Abstract
Persistent complex bereavement disorder (PCBD) is a bereavement-specific syndrome characterized by prolonged and impairing grief. Most research on this syndrome rests on the traditional latent variable model whereby symptoms reflect an underlying entity. The network (or causal system) approach offers an alternative framework for understanding PCBD that does not suffer from limitations inherent in the latent entity approach. The network approach to psychopathology conceptualizes the relation between symptoms and disorder as mereological, not reflective. That is, symptoms do not reflect an inferred, unobservable category or dimension, but rather are themselves constitutive of the disorder. Accordingly, we propose that PCBD constitutes a causal system of mutually reinforcing symptoms that arise following the death of a loved one and settle into a pathological equilibrium. In this study, we used data from the Changing Lives of Older Couples (CLOC) database to identify symptoms central to PCBD, distinguish the PCBD network from an overlapping but distinct network of depression symptoms, and examine how previously identified risk factors may contribute to the maintenance or development of PCBD. Together, these findings provide an important first step toward understanding the nature and etiology of the PCBD network.
Grief is a syndrome of cognitions, emotions, and behaviors that often arise together following the death of a loved one. It is chiefly characterized by severe pangs of emotional pain, yearning for the deceased, preoccupation with memories of the deceased and of the death, approach behavior (e.g., spending time with photographs, clothing, or other items associated with the deceased), and avoidance behavior (e.g., avoiding reminders of the death; Parkes, 1972). There is substantial variation in the extent and duration with which this syndrome occurs. For most, grief subsides over the initial weeks and months following the loss (Bonanno et al., 2002). However, for a subset of bereaved adults (6.7%), elevated and impairing levels of grief persist for years after the death (Kersting, Brahler, Glaesmer, & Wagner, 2011). This prolonged elevation of debilitating grief symptoms has been called traumatic grief (Horowitz et al., 1997), prolonged grief (Prigerson et al., 2009), complicated grief (Shear et al., 2011), and, most recently, persistent complex bereavement disorder (PCBD; American Psychiatric Association, 2013). In this manuscript, we will use grief and PCBD to denote the same syndrome, with the former applied when the syndrome is present during the first year following loss and the latter when present thereafter.
Latent Variable Approach to PCBD
Clinical researchers have conducted numerous studies aimed at differentiating PCBD from other syndromes and establishing diagnostic criteria that can reliably identify those individuals with PCBD. These studies typically involve latent variable analyses, such as factor analysis (e.g., Boelen & van den Bout, 2005) or item response theory (e.g., Prigerson et al., 2009). The theory behind these approaches is that PCBD is a latent entity that cannot be measured directly (Borsboom, 2008; Borsboom, Mellenbergh, & van Heerden, 2003). Instead researchers must infer the presence of PCBD from a set of fallible indicators (i.e., symptoms) that are caused by the latent variable. From this perspective, the relationship between PCBD and the symptoms of PCBD is one of reflective measurement, analogous to the relationship between temperature and a thermometer. PCBD is the common cause that produces the covariance among PCBD symptoms just as the ambient temperature of the room produces the covariance among the mercury readings of multiple thermometers.
This latent variable approach is problematic for PCBD. First, the symptoms of PCBD violate the axiom of local independence (i.e., the assumption that the indicators of a latent construct are independent of one another; Borsboom, 2008). This axiom is required for latent variable analyses so that covariance of the indicators can be attributed to the influence of the latent variable (i.e., the common cause) rather than to causal relations among the indicators themselves. For example, there are no causal relations between two thermometers. Placing an ice cube on thermometer A will lower its temperature reading, but the reading from thermometer B will remain unaffected. Consequently, we can attribute the covariance of the thermometers to the temperature of their shared environment. In contrast, grief theorists quite rightly assume causal relations among the symptoms of PCBD (Boelen, van den Hout, & van den Bout, 2006; Shear et al., 2007). For example, individuals with PCBD avoid reminders of the loss (symptom C6) because those reminders provoke painful emotions (symptom B2). That avoidance, in turn, maintains emotional reactivity to reminders of the loss. This reciprocal causal relationship among symptoms is so central to theories of PCBD that modifying the relationship is a principal aim of PCBD treatments (e.g., Shear, Frank, Houck, & Reynolds, 2005). Clearly, PCBD does not conform to the axiom of local independence.
More fundamentally, the latent variable approach rests on unsupported assumptions about the ontology of PCBD. It assumes that the symptoms of PCBD covary because they are caused by a common underlying disorder. According to this view, a widow experiences frequent intense yearning for her deceased spouse because she has PCBD in the same way that one coughs, spits up blood, and has chest pain because one has a lung tumor (Borsboom, 2008; Borsboom & Cramer, 2013). However, unlike the case of the tumor, PCBD cannot be distinguished from the symptoms that reflect its presence. An asymptomatic bereaved person cannot have PCBD, whereas doctors often discover tumors in people not yet experiencing any symptoms of cancer. Moreover, scholars are increasingly recognizing the limitations of the disease model and other approaches that attribute the presence of mental health syndromes to a common underlying cause (Zachar & Kendler, 2007). Efforts to identify the particular genetic, neurobiological, psychological, or social cause of a mental disorder have given way to a recognition that the etiology of mental illness is complex and multifactorial (Kendler, 2012). Accordingly, it is unlikely that there is a common underlying disease or disorder that gives rise to the symptoms of PCBD.
Network Approach to PCBD
The network (or causal system) approach to mental disorders provides a viable alternative to the latent entity approach. Foreshadowed by Boyd’s (1991) homeostatic property cluster kind conceptualization of biological species (for further discussion, see Kendler, Zachar, & Craver, 2011; McNally, 2011, pp. 203–207), the network approach conceptualizes mental disorder as a causal system of functionally interrelated symptoms that have settled into a pathological equilibrium (Borsboom & Cramer, 2013). That is, symptoms neither reflect nor result from an independent latent entity. Rather, symptoms are constitutive of the disorder. Symptoms do not cohere as a syndrome because they arise from a common underlying cause. Rather, they cohere because of the causal relations among them.
We propose that the symptoms of PCBD covary because they are elements in a mutually reinforcing network of cognitions, emotions, and behaviors that unfolds over time following the death of a loved one. In the initial weeks and months following the loss, most bereaved adults will experience some or even many elements of this syndrome. For the majority, the frequency and severity of these elements will diminish over time. However, for a minority of individuals, these elements will persist and the syndrome will ultimately reach a self-sustaining state of equilibrium. Importantly, it is not a common underlying disorder, but rather the self-reinforcing nature of the symptoms that makes them cohere as a distinguishable syndrome.
Implications of the network approach for PCBD
The network approach has implications for our understanding of PCBD that differ from those implied by the latent construct approach. First, these approaches differ in the focus given to symptoms of the disorder. In the latent variable model, symptoms are important only to the extent that they indicate the presence of the underlying disorder. In contrast, from a network perspective, the syndrome does not exist apart from its constitutive symptoms, thereby placing greater focus on understanding the individual symptoms of the syndrome.
Second, the network approach does not require adherence to the clinically implausible axiom of local independence. Indeed, causal relations among symptoms are the heart of the network approach. Accordingly, the network approach comports well with theories of PCBD that explicitly hypothesize causal relations among PCBD components (Boelen et al., 2006; Shear et al., 2007).
Third, the network and latent entity approaches differ in their construal of comorbidity. PCBD is highly comorbid with other mental disorders, including depression, posttraumatic stress disorder (PTSD), and anxiety disorders (Simon et al., 2007). These high rates of comorbidity are not surprising given the phenomenological overlap among these disorders. For example, difficulty experiencing positive emotions (i.e. emotional numbness; Kashdan, Elhai, & Frueh, 2006), loneliness (Cacioppo, Hughes, Waite, Hawkley, & Thisted, 2006; Solomon & Dekel, 2008), difficulty imagining one’s future (e.g., Brown et al., 2013; Robinaugh & McNally, 2013; Williams et al., 2007), and intrusive distressing memories (Boelen & Huntjens, 2008; Reynolds & Brewin, 1999), are all elevated in those with depression, PCBD, and PTSD.
