was placed on identical perioperative recovery schemes involving mechanical bowel preparation, postoperative feeding, removal of the Foley catheter, postoperative pain control, and additional quality measures.
Perioperative data on age, gender, American Society of Anesthesiologists (ASA) score, body mass index (BMI, kg/m2), laparotomy history, location of tumor, operative time, estimated blood loss, transfusion, intraoperative complications, conversion to additional multiports or open surgery, tumor size, resection margin, number of harvested lymph nodes, postoperative time to first flatus, postoperative length of hospital stay, postoperative complications, and mortality occurring within 30 postoperative days were collected. In addition, postoperative complications were classified into grades 1 to 5, as defined by Dindo et al. [13].
Postoperative pain control consisted of epidural anesthesia for 3 days following surgery, and perioperative management with patient controlled intravenous administration of morphine chlorhydrate with narcotics for 3 days after surgery, as reported in a previous study [14]. Nonsteroidal anti-inflammatory drugs, analgesic ketorolac tromethamine (30 mg), and opioid pethidine hydrochloride (25 mg) were also given to control pain. Subjective pain scores (on a scale of 0-10, with 0 representing no postoperative wound pain and 10 representing the worst possible wound pain) using a visual analog scale were collected at postoperative days 1, 2, 3, 4, 5, and 7, and were used to compare postoperative wound pain between the two groups between the two groups.
Surgical technique
Conventional group
All patients were placed in the modified lithotomic position and Trendelenburg position after general anesthesia. The OCTO port wound retractor (OT 301, Dalim Co., Seoul, Korea) was placed into the transumbilical minilaparotomy, and then insufflations of 12 mmHg CO2 were performed. A 30-degree, 10 mm-diameter rigid laparoscope was introduced to explore the entire abdomen. Subsequent additional ports were placed as needed according to the type of operation, via a 5-port technique.
The medial-to-lateral approach was used for both right and left sided colorectal cancers, to identify the ureter and the gonadal vessels. For right colon cancers, stapled side-to-side extracorporeal anastomosis was performed.
For rectal cancer, laparoscopic total mesorectal excision was done on the posterior side, the lateral side, and then the anterior side, with removal of Denonvillier's fascia.
An Echelon 60 ENDOPATH stapling device (Ethicon Endo Surgery, Cincinnati, OH, USA) was inserted, and transection of the segment including the specimen was performed. All specimen delivery was done via transumbilical minilaparotomy, with extension of the umbilical port. Extracorporeal transaction of the colonic segment was also performed. After anvil insertion into the proximal colonic segment and re-establishment of the pneumoperitoneum, primary anastomosis was performed with an end to end anastomosis circular stapler (Ethicon Endo Surgery).
SILS group
After making a vertical incision to the periumbilical area, an OCTO single port system (OT304, Dalim Co.), which is used for SILS composed of 4 ports (5, 5, 10, 12 mm) that are placed through a single access device, was inserted through the periumbilical minilaparotomy or in the planned right lower quadrant ileostomy site, and CO2 pneumoperitoneum was produced.
The addition of 5 mm, 12 mm, or larger trocars during the operation was regarded as conversion to multiport laparoscopic surgery. A rigid 10-mm, 30-degree laparoscope was used via the 12-mm access of the OCTO single port. For isolation and division of the middle colic vessels in the extended right hemicolectomy, the assistant surgeon inserted a grasper via the 10-mm access of the four-channeled OCTO single port, tenting the transverse mesocolon for counter-traction. Extracorporeal side-to-side ileocolic anastomosis using a linear stapler (TLC, Ethicon Endo Surgery) was performed after transumbilical specimen delivery, as in the conventional laparoscopic group.
For left side colon cancers, the medial to lateral approach was used for dividing the inferior mesenteric vessels. For mid and low rectal cancers, the assistant surgeon inserted a fan-shaped ENDO RETRACT 10-mm Retractor (Covidien, Mansfield, MA, USA) via the 10-mm access of the OCTO single port for elevation of the peritoneal reflection.
A curved linear stapler was introduced through the 12-mm access of the OCTO single port after the optic scope was changed to the 10-mm access. Following this, down to up or up to down vertical rectal transaction was performed, instead of the transversal rectal resection through a low right port done in the conventional laparoscopic group. After extracorporeal transumbilical specimen delivery, intracorporeal colorectal anastomosis was performed using a circular stapler (EEA 29 mm, Ethicon Endo surgery).
Statistical analysis
Differences between the two groups were evaluated by the chi-square test or Fisher exact test, and the Student t-test. A two-tailed P-value <0.05 was considered to be statistically significant.
