Abstract
Background
There is growing evidence of an inverse association between intelligence (IQ) and unintentional injuries.
Methods
Analyses are based on a cohort of 1,109,475 Swedish men with IQ measured in early adulthood. Men were followed-up for an average 24 years and hospital admissions for unintentional injury were recorded.
Results
198,133 (17.9%) men had at least one hospital admission for any unintentional injury during follow-up. The most common cause of unintentional injury was falling, followed by road accidents, poisoning, fire and drowning. In addition, 14,637 (1.3%) men had at least one admission for complications of medical care. After adjusting for confounding variables, lower IQ scores were associated with an elevated risk of any unintentional injury (Hazard ratio (95% confidence interval) per standard deviation decrease in IQ: 1.15 (1.14, 1.15)), and of cause-specific injuries other than drowning (poisoning (1.53 (1.49, 1.57)), fire (1.36 (1.31, 1.41)), road traffic accidents (1.25 (1.23, 1.26)), medical complications (1.20 (1.18, 1.22)), and falling (1.17 (1.16, 1.18)). These gradients were stepwise across the full IQ range.
Conclusions
Low IQ scores in early adulthood were associated with a subsequently increased risk of unintentional injury. A greater understanding of mechanisms underlying these associations may provide opportunities and strategies for prevention.
Keywords: IQ, injury, socioeconomic status, cohort
INTRODUCTION
Unintentional injuries (accidents) are a leading cause of premature mortality, morbidity and disability.(1) In people under 45 years of age injuries are more common than chronic diseases, representing a major economic burden due to increased health care costs. In spite of the public health importance, little is known about risk factors for unintentional injury. However, a small number of studies have recently identified low childhood cognitive function/intelligence (denoted IQ) as a risk factor for subsequent non-fatal injury in adulthood(2-4). Some studies have also reported inverse associations between IQ and mortality from all unintentional injuries,(5;6) road traffic accidents,(5;7) and accidental falls, poisoning, fire and drowning.(5)
Many of the existing studies have offered only modest statistical power and limited insights into the relationships between IQ and the full range of specific injury subtypes. In the present study we explore associations between IQ measured in early adulthood and subsequent hospital admissions for unintentional injury in a cohort of over one million Swedish men of whom almost two-hundred thousand had at least one hospitalisation for unintentional injury.
METHODS
Study participants and record-linkage
The record linkage used to generate this cohort has been reported previously.(8;9) The cohort comprised all non-adopted men born in Sweden from 1950 to 1976 with both biological parents identified in the Multi-Generation Register. Using unique personal identification numbers we linked this Register with the Housing Censuses records (1960 and 1970), and Military Service Conscription, Population and Cause of Death, and National Hospital Discharge Registers, resulting in 1,379,531 successful matches. Study approval was obtained from the Regional Ethics Committee, Stockholm.
Conscription examination
The military service conscription examination involves structured, standard medical assessment of physical and mental health, and cognitive function. During the years covered by this study, the law required this examination; only men of foreign citizenship or with severe disability were excused. This dataset covers examinations from 15 September 1969 to 31 December 1994, after which IQ measurement procedures changed. Average age at examination was 18.3 years (range: 16 to 25).
IQ was measured by four written subtests representing verbal, logical, spatial, and technical abilities.(10) The verbal test measures knowledge of synonyms. The logical test measures capacity to understand written instructions and apply them to problem-solving. The spatial test depicted a plan drawing of an object in its pre-assembled, two-dimensional state and required respondents to identify, from a series of drawings of fully-assembled, three-dimensional objects, which it represented. The technical test measures knowledge of chemistry and physics and implies a general knowledge component. All test scores, including a total IQ score derived from summing the subtest results, were standardized to give a Gaussian-distributed score between 1 and 9, with higher values indicating greater intellectual capacity. Standardization used for a specific conscription (calendar) year was based on the raw IQ scores during the preceding conscription years. Analyses based on the four subtests were very similar and, for brevity, the current analysis is based on total IQ score.
Childhood SES was based on the highest occupation of either parent (from 1960/1970 Population and Housing Censuses), using seven categories: non-manual (high); non-manual (intermediate); non-manual (low); farmers; skilled; unskilled; and other. Highest educational achievement (1990-2004) was also based on seven categories: primary school (<9 years); primary school (9-10 years); secondary school (≤12 years); full secondary education; university (<3 years); university (3+ years); and PhD studies. Population and Housing censuses records (1990) were used to ascertain adult SES coded as for childhood SES. Adult SES was based on own occupation for men who had an occupational code and otherwise on household SES. Blood pressure and body mass index (BMI) have been previously associated with both IQ(11;12) and unintentional injury(13;14) and were therefore included as potential confounding factors. Blood pressure, height and weight were measured by medical personnel using standard protocols and BMI was derived in the usual way (weight (kg) / height2 (m2)).
Heavy alcohol consumption and binge drinking have also been previously linked with lower IQ(15;16) and an increased risk of unintentional injury.(17;18) In addition, smoking may be a proxy measure for risk taking or poor health behaviours. Questionnaire data on smoking and alcohol consumption were collected at conscription in 1969-70 for a subgroup (3%) of men. “Risky” use of alcohol was identified(19) from at least one of: (i) consumption of 250+g 100% alcohol per week; (ii) ever consumed alcohol during a hangover; (iii) ever been apprehended for drunkenness; (iv) often been drunk.
Hospital admissions data
Hospital admissions data from 1969-2006 were based on the Swedish Hospital Discharge Register, which covered around a third of the Swedish population in 1970, rising to 71% in 1977, and 100% from 1987. The shortfall in the 1970s and 1980s occurred in counties of varying population density and socio-economic composition, and we have no reason to suppose that there was any systematic difference in IQ-injury associations in counties included and not included in the register during these early years. Admissions were coded according to the International Classification of Disease (ICD) versions 8, 9, and 10.(20-22) We identified unintentional injuries from any cause and, separately, specific subtypes of unintentional injuries with at least 200 hospital admissions during follow-up (falling, road accidents, poisoning, fire and drowning). We also examined hospital admissions for injuries due complications of medical care, which includes unintentional poisoning, unintentional cut, puncture or haemorrhage during surgical or medical care, and complications of surgical procedures. All analyses were restricted to hospital admissions occurring after conscription.