From a latent variable perspective, this overlap is problematic. Overlap in the symptoms used as indicators of an underlying disorder raises the question of whether comorbidity (i.e., the co-occurrence of two discrete latent variables) is real or a byproduct of the means used to assess the underlying condition. In contrast, the network approach posits that mental health syndromes are not distinct latent entities, but rather distinguishable yet overlapping causal networks. From this perspective, the high rate of comorbidity in PCBD is not a nosological problem to be solved. Rather, it is an expected consequence of the shared symptoms among mental health syndromes (Cramer, Waldorp, van der Maas, & Borsboom, 2010). For example, just as loneliness may contribute to the maintenance of the PCBD network, it may likewise contribute to the maintenance of the depression network (Cacioppo, Hawkley, & Thisted, 2010). Consequently, loneliness may act as a “bridge” between these two networks, increasing the likelihood of experiencing one syndrome when experiencing the other (cf. Cramer et al., 2010).
Finally, the network approach has implications for how we conceptualize risk factors for PCBD. There are numerous risk factors that may contribute to the development and maintenance of the PCBD network (Burke & Neimeyer, 2013), including characteristics of the death (e.g., traumatic loss; Momartin, Silove, Manicavasagar, & Steel, 2004), one’s relationship to the deceased (e.g., the death of a spouse or child; Cleiren, 2003), intrapersonal factors (e.g., neuroticism; Bonanno et al., 2002), and interpersonal factors (e.g., instrumental social support; Bonanno et al., 2002). However, despite the large body of research identifying these risk factors, the mechanisms by which they influence PCBD remain poorly understood.
Faced with a similar problem in other mental disorders, researchers have called for an increased focus on common pathways by which diverse risk factors have their effects on mental disorders (e.g., Howes & Kapur, 2009). The network approach clarifies these etiological pathways by suggesting that their terminus is not a latent entity, but rather individual network components. In particular, it suggests that risk factors affect the development and maintenance of the PCBD syndrome by either (1) contributing to the presence of a given PCBD symptom or (2) by modifying the relationships among PCBD symptoms.
Importantly, the network approach allows for explanatory pluralism (Kendler, 2005) in describing the contribution of risk factors to the etiology of mental disorders. Risk factors across levels of analysis (e.g., genetic, neurobiological, psychological, or social) may affect PCBD symptoms and, consequently, feed into the self-reinforcing network. Moreover, these risk factors may vary across individuals. For example, a mother who unexpectedly loses her son to suicide may become preoccupied with thoughts related to the loss and may react to those thoughts with intense painful emotions (Wilson & Gilbert, 2008). Over time this preoccupation and emotional pain may foster anger or regret regarding the loss and avoidance of things that remind her of the death, thereby maintaining the syndrome. On the other hand, a young man with poor implicit emotion regulation who loses his father to natural causes may struggle to regulate the emotional pain he feels when reminded of his death (Gyurak, Gross, & Etkin, 2011). As a result, he may become reliant on cognitive and behavioral avoidance as a means of escaping those aversive emotions, feeding into the PCBD syndrome.
In these examples, distinct risk factors operate at different levels of analysis and impact distinct PCBD symptoms. Yet, because of the causal relationships among network components, these individuals may ultimately experience a comparable syndrome. Indeed, myriad risk factors may influence the development and maintenance of PCBD following loss and the risk factors implicated in the etiology of the disorder may vary across individuals, even when those individuals experience a common syndrome.
The Current Study
In the present study, we explored the implications of the network approach for PCBD. First, we examined endorsement rates for each PCBD symptom at 6, 18, and 48 months following spousal bereavement to obtain an indication of the threshold for activation of each symptom. Second, we computed the network structure of PCBD, elucidating relations among symptoms and identifying those most central to the network. Third, to elucidate the co-occurrence of PCBD and depression, we jointly examined the network structure of PCBD and depression symptoms. Fourth, we sought to identify potential paths by which six previously identified risk factors for PCBD may influence the syndrome. Although a complete analysis of these risk factors is beyond the scope of this study, the pattern of associations between each risk factor and the individual PCBD symptoms should provide an initial assessment of which symptoms these risk factors affect and, thereby, paths by which they may influence the broader syndrome. Accordingly, we calculated the correlations between six pre-loss risk factors for PCBD and each of the individual PCBD symptoms at 6, 18, and 48 months post-loss.
Method
We analyzed data from the Changing Lives of Older Couples (CLOC) study. In this study, researchers collected baseline data from 1,532 individuals from the Detroit, Michigan area in a multi-wave prospective study of spousal bereavement. Subjects were men age 65 or older or women whose husband was at least 65 years old. All subjects were English-speaking, non-institutionalized, and able to participate in a two-hour face-to-face interview. A two-stage area probability sample was used to collect baseline information from couples starting in June 1988 and ending in April 1988. Thereafter, the researchers inspected the daily newspaper obituaries and the monthly death records maintained by the state of Michigan to identify baseline subjects who had experienced the death of a spouse. Of the 335 subjects known to have lost a spouse, 250 participated in the first wave of follow-up interviews that occurred 6 months after the loss (Wave 1). Subsequently, 210 subjects participated in the study 18 months after the loss (Wave 2), and 106 participated 48 months after the loss (Wave 3).
Measures
Persistent complex bereavement disorder
Although the CLOC study was not designed to assess PCBD, many questions in the survey assessed constructs that correspond closely to the DSM-5 PCBD symptoms (American Psychiatric Association, 2013). We used these questions to obtain an assessment of 13 of the 16 PCBD symptoms (see Table 1). No questions corresponded to symptom C3 (i.e., difficulty with positive reminiscing about the deceased), C7 (i.e., a desire to die in order to be reunited with the deceased), or C8 (i.e., difficulty trusting others since the loss). Accordingly, those symptoms did not appear in our analyses.
Table 1.
Rates of endorsement for the symptoms of persistent complex bereavement disorder at 6, 18, and 48 months post-loss
| DSM | CLOC | Mean Rating
|
Proportion Endorsed
|
||||
|---|---|---|---|---|---|---|---|
| PCBD Symptoms | Variables | W1 | W2 | W3 | W1 | W2 | W3 |
| B1: Yearning | 1429 | 3.16 | 2.96 | 2.50 | .78 | .74 | .59 |
| B2: Emotional Pain | 1433, 1624, 1635 | 2.49 | 1.97 | 1.66 | .37 | .14 | .10 |
| B3: Preoccupying Thoughts Person | 1601 | 5.41 | 5.02 | 4.39 | .58 | .36 | .20 |
| B4: Preoccupying Thoughts Death | 1607 | 2.34 | 2.10 | 1.66 | .51 | .41 | .25 |
| C1: Difficulty Accepting Loss | 1414 | 1.59 | 1.25 | 1.12 | .22 | .10 | .03 |
| C2: Emotional Numbness/Disbelief | 1415, 1416 | 1.87 | 1.58 | 1.22 | .22 | .10 | .03 |
| C4: Bitterness Related to Loss | 1417, 1418 | 1.67 | 1.56 | 1.36 | .15 | .11 | .06 |
| C5: Regrets About Death or Deceased | 1422, 1424 | 1.58 | 1.57 | 1.46 | .11 | .13 | .13 |
| C6: Avoidance of Reminders | 1611, 1625 | 1.88 | 1.80 | 1.60 | .10 | .05 | .03 |
| C9: Loneliness | 2405 | 1.86 | 1.69 | 1.46 | .18 | .15 | .07 |
| C10: Life Empty or Meaningless | 1410, 1421 | 2.36 | 1.99 | 1.79 | .30 | .20 | .18 |
| C11: Diminished Identity | 1420 | 3.12 | 2.62 | 2.18 | .80 | .62 | .49 |
| C12: Difficulty Planning Future | 3102 | 1.75 | 1.55 | -- | .26 | .18 | -- |
Note. PCBD = Persistent Complex Bereavement Disorder, CLOC = Changing Lives of Older Couples, W1 = 6 months post-loss, W2 = 18 months post-loss, W3 = 48 months post-loss. The CLOC variables provided are for Wave 1 data.