Parameters associated in univariate analysis (P < 0.10) were subjected to multivariate analysis with logistic regression to identify independently affected outcomes associated with long operation time and postoperative morbidity. Statistical analysis was performed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
Between November 2011 and September 2012, forty-four patients underwent the SILS operation for colorectal cancer, while 263 patients underwent conventional multiport laparoscopic colorectal surgery (Table 1). In the SILS group, 11 (25.0%) right hemicolectomies, 15 (34.1%) anterior resections, and 18 (40.9%) low anterior resections were performed. Eleven of 18 rectal cancer patients (61.1%) had a diverting ileostomy during the SILS operation, and the diverting ileostomy site was used as a single incision minilaparotomy in the remaining seven. Additional ports were required in 10 rectal patients (22.7%) who underwent the SILS operation (one additional port in 7, and 4 multiport conversions to conventional laparoscopic surgery in 3). The main reasons for the additional port conversion were difficulty in exposure of the peritoneal reflection (n = 3), pelvic wall dissection (n = 4), stapled rectal transaction in the narrow pelvis (n = 2), and discovery of a bulky tumor with presacral fixation (n = 1).
Table 1.
Demographics of patients
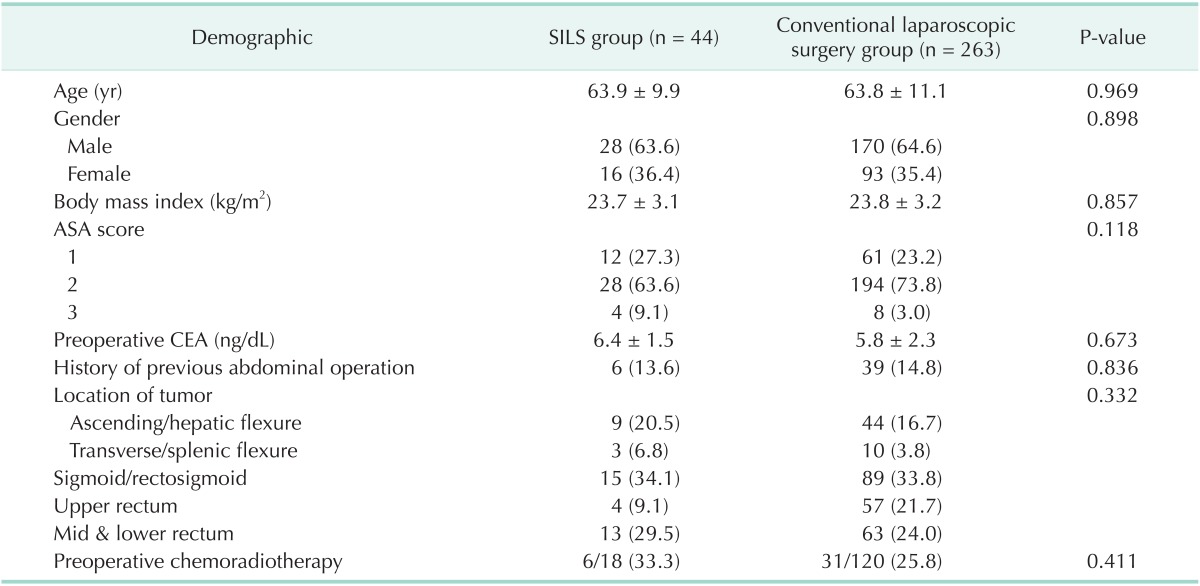
Values are presented as mean ± standard deviation or number (%).
SILS, single incision laparoscopic surgery; ASA, American Society of Anesthesiologists.
The operative data were listed in Table 2. All operations were completed without conversion to open surgery. Formation of a diverting ileostomy was higher in the SILS group (P = 0.011), and operation time was also longer in the SILS group than in the conventional laparoscopic surgery group (185.0 minutes vs. 139.2 minutes, P < 0.001).
Table 2.
