Abstract
Background
Recent events in healthcare reform have brought national attention to integrating patient experiences and expectations into quality metrics. Few studies have comprehensively evaluated the effect of patient expectations on patient-reported outcomes (PROs) following surgery. The purpose of this study is to systematically review the available literature describing the relationship between patient expectations and postoperative PROs.
Methods
We performed a search of the literature published prior to November 1, 2012. Articles were included in the review if 1) primary data were presented 2) patient expectations regarding a surgical procedure were measured 3) PROs were measured, and 4) the relationship between patient expectations and PROs was specifically examined. PROs were categorized into five subgroups: satisfaction, quality of life (QOL), disability, mood disorder, and pain. We examined each study to determine the relationship between patient expectations and PROs as well as study quality.
Results
From the initial literature search yielding 1,708 studies, 60 articles were included. Fulfillment of expectations was associated with improved PROs among 24 studies. Positive expectations were correlated with improved PROs for 28 (47%) studies, and poorer PROs for 9 (15%) studies. Eighteen studies reported that fulfillment of expectations was correlated with improved patient satisfaction, and 10 studies identified that positive expectations were correlated with improved postoperative QOL. Finally, patients with positive preoperative expectations reported less pain (8 studies) and disability (15 studies) compared with patients with negative preoperative expectations.
Conclusions
Patient expectations are inconsistently correlated with PROs following surgery, and there is no accepted method to capture perioperative expectations. Future efforts to rigorously measure expectations and explore their influence on postoperative outcomes can inform clinicians and policy-makers seeking to integrate PROs into measures of surgical quality.
Keywords: Expectations, Outcomes, Outcome assessment
In the United States, surgical procedures account for 40% of our total healthcare expenditures, and identifying effective measures of surgical quality is a top priority1-4. Although traditional quality indicators, such as hospital readmissions rates or length of stay, can be easily captured by administrative data, these outcomes may not be appropriate for all types of procedures. For example, for high-risk procedures, such as lung resection or pancreatectomy, mortality rates and procedural volume can distinguish surgeon and hospital performance 5,6. However, for common, low-risk procedures, these endpoints are exceedingly rare and not sensitive enough to distinguish variation in patient outcomes 7. Instead, patient-reported outcomes (PROs), such as health-related quality of life and disability, can illuminate differences in treatment effectiveness. In 2010, the Patient Centered Outcomes Research Institute was funded by the Affordable Care Act, and established PROs as a central component of healthcare policy and reform 8-10. Therefore, understanding the factors that influence PROs following surgery can inform strategies to improve the quality of surgical care.
Patients enter each decision for surgery with expectations regarding the effectiveness of the procedure and their postoperative recovery. Their ability to accurately predict these outcomes is the foundation of an informed decision. However, most patients have inaccurate perceptions of both disease conditions and surgery. For example, women incorrectly estimate the quality of life and stigma associated with surgery for breast cancer 11. Similarly, patients with kidney disease often overestimate quality of life following renal transplantation, and the general public predicts poorer quality of life associated with spinal cord injury or colostomy creation than patients report 12-17. Physicians also have difficulty predicting patient recovery and adaptation following surgery 18. For example, physicians often underestimate quality of life following colorectal surgery, such as colostomy creation or total colectomy 19,20. These misconceptions can undermine the process of informed consent, erode patient trust in their physicians, and exacerbate medico-legal tensions. Therefore, understanding the effect of patient expectations on postoperative experiences and outcomes can identify communication barriers between patients and surgeons and improve the decision-making process for patients facing surgery.
To date, the influence of preoperative expectations on PROs following surgery has not been systematically reviewed, and few physicians routinely address patient expectations prior to surgery 21. Therefore, the purpose of this study is to examine the literature describing the relationship between patient expectations and 5 specific PROs following surgery: satisfaction, quality of life, disability, mood disorders, and pain. We hypothesize that patients whose preoperative expectations are sufficiently met following surgery will experience improved outcomes compared with patients whose experience falls short of their expectations.
METHODS
Data sources
A search of the available English language literature published prior to November 1, 2012, was performed by two authors (EM, ES) using the Ovid Medline database. The search was performed using the following Medical Subject Heading (MeSH) terms: patient* and expectation*. The asterisk indicates a truncation function in the search engine, used to include all variations of the search term (e.g patient, patients). We further restricted our search to include only articles that contained patient* in the title or abstract and expectation* in the title. Within the database, we included both indexed and non-indexed citations, and reviewed each article to determine study eligibility and quality.
Study Selection
Articles were included in the review if they met the following inclusion criteria: 1) primary data were presented for adult patients 2) patient expectations regarding a surgical procedure were measured preoperatively and postoperatively 3) PROs were measured preoperatively and postoperatively, and 4) the relationship between patient expectations and PROs was specifically examined. Articles that were not published in the English language were excluded, as well as studies not including primary data (editorials, commentaries, and review papers).
Data Abstraction
The data from each included article were abstracted using a standardized abstraction form. This form included the number of subjects, surgical procedure, method for measuring patient expectations, method of measurement and results of objective outcomes, method of measurement and results of PROs, methodological concerns, and quality assessment. We specifically examined each article to determine the relationship between expectations and PROs, which included either a description of fulfillment of expectations (the match between preoperative expectations and postoperative PRO) and/or an empiric measure of expectation and an empiric measure of PROs.
Assessment of Study Eligibility and Quality
The articles were screened in three phases using our predetermined inclusion and exclusion criteria. The first screen included a review of the titles, and the second screen examined study abstracts. Articles were included if we were unable to determine whether they met the inclusion criteria based on the title or abstract screen. Finally, a full text screen was conducted of the remaining articles to determine if the inclusion criteria were fully met.
After the screening process was complete, we separated the articles into two subgroups based on how the authors measured outcomes: 1) articles reporting PROs such as satisfaction, quality of life or disability and 2) articles reporting objective outcomes such as mortality rate, independent observer’s assessment, or visual acuity. Within each subgroup, we examined the conclusions that each paper found regarding the relationship between patient expectations and outcomes. Based on these findings, we evaluated the overall relationship between expectations and outcomes for each subgroup.
For all of the included studies we assessed the quality of the study using a modified set of criteria for evaluating cohort studies from the US Preventative Services Task Force (USPSTF).22 At least one author assessed the quality of each included study based on the above criteria, and all disagreements were resolved by consensus among authors.