For most CLOC variables, subjects either rated symptom frequency on a four point scale ranging from “never” to “often” or expressed their strength of agreement to statements on a four point scale ranging from “very true” to “not true.” For the latter, scores were reverse coded so that higher scores reflected greater agreement with the statement. For the question assessing symptom B3 (i.e., preoccupation with thoughts related to the deceased), subjects rated the frequency of thoughts on a six point scale ranging from “several times per day” to “never.” This item was reverse coded so that higher scores reflected greater frequency of thoughts. Where multiple variables assessed a symptom, we calculated the mean of those variables.
For Aim 1, we report both the mean rating for each symptom and the rate of symptom endorsement. For the majority of symptoms, we defined symptom presence as a rating of three or higher on the four-point scale (i.e., either experiencing the symptom at least “sometimes” or rating the statement as being at least “somewhat true”). For symptom B3, symptom presence was defined as endorsing thoughts several times per day.
Depression
Depression symptoms were assessed with a nine item version of the Center for Epidemiological Studies Depression scale (CESD; Radloff, 1977). Of the nine items, two were omitted because they reflected interpersonal difficulty (i.e., “I felt that people disliked me” and “people were unfriendly”) rather than symptoms of depression. An additional CESD item reflecting loneliness (i.e., “I felt lonely”) was included in the analyses, but was identified as a PCBD symptom (C9).
Risk Factors
In a previous study examining risk factors for PCBD using this data set, Bonanno and colleagues (2002) identified six pre-loss risk factors that distinguished those with low or absent grief at six months following the loss (i.e., resilience) from those with initially or persistently elevated grief symptoms (i.e., common grief and chronic grief, respectively). These baseline risk factors included three interpersonal risk factors (i.e., interpersonal dependence, spousal dependence, and instrumental social support) and three intrapersonal risk factors (i.e., emotional stability [neuroticism], belief in a just world, and acceptance of death). Here we examined each of these six risk factors assessed at baseline and their prospective associations with individual PCBD symptoms at 6, 18, and 48 months post-loss.
Interpersonal risk factors
Interpersonal dependence was measured by nine items from the Interpersonal Dependency Scale (CLOC variable v610; α = .66; Hirschfeld et al., 1977). Items assess thoughts, feelings, and behaviors related to the need to associate with valued others (e.g., “I don’t need much from other people”) and the perceived consequences if those social connections were lost (e.g., “I would feel hopeless if I were deserted by someone I love”). Spousal dependence was measured by three items created for the CLOC study (CLOC variable v711; α = .74). Items focus on the perceived consequences of losing the spouse (e.g., “I would feel completely lost if I didn’t have my [husband/wife]”). Instrumental support from family and friends was measured by three items directly querying the ability to rely on others to provide instrumental support if needed (e.g., “If you and your [husband/wife] needed extra help with general housework or home maintenance, how much could you count on friends or family members to help you?”; CLOC variable v652; α = .68).
Intrapersonal Risk Factors
Emotional stability was measured by eleven items from the neuroticism subscale of an abbreviated version of the NEO Personality Inventory (Cost & McCrae; 1992; CLOC variable v604; α = .70). Higher scores indicate greater emotional stability (and less neuroticism). Just world beliefs were measured by six items (e.g., “By and large, people get what they deserve”; CLOC variable v655; α = .76) and acceptance of death was measured by four items (e.g., “Death is simply a part of the process of life”; CLOC variable v656; α = .57) created for the CLOC study.
Statistical Analyses
Aim 2
To assess our second aim, we computed a series of networks with the R package qgraph (Epskamp, Cramer, Waldorp, Schmittmann, & Borsboom, 2012). Networks consist of two fundamental pieces: a set of elements, represented by nodes, and the relationships among those elements, represented by edges (i.e., the lines that connect the nodes). For each of the Aim 2 networks, nodes represented PCBD symptoms and edges represented the relationship between those symptoms. For each network, we used the mean rating as our assessment of each symptom rather than the dichotomized variable indicating symptom presence. Two types of networks were computed, distinguished by the types of relationship represented by the edges: association networks and relative importance networks.
Association networks
In an association network, an edge connecting two symptoms represents the zero-order correlation between them. Edges under r = .1 were omitted. The resultant network is weighted and undirected (i.e., it specifies the strength but not the direction of the relationship). The position of the nodes within the network is based on an algorithm that places nodes with stronger associations in the center of the network and nodes with weaker associations on the periphery of the network (Fruchterman & Reingold, 1991).
Relative importance networks
Association networks provide a helpful initial assessment of the relationships among symptoms. However, because correlations between two symptoms may arise from a causal relation between those symptoms, a shared association with a third symptom, or another third variable that contributes to both symptoms, association networks are limited in their ability to illuminate the causal structure of the syndrome. To better explore potential causal relationships among symptoms, we constructed a second type of network at each of the three waves of data collection. For these networks, edges represented the relative importance of a given symptom (X) as a predictor of another symptom (Y). Relative importance metrics quantify the contribution of a given regressor to the prediction of the criterion in multiple regression. In the current analyses, relative importance denotes the proportionate contribution that symptom X makes to R2 (where symptom Y is the criterion and the model includes all other PCBD symptoms), considering both the correlation between symptom X and symptom Y and the effect of symptom X on symptom Y adjusted for the other PCBD symptoms (for further discusssion of relative importance, see Johnson & LeBreton, 2004). By accounting for the influence of the other symptoms in the network, relative importance should better address the possibility that two symptoms are only associated because of their shared association with another symptom and, thereby, should better identify direct relationships among symptoms.
We used the R package relaimpo (Gromping, 2006) to compute relative importance, indexed by the normalized lmg metric (for further details regarding the calculation of lmg, see Gromping, 2006, pp. 9–12). The relative importance networks are weighted and directed (i.e., they specify both the strength and the direction of the relationship). Importantly, the direction of these relationships reflects the direction of prediction, not the direction of causality. As with the association networks, the relative importance networks were constructed with the R package qgraph (Epskamp et al., 2012) and nodes with stronger associations were placed in the center of the network while nodes with weaker connections were placed in the periphery. To our knowledge, this study is the first to define edges using relative importance.
Measures of node centrality
To quantify the importance of each symptom to the network, we calculated three indices of node centrality: strength, closeness, and betweenness. Node strength is the sum of the weights of the edges attached to that node. Closeness was calculated as the inverse of the mean of the shortest weighted path lengths between a given node and all other nodes in the network. Betweenness was calculated as the number of times in which a given node lies on the shortest path between two other nodes. Each index was calculated with the R package qgraph (Epskamp et al., 2012). For each index, higher values reflect greater centrality in the network.
Aim 3
To assess our third aim, we computed an association network at each of the three waves of data collection in which each node represented a symptom of either PCBD or depression. In addition, we used the spin glass algorithm (Reichardt & Bornholdt, 2006), γ = 1, start temperature = 1, stop temperature = .01, cooling factor = .99, spins = 19, to examine the community structure of the network that included each of these 19 symptoms. This analysis was conducted with the R package igraph (Csardi & Nepusz, 2006).
Aim 4
To explore paths by which known risk factors for grief or PCBD may influence the broader PCBD syndrome, we calculated the zero-order correlations between the risk factors and each of the PCBD symptoms at each wave of data collection. We used the Benjamini-Hochberg (B-H) procedure (Benjamini & Hochberg, 1995) to hold the false discovery rate at 5% for the 228 correlations between these risk factors and the PCBD symptoms.
Results
Subjects
Among the 265 subjects who participated in at least one of the three waves of data collection, most were Caucasian (84.5%) and female (85.3%). The mean age at the Wave 1 assessment was 70.2 years old (SD = 6.9). The mean duration of marriage at the baseline assessment was 42.9 years (SD = 12.9) and the Wave 1 assessments were conducted a mean of 37.3 months following the baseline assessment (SD = 18.2).
Symptoms in the Network
The mean scores and rates of endorsement for each symptom appear in Table 1. The most frequently endorsed symptoms across all three waves were yearning and a sense of diminished identity. The least frequently endorsed symptom across all three waves was avoidance. Subjects endorsed a mean of 4.56 (SD = 2.84), 3.29 (SD = 2.42), and 2.03 (SD = 2.09) symptoms at Waves 1, 2, and 3, respectively. The modal number of symptoms endorsed was 3, 3, and 0, at Waves 1, 2, and 3, respectively. Notably, endorsement rates for each symptom declined over time with the exception of C5 (i.e., regrets about the circumstances surrounding the loss).