Statistical methods
Cox proportional hazards regression was used to explore IQ-unintentional injury associations having first checked that proportional hazards assumptions were not violated. As all hospital admissions were included, men could have more than one injury recorded. The main analyses were based on the first unintentional injury for any cause or for cause-specific injury. Thus, a man with two admissions for unintentional falls and one for unintentional poisoning would contribute to: (i) all unintentional injuries (first injury), (ii) unintentional falls (first falling injury), and (iii) unintentional poisoning (only poisoning injury). Follow-up began on the date of conscription and ended on the earliest of: date of injury, death, emigration, or 31 December 2006. Hazard ratios (HR) and 95% confidence intervals (CI) for all unintentional injuries combined were computed for: (i) IQ in 9 categories relative to the highest (IQ=9), and (ii) a standard deviation (SD) decrease in IQ. Analyses of cause-specific injuries were based on fewer events and HRs (95% CI) were therefore calculated for IQ in four groups (7-9, 5-6, 3-4, 1-2) to preserve statistical power and for ease of presentation across all injury endpoints.
All analyses were adjusted for conscription age. Separate models were used to adjust for childhood circumstances, based on childhood SES and adult height (although largely under genetic control, adult stature is a widely used indicator of pre-adult suboptimal nutrition and socioeconomic adversity(23)), adult SES, blood pressure and BMI. Models with multiple adjustments also included conscription centre and birth year. The effects of adjusting for educational achievement were examined separately due to its close correlation with IQ. Analyses are based on men with complete data for all variables. In the subgroup of men with appropriate data, we assessed the impact of adjusting IQ-injury associations for smoking (smoker vs. non-smoker) and alcohol (risky alcohol use vs. not).
One concern with identifying unintentional injuries from routinely coded hospital discharge data is that some injuries might, in reality, have been attempted suicides. We therefore repeated the main analyses excluding men with any hospital discharge for intentional (suicide) injuries. Moreover, psychiatric illness has been linked with both injury mortality(24) and IQ,(10;25) making it a plausible confounder or mediator of IQ-unintentional injury associations and we therefore also repeated the main analyses (a) excluding men with pre-conscription hospital discharges for psychiatric illness (ICD 8/9 codes: 290-319), and (b) in the full cohort, adjusting for concurrent psychiatric discharges during follow-up. In further analyses we excluded men with a pre-conscription hospital discharge for any injury to addresses the possibility that men prone to injuries might have had a pre-conscription head injury, detrimentally affecting their performance on the conscription IQ test, and increasing their likelihood of subsequent injury. Finally, our main analyses were based on the first unintentional injury during follow-up. However, among men who had a hospital admission for unintentional injury, 71% had only one admission, 18% had two admissions and 11% had three or more. We therefore repeated the analyses based on the total number of admissions for each type of unintentional injury using Poisson regression for injury rates during follow-up.
RESULTS
Of 1,379,531 men in the original cohort, 1,109,475 (80.4%) had complete data and are included in the analyses. The most common reason for exclusion was missing IQ (N= 213,861). Those with missing data had lower SES and educational attainments. Men were followed-up for an average 24.2 years. The ICD codes used to identify hospital admissions for unintentional injuries are shown in Table 1. A total of 198,133 (17.9%) men included in the analyses had at least one admission for any unintentional injury during follow-up compared with 14,282 (5.3%) in men with missing data. The most common cause of unintentional injury was falling (7.5% of men included in the analyses), followed by road accidents (4.3%), poisoning (0.5%), fire (0.3%) and drowning (0.03%). In addition, 14,637 (1.3%) men had at least one admission as a result of complications of medical care.
Table 1. Number of men with at least one hospital admission for unintentional injury during follow-up (N=1,109,475).
| ICD 8/9 codes | ICD 10 codes | N1 | |
|---|---|---|---|
| All unintentional injuries2 | E800-E949 | V01-X59, Y85-86 | 198,133 |
| Falls | E880-E888 | W00-W19 | 82,706 |
| Road accidents | E810-E829 | See footnote3 | 47,199 |
| Poisoning | E850-E869 | X40-X49 | 6,021 |
| Fire | E890-E899 | X00-X09 | 2,967 |
| Drowning | E910 | W65-W74 | 331 |
| Complications of medical care | E870-E879 | Y40-Y84, Y88 | 14,637 |
Note: men could have more than one type of unintentional injury
Excluding complications of medical care
V01.1-V01.9, V02.1-V02.9, V03.1-V03.9, V04.1-V04.9, V06.1-V06.9, V09.2, V09.3, V10.3-V10.9, V11.3-V11.9, V12.3-V12.9, V13.3-V13.9, V14.3-V14.9, V15.4-V15.9, V16.4-V16.9, V17.4-V17.9, V18.4-V18.9, V19.4-V19.9, V20.3-V20.9, V21.3-V21.9, V22.3-V22.9, V23.3-V23.9, V24.3-V24.9, V25.3-V25.9, V26.3-V26.9, V27.3-V27.9, V28.3-V28.9, V29.4-V29.9, V30.4-V30.9, V31.4-V31.9, V32.4-V32.9, V33.4-V33.9, V34.4-V34.9, V35.4-V35.9, V36.4-V36.9, V37.4-V37.9, V38.4-V38.9, V39.4-V39.9, V40.4-V40.9, V41.4-V41.9, V42.4-V42.9, V43.4-V43.9, V44.4-V44.9, V45.4-V45.9, V46.4-V46.9, V47.4-V47.9, V48.4-V48.9, V49.4-V49.9, V50.4-V50.9, V51.4-V51.9, V52.4-V52.9, V53.4-V53.9, V54.4-V54.9, V55.4-V55.9, V56.4-V56.9, V57.4-V57.9, V58.4-V58.9, V59.4-V59.9, V60.4-V60.9, V61.4-V61.9, V62.4-V62.9, V63.4-V63.9, V64.4-V64.9, V65.4-V65.9, V66.4-V66.9, V67.4-V67.9, V68.4-V68.9, V69.4-V69.9, V70.4-V70.9, V71.4-V71.9, V72.4-V72.9, V73.4-V73.9, V74.4-V74.9, V75.4-V75.9, V76.4-V76.9, V77.4-V77.9, V78.4-V78.9, V79.4-V79.9, V80.3-V80.5, V81.1, V82.1, V82.8-V82.9, V83.0-V83.3, V84.0-V84.3, V85.0-V85.3, V86.0-V86.3, V87.0-V87.9, V89.2-V89.3, V89.9, V99 and Y850.