RESULTS
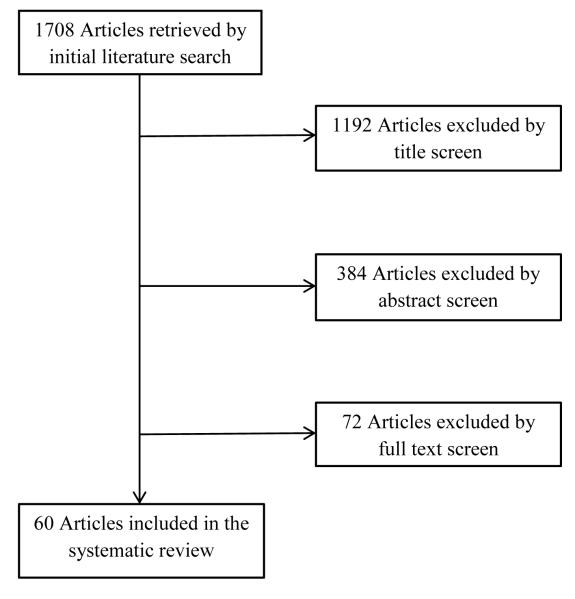
The initial literature search included 1,708 studies (Figure 1). After screening the titles, abstracts, and full texts, 60 articles were included in this review, encompassing 13 different surgical specialties (Online resources 1 & 2). Orthopedic surgery studies were most common (28 articles), as well as neurosurgery (6 articles) and cardiology (5 articles). In total, this systematic review includes 13,806 patients, with an average of 234 patients in each study.
Fig. 1.
Inclusion/exclusion tree.
Patient expectations
Methods used to measure patient expectations varied widely among studies (Appendix 1). Of the 60 studies, only 10 (17%) used previously validated surveys. For example, the Musculoskeletal Outcomes Data Evaluation and Management System (MODEMS) expectation survey measures patient expectations regarding pain relief, daily activity, sleep comfort, return to work, ability to exercise, and future disability 23. Three studies also used the Hospital for Special Surgery Knee Replacement Expectations Survey, which was validated in a group of 160 knee arthroplasty patients 24. This survey consists of 20 items measuring patient expectations regarding pain relief, ability to walk, ability to engage in various activities, and lifestyle considerations. In contrast, 15 studies (25%) used qualitative methods (structured, semi-structured, or open-ended interviews) to assess patient expectations, 27 studies (45%) used ad hoc surveys, and 8 studies (13%) used modified outcomes surveys.
Patient expectations and patient-reported outcome
Table 1 summarizes the relationship between patient expectations and PROs. Specific details regarding findings and limitations for each specific study are listed in Appendix 2. In this review, 24 (40%) studies found that the fulfillment of expectations was correlated with improved PROs, and patient expectations were not correlated with postoperative PROs in 12 (20%) studies. After quality review, 8 studies were deemed “good” quality, 41 were “fair” quality, and 11 were of “poor” quality. (Appendix 3)
Table 1.
Preoperative expectations and postoperative patient-reported outcomes.
| Expectation/outcome relationship | Number of studies |
Percentage of studies |
|---|---|---|
| Fulfillment of expectations related to improved postoperative PROs |
24 | 40% |
| Positive expectations related to improved postoperative PROs | 28 | 46.7% |
| Positive expectations related to worse postoperative PROs | 9 | 15% |
| No correlation between expectations and postoperative PROs | 12 | 20% |
Table 2 details the relationship between patient expectations and 5 specific health-related quality of life outcomes: patient satisfaction, quality of life, disability, mood disorders (ex. anxiety, depression), and pain.
Table 2.
The relationship between preoperative expectations and specific postoperative patient-reported outcomes.
| Expectation/outcome relationship | Number of studies |
Percentage of studies in subgroup |
Percentage of all studies included in the review |
|
|---|---|---|---|---|
|
Satisfaction
(36 studies) |
Fulfillment of expectations related to greater satisfaction |
18 | 50% | 30% |
| Positive expectations related to greater satisfaction |
9 | 25% | 15% | |
| Positive expectations related to worse satisfaction |
8 | 22.2% | 13.3% | |
| No correlation between expectations and satisfaction |
5 | 13.9% | 8.3% | |
| Did not assess satisfaction | 24 | N/A | 40% | |
|
Quality of
life (19 studies) |
Fulfillment of expectations related to greater QOL |
4 | 21% | 6.7% |
| Positive expectations related to greater QOL |
10 | 52.6% | 16.7% | |
| Positive expectations related to worse QOL |
0 | 0% | 0% | |
| No correlation between expectations and QOL |
6 | 31.6% | 10% | |
| Did not assess QOL | 41 | N/A | 68.3% | |
|
Disability
(24 studies) |
Fulfillment of expectations related to less disability |
4 | 16.7% | 6.7% |
| Positive expectations related to less disability |
15 | 62.5% | 25% | |
| Positive expectations related to greater disability |
1 | 4.2% | 1.7% | |
| No correlation between expectations and satisfaction |
4 | 16.7% | 6.7% | |
| Did not assess disability | 36 | N/A | 60% | |
|
Mood
disorders (5 studies) |
Fulfillment of expectations related to less mood disturbance |
0 | 0% | 0% |
| Positive expectations related to less mood disturbance |
3 | 60% | 5% | |
| Positive expectations related to greater mood disturbance |
1 | 20% | 1.7% | |
| No correlation between expectations and mood disturbance |
1 | 20% | 1.7% | |
| Did not assess mood disorders |
55 | N/A | 91.7% | |
|
Pain
(13 studies) |
Fulfillment of expectations related to less pain |
1 | 7.7% | 1.7% |
| Positive expectations related to less pain |
8 | 61.5% | 13.3% | |
| Positive expectations related to greater pain |
1 | 7.7% | 1.7% | |
| No correlation between expectations and pain |
3 | 23.1% | 5% | |
| Did not assess pain | 47 | N/A | 78.3% | |
Satisfaction
There were 36 studies (6,722 patients) that investigated the relationship between patient expectations and patient satisfaction 23,25-59. Nine studies used a single question to evaluate satisfaction such as: “How do you feel about the result of your surgery?” Five studies used ad hoc questionnaires composed of multiple questions regarding satisfaction. For example, Brandberg et al. 27 used a series of 7-point scales to ask women undergoing breast reconstruction what their satisfaction was regarding breast size, softness, shape, and scarring.
Eighteen studies (2,079 patients) identified that fulfillment of expectations was associated with greater satisfaction. For example, Noble et al. 46 measured expectation fulfillment in knee arthroplasty patients. They found that satisfaction was highly related to fulfillment of expectations, specifically regarding activity level. Satisfaction was also related to the level of preoperative expectations. In nine studies (1,627 patients), positive preoperative expectations correlated with postoperative satisfaction. For example, De Groot et al. 29 used semi-structured interviews to measure expectations regarding pain, length of recovery, and return to work. Patients who expected more pain and a more difficult recovery were less satisfied compared with patients with expectations of an easier recovery. In contrast, eight studies (1,071 patients) found that patients with positive preoperative expectations were more likely to be dissatisfied following surgery. For example, in a study on 180 patients undergoing total hip arthroplasty, Mancuso et al. 60 found that patients who expected to be highly active following surgery, such as engaging in sports, dancing, travelling, and hiking, reported greater dissatisfaction. Five studies (2,678 patients) did not find a correlation between expectations and postoperative satisfaction among patients undergoing knee arthroplasty, hip replacement, and bariatric surgery.