Relationships Among Symptoms
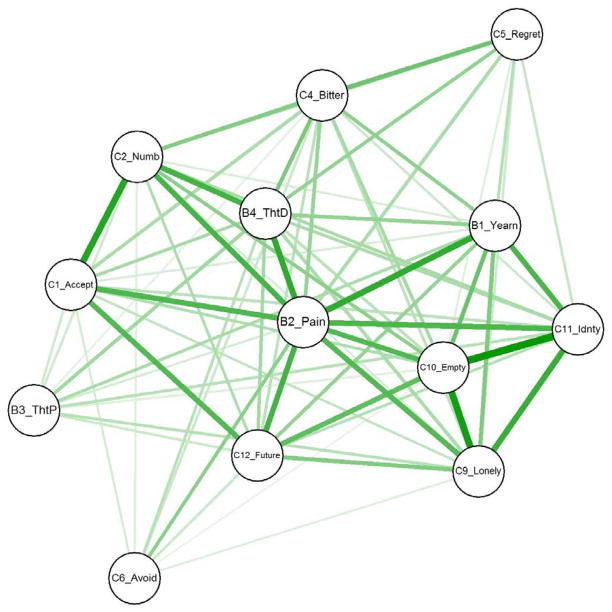
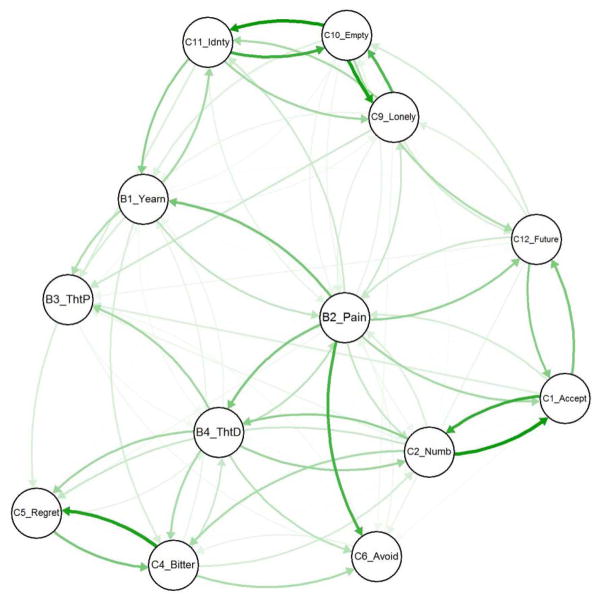
The association and relative importance networks for PCBD symptoms at 18 months post-loss appear in Figures 1 and 2, respectively. The strength, closeness, and betweenness of each symptom at each wave of data collection for the association networks and relative importance networks appear in Tables 3 and 4, respectively.
Figure 1.
Association network for symptoms of PCBD at 18 months post-loss. Each node represents a symptom. Each edge represents the zero-order correlation between two symptoms, and thickness signifies its magnitude. Edges under .1 were omitted from the network. Symptoms with stronger inter-symptom associations appear in the center for the network.
Figure 2.
Directed network for PCBD symptoms at 18 months post-loss. Each node represents a PCBD symptom. Each edge represents the relative importance of a symptom as a predictor of another symptom, and thickness signifies its magnitude. Edges under .05 were omitted from the networks. Arrows indicate the direction of prediction. Symptoms with stronger inter-symptom relative importance appear in the center for the network.
Table 3.
Indices of node centrality for the directed networks of persistent complex bereavement disorder symptoms at 6, 18, and 48-months post-loss
| W1: 6 months | W2: 18 months | W3: 48 months | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| PCBD Symptom | OS | C | B | OS | C | B | OS | C | B |
| B2: Emotional Pain | 1.75 | 0.0112 | 24 | 1.71 | 0.0110 | 30 | 1.55 | 0.0091 | 31 |
| B4: Thoughts Death | 1.68 | 0.0108 | 26 | 1.24 | 0.0086 | 17 | 1.25 | 0.0081 | 24 |
| C10: Life Empty | 1.56 | 0.0095 | 22 | 1.32 | 0.0073 | 7 | 1.25 | 0.0075 | 6 |
| C2: Numbness/Disbelief | 1.40 | 0.0091 | 12 | 1.25 | 0.0077 | 11 | 1.25 | 0.0066 | 8 |
| B1: Yearning | 0.86 | 0.0074 | 5 | 0.99 | 0.0082 | 12 | 0.84 | 0.0075 | 13 |
| C1: Difficulty Accepting | 1.10 | 0.0079 | 3 | 0.99 | 0.0079 | 7 | 1.21 | 0.0068 | 7 |
| C12: Future | 0.83 | 0.0070 | 0 | 0.97 | 0.0075 | 7 | -- | -- | -- |
| C11: Diminished Identity | 0.71 | 0.0059 | 6 | 1.04 | 0.0073 | 11 | 1.51 | 0.0081 | 2 |
| C4: Bitterness about loss | 0.82 | 0.0063 | 4 | 1.02 | 0.0063 | 9 | 0.91 | 0.0079 | 14 |
| C9: Loneliness | 0.86 | 0.0075 | 4 | 1.04 | 0.0066 | 1 | 0.51 | 0.0055 | 0 |
| B3: Thoughts Person | 0.71 | 0.0057 | 7 | 0.46 | 0.0042 | 0 | 0.55 | 0.0066 | 4 |
| C6: Avoidance | 0.50 | 0.0044 | 0 | 0.42 | 0.0046 | 0 | 0.58 | 0.0070 | 3 |
| C5: Regret | 0.22 | 0.0042 | 0 | 0.55 | 0.0049 | 0 | 0.60 | 0.0062 | 2 |
Note. PCBD = Persistent complex bereavement disorder; OS = Out Strength; C=Closeness; B=Betweenness. Network components are arranged in descending order of mean closeness across the three waves.
Table 4.
Pre-loss risk factors and their associations with symptoms of persistent complex bereavement disorder at 6, 18, and 48 months post-loss
| Interpersonal Risk Factors | Intrapersonal Risk Factors | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
| Dependence on Others | Dependence on Spouse | Instrumental Support | Emotional Stability | Acceptance of Death | Just World | ||||||||
|
| |||||||||||||
| W1 | W2 | W3 | W1 | W2 | W1 | W2 | W3 | W1 | W2 | W1 | W2 | W1 | |
| B1: Yearning | .21 | .26 | |||||||||||
| B2: Emotional Pain | .23 | .29 | .25 | .24 | −.19 | ||||||||
| B3: Thoughts Person | .17 | .21 | |||||||||||
| B4: Thoughts Death | .28 | .23 | .29 | ||||||||||
| C1: Difficulty Accepting | .19 | −.16 | |||||||||||
| C2: Numbness/Disbelief | .29 | .29 | .35 | −.23 | −.18 | −.17 | −.24 | ||||||
| C4: Bitterness about loss | .17 | ||||||||||||
| C5: Regret | −.17 | −.18 | −.20 | ||||||||||
| C9: Loneliness | .19 | .20 | −.29 | −.20 | −.33 | −.20 | |||||||
| C10: Life Empty/Meaningless | .20 | .28 | .25 | .20 | −.25 | −.24 | −.18 | −.20 | −.17 | −.25 | −.25 | ||
| C11: Diminished Identity | .16 | .23 | .29 | .18 | .19 | −.22 | |||||||
| C12: Future | .25 | .26 | -- | .26 | .24 | −.21 | −.23 | -- | |||||
Note. W1 = 6 months post-loss, W2 = 18 months post-loss, W3 = 48 months post-loss. Only correlations that remained statistically significant after controlling the false-discovery rate at 5% are displayed.