Characteristics of men included in the analyses are shown in Table 2. Men with lower IQ scores were somewhat shorter and had slightly higher BMI. Differences in SES and education were stepwise, with lower IQ men increasingly less likely to have parents from a non-manual SES, to be from a non-manual SES, or to have been university educated.
Table 2. Characteristics of 1,109,475 men included in analyses.
| IQ score | ||||
|---|---|---|---|---|
| 1 or 2 | 3 or 4 | 5 or 6 | 7, 8 or 9 | |
| N | 104,448 | 275,006 | 443,512 | 286,509 |
| Mean (SD) | ||||
| Age (years) | 18.3 (0.6) | 18.2 (0.6) | 18.3 (0.6) | 18.4 (0.6) |
| Height (cm) | 177.3 (6.7) | 178.4 (6.5) | 179.4 (6.4) | 180.4 (6.4) |
| BMI (kg/m2) | 21.9 (3.4) | 21.8 (3.0) | 21.6 (2.7) | 21.4 (2.5) |
| Systolic blood pressure (mmHg) | 128.5 (11.0) | 128.4 (10.8) | 128.5 (10.8) | 128.6 (10.9) |
| N (%) | ||||
| Parents in non-manual occupation | 20,816 (19.9) | 81,949 (29.8) | 196,478 (44.3) | 176,538 (61.6) |
| Subject in non-manual occupation | 7,814 (7.5) | 42,403 (15.4) | 116,188 (26.2) | 118,296 (41.3) |
| University educated | 3,561 (3.4) | 31,603 (11.5) | 145,599 (32.8) | 192,593 (67.2) |
| Hospital admission for any unintentional injury | 24,242 (23.2) | 57,206 (20.8) | 76,973 (17.4) | 39,712 (13.9) |
Table 3 presents HRs (95% CI) for any unintentional injury (excluding medical complications) for IQ score relative to the highest-scoring group (IQ=9). There were consistent stepwise increases in injury hazard across all nine IQ groups (p for trend <0.001). In age-adjusted analyses, men in the lowest IQ group were more than twice as likely to have an unintentional injury as those in the highest group and a SD (1.9 point) decrease in IQ score was associated with a 20% (95% CI: 20%, 21%) increase in risk. Adjustment for BMI and blood pressure had no effect (results not shown but available upon request). Associations were weakened by adjustments for childhood and adult SES and education but striking gradients of increasing injuries with decreasing IQ score remained.
Table 3. Hazard ratio (95% CI) for any unintentional injury by IQ.
| IQ score | N (injury / no injury) | Adjusted for age | Adjusted for age and childhood SES1 | Adjusted for age and adult SES | Multiple adjustment2 (excluding education) | Multiple adjustment3 (including education) |
|---|---|---|---|---|---|---|
| 9 | 5,798 / 43,677 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 8 | 12,284 / 78,225 | 1.16 (1.12, 1.19) | 1.15 (1.11, 1.18) | 1.14 (1.11, 1.18) | 1.13 (1.09, 1.17) | 1.09 (1.06, 1.12) |
| 7 | 21,630 / 124,895 | 1.26 (1.22, 1.30) | 1.23 (1.20, 1.27) | 1.22 (1.19, 1.26) | 1.19 (1.16, 1.23) | 1.11 (1.08, 1.15) |
| 6 | 31,924 / 162,432 | 1.41 (1.37, 1.45) | 1.37 (1.33, 1.41) | 1.34 (1.30, 1.37) | 1.30 (1.26, 1.33) | 1.17 (1.13, 1.20) |
| 5 | 45,049 / 204,107 | 1.64 (1.59, 1.68) | 1.58 (1.53, 1.62) | 1.51 (1.47, 1.55) | 1.43 (1.39, 1.47) | 1.25 (1.22, 1.29) |
| 4 | 32,960 / 129,846 | 1.74 (1.70, 1.79) | 1.67 (1.62, 1.72) | 1.59 (1.54, 1.63) | 1.52 (1.48, 1.57) | 1.30 (1.27, 1.34)0 |
| 3 | 24,246 / 87,954 | 1.89 (1.83, 1.94) | 1.80 (1.74, 1.85) | 1.69 (1.64, 1.74) | 1.61 (1.57, 1.66) | 1.37 (1.33, 1.41) |
| 2 | 16,604 / 56,144 | 2.02 (1.96, 2.08) | 1.92 (1.86, 1.98) | 1.79 (1.73, 1.84) | 1.70 (1.65, 1.76) | 1.43 (1.38, 1.48) |
| 1 | 7,638 / 24,062 | 2.11 (2.04, 2.18) | 2.00 (1.93, 2.07) | 1.84 (1.78, 1.91) | 1.78 (1.71, 1.84) | 1.48 (1.43, 1.54) |
| P 4 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| SD decrease | 198,133 / 911,342 | 1.20 (1.20, 1.21) | 1.18 (1.18, 1.19) | 1.16 (1.15, 1.16) | 1.15 (1.14, 1.15) | 1.10 (1.09, 1.10) |
| P | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Childhood SES and adult height
Adjusted for age, conscription centre, year of birth, childhood SES, adult height, BMI, systolic blood pressure, and adult SES
Adjusted for age, conscription centre, year of birth, childhood SES, adult height, BMI, systolic blood pressure, adult SES, and educational attainment
p for trend across nine categories of IQ score
Table 4 presents similar results for unintentional injury subtypes. HRs (95% CI) are presented for four categories of IQ score relative to the highest (7-9). Again, stepwise increases in age-adjusted hazard with decreasing IQ were apparent for all injuries other than drowning, for which there was no marked association. The strength of associations varied across the injury subtypes (in decreasing order of magnitude, age-adjusted HRs (95% CI) for a SD decrease in IQ: poisoning (1.53 (1.49, 1.57)), fire (1.36 (1.31, 1.41)), road traffic accidents (1.25 (1.23, 1.26)), complications of medical care (1.20 (1.18, 1.22)), and falling (1.17 (1.16, 1.18))). Adjustments for SES and, more markedly, education led to some attenuation of these associations but consistent gradients of increasing injury with decreasing IQ score remained.