Quality of Life
We identified 19 studies (5,209 patients) that examined the effect of patient expectations on postoperative quality of life (QOL) 23,26,28,32,58,61-74. Thirteen studies assessed QOL using the Short Form-36 (SF-36) questionnaire, a generic health status survey that captures pain, disability, and psychosocial outcomes. Two studies used the EQ5D questionnaire, a standardized instrument that assesses mobility, self-care, usual activities, pain, anxiety, and depression 63,65. The Schedule for the Evaluation of Individual Quality of Life questionnaire, which includes 5 visual analog-based measures regarding quality of life, was used in 1 study of 57 patients undergoing lumbar spine surgery 73. The Nottingham Health Profile (NHP) was used to examine QOL among 398 patients undergoing prostatectomy 64. The NHP is composed of 38 questions grouped into six domains including sleeping difficulties, energy levels, emotional reactions, pain, problems with mobility, and social interactions 64. One study on patients undergoing liver transplant surgery used the Sickness Impact Profile (SIP), composed of 136 items regarding physical factors, psychosocial factors, and independence 68. Two studies in patients undergoing heart transplant and total hip arthroplasty used ad hoc surveys to measure QOL 28,70.
Ten studies (2,624 patients) found that positive preoperative expectations were correlated with greater QOL following surgery. For example, in a study of 125 patients undergoing rotator cuff repair, Henn et al. 67 identified a positive correlation between overall pre-operative expectations and postoperative QOL as measured by the SF-36 and visual analog scales. Four studies (1,395 patients) found that the fulfillment of preoperative patient expectations was associated with greater postoperative QOL. For example, in a study of 881 patients undergoing total joint replacement of the knee or hip, Gonzalez et al. 65 found that patients whose expectations were fulfilled reported higher QOL as measured by the SF-12 and EuroQOL. Six studies (809 patients) did not find a correlation between preoperative expectations and QOL among patients undergoing total hip arthroplasty, total knee arthroplasty, and prostatectomy.
Disability
Twenty four studies (8,844 patients) measured outcomes using disability, including measurements of function, mobility, symptom frequency, and activity limitation 23,26,28,32,36,37,40,50,58,60,62-64,66,67,70-72,75-80. The most common instrument used to measure disability was the Western Ontario and McMaster Universities Arthritis Index (WOMAC), which was used in 7 studies in patients undergoing either hip or knee arthroplasty 26,32,40,62,66,71,77. The WOMAC is a 24-item questionnaire used for measuring outcomes in patients with arthritis of the knee and hip that has 17 questions regarding functional limitation 81. Two studies on patients undergoing rotator cuff repair and carpal tunnel release surgery used the Disabilities of the Arm, Shoulder and Hand questionnaire (DASH), a 30-item instrument that captures upper extremity disability36,67,82. The Oswestry Disability Index was used in 2 studies on patients undergoing lumbar and cervical spine surgery 23,58. This index measures functional ability and pain among patients with lower back conditions 83.
Fifteen studies (6,789 patients) found that positive preoperative expectations were correlated with better functional outcomes. For example, in a study of 908 patients undergoing total hip replacement, patients with higher preoperative expectations had better WOMAC scores in the functional and stiffness domains 77. Additionally, four studies found that fulfillment of expectations was associated with lower disability scores following surgery. For example, in a study of 487 patients undergoing total hip arthroplasty, fulfillment of preoperative expectations was correlated with higher postoperative Lower Limb Core score 24. One study in patients undergoing colorectal surgery found that patients with high expectations had worse postoperative disability. This study found that patients with high expectations had higher postoperative fatigue79. Five studies found no relationship between preoperative expectations and postoperative disability among patients undergoing total hip arthroplasty, total knee arthroplasty, carpal tunnel release, and lumbar disc decompression.
Mood disorders
Five studies (702 patients) measured postoperative mood disorders including depression, anxiety, anger, and mental distress 39,61,69,70,84. Three of these studies used validated questionnaires. Chunta et al. 61 used the Hospital Anxiety and Depression Scale (HADS), a 14-item instrument, to measure anxiety and depression in 54 patients undergoing open heart surgery85. Leedham et al. 70 used the Profile of Mood States Scale (POMS), a 44-item instrument, to measure overall mood disturbance in 31 patients undergoing heart transplant surgery 86. Wallace et al. 84 used the State Anxiety Scale, a 20-item instrument, to measure fear in a group of 121 patients undergoing laparoscopic surgery for infertility investigation 87. The remaining two studies on patients undergoing hematopoietic stem cell transplant and coronary artery bypass surgery used ad hoc questionnaires to measure depression and anxiety 39,69.
In three studies (206 patients), positive preoperative expectations were associated with a lower rate of mood disturbance. For example, Leedham et al. 70 found that patients undergoing heart transplantation who were more positive preoperatively had lower postoperative POMS scores. However, among 183 patients undergoing coronary artery bypass grafting (CABG) surgery, patients with positive preoperative expectations were more likely to experience anger and depression following surgery 39. Finally, there was no correlation between preoperative expectation and postoperative mood disturbance among patients undergoing hematopoietic stem cell transplantation, and patients with high expectations had similar depressive symptoms compared with patients with low expectations 69.
Pain
Thirteen studies (3,523 patients) examined the relationship between preoperative expectations and postoperative pain 26,28,37,40,43,62,65-67,71,77,84,88. Seven studies in patients undergoing hip arthroplasty and knee arthroplasty measured pain using the WOMAC questionnaire. Three studies in patients undergoing hip arthroplasty, colonoscopy, and rotator cuff repair used visual analogue scales to measure pain. Three studies in patients undergoing laparoscopic surgery for infertility investigation, orthognathic surgery, and lumbar disc decompression surgery used ad hoc instruments 37,78,84.
In eight studies (2,288 patients), positive expectations were correlated with lower postoperative pain scores. For example, in a study of 598 patients undergoing total knee arthroplasty, patients who expected minimal postoperative pain reported less pain as measured by WOMAC scores compared with patients who expected severe postoperative pain 40. In contrast, one study (106 patients) found that high preoperative expectations were related to greater postoperative pain among hip replacement patients 62. One study found that in a cohort of 881 patients, those who had their expectations fulfilled had lower pain scores 65. Three studies did not find a correlation between expectations and postoperative pain scores. For example, in a study of 60 patients undergoing total hip arthroplasty, patients with higher expectations reported similar WOMAC pain scores compared with patients with lower preoperative expectations 66.
DISCUSSION
In this systematic review, preoperative expectations were inconsistently correlated with postoperative PROs following surgery. In the majority of studies, positive expectations were correlated with improved PROs, even if expectations were not completely met. However, a large proportion of studies reported worse PROs with fulfillment of expectations, and 20% failed to identify any relationship between PROs and patient expectations. Finally, there are few validated methods by which patient expectations are captured perioperatively, and wide variation exists in the types of instruments used to gather this data.