Operative results
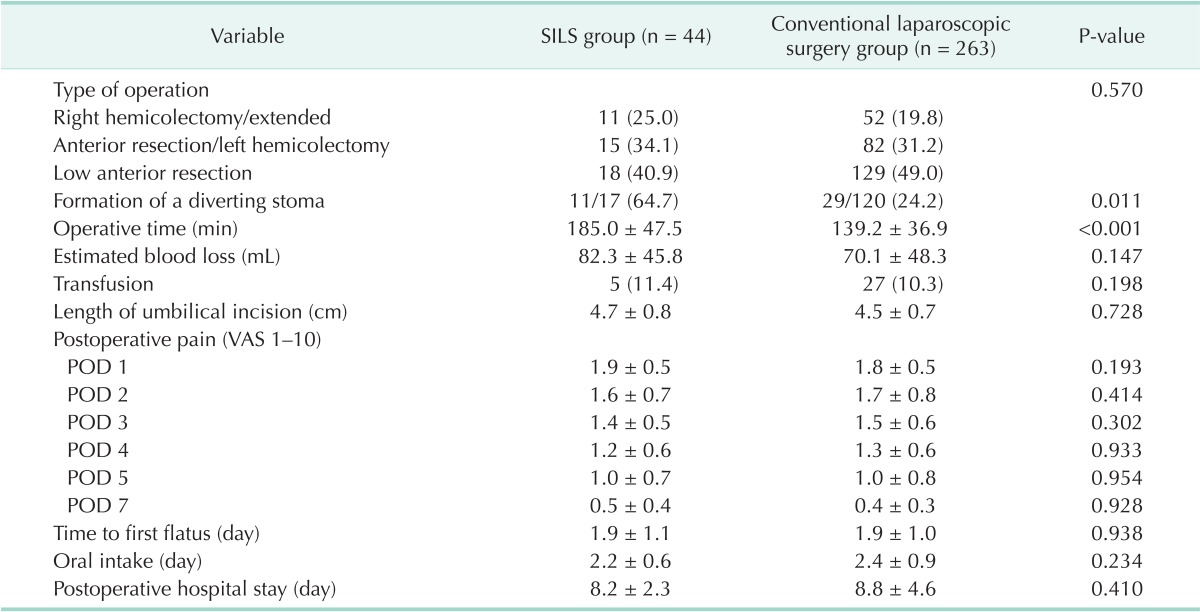
Values are presented as number (%) or mean ± standard deviation.
VAS, visual analog scale.
There were no significant differences in the pathologic data (Table 3). Postoperative morbidity was similar in both groups (Table 4). Fourteen patients of anastomotic leakage were managed with a diverting loop ileostomy, irrigation and drainage. Intraabdominal bleeding was noted in four patients; one patient of the SILS group was managed conservatively, while the other three were managed