As noted above, the relative importance networks are weighted and directed; their edges specify both the strength and direction of the association between two symptoms, with the arrow originating at the predictor symptom and pointing toward the predicted symptom. Importantly, these arrows do not imply causality. For example, an arrow pointing from emotional pain (B2) to thoughts related to the death (B4) does not indicate that emotional pain causes thoughts related to the death. It merely denotes that emotional pain has a high level of relative importance as a predictor of thoughts related to the death.
Comorbidity
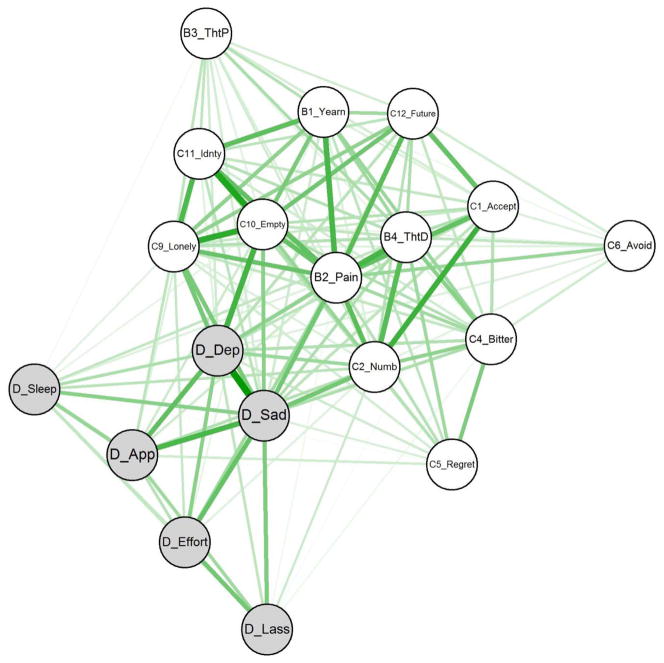
The association network for PCBD and depression symptoms at 18 months post-loss appears in Figure 3. The spin glass algorithm detected two communities of nodes in this network. One community comprised all 13 PCBD symptoms. The other comprised all 6 depression symptoms. Comparable results were obtained for the network at 6 and 48 months post-loss. At 6 months, the algorithm detected an identical community structure with the exception of the ‘loneliness’ symptom, which appeared in the community of depression symptoms. At 48 months, the algorithm detected 3 communities with the first comprising the 6 depression symptoms, the second comprising the majority of the PCBD symptoms, and the third comprising the PCBD symptoms C1 (i.e., difficulty accepting the loss) and C2 (i.e., disbelief or emotional numbness).
Figure 3.
Association network for PCBD and depression symptoms at 18 months post-loss. White nodes denote PCBD symptoms. Grey nodes denote depression symptoms. Each edge represents the zero-order correlation between two symptoms, and thickness signifies magnitude. Symptoms with stronger inter-symptom associations appear in the center for the network. D_Dep = depressed mood, D_Sad = sadness, D_Sleep = restless sleep, D_App = poor appetite, D_Effort = everything was an effort, D_Lass = lassitude.
Risk Factors
The zero-order correlations among the six pre-loss risk factors and each of the symptoms of PCBD appear in Table 4. Only those correlations that remained statistically significant after applying the B-H procedure are displayed. Each of the six previously identified risk factors for PCBD demonstrated a prospective association with at least one PCBD symptom, thereby providing some indication of how these risk factors may influence the broader syndrome.
Discussion
To our knowledge, this study is the first to examine the PCBD syndrome from a network perspective. Most fundamentally, our results support the syndromic integrity of PCBD and provide the first assessment of its network structure. In contrast to recent studies adopting a latent construct approach (e.g., Prigerson et al., 2009), our results suggest that emotional pain, rather than yearning, is the core symptom of PCBD. In addition, our results shed light on the prevalence of individual PCBD symptoms, their relations to one another, the relationship of the PCBD network to a network of depression symptoms, and the paths by which previously identified risk factors for PCBD may influence the syndrome. Below, we discuss each of these findings in more detail and conclude by providing suggestions for future research.
Review of Major Findings
Examining PCBD symptoms
The proportion of individuals reporting a given symptom provides an indication of the threshold for activation of that symptom. Higher frequency indicates a lower threshold of activation. Yearning and a sense of diminished identity were endorsed with notably greater frequency than each of the other symptoms. Indeed, yearning was endorsed by the majority of subjects, even at 48 months post-loss (cf. Horowitz et al., 1997, p. 906). These findings suggest that yearning and a sense of diminished identity have a low threshold of activation in conjugally bereaved adults and may act as “gateways” into the PCBD syndrome, initiating the cascade of activation among symptoms that produces emergence of the syndrome. However, the high frequency of these symptoms in the context of low overall symptom endorsement also suggests that the presence of these symptoms alone is unlikely to produce syndrome emergence.
Examining the PCBD network
The results of our network analyses are the core findings of this study, providing a first look at the network structure of PCBD. The structure of the network remained relatively consistent across all three waves of data collection. In addition, each PCBD symptom was significantly positively correlated with multiple symptoms in the network, supporting the syndromic integrity of PCBD.
Across network types, centrality indices, and waves of data collection, emotional pain was consistently the most central symptom. This finding dovetails with early clinical observations (e.g., Lindemann, 1994, p. 155). Indeed, Parkes (1972, p. 39) proposed that pangs of “severe anxiety and psychological pain” are “the most characteristic feature of grief.” However, this finding also contrasts with some recent conceptualizations of PCBD which have excluded emotional pain from the diagnostic criteria for this syndrome (e.g., Prigerson et al., 2009). This shift away from emotional pain in grief research is especially notable given recent advances in our understanding of the role played by pain affect in maintaining social attachments (Eisenberger, 2012). Our findings suggest that grief researchers should draw on these advances and more closely examine emotional pain in PCBD.
The relative importance network (see Figure 2) provides clues as to how emotional pain may influence the PCBD network. For example, emotional pain exhibited high relative importance as a predictor of avoidance, whereas yearning did not, suggesting that emotional pain may be the affective experience that drives grief-related avoidance. Emotional pain also strongly predicted thoughts related to the death, but did not exhibit high relative importance as a predictor of thoughts related to the deceased. Because efforts to avoid thoughts related to the death may have the ironic effect of heightening their accessibility (Wegner, 1994), these symptoms may constitute a positive feedback loop (i.e., thoughts about the death → emotional pain → avoidance → thoughts about the death) that contributes to the maintenance of the syndrome.
Interestingly, our results suggest the possibility of another self-reinforcing cycle. Just as emotional pain was a strong predictor of thoughts related to the death but not the deceased, yearning had high relative importance as a predictor of thoughts related to the deceased but not the death. Although there was no behavioral correlate of yearning in our data, proximity seeking (i.e., thoughts or behaviors aimed at increasing a sense of connection to the deceased) is a plausible behavioral consequence of yearning for the presence of the deceased. Excessive proximity seeking may, in turn, increase the accessibility of thoughts related to the deceased (Field, Nichols, Holen, & Horowitz, 1999), thereby creating a second positive feedback loop (i.e., thoughts about the deceased → yearning → proximity seeking → thoughts about the deceased) that maintains the syndrome. However, given the absence of proximity seeking in the current analyses, this possibility remains speculative.
Comorbidity
PCBD symptoms cohered as a community of symptoms distinguishable from the community of depression symptoms, providing additional evidence that PCBD is a syndrome distinct from depression. Importantly, however, there was also substantial overlap between the PCBD and depression syndromes. Feeling that life is empty or meaningless, loneliness, emotional pain, and disbelief or emotional numbness were especially strongly associated with sadness and depressed mood, thereby bridging the two networks and potentially contributing to the high rates of comorbid depression and PCBD (Simon et al., 2007). In contrast to the latent entity approach, which emphasizes the importance of symptoms that can act as efficient indicators of a specific latent entity (e.g., yearning in PCBD), the network approach awards greater significance to these bridge symptoms because of their ability to influence both networks and increase the likelihood of experiencing one when experiencing the other. Accordingly, our analyses suggest that feeling that life is empty or meaningless, loneliness, emotional pain, and emotional numbing may be especially important to consider in the context of comorbidity between PCBD and depression.