Table 4. Hazard ratio (95% CI) for specific unintentional injuries by IQ.
| IQ score | N (injury / no injury) | Adjusted for age | Multiple adjustment1 (excluding education) |
Multiple adjustment2 (including education) |
|---|---|---|---|---|
| Falling | ||||
| 7-9 | 17,006 / 269,503 | 1.00 | 1.00 | 1.00 |
| 5/6 | 32,027 / 411,485 | 1.24 (1.22, 1.27) | 1.19 (1.17, 1.21) | 1.13 (1.11, 1.16) |
| 3/4 | 23,818 / 251,188 | 1.45 (1.42, 1.48) | 1.35 (1.32, 1.38) | 1.26 (1.23, 1.29) |
| 1/2 | 9,855 / 94,593 | 1.59 (1.55, 1.63) | 1.46 (1.42, 1.50) | 1.35 (1.31, 1.39) |
| P 3 | <0.001 | <0.001 | <0.001 | |
| SD decrease | 82,706 / 1,026,769 | 1.17 (1.16, 1.18) | 1.14 (1.13, 1.15) | 1.11 (1.10, 1.12) |
| P | <0.001 | <0.001 | <0.001 | |
| Road accident | ||||
| 7-9 | 9,088 / 277,421 | 1.00 | 1.00 | 1.00 |
| 5/6 | 17,611 / 425,901 | 1.27 (1.23, 1.30) | 1.14 (1.11, 1.17) | 1.00 (0.97, 1.03) |
| 3/4 | 13,805 / 261,201 | 1.54 (1.50, 1.58) | 1.33 (1.30, 1.37) | 1.09 (1.06, 1.12) |
| 1/2 | 6,695 / 97,753 | 1.99 (1.93, 2.06) | 1.65 (1.60, 1.71) | 1.30 (1.25, 1.35) |
| P 3 | <0.001 | <0.001 | <0.001 | |
| SD decrease | 47,199 / 1,062,276 | 1.25 (1.23, 1.26) | 1.18 (1.16, 1.19) | 1.09 (1.07, 1.10) |
| P | <0.001 | <0.001 | <0.001 | |
| Poisoning | ||||
| 7-9 | 856 / 285,653 | 1.00 | 1.00 | 1.00 |
| 5/6 | 2,021 / 441,491 | 1.58 (1.46, 1.71) | 1.42 (1.31, 1.54) | 1.18 (1.09, 1.29) |
| 3/4 | 1,997 / 273,009 | 2.40 (2.22, 2.60) | 2.00 (1.84, 2.18) | 1.51 (1.38, 1.65) |
| 1/2 | 1,147 / 103,301 | 3.65 (3.34, 3.99) | 2.80 (2.54, 3.08) | 1.99 (1.80, 2.20) |
| P 3 | <0.001 | <0.001 | <0.001 | |
| SD decrease | 6,021 / 1,103,454 | 1.53 (1.49, 1.57) | 1.41 (1.37, 1.45) | 1.28 (1.24, 1.31) |
| P | <0.001 | <0.001 | <0.001 | |
| Fire | ||||
| 7-9 | 484 / 286,025 | 1.00 | 1.00 | 1.00 |
| 5/6 | 1,117 / 442,395 | 1.50 (1.35, 1.67) | 1.33 (1.19, 1.49) | 1.16 (1.03, 1.30) |
| 3/4 | 908 / 274,098 | 1.92 (1.71, 2.14) | 1.57 (1.39, 1.76) | 1.27 (1.12, 1.43) |
| 1/2 | 458 / 103,990 | 2.55 (2.25, 2.90) | 1.97 (1.71, 2.25) | 1.53 (1.32, 1.77) |
| P3*** | <0.001 | <0.001 | <0.001 | |
| SD decrease | 2,967 / 1,106,508 | 1.36 (1.31, 1.41) | 1.25 (1.20, 1.30) | 1.16 (1.11, 1.21) |
| P | <0.001 | <0.001 | <0.001 | |
| Drowning | ||||
| 7-9 | 79 / 286,430 | 1.00 | 1.00 | 1.00 |
| 5/6 | 127 / 443,385 | 1.07 (0.81, 1.42) | 1.02 (0.76, 1.37) | 1.01 (0.74, 1.36) |
| 3/4 | 92 / 274,914 | 1.21 (0.90, 1.63) | 1.12 (0.81, 1.55) | 1.10 (0.78, 1.55) |