by suture hemostasis. Among five patients with anastomotic bleeding, three were controlled by colonoscopic clipping, and two had re-explored suture hemostasis. No mortality was observed postoperatively.
Table 3.
Pathologic outcomes
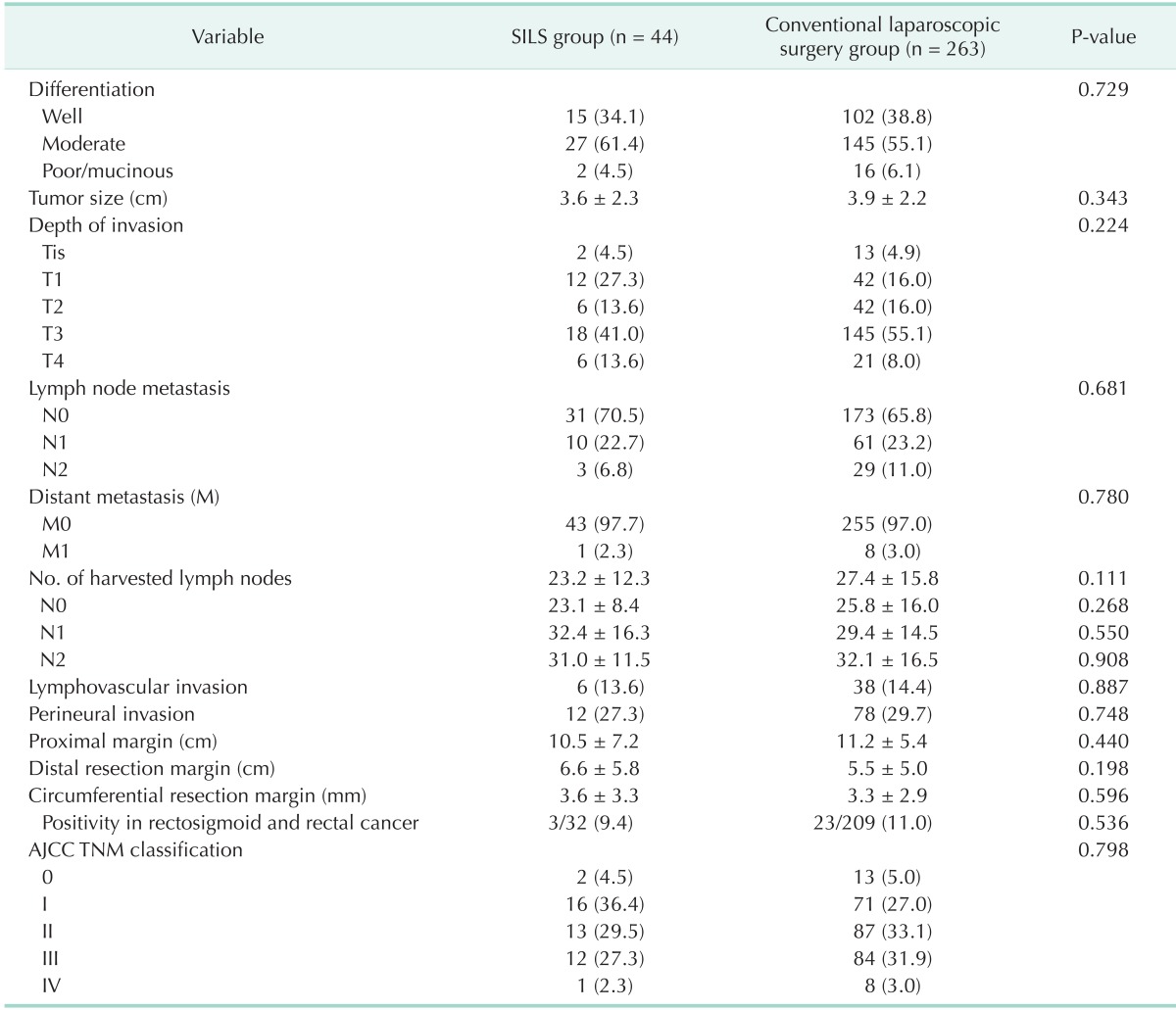
Values are presented as number (%) or mean ± standard deviation.
SILS, single incision laparoscopic surgery; AJCC, American Joint Committee on Cancer.
Table 4.
Perioperative complications
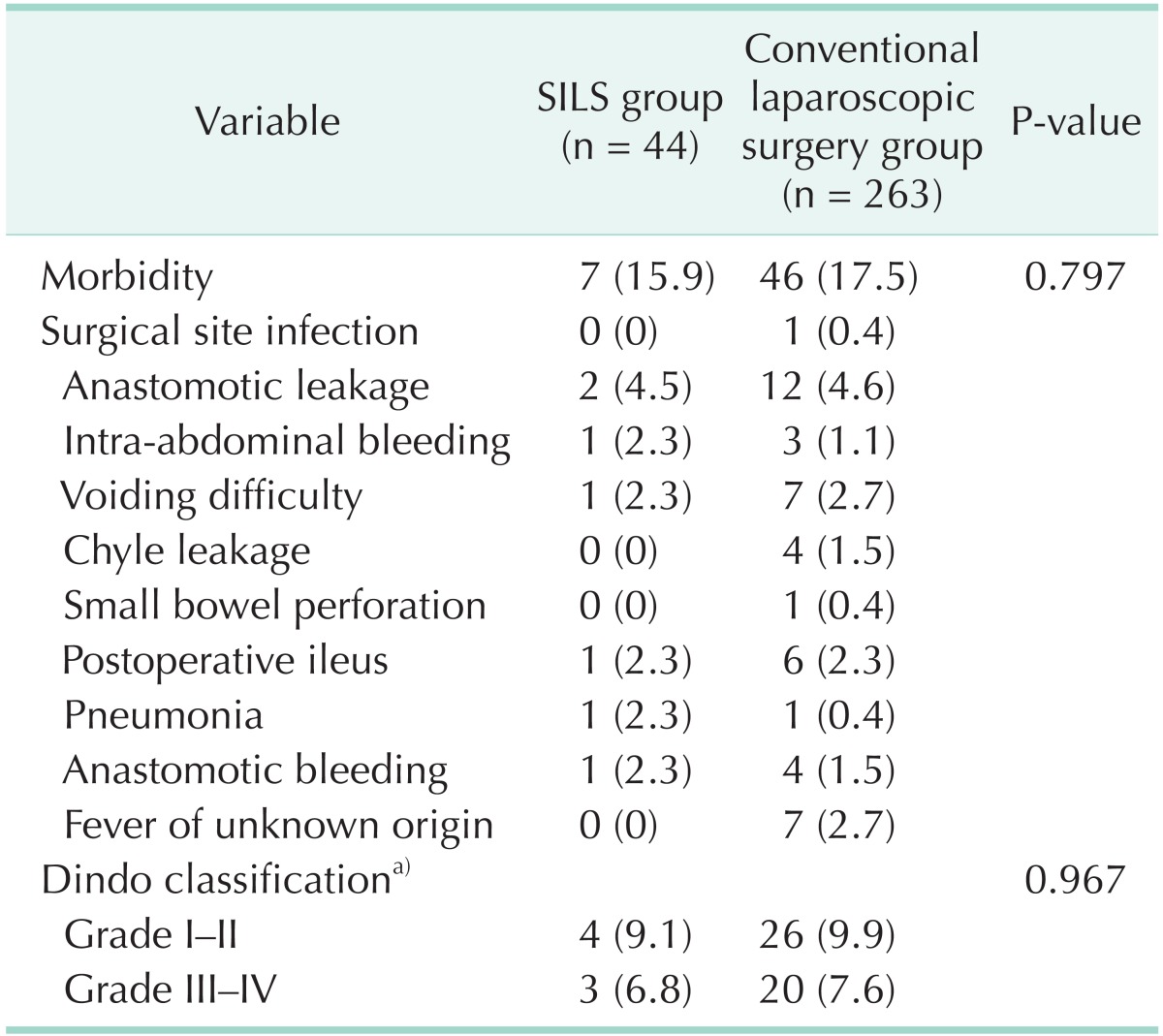
Values are presented as number (%).