Risk Factors for PCBD
Grief researchers have identified numerous risk factors for PCBD. However, the mechanisms by which those risk factors affect the syndrome are unclear. The network approach has the potential to clarify these etiological pathways. From this approach, risk factors should influence PCBD either through its direct influence on particular symptoms or by modifying the relationships among symptoms in the network. Here, we investigated the former possibility for six previously identified risk factors for grief or PCBD by assessing their prospective associations with individual PCBD symptoms at 6, 18, and 48-months post-loss.
Interpersonal risk factors
Of the six risk factors examined, interpersonal dependence was associated with the greatest number of symptoms. Its strongest and most consistent associations were with emotional pain, thoughts about the death, feeling disbelief or emotional numbness, and a sense of diminished identity. It is worth considering these findings in the context of research on emotional (or social) pain. Eisenberger and Lieberman (2004) have posited that the pain affect experienced upon the loss of social connection, such as the death of a loved one, is part of a “neural alarm system” that detects, and prompts efforts to prevent, social separation. Because the cost of social separation would presumably be greatest among those with high interpersonal dependence, these individuals may be expected to experience elevated activity in this neural alarm system following loss (i.e., greater pain affect) and to devote heightened attention to the social disconnection (i.e., thoughts related to the death).
Much like interpersonal dependence, spousal dependence was associated with feelings that life is empty or meaningless, a sense of diminished identity, and difficulty imagining the future. The most notable difference between interpersonal and spousal dependence was in their associations with distinct types of cognitions. Whereas interpersonal dependence was associated with thoughts related to the death, spousal dependence was associated with thoughts related to the deceased. Together, the findings for spousal dependence suggest that those with greater dependence prior to the loss may be at risk for PCBD because of the increased risk for preoccupying thoughts related to the deceased and a sense that one’s identity, meaning in life, and plans for the future are lost without the deceased. These findings are in keeping with Maccallum and Bryant’s (2013) cognitive attachment model in which they posit that a merged identity with the deceased will enhance the accessibility of deceased-related memories and reduce the ability to imagine the future following loss.
A lack of instrumental social support prior to the loss was most strongly and consistently associated with increased loneliness. This finding is in keeping with past research on the association between social support and loneliness (Cacioppo et al., 2010). As discussed above, loneliness had associations with both the PCBD and the depression networks in our study. Accordingly, our results suggest the possibility that loneliness may be one path by which a lack of social support contributes to both the depression and PCBD syndromes.
Intrapersonal risk factors
Grief researchers have posited that individuals whose beliefs about themselves and the world can accommodate the death of a loved one may be less likely to attempt to find meaning in the death (Bonanno et al., 2002) and, consequently, may exhibit better adjustment to the loss (Davis, Wortman, Lehman, & Silver, 2000). Consistent with that possibility, we found that acceptance of death prior to the loss was negatively associated with two symptoms at both 6 and 18 months post-loss: feeling disbelief or emotional numbness and a feeling that life is empty or meaningless. Similarly, beliefs in a just world, which may aid in the persistence of hope that the world retains meaning despite personal tragedies (Wu et al., 2011), were negatively associated with feelings that life is empty or meaningless at 6 months post-loss.
Finally, emotional stability was most consistently negatively associated with emotional numbness and a feeling that life is empty or meaningless. In addition, it was the only risk factor other than interpersonal dependence that was associated with emotional pain at 18 months post-loss. Although the association was relatively small, the centrality of emotional pain to the PCBD network suggests that emotional stability and its association with emotional pain may, nonetheless be worthy of further study.
Limitations, Implications, and Future Directions
Individual elements of the PCBD network
The symptom prevalence rates reported here and elsewhere (e.g., Horowitz et al., 1997) provide information about the threshold for activation of PCBD symptoms and their persistence over time. However, there are limitations to our findings regarding the individual elements of the PCBD network. First, we used items from the CLOC survey to assess the proposed diagnostic criteria for PCBD. For most criteria, there was a close correspondence between the PCBD criterion (e.g., “feeling alone or detached from other individuals since the death”) and the CLOC item (e.g., “I feel lonely”). However, not all PCBD criteria were queried so directly and we could not identify an appropriate CLOC item for three PCBD criteria.
More fundamentally, the diagnostic criteria themselves were not intended to provide a comprehensive list of elements operative in this self-reinforcing network. Decisions about which items to include in the diagnostic criteria sets are made with motivations irrelevant or inconsistent with the network approach (e.g., excluding criteria that overlap with other mental disorders). Consequently, important items risk omission. As noted above, proximity seeking in response to yearning is a plausible symptom worth examining in the future, especially in the context of yearning and preoccupation with thoughts related to the deceased. Similarly, behavioral inactivity (i.e., a decrease in physical activity; cf. depressive avoidance; Boelen et al., 2006) is worthy of study in the PCBD network given its possible association with emptiness and emotional numbness, symptoms identified as being highly central to the PCBD syndrome.
In addition, many PCBD symptoms in the diagnostic criteria are poorly defined. For example, it is unclear whether emotional numbness denotes a generalized deficit in emotional responding or one confined to positive affect (cf. Litz, 1992). Even when precise, definitions vary among researchers. For example, Stroebe et al. (2010, p. 90) define yearning as “the extent to which one misses the person one lost,” whereas Carr and colleagues (2000, p. 200) define it as “an intermittent, recurrent, and obtrusive wish or need to recover the person who has died” (cf. Parkes, 1972, p. 42). This vagueness impedes measurement. Further exacerbating this problem, several symptoms conflate multiple phenomena under a single symptom. For example, Criterion C2 includes both experiencing disbelief and experiencing emotional numbness in regards to the loss. Surely, these are distinguishable experiences. Clear definitions and better measurement of individual elements of the PCBD network will be a critical foundational step in future research on PCBD.
PCBD network structure
Our results regarding the PCBD network identified emotional pain as playing a central role in the structure of PCBD. Accordingly, in future studies, researchers should aim to better understand this symptom and its relationship to other PCBD symptoms. Our results further suggest that the possibility of two feedback loops that may serve as the backbone of this disorder: the first comprising emotional pain, thoughts of the death, and avoidance and the second comprising yearning, thoughts of the deceased, and, potentially, proximity seeking. Although our findings are very preliminary in this regard, exploring the possibility of these feedback loops is likely to be a productive area in which to begin further examining the structure of PCBD. Finally, our results identified two additional groups of symptoms worthy of future study. Loneliness, a sense of diminished identity, and a feeling that life is empty or meaningless each exhibited high relative importance as predictors of one another. Similarly, difficulty accepting the death both predicted and was predicted by difficulty imagining the future and emotional numbness or disbelief regarding the death. In future studies, researchers should further examine these relationships to determine if these observed associations are the result of causal relationships among the symptoms, shared risk factors such as interpersonal or spousal dependence, or a combination of those influences.
Understanding the relations among symptoms is at the heart of the network approach. Network analyses (Newman, Barabási, & Watts, 2006), including intra-individual time-series data (Borsboom & Cramer, 2013), will advance our understanding of these relationships. However, researchers taking a network approach to understanding PCBD are not limited to using network analyses. Indeed, the best means of testing causality in the relationships among symptoms is simple experimental manipulation (e.g., does reducing loneliness diminish yearning?). We suspect that many different methods will ultimately be required to effectively unravel the causal web of PCBD symptoms.
Comorbidity with other mental disorders
Another productive area of research for those taking a network approach to PCBD will be the assessment of comorbidity between PCBD and other mental disorders. In this study, we focused on the comorbidity between PCBD and depression. However, PCBD is frequently comorbid with other syndromes, including anxiety disorders and PTSD. Researchers should examine the symptom overlap between these syndromes to determine if it is sufficient to account for the rates of co-occurrence between those disorders (Borsboom, Cramer, Schmittmann, Epskamp, & Waldorp, 2011) or if additional factors (e.g., shared risk factors) may also contribute to the high rates of comorbidity (see Cramer et al., 2010 for further discussion of the implications of a network approach for comorbidity among mental disorders).