| 1/2 | 33 / 104,415 | 1.14 (0.76, 1.71) | 0.99 (0.64, 1.52) | 0.99 (0.63, 1.56) |
| P 3 | 0.26 | 0.75 | 0.79 | |
| SD decrease | 331 / 1,109,144 | 1.05 (0.94, 1.17) | 1.00 (0.89, 1.13) | 1.00 (0.88, 1.13) |
| P | 0.38 | 0.98 | 0.95 | |
| Medical complication | ||||
| 7-9 | 2,964 / 283,545 | 1.00 | 1.00 | 1.00 |
| 5/6 | 5,595 / 437,917 | 1.22 (1.17, 1.28) | 1.19 (1.14, 1.25) | 1.12 (1.06, 1.17) |
| 3/4 | 4,217 / 270,789 | 1.47 (1.41, 1.54) | 1.38 (1.31, 1.45) | 1.25 (1.18, 1.31) |
| 1/2 | 1,861 / 102,587 | 1.71 (1.61, 1.81) | 1.58 (1.48, 1.68) | 1.41 (1.32, 1.50) |
| P 3 | <0.001 | <0.001 | <0.001 | |
| SD decrease | 14,637 / 1,094,838 | 1.20 (1.18, 1.22) | 1.17 (1.15, 1.19) | 1.13 (1.11, 1.15) |
| P | <0.001 | <0.001 | <0.001 | |
Adjusted for age, conscription centre, year of birth, childhood SES, adult height, BMI, systolic blood pressure, and adult SES
Adjusted for age, conscription centre, year of birth, childhood SES, adult height, BMI, systolic blood pressure, adult SES, and educational attainment
p for trend across four categories of IQ score
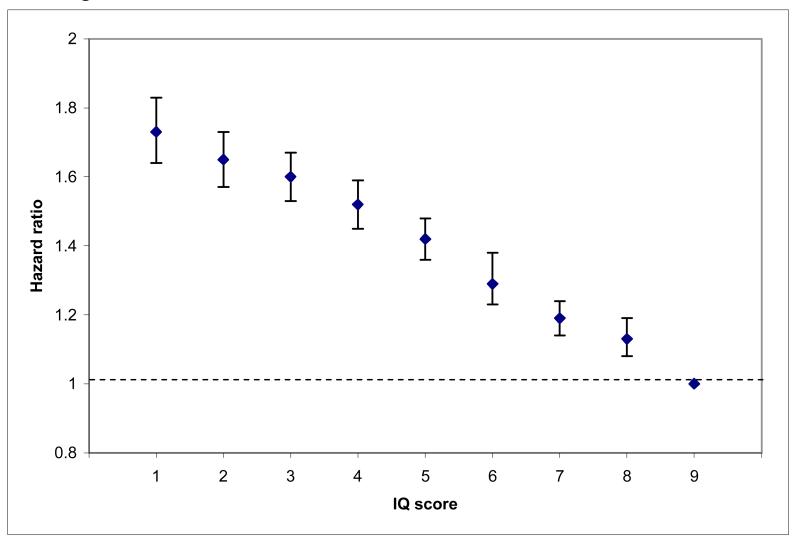
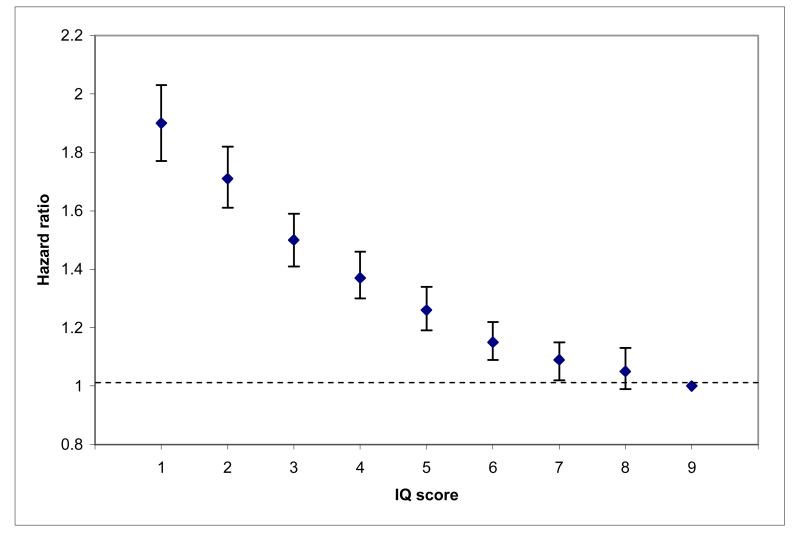
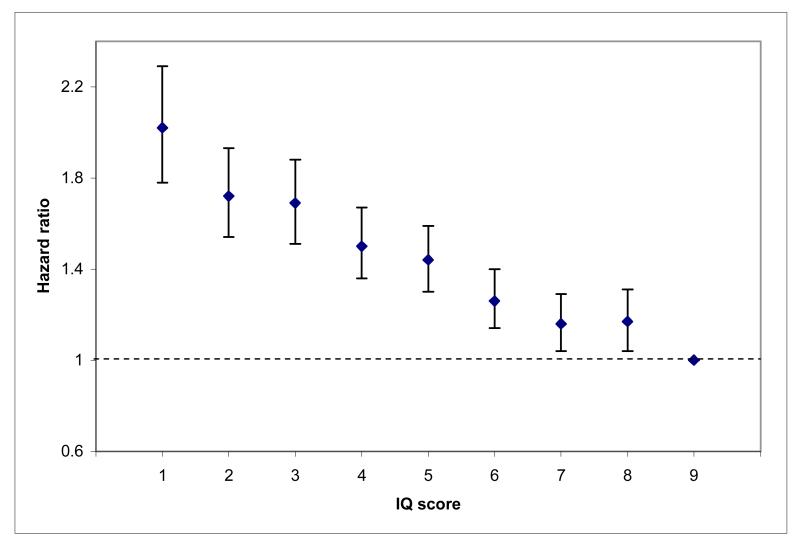
For injury subtypes with sufficient events to compute HRs across all nine IQ groups (falls, road accidents, poisoning, medical complications), we present Figures 1a-d. Incremental, inverse associations across all nine IQ categories are clearly apparent, with higher cognition associated with reduced injury risk.
Figure 1.
a: Hazard ratio (95% CI) for unintentional falls by IQ with multiple adjustments excluding education
b: Hazard ratio (95% CI) for road accidents by IQ with multiple adjustments excluding education
c: Hazard ratio (95% CI) for unintentional poisoning by IQ with multiple adjustments excluding education
d: Hazard ratio (95% CI) for complications of medical care by IQ with multiple adjustments excluding education
In the subgroup of men with smoking and alcohol data, there was little impact of adjustment for smoking status at conscription. Adjustment for risky alcohol use had slightly more effect but was still modest. The greatest but still marginal attenuation was observed for unintentional poisoning injuries (HR (95% CI) for SD decrease in IQ adjusted for age only: 1.51 (1.34, 1.70); adjusted for age and smoking: 1.46 (1.29, 1.65); and adjusted for age and risky alcohol use: 1.42 (1.26, 1.61)).