SILS, single incision laparoscopic surgery.
Grade I: any deviation from the normal postoperative course without the need for pharmacological treatment or surgical, endoscopic and radiological interventions. Grade II: requiring pharmacological treatment with drugs other than those allowed for grade I complications. Grade III: requiring surgical, endoscopic or radiological intervention. Grade IV: life-threatening complication requiring intensive care unit management.
a)Classification of surgical complications according to Dindo et al. [13].
In the analysis of 32 patients with rectosigmoid and rectal cancer in the SILS group, patients with mid and lower rectal cancer had a higher tendency to undergo longer operations (168.2 minutes vs. 223.8 minutes, P = 0.002) and to have subsequent diverting stoma (P < 0.001) than those with rectosigmoid and upper rectal cancer (Table 5). Furthermore, these patients had a 9.917-fold greater risk of requiring additional ports (95% confidence interval [CI], 1.597-61.597, P = 0.007) than those of rectosigmoid and upper rectum who underwent SILS.
Table 5.
Characteristics of 32 patients who underwent SILS operation according to the tumor location of rectosigmoid and rectal cancer
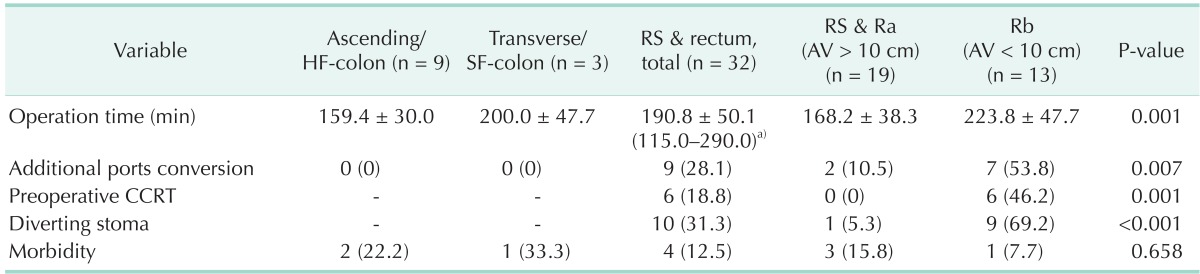
Values are presented as mean ± standard deviation or number (%).
SILS, single incision laparoscopic surgery; HF, hepatic flexure; SF, splenic flexure; RS, rectosigmoid; Ra, upper rectum; Rb, mid and lower rectum; CCRT, chemoradiation therapy.
a)Range.
Univariate and multivariate analyses showed that tumors located in the rectum (95% [CI], 1.858-10.560; P = 0.001), SILS (95% CI, 3.450-20.233; P < 0.001), diverting stoma (95% CI, 1.606-9.288; P = 0.003), and transfusion (95% CI, 1.092-7.854; P = 0.033) were independent risk factors for a longer operation time (>180 minutes).
DISCUSSION
SILS has emerged as a new generation of laparoscopic colorectal surgery that is akin to conventional surgery, with the added benefit of better cosmesis, reduced morbidity, reduced postoperative pain, and reduced length of hospital stay, along with minimal trocar related potential complications of abdominal trauma, vessel injury, wound infection, trocar site hernia, and port-recurrences [15,16,17,18]. However, its use for rectal cancer treatment is still under debate due to pelvic exposure, especially for low rectal dissection.
The disadvantages of SILS are cross hand phenomenon and loss of triangulation [8,19,20]. Fully tilting the patient toward the right side of the reverse Trendelenburg position using gravity and a transparietal sling suture may facilitate counterattraction to overcome the lack of triangulation [11,14,21].