Risk Factors
Our exploratory analysis of the associations among known risk factors for PCBD and the individual symptoms of PCBD provide some insight into how these risk factors may contribute to the emergence or maintenance of the broader PCBD syndrome. A complete analysis of these risk factors and their relationship to PCBD was beyond the scope of this study. For example, our analyses do not clarify whether the correlations we observed are direct effects on the symptom (e.g., interpersonal dependence directly contributing to emotional pain) or indirect effects through other symptoms (e.g., interpersonal dependence contributing to emotional pain through its effect on preoccupation with thoughts related to the death). In addition, we did not examine the possibility that these risk factors may influence the syndrome by modifying associations among symptoms. Nonetheless, our findings are a first step that can guide future research aimed at clarifying how these risk factors influence the PCBD syndrome.
Kendler (2005) advocated integrative pluralism (and “patchy reductionism”) as an appropriate investigative strategy for psychopathology research. Consistent with that position, we propose that researchers should strive to identify and piece together the many genetic, neurobiological, psychological, and social factors that contribute to specific PCBD symptoms or modify the relationships among them with the aim of clarifying small parts of the causal network that leads to the emergence of this syndrome. It will likely be productive to begin by examining factors likely to have moderate to large effects on symptoms central to the network, as those symptoms are, in turn, the most likely to contribute to syndrome emergence. Indeed, in our examination of the six risk factors previously associated with grief or PCBD, each was associated with at least one of the three most central symptoms in the PCBD network.
Treatment implications
The network approach has important clinical implications, pointing to key symptom targets whose resolution should produce beneficial effects that propagate through the network. Our analyses suggest that reducing emotional pain and thoughts related to the death are promising targets of intervention. In addition, the network approach may help to inform the mechanisms of change by which treatments have their effect on PCBD, an issue critical to our ability to treat this syndrome (Kazdin, 2007). In particular, using repeated assessments of individual symptoms over the course of treatment, researchers can identify (1) which symptoms are directly reduced by an intervention and (2) how those initial reductions propagate through the network.
Conclusion
The network (or causal system) approach is a promising new means of conceptualizing PCBD with noteworthy methodological and theoretical advantages over the latent variable approach. Most notably, it illuminates functional relations among symptoms – a phenomenon proscribed by latent variable approaches. Our analyses support the conceptualization of PCBD as a network of thoughts, feelings, and behaviors that overlap with, but are distinguishable from, symptoms of depression. Emotional pain was the symptom most central to this network, suggesting that this symptom may be an important target for treatment and a profitable starting point for researchers examining the etiology of this syndrome. Our findings further suggest that low emotional stability and greater interpersonal dependence may be two factors that contribute to persistent emotional pain following loss.
The findings reported here should be regarded only as a first step in examining PCBD from a network perspective. Our analyses were primarily descriptive and exploratory. Moreover, our reliance on cross-sectional analyses precluded us from confirming causal relationships among symptoms. Despite these limitations, our findings provide a first look at the network structure of PCBD and revealed patterns of association that can guide future research. In future studies, researchers should build on the findings reported here, making use of both network analysis and experimental manipulation to clarify the causal network of PCBD symptoms.
Table 2.
Indices of node centrality for the association network of persistent complex bereavement disorder symptoms at 6, 18, and 48-months post-loss
| W1: 6 months | W2: 18 months | W3: 48 months | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| PCBD Symptom | S | C | B | S | C | B | S | C | B |
| B2: Emotional Pain | 4.69 | 0.0301 | 8 | 4.40 | 0.0283 | 20 | 3.83 | 0.0307 | 18 |
| B4: Thoughts Death | 4.29 | 0.0283 | 16 | 3.55 | 0.0235 | 4 | 3.64 | 0.0281 | 6 |
| C10: Life Empty | 4.56 | 0.0284 | 4 | 3.70 | 0.0221 | 0 | 3.75 | 0.0291 | 8 |
| C2: Numbness/Disbelief | 4.32 | 0.0269 | 2 | 3.41 | 0.0220 | 2 | 3.04 | 0.0238 | 8 |
| C11: Diminished Identity | 3.08 | 0.0206 | 0 | 3.49 | 0.0220 | 0 | 3.72 | 0.0290 | 2 |
| B1: Yearning | 3.54 | 0.0228 | 0 | 3.40 | 0.0229 | 0 | 3.28 | 0.0258 | 0 |
| C4: Bitterness about loss | 3.52 | 0.0232 | 0 | 3.10 | 0.0203 | 0 | 3.38 | 0.0265 | 2 |
| C12: Future | 3.58 | 0.0232 | 0 | 3.22 | 0.0212 | 0 | -- | -- | -- |
| C9: Loneliness | 3.73 | 0.0240 | 0 | 3.45 | 0.0216 | 0 | 2.61 | 0.0201 | 0 |
| C1: Difficulty Accepting | 3.75 | 0.0232 | 0 | 3.14 | 0.0202 | 0 | 2.22 | 0.0184 | 0 |
| B3: Thoughts Person | 2.52 | 0.0180 | 0 | 2.18 | 0.0153 | 0 | 2.32 | 0.0202 | 0 |
| C5: Regret | 1.82 | 0.0143 | 0 | 2.26 | 0.0163 | 0 | 2.54 | 0.0208 | 0 |
| C6: Avoidance | 2.14 | 0.0168 | 0 | 1.87 | 0.0149 | 0 | 1.41 | 0.0180 | 0 |
Note. PCBD = Persistent complex bereavement disorder; S = Strength; C=Closeness; B=Betweenness. Network components are arranged in descending order of mean closeness across the three waves.
Acknowledgments
The Changing Lives of Older Couples study was supported by grants from the Nancy Pritzker Research Network and the National Institute of Aging (P1 AG05561-01). The work for this article was funded by a Sackler Scholarship in Psychobiology awarded to the first author.
References
- Association AP. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- Boelen PA, Huntjens RJC. Intrusive images in grief: An exploratory study. Clinical Psychology & Psychotherapy. 2008;15:217–226. doi: 10.1002/Cpp.568. [DOI] [PubMed] [Google Scholar]
- Boelen PA, van den Bout J. Complicated grief, depression, and anxiety as distinct postloss syndromes: A confirmatory factor analysis study. American Journal of Psychiatry. 2005;162:2175–2177. doi: 10.1176/appi.ajp.162.11.2175. [DOI] [PubMed] [Google Scholar]
- Boelen PA, van den Hout MA, van den Bout J. A cognitive-behavioral conceptualization of complicated grief. Clinical Psychology: Science and Practice. 2006;13:109–128. doi: 10.1111/j.1468-2850.2006.00013.x. [DOI] [Google Scholar]
- Bonanno GA, Wortman CB, Lehman DR, Tweed RG, Haring M, Sonnega J, Nesse RM. Resilience to loss and chronic grief: a prospective study from preloss to 18-months postloss. Journal of Personality and Social Psychology. 2002;83:1150–1164. doi: 10.1037/0022-3514.83.5.1150. [DOI] [PubMed] [Google Scholar]
- Borsboom D. Psychometric perspectives on diagnostic systems. Journal of Clinical Psychology. 2008;64:1089–1108. doi: 10.1002/jclp.20503. [DOI] [PubMed] [Google Scholar]
- Borsboom D, Cramer AO. Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology. 2013;9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- Borsboom D, Cramer AO, Schmittmann VD, Epskamp S, Waldorp LJ. The small world of psychopathology. PLoS One. 2011;6:e27407. doi: 10.1371/journal.pone.0027407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D, Mellenbergh GJ, van Heerden J. The theoretical status of latent variables. Psychological Review. 2003;110:203–219. doi: 10.1037/0033-295X.110.2.203. [DOI] [PubMed] [Google Scholar]