Results from analyses (a) based on men with no pre-conscription psychiatric illness; (b) adjusted for concurrent psychiatric illness during follow-up; (c) based on men with no pre-conscription injuries; and (d) using Poisson regression, were almost identical to those presented in Tables 3 and 4.
A total of 13,287 (1.2%) men had at least one hospital admission for intentional (attempted suicide) injury during follow-up. These men were 3.80 (95% CI: 3.67, 3.93) times more likely to have an unintentional injury admission than those with no admission for attempted suicide. This was most marked for unintentional poisoning: men with any intentional injury were 16.17 (15.05, 17.38) times more likely to have an unintentional poisoning admission than those without. HRs for IQ-unintentional injury associations in men with no attempted suicide admissions were marginally smaller than those based on all men. The most marked difference was in unintentional poisonings (age-adjusted HR (95% CI) for SD decrease in IQ in all men vs. men with no attempted suicide admissions: 1.53 (1.49, 1.57) vs. 1.46 (1.42, 1.51)).
DISCUSSION
We observed consistent, striking, step-wise associations of increasing injury rates with decreasing IQ for all injuries other than drowning. Associations were somewhat attenuated by adjustment for potential confounding or mediating factors, most markedly education. However, as education and IQ are moderately to highly positively correlated,(26) adjusting IQ associations for education is debateable. Substantial attenuation by education may signal a pathway through which IQ might influence injury risk; equally, however, IQ-education correlations raise issues of co-linearity and inclusion of education in multivariable models may be over-adjustment.
Strengths and limitations
Analyses were based on a cohort of over one million men, well-defined for SES, followed for an average 24 years, and with IQ measured in early adulthood. The large sample size and lengthy follow-up provide good statistical power and have allowed investigation of specific injury subtypes. Results are based on a moderately large number of comparisons and the large sample size means that confidence intervals are, inevitably, narrow. However, our conclusions are based on the magnitude and consistency of results overall, rather than focussing on the results of individual comparisons or p-values.
Unintentional injuries were identified from routine hospital discharge data and only includes injuries resulting in hospital admission; however, as hospital treatment in Sweden is free, we have no reason to suppose there was any systematic bias resulting from this approach. Furthermore, injuries requiring hospital admission are likely to have the greatest impact on morbidity, disability, and premature mortality. Our results are limited to men and provide no information on IQ-unintentional injury associations in women, although we can think of no plausible explanations for differential IQ-injury gradients.
Finally, almost 20% of men were excluded from analyses, mostly because of missing IQ, and there were fewer injuries in this group. Educational achievement was generally lower, suggesting that excluded men may have been in the lower IQ range. The lower injury rates in these men therefore suggest that our HRs may be slight overestimates. However, their magnitude is consistent with those reported elsewhere(2;3), and the step-wise nature of the associations across all nine IQ scores make it unlikely that they are substantially due to selection bias.
Possible explanations for associations
The aetiology of unintentional injury is complex but there is emerging evidence(2-4) that IQ may have an important role and a number of plausible explanations have been offered. For example, individuals with lower IQ may have lower processing skills,(27) resulting in a reduced perception of risk and an increased tendency to engage in risky activities, e.g. dangerous climbing, fast driving, or swimming in unknown/dangerous waters. Alternatively, low IQ has been associated with poor psychomotor coordination(28) and poor health behaviours such as binge drinking,(16) and these factors may also increase injury risk. In a restricted dataset, we saw a small attenuation of effect after adjustment for risky alcohol use, which provides some support for this view.
Low IQ also tends to correlate with lower SES and income and, in men, lower SES in childhood(29) and adulthood(30) has been linked to unintentional injury mortality, possibly as a result of living and working in more hazardous environments. However, occupational SES associations with unintentional injury subtypes are complex. A recent study(4) reported an excess of workplace injuries in men in unskilled or manual occupations and an excess of sporting injuries in professional and managerial occupations. This may, at least in part, explain the lack of any IQ-drowning association in these data as higher SES, and therefore higher IQ, men are more likely to take part in water sports; equally however, this analysis was based on relatively few events.
The relative strength of the remaining IQ-injury associations varied. It is difficult to speculate on the reasons for this variation without further details on the circumstances surrounding the injuries. However, those most likely to involve a third party (road accidents or medical complications) or an occupational element (falling) were the weakest. It is notable that injuries due to complications of medical care, which should be independent of cognitive function, also showed a steady increase with decreasing IQ. This may be due to poorer health in lower IQ individuals(31) who have more contact with medical professionals and, correspondingly, more opportunity to experience complications. However, it may also indicate that known inequalities stemming from low IQ or SES extend into medical care.
The strongest association was observed for unintentional poisoning, and stronger IQ-unintentional poisoning associations have been reported in other studies of morbidity(2) and mortality(5). This may be because intentional poisoning is one of the suicide methods most likely to be miscoded as unintentional but we found no substantive evidence to support this view. Just under half of unintentional poisonings were from medicines and, although lower IQ individuals may have a higher frequency of medication use due to greater general morbidity, there is also evidence that lower cognitive function is associated with a reduced capacity to manage self-medication.(32;33)
Public health implications
Although genetics determine IQ to a large degree, there is some evidence that educational interventions may increase IQ in childhood.(34-36) Alternatively, targeted approaches to directly reduce unintentional injuries might concentrate on individuals with lower IQ scores who may live and work in more hazardous environments where falls, fire and road injuries are more common. Interventions might include improving environments, restricting access to toxic substances or unsafe areas or, given the consistently strong associations with unintentional poisoning, improving labelling on medicines and household products.
In conclusion, we observed consistent, step-wise associations of increasing unintentional injury risk with decreasing IQ score that were robust to adjustment for SES and other confounding factors. Our results are consistent with other studies but evidence is still scant and further research is needed to confirm and further explore these findings. A deeper understanding of IQ-injury associations will inform public health strategies that may lead to a reduction in future injuries.