Application of single port laparoscopic surgery to rectal cancer is very limited in that rectal mobilization and total mesorectal excision with SILS demands technical efficiency to avoid tearing and shallow breaks into the mesorectum [17,21,22]. Bulut et al. [21] reported the initial experiences with 10 cases of single-port laparoscopic surgery for rectal cancer, in which an extra 5-mm port was added in 2 cases (20%) to deal with intraoperative complications.
In the present study, with regard to the deep bony pelvis, the planned ileostomy site was used for SILS minilaparotomy instead of making a transumbilical incision in seven of the rectal cancer cases, and switching of the locations between the operator and the optic scopist was helpful for more suitable and precise reach into the deep pelvis. Additional ports were used in 9 out of 32 patients (28.1%) with rectosigmoid and rectum cancer. Mid and lower rectal cancer had a higher requirement for additional ports than rectosigmoid and rectum cancer. The need for additional ports in SILS for rectal cancer in the present study also caused difficulty in exposure, suggesting that narrow pelvic dissection beyond the peritoneal reflection might be a limitation of SILS, in the attempt to keep oncologic principles.
Transumbilical area was determined as the suitable area for multiaccess single apparatus for upper rectal cancer, and the site for diverting ileostomy was chosen for SILS minilaparotomy in tumors located in the mid rectum. For SILS in lower rectal cancer, using the transanal approach for total mesorectal excision might be a helpful solution [23,24,25].
Operation time of the SILS group was longer than that of the conventional laparoscopic group in the present study. Some previous reports reported a similar operation time for SILS to conventional multiports surgery [26,27], whereas others required a longer time than the conventional group [17,18]. In the present study, risk factors related to longer operation time included rectal tumor location, SILS technique, diverting stoma formation, and transfusion. Factors such as being overweight (i.e., BMI > 25 kg/m2) or having a history of laparotomy were not found to be related.
In comparison with the operation time of 185.0 minutes via SILS with that of 225.5 minutes via a previously reported reduced port laparoscopic colectomy [14], operation time became shorter as the surgeon gained more experience. Presently, operating time became shorter as more cases were performed, and comparison of the operation time of the first 10 SILS cases to the last 10 cases revealed a significant difference in the mean operation time: last 10 cases (153.5 ± 33.8 minutes) vs. first 10 cases (190.5 ± 37.1 minutes) (P = 0.032). These results show that the operation time required for SILS may become shorter with surgeons' experience.
The length of minilaparotomy for specimen delivery was comparable in both groups in the present study, and is in good agreement with a study that reported incision length to be determined by the specimen size, BMI and abdominal wall, rather than the operation method of SILS or conventional laparoscopy [16].
No conversion to open procedure was required in the present study. During the SILS procedure, conversion to an open procedure could be avoided by performing an easy conversion to conventional laparoscopic surgery by adding additional ports as necessary. Moreover, both SILS and conventional laparoscopic surgery for selective patients, performed by experienced laparoscopic surgeons, might lead to the continued use of the laparoscopic approach with the avoidance of negative outcomes associated with open conversions [16,20,28,29].
The total cost increase was only that incurred by the use of the multi trocared OCTO port of 250 Euro, thus the operative cost was not significantly different than the average cost of conventional standard multiport surgery (average cost of 80 Euro per each port), and not inferior in the aspect of cost effectiveness (the total comparative financial data are not shown).
One potential advantage of the SILS technique for colectomy is decreased postoperative pain, considering the reduced number of additional ports to avoid trauma at separate sites on the abdominal wall, which may decrease early postoperative pain [16,26,30], although no significant reduction in the postoperative pain score was detected in the present study. This may be due to the postoperative epidural/narcotic analgesics pain management used.
Potential drawbacks of this study include the retrospective nature, the heterogeneous group with very small subgroups, lack of objective measurement of postoperative pain, quality of cosmesis or satisfaction of body contour, and parameters of postoperative immunologic response. Larger-sized, planned multicenter prospective randomized trials are warranted, and long-term oncologic outcomes should be reported to generalize the results to all colorectal patients. The limited role of an assistant surgeon and the negative impact of education should be discussed on the topic of surgical training [29]. In conclusion, SILS is a feasible and safe operation akin to conventional laparoscopic colectomy, when performed by experienced laparoscopic colorectal surgeons. The short-term surgical outcome of SILS for colon cancer might be acceptable without disturbing oncologic principles.
Footnotes
This paper was presented as a poster at the Scientific Session of 2013 SAGES Annual Meeting, 17-20 April, 2013, Baltimore, MD, USA.
No potential conflict of interest relevant to this article was reported.