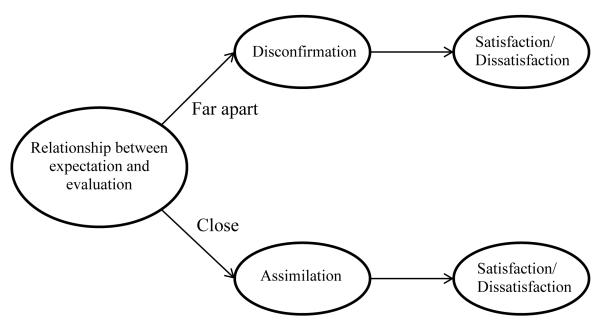
Previous research in consumer marketing provides insight into the mechanisms by which patient expectations could influence postoperative experiences. For example, the expectancy-discrepancy theory postulates that expectations create a point of reference for an individual to evaluate an event (Figure 2) 89. When an outcome meets or exceeds expectations, an individual is satisfied. Although we observed a correlation between fulfillment of expectations and higher satisfaction for some procedures, this theory may not fully explain the relationship between expectations and PROs for all patients. The assimilation-contrast theory suggests that an individual’s evaluation of a service is affected by their expectations 90. For example, when an individual’s evaluation of the event is close to their expectations, the patient will adjust their evaluation to match their preoperative expectation (this is called assimilation). Conversely, when their experience does not match their expectations, the individual emphasizes this difference (contrast), which may be negative or positive (Figure 4) 91. Although these theories have been described for consumers, they are also relevant for patients facing complex health-care decisions and invasive procedures.
Fig. 2.
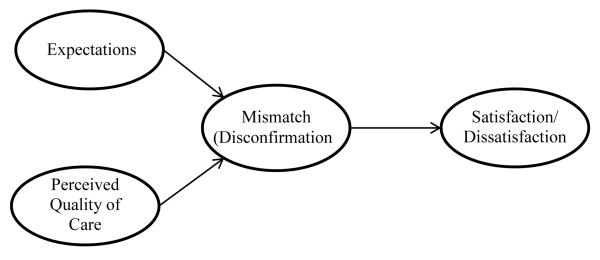
The Expectancy-discrepancy model. Expectations form a point of reference for the patient to evaluate the procedure. If the evaluation (perceived quality of care) is better than expected, there is positive a positive mismatch (positive disconfirmation), leading to satisfaction. If the evaluation is worse than expected, there is a negative mismatch (negative disconfirmation), leading to dissatisfaction.
Fig. 4.
A diagram of the assimilation-contrast model. When the evaluation of the procedure is far from the individual’s expectations, the patient will emphasize the mismatch between their expectations and their evaluation (disconfirmation). When the evaluation of the procedure is close to expectations, assimilation occurs, and the individual will adjust their evaluation to be in accordance with their expectations.
For many conditions, several treatment options may exist with different risks, benefits, and costs associated with each choice. For example, many women with early stage breast cancer are candidates for either breast-conserving surgery with radiation or mastectomy for local tumor control 92. Preference-sensitive care describes treatment in which the decision for a specific therapy should reflect patients’ personal values and preferences, and relies on an informed patient reaching their decision with their physician 93. Despite the recent explosion of healthcare information readily available through advances in information and computer technology, patient knowledge of their health status and understanding of surgical procedures remains uniformly low94,95. For example, less than 50% of women who undergo surgery for breast cancer are aware of differences in local recurrence rates and survival between lumpectomy and mastectomy 96. These knowledge gaps not only contribute to inaccurate patient expectations, but may also undermine patient decision-making for preference-sensitive conditions.
Our study has several limitations. First, there was significant heterogeneity in the methods used to assess, quantify, and report preoperative expectations and postoperative PROs. These differences limited our ability to quantify the association between expectations and PROs across studies. Furthermore, although we relied on standard Medical Subject Heading (MeSH) terms, our accuracy is limited to how precisely the articles within search engines were indexed by these specific terms. Additional unpublished work or studies published in languages other than English were not included in this review, which may have biased our results. Finally, the majority of studies that were included in this review were observational, and we cannot comment on causality of our findings.
Despite these limitations, this study represents an first step to synthesize the literature regarding the methods available to assess patient expectations and their influence on PROs. For surgeons in practice, defining patient expectations at the time of surgical-decision making can potentially improve the process of informed consent and prepare patients for their postoperative recovery and the possibility of complications and setbacks. Decision support tools, such as informational booklets, photographs, and educational videos, can enhance communication between surgeons and patients and improve patient knowledge regarding their conditions and treatment options 97. For researchers and policy-makers, developing accurate and relevant decision support systems that can be easily implemented in clinical settings can improve the quality of physician consultations and enhance patient satisfaction with their care. Furthermore, few instruments exist to capture patient expectations, and the majority are tailored to specific conditions. Generic item instruments, such as the Patient Reported Outcome Measurement Information System (PROMIS), can capture self-reported health status, and provide a common metric across a variety of conditions.98,99 Similar principles could be applied to measure patient expectations in a comparable and efficient way. Attention to capturing patient expectations and optimizing decision quality for patients facing surgery can ultimately minimize unwarranted variation for preference-sensitive conditions 100.
Given recent national interest in utilizing PROs as indicators of healthcare quality, defining the effect of patient expectations on PROs after surgery is essential in order to improve patient experiences following surgery and enhance communication between surgeons and their patients. Future studies that examine patient expectations longitudinally and identify those factors that influence expectations will deepen our understanding of the complex relationship between patient perception and postoperative recovery.
Supplementary Material
Fig. 3.
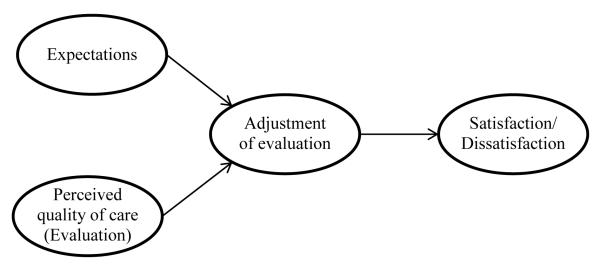
The Assimilation model. If the individual’s perceived quality of care is different from what they expected, they will adjust their evaluation to be closer to their expectation. The adjusted evaluation then leads to satisfaction or dissatisfaction with the procedure.
Table 3.
Expectations and objective outcomes in surgery patients.
| Expectation/outcome relationship |
Number of studies |
Percentage of studies in subgroup |
Percentage of all studies included in the review |
|---|---|---|---|
| Fulfillment of expectations related to improved objective outcomes |
6 | 75% | 10% |
| Positive expectations related to improved objective outcomes |
2 | 25% | 3.3% |
| Positive expectations related to worse objective outcomes |
0 | 0% | 0% |
| No correlation between expectations and objective outcomes |
0 | 0% | 0% |
Acknowledgments
Supported in part by grants from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (2R01 AR047328-06) National Institute of Arthritis and Musculoskeletal and Skin Diseases and National Institute on Aging (R01 AR062066) and a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) (To Dr. Kevin C. Chung).