What is already known on this subject?
Unintentional injuries (accidents) are a leading cause of morbidity, mortality and disability, particularly in younger age groups. However, in spite of the economic and public health burden of injuries, relatively little is known about their aetiology, which limits strategies for prevention. A small number of recent studies have suggested that fatal and non-fatal injuries may be more common in individuals with lower intelligence (IQ).
What does this study add?
We have examined associations between IQ measured in early adulthood and subsequent hospital admissions for (non-fatal) unintentional injury in a cohort of over 1,000,000 Swedish men (around 100 times more than previously studied in this context) followed-up for an average of 24 years. In addition to providing superior statistical power, this has enabled us to look at specific injury subtypes in more detail than has been previously possible. After adjusting for confounding variables, lower IQ scores were associated with an elevated risk of any unintentional injury and of injuries due to poisoning, fire, road traffic accidents, medical complications, and falling; associations were step-wise across the full IQ range.
Acknowledgements and Funding
David Batty is a Wellcome Trust Fellow (WBS U.1300.00.006.00012.01). The MRC Social and Public Health Sciences Unit receives funding from the UK Medical Research Council and the Chief Scientist Office at the Scottish Government Health Directorates. The Centre for Cognitive Ageing and Cognitive Epidemiology is supported by the Biotechnology and Biological Sciences Research Council, the Engineering and Physical Sciences Research Council, the Economic and Social Research Council, the Medical Research Council, and the University of Edinburgh as part of the cross-council Lifelong Health and Wellbeing initiative.
Footnotes
Conflict of interest: None.
The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive licence (or non-exclusive for government employees) on a worldwide basis to the BMJ Publishing Group Ltd and its Licensees to permit this article (if accepted) to be published in Journal of Epidemiology and Community Health and any other BMJPGL products to exploit all subsidiary rights, as set out in our licence (http://jech.bmj.com/ifora/licence.pdf).
Reference List
- (1).Peden M, McGee K, Sharma G. The Injury Chartbook: A Graphical Overview of the Global Burden of Injuries. World Health Organisation; Geneva, Switzerland: 2002. [Google Scholar]
- (2).Osler M, Andersen AMN, Laursen B, Lawlor DA. Cognitive function in childhood and early adulthood and injuries later in life: the Metropolit 1953 male birth cohort. Int J Epidemiol. 2007;36:212–9. doi: 10.1093/ije/dyl261. [DOI] [PubMed] [Google Scholar]
- (3).Lawlor DA, Clark H, Leon DA. Associations between childhood intelligence and hospital admissions for unintentional injuries in adulthood: the Aberdeen Children of the 1950s cohort study. Am J Public Health. 2007;97:291–7. doi: 10.2105/AJPH.2005.080168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (4).Batty GD, Deary IJ, Schoon I, Gale CR. Childhood mental ability in relation to cause-specific accidents in adulthood: the 1970 British Birth Cohort Study. Q J Med. 2007;100:405–14. doi: 10.1093/qjmed/hcm039. [DOI] [PubMed] [Google Scholar]
- (5).Batty GD, Gale CR, Tynelius P, Deary IJ, Rasmussen F. IQ in early adulthood, socio-economic position, and unintentional injury mortality by middle-age: cohort study of over one million Swedish men. Am J Epidemiol. 2009;169:606–15. doi: 10.1093/aje/kwn381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (6).Hemmingsson T, Melin B, Allebeck P, Lundberg I. The association between cognitive ability measured at ages 18-20 and mortality during 30 years of follow-up - a prospective observational study among Swedish males born 1949-51. Int J Epidemiol. 2006;35:665–70. doi: 10.1093/ije/dyi321. [DOI] [PubMed] [Google Scholar]
- (7).O’Toole BI. Intelligence and behaviour and motor vehicle accident mortality. Accid Anal Prev. 1990;22:211–21. doi: 10.1016/0001-4575(90)90013-b. [DOI] [PubMed] [Google Scholar]
- (8).Gunnell D, Magnusson PKE, Rasmussen F. Low intelligence test scores in 18 year old men and risk of suicide: cohort study. BMJ. 2004;330:167–70. doi: 10.1136/bmj.38310.473565.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (9).Batty GD, Wennerstad KM, Smith GD, Gunnell D, Deary IJ, Tynelius P, Rasmussen F. IQ in early adulthood and later cancer risk: cohort study of one million Swedish men. Ann Oncol. 2007;18:21–8. doi: 10.1093/annonc/mdl473. [DOI] [PubMed] [Google Scholar]
- (10).Zammit S, Allebeck P, David AS, Dalman C, Hemmingsson T, Lundberg I, Lewis G. A longitudinal study of premorbid IQ score and risk of developing schizophrenia, bipolar disorder, severe depression, and other nonaffective psychoses. Arch Gen Psychiatry. 2004;61:354–60. doi: 10.1001/archpsyc.61.4.354. [DOI] [PubMed] [Google Scholar]
- (11).Starr JM, Taylor MD, Hart CL, Davey Smith G, Whalley LJ, Hole DJ, Wilson V, Deary IJ. Childhood mental ability and blood pressure at midlife: linking the Scottish Mental Survey 1932 and the Midspan studies. J Hypertens. 2004;22:893–7. doi: 10.1097/00004872-200405000-00009. [DOI] [PubMed] [Google Scholar]
- (12).Chandola T, Deary IJ, Blane D, Batty GD. Childhood IQ in relation to obesity and weight gain in adult life: the National Child Development (1958) Study. Int J Obes. 2006;30:1422–32. doi: 10.1038/sj.ijo.0803279. [DOI] [PubMed] [Google Scholar]
- (13).Terry PD, Abramson JL, Neaton JD, MRFIT Research Group Blood pressure and risk of death from external causes among men screened for the Multiple Risk Factor Intervention Trial. Am J Epidemiol. 2007;165:294–301. doi: 10.1093/aje/kwk014. [DOI] [PubMed] [Google Scholar]