References
- 1.Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350:2050–2059. doi: 10.1056/NEJMoa032651. [DOI] [PubMed] [Google Scholar]
- 2.Akmal Y, Bailey C, Baek JH, Metchikian M, Pigazzi A. Oncological outcomes of laparoscopic colon resection for cancer after implementation of a full-time preceptorship. Surg Endosc. 2011;25:2967–2971. doi: 10.1007/s00464-011-1654-9. [DOI] [PubMed] [Google Scholar]
- 3.Braga M, Frasson M, Zuliani W, Vignali A, Pecorelli N, Di Carlo V. Randomized clinical trial of laparoscopic versus open left colonic resection. Br J Surg. 2010;97:1180–1186. doi: 10.1002/bjs.7094. [DOI] [PubMed] [Google Scholar]
- 4.Kang SB, Park JW, Jeong SY, Nam BH, Choi HS, Kim DW, et al. Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol. 2010;11:637–645. doi: 10.1016/S1470-2045(10)70131-5. [DOI] [PubMed] [Google Scholar]
- 5.Laurent C, Leblanc F, Wutrich P, Scheffler M, Rullier E. Laparoscopic versus open surgery for rectal cancer: long-term oncologic results. Ann Surg. 2009;250:54–61. doi: 10.1097/SLA.0b013e3181ad6511. [DOI] [PubMed] [Google Scholar]
- 6.Lacy AM, Delgado S, Castells A, Prins HA, Arroyo V, Ibarzabal A, et al. The long-term results of a randomized clinical trial of laparoscopy-assisted versus open surgery for colon cancer. Ann Surg. 2008;248:1–7. doi: 10.1097/SLA.0b013e31816a9d65. [DOI] [PubMed] [Google Scholar]
- 7.Brunner W, Schirnhofer J, Waldstein-Wartenberg N, Frass R, Weiss H. Single incision laparoscopic sigmoid colon resections without visible scar: a novel technique. Colorectal Dis. 2010;12:66–70. doi: 10.1111/j.1463-1318.2009.01894.x. [DOI] [PubMed] [Google Scholar]
- 8.Adair J, Gromski MA, Lim RB, Nagle D. Single-incision laparoscopic right colectomy: experience with 17 consecutive cases and comparison with multiport laparoscopic right colectomy. Dis Colon Rectum. 2010;53:1549–1554. doi: 10.1007/DCR.0b013e3181e85875. [DOI] [PubMed] [Google Scholar]
- 9.Chambers WM, Bicsak M, Lamparelli M, Dixon AR. Single-incision laparoscopic surgery (SILS) in complex colorectal surgery: a technique offering potential and not just cosmesis. Colorectal Dis. 2011;13:393–398. doi: 10.1111/j.1463-1318.2009.02158.x. [DOI] [PubMed] [Google Scholar]
- 10.Remzi FH, Kirat HT, Geisler DP. Laparoscopic single-port colectomy for sigmoid cancer. Tech Coloproctol. 2010;14:253–255. doi: 10.1007/s10151-009-0545-8. [DOI] [PubMed] [Google Scholar]
- 11.Fujii S, Watanabe K, Ota M, Watanabe J, Ichikawa Y, Yamagishi S, et al. Single-incision laparoscopic surgery using colon-lifting technique for colorectal cancer: a matched case-control comparison with standard multiport laparoscopic surgery in terms of short-term results and access instrument cost. Surg Endosc. 2012;26:1403–1411. doi: 10.1007/s00464-011-2047-9. [DOI] [PubMed] [Google Scholar]
- 12.Geisler D, Garrett T. Single incision laparoscopic colorectal surgery: a single surgeon experience of 102 consecutive cases. Tech Coloproctol. 2011;15:397–401. doi: 10.1007/s10151-011-0756-7. [DOI] [PubMed] [Google Scholar]
- 13.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lim SW, Kim HJ, Kim CH, Huh JW, Kim YJ, Kim HR. Umbilical incision laparoscopic colectomy with one additional port for colorectal cancer. Tech Coloproctol. 2013;17:193–199. doi: 10.1007/s10151-012-0900-z. [DOI] [PubMed] [Google Scholar]
- 15.Lai CW, Edwards TJ, Clements DM, Coleman MG. Single port laparoscopic right colonic resection using a 'vessel-first' approach. Colorectal Dis. 2012;14:1138–1144. doi: 10.1111/j.1463-1318.2011.02898.x. [DOI] [PubMed] [Google Scholar]