References
- 1.Institute of Medicine (U.S.) Crossing the quality chasm : a new health system for the 21st century. National Academy Press; Washington, D.C.: 2001. Committee on Quality of Health Care in America. [PubMed] [Google Scholar]
- 2.Prioritization IoMCoCER . Initial National Priorities for Comparative Effectiveness Research. The National Academies Press; Washington, D.C.: 2009. [Google Scholar]
- 3.Birkmeyer JD, Gust C, Baser O, Dimick JB, Sutherland JM, Skinner JS. Medicare payments for common inpatient procedures: implications for episode-based payment bundling. Health Serv Res. 2010 Dec;45(6 Pt 1):1783–1795. doi: 10.1111/j.1475-6773.2010.01150.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kohn LT, Corrigan J, Donaldson MS, Institute of Medicine (U.S.) To err is human building a safer health system. National Academy Press; Washington, D.C.: 1999. Committee on Quality of Health Care in America. http://www.nap.edu/books/0309068371/html/ [PubMed] [Google Scholar]
- 5.Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002 Apr 11;346(15):1128–1137. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 6.Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003 Nov 27;349(22):2117–2127. doi: 10.1056/NEJMsa035205. [DOI] [PubMed] [Google Scholar]
- 7.Birkmeyer JD, Dimick JB, Birkmeyer NJ. Measuring the quality of surgical care: structure, process, or outcomes? J Am Coll Surg. 2004 Apr;198(4):626–632. doi: 10.1016/j.jamcollsurg.2003.11.017. [DOI] [PubMed] [Google Scholar]
- 8.Brook RH. Can the Patient-Centered Outcomes Research Institute become relevant to controlling medical costs and improving value? Jama. 2011 Nov 9;306(18):2020–2021. doi: 10.1001/jama.2011.1621. [DOI] [PubMed] [Google Scholar]
- 9.Laine C, Davidoff F. Patient-centered medicine. A professional evolution. Jama. 1996 Jan 10;275(2):152–156. [PubMed] [Google Scholar]
- 10.Rao JK, Weinberger M, Kroenke K. Visit-specific expectations and patient-centered outcomes: a literature review. Arch Fam Med. 2000 Nov-Dec;9(10):1148–1155. doi: 10.1001/archfami.9.10.1148. [DOI] [PubMed] [Google Scholar]
- 11.Waljee JF, Ubel PA, Atisha DM, Hu ES, Alderman AK. The Choice for Breast Cancer Surgery: Can Women Accurately Predict Postoperative Quality of Life and Disease-Related Stigma? Ann Surg Oncol. 2011 Sep;18(9):2477–2482. doi: 10.1245/s10434-011-1582-x. [DOI] [PubMed] [Google Scholar]
- 12.Ubel PA, Loewenstein G, Jepson C. Disability and sunshine: can hedonic predictions be improved by drawing attention to focusing illusions or emotional adaptation? Journal of experimental psychology. Applied. 2005 Jun;11(2):111–123. doi: 10.1037/1076-898X.11.2.111. [DOI] [PubMed] [Google Scholar]
- 13.Damschroder LJ, Zikmund-Fisher BJ, Ubel PA. The impact of considering adaptation in health state valuation. Social science & medicine. 2005 Jul;61(2):267–277. doi: 10.1016/j.socscimed.2004.11.060. [DOI] [PubMed] [Google Scholar]
- 14.Smith D, Loewenstein G, Jepson C, Jankovich A, Feldman H, Ubel P. Mispredicting and misremembering: patients with renal failure overestimate improvements in quality of life after a kidney transplant. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 2008 Sep;27(5):653–658. doi: 10.1037/a0012647. [DOI] [PubMed] [Google Scholar]
- 15.Smith DM, Sherriff RL, Damschroder L, Loewenstein G, Ubel PA. Misremembering colostomies? Former patients give lower utility ratings than do current patients. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 2006 Nov;25(6):688–695. doi: 10.1037/0278-6133.25.6.688. [DOI] [PubMed] [Google Scholar]
- 16.Smith DM, Loewenstein G, Rozin P, Sherriff RL, Ubel PA. Sensitivity to disgust, stigma, and adjustment to life with a colostomy. Journal of research in personality. 2007 Aug;41(4):787–803. doi: 10.1016/j.jrp.2006.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ram AN, Curtin CM, Chung KC. Population-based utilities for upper extremity functions in the setting of tetraplegia. J Hand Surg Am. 2009 Nov;34(9):1674–1681. e1671. doi: 10.1016/j.jhsa.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilson KA, Dowling AJ, Abdolell M, Tannock IF. Perception of quality of life by patients, partners and treating physicians. Qual Life Res. 2000;9(9):1041–1052. doi: 10.1023/a:1016647407161. [DOI] [PubMed] [Google Scholar]
- 19.Brown LK, Waljee AK, Higgins PD, Waljee JF, Morris AM. Proximity to disease and perception of utility: physicians’ vs patients’ assessment of treatment options for ulcerative colitis. Diseases of the colon and rectum. 2011 Dec;54(12):1529–1536. doi: 10.1097/DCR.0b013e31823436a8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boyd NF, Sutherland HJ, Heasman KZ, Tritchler DL, Cummings BJ. Whose utilities for decision analysis? Med Decis Making. 1990 Jan-Mar;10(1):58–67. doi: 10.1177/0272989X9001000109. [DOI] [PubMed] [Google Scholar]
- 21.Rozenblum R, Lisby M, Hockey PM, et al. Uncovering the blind spot of patient satisfaction: an international survey. BMJ Qual Saf. 2011 Nov;20(11):959–965. doi: 10.1136/bmjqs-2011-000306. [DOI] [PubMed] [Google Scholar]
- 22.Harris RP, Helfand M, Woolf SH, et al. Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med. 2001 Apr;20(3 Suppl):21–35. doi: 10.1016/s0749-3797(01)00261-6. [DOI] [PubMed] [Google Scholar]
- 23.Soroceanu A, Ching A, Abdu W, McGuire K. Relationship between preoperative expectations, satisfaction, and functional outcomes in patients undergoing lumbar and cervical spine surgery: a multicenter study. Spine. 2012 Jan 15;37(2):E103–108. doi: 10.1097/BRS.0b013e3182245c1f. [DOI] [PubMed] [Google Scholar]
- 24.Mancuso CA, Sculco TP, Wickiewicz TL, et al. Patients’ expectations of knee surgery. J Bone Joint Surg Am. 2001 Jul;83-A(7):1005–1012. doi: 10.2106/00004623-200107000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Addisu Z, Solomon B. Patients’ preoperative expectation and outcome of cataract surgery at jimma university specialized hospital -department of ophthalmology. Ethiopian Journal of Health Sciences. 2011 Mar;21(1):47–55. doi: 10.4314/ejhs.v21i1.69044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Becker R, Doring C, Denecke A, Brosz M. Expectation, satisfaction and clinical outcome of patients after total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy. 2011 Sep;19(9):1433–1441. doi: 10.1007/s00167-011-1621-y. [DOI] [PubMed] [Google Scholar]