- (14).Whitlock G, Norton R, Clark T, Jackson R, MacMahon S. Is body mass index a risk factor for motor vehicle driver injury? A cohort study with prospective and retrospective outcomes. Int J Epidemiol. 2003;32:147–9. doi: 10.1093/ije/dyg022. [DOI] [PubMed] [Google Scholar]
- (15).Batty GD, Deary IJ, Schoon I, Emslie C, Hunt K, Gale CR. Childhood mental ability and adult alcohol intake and alcohol problems: the 1970 British Cohort Study. Am J Public Health. 2008;98:2237–43. doi: 10.2105/AJPH.2007.109488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (16).Batty GD, Deary IJ, MacIntyre S. Childhood IQ and life course socioeconomic position in relation to alcohol induced hangovers in adulthood: the Aberdeen children of the 1950s study. J Epidemiol Community Health. 2006;60:872–4. doi: 10.1136/jech.2005.045039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (17).Kool B, Ameratunga S, Robinson E, Crengle S, Jackson R. The contribution of alcohol to falls at home among working age adults. Alcohol. 2008;42:383–8. doi: 10.1016/j.alcohol.2008.04.004. [DOI] [PubMed] [Google Scholar]
- (18).Connor J, Norton R, Ameratunga S, Jackson R. The contribution of alcohol to serious car crash injuries. Epidemiology. 2004;15:337–44. doi: 10.1097/01.ede.0000120045.58295.86. [DOI] [PubMed] [Google Scholar]
- (19).Hemmingsson T, Lundberg I. How far are socioeconomic differences in coronary heart disease hospitalization, all-cause mortality and cardiovascular mortality among adult Swedish males attributable to negative childhood circumstances and behaviour in adolescence? Int J Epidemiol. 2005;34:260–7. doi: 10.1093/ije/dyh314. [DOI] [PubMed] [Google Scholar]
- (20).Manual of the International Statistical Classification of Diseases, Injuries, and Causes of Death. 8th revision World Health Organisation; Geneva: 1967. [Google Scholar]
- (21).International Statistical Classification of Diseases and Related Health Problems. 10th revision World Health Organisation; Geneva: 1992. [Google Scholar]
- (22).Manual of the International Statistical Classification of Diseases, Injuries, and Causes of Death. 9th revision World Health Organisation; Geneva: 1977. [Google Scholar]
- (23).Gunnell D. Can adult anthropometry be used as a biomarker for prenatal and childhood exposures? Int J Epidemiol. 2002;31:390–4. [PubMed] [Google Scholar]
- (24).Hiroeh U, Appleby L, Mortensen PB, Dunn G. Death by homicide, suicide, and other unnatural causes in people with mental illness: a population study. Lancet. 2001;358:2110–2. doi: 10.1016/S0140-6736(01)07216-6. [DOI] [PubMed] [Google Scholar]
- (25).Gale CR, Deary IJ, Boyle SH, Barefoot J, Mortensen LH, Batty GD. Cognitive ability in early adulthood and risk of 5 specific psychiatric disorders in middle age: the Vietnam Experience Study. Arch Gen Psychiatry. 2008;65:1410–8. doi: 10.1001/archpsyc.65.12.1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (26).Deary IJ, Strand S, Smith P, Fernandes C. Intelligence and educational achievement. Intelligence. 2007;35:13–21. [Google Scholar]
- (27).Whalley LJ, Deary IJ. Longitudinal cohort study of childhood IQ and survival up to age 76. BMJ. 2001;322:819. doi: 10.1136/bmj.322.7290.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (28).Gale CR, Batty GD, Cooper C, Deary IJ. Psychomotor coordination and intelligence in childhood and health in adulthood - testing the system integrity hypothesis. Psychosom Med. 2009;71:675–681. doi: 10.1097/PSY.0b013e3181a63b2e. [DOI] [PubMed] [Google Scholar]
- (29).Lawlor DA, Sterne JAC, Tynelius P, Davey Smith G, Rasmussen F. Association of childhood socioeconomic position with cause-specific mortality in a prospective record linkage study of 1,838,384 individuals. Am J Epidemiol. 2006;164:907–15. doi: 10.1093/aje/kwj319. [DOI] [PubMed] [Google Scholar]
- (30).Steenland K, Halperin W, Hu S, Walker JT. Deaths due to injuries among employed adults: the effects of socioeconomic class. Epidemiology. 2003;14:74–9. doi: 10.1097/00001648-200301000-00017. [DOI] [PubMed] [Google Scholar]
- (31).Hart CL, Taylor MD, Davey Smith G, Whalley LJ, Starr JM, Hole DJ, Wilson V, Deary IJ. Childhood IQ, social class, deprivation and their relationships with mortality and morbidity risk in later life: prospective observational study linking the Scottish Mental Survey 1932 and the Midspan studies. Psychosom Med. 2003;65:877–83. doi: 10.1097/01.psy.0000088584.82822.86. [DOI] [PubMed] [Google Scholar]
- (32).Anderson K, Jue SG, Madaras-Kelly KJ. Identifying patients at risk for medication mismanagement: using cognitive screens to predict a patient’s accuracy in filling a pillbox. Consultant Pharmacist. 2008;23:459–72. doi: 10.4140/tcp.n.2008.459. [DOI] [PubMed] [Google Scholar]
- (33).Maddigan SL, Farris KB, Keating N, Wiens CA, Johnson JA. Predictors of older adults’ capacity for medication management in a self-medication program. Journal of Aging and Health. 2003;15:332–52. doi: 10.1177/0898264303251893. [DOI] [PubMed] [Google Scholar]
- (34).Sternberg R, Grigorenko E. Environmental effects on cognitive abilities. Erlbaum; Mahwah, NJ: 2001. [Google Scholar]
- (35).Ramey CT, Ramey SL. Early learning and school readiness: Can early intervention make a difference? Merrill-Palmer Quarterly Journal of Developmental Psychology. 2004;50:471–91. [Google Scholar]
- (36).Barnett WS, Camilli G. Compensatory preschool education, cognitive development, and “race”. In: Fish JM, editor. Race and Intelligence. Separating science from myth. Lawrence Erlbaum Associates; London: 2002. pp. 369–406. [Google Scholar]