- 16.Papaconstantinou HT, Sharp N, Thomas JS. Single-incision laparoscopic right colectomy: a case-matched comparison with standard laparoscopic and hand-assisted laparoscopic techniques. J Am Coll Surg. 2011;213:72–80. doi: 10.1016/j.jamcollsurg.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 17.Kim SJ, Ryu GO, Choi BJ, Kim JG, Lee KJ, Lee SC, et al. The short-term outcomes of conventional and single-port laparoscopic surgery for colorectal cancer. Ann Surg. 2011;254:933–940. doi: 10.1097/SLA.0b013e318237826b. [DOI] [PubMed] [Google Scholar]
- 18.Champagne BJ, Lee EC, Leblanc F, Stein SL, Delaney CP. Single-incision vs straight laparoscopic segmental colectomy: a case-controlled study. Dis Colon Rectum. 2011;54:183–186. doi: 10.1007/DCR.0b013e3181fd48af. [DOI] [PubMed] [Google Scholar]
- 19.Law WL, Fan JK, Poon JT. Single-incision laparoscopic colectomy: early experience. Dis Colon Rectum. 2010;53:284–288. doi: 10.1007/DCR.0b013e3181c959ba. [DOI] [PubMed] [Google Scholar]
- 20.Makino T, Milsom JW, Lee SW. Feasibility and safety of single-incision laparoscopic colectomy: a systematic review. Ann Surg. 2012;255:667–676. doi: 10.1097/SLA.0b013e31823fbae7. [DOI] [PubMed] [Google Scholar]
- 21.Bulut O, Nielsen CB, Jespersen N. Single-port access laparoscopic surgery for rectal cancer: initial experience with 10 cases. Dis Colon Rectum. 2011;54:803–809. doi: 10.1007/DCR.0b013e3182147b4d. [DOI] [PubMed] [Google Scholar]
- 22.Bulut O, Nielsen CB. Single-incision laparoscopic low anterior resection for rectal cancer. Int J Colorectal Dis. 2010;25:1261–1263. doi: 10.1007/s00384-010-0947-0. [DOI] [PubMed] [Google Scholar]
- 23.Dumont F, Goere D, Honore C, Elias D. Transanal endoscopic total mesorectal excision combined with single-port laparoscopy. Dis Colon Rectum. 2012;55:996–1001. doi: 10.1097/DCR.0b013e318260d3a0. [DOI] [PubMed] [Google Scholar]
- 24.Gaujoux S, Bretagnol F, Au J, Ferron M, Panis Y. Single port access proctectomy with total mesorectal excision and intersphincteric resection with a primary transanal approach. Colorectal Dis. 2011;13:e305–e307. doi: 10.1111/j.1463-1318.2011.02676.x. [DOI] [PubMed] [Google Scholar]
- 25.Zhang H, Zhang YS, Jin XW, Li MZ, Fan JS, Yang ZH. Transanal single-port laparoscopic total mesorectal excision in the treatment of rectal cancer. Tech Coloproctol. 2013;17:117–123. doi: 10.1007/s10151-012-0882-x. [DOI] [PubMed] [Google Scholar]
- 26.Champagne BJ, Papaconstantinou HT, Parmar SS, Nagle DA, Young-Fadok TM, Lee EC, et al. Single-incision versus standard multiport laparoscopic colectomy: a multicenter, case-controlled comparison. Ann Surg. 2012;255:66–69. doi: 10.1097/SLA.0b013e3182378442. [DOI] [PubMed] [Google Scholar]
- 27.Poon JT, Cheung CW, Fan JK, Lo OS, Law WL. Single-incision versus conventional laparoscopic colectomy for colonic neoplasm: a randomized, controlled trial. Surg Endosc. 2012;26:2729–2734. doi: 10.1007/s00464-012-2262-z. [DOI] [PubMed] [Google Scholar]
- 28.Gandhi DP, Ragupathi M, Patel CB, Ramos-Valadez DI, Pickron TB, Haas EM. Single-incision versus hand-assisted laparoscopic colectomy: a case-matched series. J Gastrointest Surg. 2010;14:1875–1880. doi: 10.1007/s11605-010-1355-z. [DOI] [PubMed] [Google Scholar]
- 29.Leblanc F, Champagne BJ, Augestad KM, Stein SL, Marderstein E, Reynolds HL, et al. Single incision laparoscopic colectomy: technical aspects, feasibility, and expected benefits. Diagn Ther Endosc. 2010;2010:913216. doi: 10.1155/2010/913216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vasilakis V, Clark CE, Liasis L, Papaconstantinou HT. Noncosmetic benefits of single-incision laparoscopic sigmoid colectomy for diverticular disease: a case-matched comparison with multiport laparoscopic technique. J Surg Res. 2013;180:201–207. doi: 10.1016/j.jss.2012.04.063. [DOI] [PubMed] [Google Scholar]