- 27.Brandberg Y, Arver B, Johansson H, Wickman M, Sandelin K, Liljegren A. Less correspondence between expectations before and cosmetic results after risk-reducing mastectomy in women who are mutation carriers: a prospective study. European Journal of Surgical Oncology. 2012 Jan;38(1):38–43. doi: 10.1016/j.ejso.2011.10.010. [DOI] [PubMed] [Google Scholar]
- 28.Burton KE, Wright V, Richards J. Patients’ expectations in relation to outcome of total hip replacment surgery. Annals of the Rheumatic Diseases. 1979 Oct;38(5):471–474. doi: 10.1136/ard.38.5.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Groot KI, Boeke S, Passchier J. Preoperative expectations of pain and recovery in relation to postoperative disappointment in patients undergoing lumbar surgery. Med Care. 1999 Feb;37(2):149–156. doi: 10.1097/00005650-199902000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Eisler T, Svensson O, Tengstrom A, Elmstedt E. Patient expectation and satisfaction in revision total hip arthroplasty. Journal of Arthroplasty. 2002 Jun;17(4):457–462. doi: 10.1054/arth.2002.31245. [DOI] [PubMed] [Google Scholar]
- 31.Finlay PM, Atkinson JM, Moos KF. Orthognathic surgery: patient expectations; psychological profile and satisfaction with outcome. British Journal of Oral & Maxillofacial Surgery. 1995 Feb;33(1):9–14. doi: 10.1016/0266-4356(95)90078-0. [DOI] [PubMed] [Google Scholar]
- 32.Gandhi R, Davey JR, Mahomed N. Patient expectations predict greater pain relief with joint arthroplasty. Journal of Arthroplasty. 2009 Aug;24(5):716–721. doi: 10.1016/j.arth.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 33.Gepstein R, Arinzon Z, Adunsky A, Folman Y. Decompression surgery for lumbar spinal stenosis in the elderly: preoperative expectations and postoperative satisfaction. Spinal Cord. 2006 Jul;44(7):427–431. doi: 10.1038/sj.sc.3101857. [DOI] [PubMed] [Google Scholar]
- 34.Haworth RJ, Hopkins J, Ells P, Ackroyd CE, Mowat AG. Expectations and outcome of total hip replacement. Rheumatology & Rehabilitation. 1981 May;20(2):65–70. doi: 10.1093/rheumatology/20.2.65. [DOI] [PubMed] [Google Scholar]
- 35.Iversen MD, Daltroy LH, Fossel AH, Katz JN. The prognostic importance of patient pre-operative expectations of surgery for lumbar spinal stenosis. Patient Education & Counseling. 1998 Jun;34(2):169–178. doi: 10.1016/s0738-3991(97)00109-2. [DOI] [PubMed] [Google Scholar]
- 36.Kadzielski J, Malhotra LR, Zurakowski D, Lee S-GP, Jupiter JB, Ring D. Evaluation of preoperative expectations and patient satisfaction after carpal tunnel release. Journal of Hand Surgery - American Volume. 2008 Dec;33(10):1783–1788. doi: 10.1016/j.jhsa.2008.06.019. [DOI] [PubMed] [Google Scholar]
- 37.Kiyak HA, Vitaliano PP, Crinean J. Patients’ expectations as predictors of orthognathic surgery outcomes. Health Psychology. 1988;7(3):251–268. doi: 10.1037//0278-6133.7.3.251. [DOI] [PubMed] [Google Scholar]
- 38.Kramer AC, Schweber A. Patient expectations prior to coloplast titan penile prosthesis implant predicts postoperative satisfaction. Journal of Sexual Medicine. 2010 Jun;7(6):2261–2266. doi: 10.1111/j.1743-6109.2010.01799.x. [DOI] [PubMed] [Google Scholar]
- 39.Lindsay GM, Smith LN, Hanlon P, Wheatley DJ. Coronary artery disease patients’ perception of their health and expectations of benefit following coronary artery bypass grafting. Journal of Advanced Nursing. 2000 Dec;32(6):1412–1421. doi: 10.1046/j.1365-2648.2000.01621.x. [DOI] [PubMed] [Google Scholar]
- 40.Lingard EA, Sledge CB, Learmonth ID, Kinemax Outcomes G. Patient expectations regarding total knee arthroplasty: differences among the United States, United kingdom, and Australia. Journal of Bone & Joint Surgery - American Volume. 2006 Jun;88(6):1201–1207. doi: 10.2106/JBJS.E.00147. [DOI] [PubMed] [Google Scholar]
- 41.Lutz GK, Butzlaff ME, Atlas SJ, Keller RB, Singer DE, Deyo RA. The relation between expectations and outcomes in surgery for sciatica. J Gen Intern Med. 1999 Dec;14(12):740–744. doi: 10.1046/j.1525-1497.1999.10417.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mancuso CA, Salvati EA, Johanson NA, Peterson MG, Charlson ME. Patients’ expectations and satisfaction with total hip arthroplasty. Journal of Arthroplasty. 1997 Jun;12(4):387–396. doi: 10.1016/s0883-5403(97)90194-7. [DOI] [PubMed] [Google Scholar]
- 43.Mannion AF, Kampfen S, Munzinger U, Kramers-de Quervain I. The role of patient expectations in predicting outcome after total knee arthroplasty. Arthritis Res Ther. 2009;11(5):R139. doi: 10.1186/ar2811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McGregor AH, Hughes SPF. The evaluation of the surgical management of nerve root compression in patients with low back pain: Part 2: patient expectations and satisfaction. Spine. 2002 Jul 1;27(13):1471–1476. doi: 10.1097/00007632-200207010-00019. discussion 1476-1477. [DOI] [PubMed] [Google Scholar]
- 45.Nilsdotter AK, Toksvig-Larsen S, Roos EM. Knee arthroplasty: are patients’ expectations fulfilled? A prospective study of pain and function in 102 patients with 5-year follow-up. Acta Orthopaedica. 2009 Feb;80(1):55–61. doi: 10.1080/17453670902805007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clinical Orthopaedics & Related Research. 2006 Nov;452:35–43. doi: 10.1097/01.blo.0000238825.63648.1e. [DOI] [PubMed] [Google Scholar]
- 47.Olson RE, Laskin DM. Expectations of patients from orthognathic surgery. Journal of Oral Surgery. 1980 Apr;38(4):283–285. [PubMed] [Google Scholar]
- 48.Ostler S, Kiyak HA. Treatment expectations versus outcomes among orthognathic surgery patients. International Journal of Adult Orthodontics & Orthognathic Surgery. 1991;6(4):247–255. [PubMed] [Google Scholar]
- 49.Pager CK. Expectations and outcomes in cataract surgery: a prospective test of 2 models of satisfaction. Archives of Ophthalmology. 2004 Dec;122(12):1788–1792. doi: 10.1001/archopht.122.12.1788. [DOI] [PubMed] [Google Scholar]
- 50.Ronnberg K, Lind B, Zoega B, Halldin K, Gellerstedt M, Brisby H. Patients’ satisfaction with provided care/information and expectations on clinical outcome after lumbar disc herniation surgery. Spine. 2007 Jan 15;32(2):256–261. doi: 10.1097/01.brs.0000251876.98496.52. [DOI] [PubMed] [Google Scholar]
- 51.Singh A, Kendal A, Trivedi D, Cazabon S. Patient expectation and satisfaction after macular hole surgery. Optometry & Vision Science. 2011 Feb;88(2):312–316. doi: 10.1097/OPX.0b013e3182058fc0. [DOI] [PubMed] [Google Scholar]
- 52.Snell L, McCarthy C, Klassen A, et al. Clarifying the expectations of patients undergoing implant breast reconstruction: a qualitative study. Plast Reconstr Surg. 2010 Dec;126(6):1825–1830. doi: 10.1097/PRS.0b013e3181f44580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Toyone T, Tanaka T, Kato D, Kaneyama R, Otsuka M. Patients’ expectations and satisfaction in lumbar spine surgery. Spine. 2005 Dec 1;30(23):2689–2694. doi: 10.1097/01.brs.0000187876.14304.15. [DOI] [PubMed] [Google Scholar]
- 54.Velanovich V, Kamolz T, Pointner R, Contini S. Qualitative analysis of the expectations of antireflux surgical outcomes of patients from different nationalities. Diseases of the Esophagus. 2006;19(2):88–93. doi: 10.1111/j.1442-2050.2006.00546.x. [DOI] [PubMed] [Google Scholar]
- 55.Wheelock I, Peterson C, Buchtel HA. Presurgery expectations, postsurgery satisfaction, and psychosocial adjustment after epilepsy surgery. Epilepsia. 1998 May;39(5):487–494. doi: 10.1111/j.1528-1157.1998.tb01410.x. [DOI] [PubMed] [Google Scholar]
- 56.Wilson SJ, Saling MM, Kincade P, Bladin PF. Patient expectations of temporal lobe surgery. Epilepsia. 1998 Feb;39(2):167–174. doi: 10.1111/j.1528-1157.1998.tb01354.x. [DOI] [PubMed] [Google Scholar]
- 57.Wilson SJ, Saling MM, Lawrence J, Bladin PF. Outcome of temporal lobectomy: expectations and the prediction of perceived success. Epilepsy Research. 1999 Aug;36(1):1–14. doi: 10.1016/s0920-1211(99)00016-9. [DOI] [PubMed] [Google Scholar]
- 58.Yee A, Adjei N, Do J, Ford M, Finkelstein J. Do patient expectations of spinal surgery relate to functional outcome? Clinical Orthopaedics & Related Research. 2008 May;466(5):1154–1161. doi: 10.1007/s11999-008-0194-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zijlstra H, Larsen JK, de Ridder DTD, van Ramshorst B, Geenen R. Initiation and maintenance of weight loss after laparoscopic adjustable gastric banding. The role of outcome expectation and satisfaction with the psychosocial outcome. Obesity Surgery. 2009 Jun;19(6):725–731. doi: 10.1007/s11695-008-9572-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mancuso CA, Jout J, Salvati EA, Sculco TP. Fulfillment of patients’ expectations for total hip arthroplasty. Journal of Bone & Joint Surgery - American Volume. 2009 Sep;91(9):2073–2078. doi: 10.2106/JBJS.H.01802. [DOI] [PubMed] [Google Scholar]
- 61.Chunta KS. Expectations, anxiety, depression, and physical health status as predictors of recovery in open-heart surgery patients. Journal of Cardiovascular Nursing. 2009 Nov-Dec;24(6):454–464. doi: 10.1097/JCN.0b013e3181ac8a3c. [DOI] [PubMed] [Google Scholar]
- 62.Cross M, Lapsley H, Barcenilla A, Parker D, Coolican M, March L. Patient expectations of hip and knee joint replacement surgery and postoperative health status. The Patient: Patient-Centered Outcomes Research. 2009 Mar 1;2(1):51–60. doi: 10.2165/01312067-200902010-00006. [DOI] [PubMed] [Google Scholar]
- 63.Davidge K, Bell R, Ferguson P, Turcotte R, Wunder J, Davis AM. Patient expectations for surgical outcome in extremity soft tissue sarcoma. Journal of Surgical Oncology. 2009 Oct 1;100(5):375–381. doi: 10.1002/jso.21301. [DOI] [PubMed] [Google Scholar]
- 64.Flood AB, Lorence DP, Ding J, McPherson K, Black NA. The role of expectations in patients’ reports of post-operative outcomes and improvement following therapy. Med Care. 1993 Nov;31(11):1043–1056. doi: 10.1097/00005650-199311000-00006. [DOI] [PubMed] [Google Scholar]
- 65.Gonzalez Saenz de Tejada M, Escobar A, Herrera C, Garcia L, Aizpuru F, Sarasqueta C. Patient expectations and health-related quality of life outcomes following total joint replacement. Value in Health. 2010 Jun-Jul;13(4):447–454. doi: 10.1111/j.1524-4733.2009.00685.x. [DOI] [PubMed] [Google Scholar]
- 66.Haddad FS, Garbuz DS, Chambers GK, Jagpal TJ, Masri BA, Duncan CP. The expectations of patients undergoing revision hip arthroplasty. Journal of Arthroplasty. 2001 Jan;16(1):87–91. doi: 10.1054/arth.2001.17937. [DOI] [PubMed] [Google Scholar]
- 67.Henn RF, 3rd, Kang L, Tashjian RZ, Green A. Patients’ preoperative expectations predict the outcome of rotator cuff repair. Journal of Bone & Joint Surgery - American Volume. 2007 Sep;89(9):1913–1919. doi: 10.2106/JBJS.F.00358. [DOI] [PubMed] [Google Scholar]
- 68.Holzner B, Kemmler G, Kopp M, et al. Preoperative expectations and postoperative quality of life in liver transplant survivors. Archives of Physical Medicine & Rehabilitation. 2001 Jan;82(1):73–79. doi: 10.1053/apmr.2001.19013. [DOI] [PubMed] [Google Scholar]
- 69.Lee SJ, Loberiza FR, Rizzo JD, Soiffer RJ, Antin JH, Weeks JC. Optimistic expectations and survival after hematopoietic stem cell transplantation. Biology of Blood & Marrow Transplantation. 2003 Jun;9(6):389–396. doi: 10.1016/s1083-8791(03)00103-4. [DOI] [PubMed] [Google Scholar]
- 70.Leedham B, Meyerowitz BE, Muirhead J, Frist WH. Positive expectations predict health after heart transplantation. Health Psychology. 1995 Jan;14(1):74–79. doi: 10.1037//0278-6133.14.1.74. [DOI] [PubMed] [Google Scholar]
- 71.Mahomed NN, Liang MH, Cook EF, et al. The importance of patient expectations in predicting functional outcomes after total joint arthroplasty. Journal of Rheumatology. 2002 Jun;29(6):1273–1279. [PubMed] [Google Scholar]
- 72.Oh JH, Yoon JP, Kim JY, Kim SH. Effect of expectations and concerns in rotator cuff disorders and correlations with preoperative patient characteristics. Journal of Shoulder & Elbow Surgery. 2012 Jun;21(6):715–721. doi: 10.1016/j.jse.2011.10.017. [DOI] [PubMed] [Google Scholar]
- 73.Saban KL, Penckofer SM. Patient expectations of quality of life following lumbar spinal surgery. Journal of Neuroscience Nursing. 2007 Jun;39(3):180–189. doi: 10.1097/01376517-200706000-00009. [DOI] [PubMed] [Google Scholar]
- 74.Sears SF, Serber ER, Lewis TS, et al. Do positive health expectations and optimism relate to quality-of-life outcomes for the patient with an implantable cardioverter defibrillator? Journal of Cardiopulmonary Rehabilitation. 2004 Sep-Oct;24(5):324–331. doi: 10.1097/00008483-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 75.Barefoot JC, Brummett BH, Williams RB, et al. Recovery expectations and long-term prognosis of patients with coronary heart disease. Arch Intern Med. 2011 May 23;171(10):929–935. doi: 10.1001/archinternmed.2011.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Borkan JM, Quirk M. Expectations and outcomes after hip fracture among the elderly. International Journal of Aging & Human Development. 1992;34(4):339–350. doi: 10.2190/4KLB-5CM4-1RRX-3U4U. [DOI] [PubMed] [Google Scholar]
- 77.Judge A, Cooper C, Arden NK, et al. Pre-operative expectation predicts 12-month post operative outcome among patients undergoing primary total hip replacement in European orthopaedic centres. Osteoarthritis & Cartilage. 2011 Jun;19(6):659–667. doi: 10.1016/j.joca.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 78.Mannion AF, Junge A, Elfering A, Dvorak J, Porchet F, Grob D. Great expectations: really the novel predictor of outcome after spinal surgery? Spine. 2009 Jul 1;34(15):1590–1599. doi: 10.1097/BRS.0b013e31819fcd52. [DOI] [PubMed] [Google Scholar]
- 79.Paddison JS, Booth RJ, Cameron LD, Robinson E, Frizelle FA, Hill AG. Fatigue after colorectal surgery and its relationship to patient expectations. Journal of Surgical Research. 2009 Jan;151(1):145–152. doi: 10.1016/j.jss.2008.01.030. [DOI] [PubMed] [Google Scholar]
- 80.Suda AJ, Seeger JB, Bitsch RG, Krueger M, Clarius M. Are patients’ expectations of hip and knee arthroplasty fulfilled? A prospective study of 130 patients. Orthopedics. 2010 Feb;33(2):76–80. doi: 10.3928/01477447-20100104-07. [DOI] [PubMed] [Google Scholar]
- 81.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988 Dec;15(12):1833–1840. [PubMed] [Google Scholar]
- 82.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996 Jun;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 83.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976) 2000 Nov 15;25(22):2940–2952. doi: 10.1097/00007632-200011150-00017. discussion 2952. [DOI] [PubMed] [Google Scholar]
- 84.Wallace LM. Surgical patients’ expectations of pain and discomfort: does accuracy of expectations minimise post-surgical pain and distress? Pain. 1985 Aug;22(4):363–373. doi: 10.1016/0304-3959(85)90042-9. [DOI] [PubMed] [Google Scholar]
- 85.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983 Jun;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 86.Scheier MF, Carver CS. Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health Psychology. 1985;4(3):219–247. doi: 10.1037//0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- 87.Bieling PJ, Antony MM, Swinson RP. The State-Trait Anxiety Inventory, Trait version: structure and content re-examined. Behav Res Ther. 1998 Jul-Aug;36(7-8):777–788. doi: 10.1016/s0005-7967(98)00023-0. [DOI] [PubMed] [Google Scholar]
- 88.Gavaruzzi T, Carnaghi A, Lotto L, et al. Recalling pain experienced during a colonoscopy: pain expectation and variability. British Journal of Health Psychology. 2010 May;15(Pt 2):253–264. doi: 10.1348/135910709X458305. [DOI] [PubMed] [Google Scholar]
- 89.Oliver RL. A Cognitive Model of the Antecedents and Consequences of Satisfaction Decisions. J Marketing Res. 1980;17(4):460–469. [Google Scholar]
- 90.Anderson RE. Consumer Dissatisfaction - Effect of Disconfirmed Expectancy on Perceived Product Performance. J Marketing Res. 1973;10(1):38–44. [Google Scholar]
- 91.Thompson AG, Sunol R. Expectations as determinants of patient satisfaction: concepts, theory and evidence. International Journal for Quality in Health Care. 1995 Jun;7(2):127–141. doi: 10.1093/intqhc/7.2.127. [DOI] [PubMed] [Google Scholar]
- 92.Katz SJ, Lantz PM, Janz NK, et al. Patient involvement in surgery treatment decisions for breast cancer. J Clin Oncol. 2005 Aug 20;23(24):5526–5533. doi: 10.1200/JCO.2005.06.217. [DOI] [PubMed] [Google Scholar]
- 93.Hawley ST, Lantz PM, Janz NK, et al. Factors associated with patient involvement in surgical treatment decision making for breast cancer. Patient Educ Couns. 2007 Mar;65(3):387–395. doi: 10.1016/j.pec.2006.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.O’Connor AM, Llewellyn-Thomas HA, Flood AB. Modifying unwarranted variations in health care: shared decision making using patient decision aids. Health Aff (Millwood) 2004;(Suppl Variation):VAR63–72. doi: 10.1377/hlthaff.var.63. [DOI] [PubMed] [Google Scholar]
- 95.Fagerlin A, Lakhani I, Lantz PM, et al. An informed decision? Breast cancer patients and their knowledge about treatment. Patient Educ Couns. 2006 Dec;64(1-3):303–312. doi: 10.1016/j.pec.2006.03.010. [DOI] [PubMed] [Google Scholar]
- 96.Lee CN, Chang Y, Adimorah N, et al. Decision making about surgery for early-stage breast cancer. J Am Coll Surg. 2012 Jan;214(1):1–10. doi: 10.1016/j.jamcollsurg.2011.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.O’Connor AM, Stacey D, Rovner D, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2001;3:CD001431. doi: 10.1002/14651858.CD001431. [DOI] [PubMed] [Google Scholar]
- 98.Fries J, Bruce B, Cella D. The promise of PROMIS: using item response theory to improve assessment of patient-reported outcomes. Clinical and experimental rheumatology. 2005;23(5):53. [PubMed] [Google Scholar]
- 99.Cella D, Yount S, Rothrock N, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH Roadmap cooperative group during its first two years. Med Care. 2007 May;45(5 Suppl 1):S3–S11. doi: 10.1097/01.mlr.0000258615.42478.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sepucha KR, Fowler FJ, Jr., Mulley AG., Jr. Policy support for patient-centered care: the need for measurable improvements in decision quality. Health Aff (Millwood) 2004;(Suppl Variation):VAR54–62. doi: 10.1377/hlthaff.var.54. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.