- Boyd R. Realism, anti-foundationalism and the enthusiasm for natural kinds. Philosophical Studies. 1991;61:127–148. doi: 10.1007/BF00385837. [DOI] [Google Scholar]
- Brown AD, Root JC, Romano TA, Chang LJ, Bryant RA, Hirst W. Overgeneralized autobiographical memory and future thinking in combat veterans with posttraumatic stress disorder. Journal of Behavior Therapy and Experimental Psychiatry. 2013;44:129–134. doi: 10.1016/j.jbtep.2011.11.004. [DOI] [PubMed] [Google Scholar]
- Burke LA, Neimeyer RA. Prospective risk factors for complicated grief. In: Stroebe M, Shchut H, van den Bout J, editors. Complicated grief: Scientific foundations for health care professionals. New York NY: Routledge; 2013. [Google Scholar]
- Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychology & Aging. 2010;25:453–463. doi: 10.1037/a0017216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: Cross-sectional and longitudinal analyses. Psychology & Aging. 2006;21:140–151. doi: 10.1037/0882-7974.21.1.140. [DOI] [PubMed] [Google Scholar]
- Carr D, House JS, Kessler RC, Nesse RM, Sonnega J, Wortman C. Marital quality and psychological adjustment to widowhood among older adults: A longitudinal analysis. The Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 2000;55:S197–207. doi: 10.1093/geronb/55.4.s197. [DOI] [PubMed] [Google Scholar]
- Cleiren M. Bereavement and adaptation: A comparative study of the aftermath of death. Washington, D.C: Hemisphere; 2003. [Google Scholar]
- Cramer AO, Waldorp LJ, van der Maas HL, Borsboom D. Comorbidity: A network perspective. Behavioral and Brain Sciences. 2010;33:137–150. doi: 10.1017/S0140525X09991567. [DOI] [PubMed] [Google Scholar]
- Csardi G, Nepusz T. The igraph software package for complex network research. International Journal of Complex Systems. 2006:1695. [Google Scholar]
- Davis CG, Wortman CB, Lehman DR, Silver RC. Searching for meaning in loss: Are clinical assumptions correct? Death Studies. 2000;24:497–540. doi: 10.1080/07481180050121471. [DOI] [PubMed] [Google Scholar]
- Eisenberger NI. The neural bases of social pain: evidence for shared representations with physical pain. Psychosomatic Medicine. 2012;74:126–135. doi: 10.1097/PSY.0b013e3182464dd1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberger NI, Lieberman MD. Why rejection hurts: a common neural alarm system for physical and social pain. Trends in Cognitive Sciences. 2004;8:294–300. doi: 10.1016/j.tics.2004.05.010. [DOI] [PubMed] [Google Scholar]
- Epskamp S, Cramer AO, Waldorp LJ, Schmittmann VD, Borsboom D. Qgraph: Network visualizations of relationships in psychometric data. Journal of Statistical Software. 2012;48:1–18. [Google Scholar]
- Field NP, Nichols C, Holen A, Horowitz MJ. The relation of continuing attachment to adjustment in conjugal bereavement. Journal of Cosulting and Clinical Psychology. 1999;67:212–218. doi: 10.1037//0022-006x.67.2.212. [DOI] [PubMed] [Google Scholar]
- Fruchterman TMJ, Reingold EM. Graph Drawing by Force-Directed Placement. Software-Practice & Experience. 1991;21:1129–1164. doi: 10.1002/spe.4380211102. [DOI] [Google Scholar]
- Gromping U. Relative importance for linear regression in R: The package relaimpo. Journal of Statistical Software. 2006;17 [Google Scholar]
- Gyurak A, Gross JJ, Etkin A. Explicit and implicit emotion regulation: A dual-process framework. Cognition & Emotion. 2011;25:400–412. doi: 10.1080/02699931.2010.544160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschfeld RMA, Klerman GL, Gough HG, Barrett J, Korchin SJ, Chodoff P. A measure of interpersonal dependency. Journal of Personality Assessment. 1977;41:610–618. doi: 10.1207/s15327752jpa4106_6. [DOI] [PubMed] [Google Scholar]
- Horowitz MJ, Siegel B, Holen A, Bonanno GA, Milbrath C, Stinson CH. Diagnostic criteria for complicated grief disorder. American Journal of Psychiatry. 1997;154:904–910. doi: 10.1176/ajp.154.7.904. [DOI] [PubMed] [Google Scholar]
- Howes OD, Kapur S. The dopamine hypothesis of schizophrenia: version III--the final common pathway. Schizophrenia Bulletin. 2009;35:549–562. doi: 10.1093/schbul/sbp006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JW, LeBreton JM. History and use of relative importance indices in organizational research. Organizational Research Methods. 2004;7:238–257. doi: 10.1177/1094428104266510. [DOI] [Google Scholar]
- Kashdan TB, Elhai JD, Frueh BC. Anhedonia and emotional numbing in combat veterans with PTSD. Behavior Research and Therapy. 2006;44:457–467. doi: 10.1016/j.brat.2005.03.001. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology. 2007;3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- Kendler KS. Toward a philophical structure for psychiatry. American Journal of Psychiatry. 2005;162:433–440. doi: 10.1176/appi.ajp.162.3.433. [DOI] [PubMed] [Google Scholar]
- Kendler KS. The dappled nature of causes of psychiatric illness: Replacing the organic-functional/hardware-software dichotomy with empirically based pluralism. Molecular Psychiatry. 2012;17:377–388. doi: 10.1038/mp.2011.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Zachar P, Craver C. What kind of things are psychiatric disorders? Psychological Medicine. 2011;41:1143–1150. doi: 10.1017/S0033291710001844. [DOI] [PubMed] [Google Scholar]
- Kersting A, Brahler E, Glaesmer H, Wagner B. Prevalence of complicated grief in a representative population-based sample. Journal of Affective Disorders. 2011;131:339–343. doi: 10.1016/j.jad.2010.11.032. [DOI] [PubMed] [Google Scholar]
- Lindemann E. Symptomatology and management of acute grief. 1944. American Journal of Psychiatry. 1994;151:155–160. doi: 10.1176/ajp.151.6.155. [DOI] [PubMed] [Google Scholar]
- Litz BT. Emotional numbing in combat-related posttraumatic-stress-disorder: A critical-review and reformulation. Clinical Psychology Review. 1992;12:417–432. doi: 10.1016/0272-7358(92)90125-R. [DOI] [Google Scholar]
- Maccallum F, Bryant RA. A Cognitive Attachment Model of prolonged grief: Integrating attachments, memory, and identity. Clinical Psychology Review. 2013;33:713–727. doi: 10.1016/j.cpr.2013.05.001. [DOI] [PubMed] [Google Scholar]
- McNally RJ. What is mental illness? Cambridge, MA: The Belknap Press of Harvard University Press; 2011. [Google Scholar]
- Momartin S, Silove D, Manicavasagar V, Steel Z. Complicated grief in Bosnian refugees: Associations with posttraumatic stress disorder and depression. Comprehensive Psychiatry. 2004;45:475–482. doi: 10.1016/j.comppsych.2004.07.003. [DOI] [PubMed] [Google Scholar]
- Newman MEJ, Barabási A-Ls, Watts DJ. The structure and dynamics of networks. Princeton: Princeton University Press; 2006. [Google Scholar]
- Parkes CM. Bereavement: Studies of grief in adult life. International Universities Press; 1972. [Google Scholar]
- Prigerson HG, Horowitz MJ, Jacobs SC, Parkes CM, Aslan M, Goodkin K, Maciejewski PK. Prolonged grief disorder: Psychometric validation of criteria proposed for DSM-V and ICD-11. PLoS Med. 2009;6:e1000121. doi: 10.1371/journal.pmed.1000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Reichardt J, Bornholdt S. When are networks truly modular? Physical Review E. 2006;74:016110. doi: 10.1016/j.physd.2006.09.009. [DOI] [Google Scholar]
- Reynolds M, Brewin CR. Intrusive memories in depression and posttraumatic stress disorder. Behavior Research and Therapy. 1999;37:201–215. doi: 10.1016/S0005-7967(98)00132-6. [DOI] [PubMed] [Google Scholar]
- Robinaugh DJ, McNally RJ. Remembering the past and envisioning the future in bereaved adults with and without complicated grief. Clinical Psychological Science. 2013;3:290–300. doi: 10.1177/2167702613476027. [DOI] [Google Scholar]
- Shear K, Frank E, Houck PR, Reynolds CF., 3rd Treatment of complicated grief: a randomized controlled trial. Journal of the American Medical Association. 2005;293:2601–2608. doi: 10.1001/jama.293.21.2601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shear K, Monk T, Houck P, Melhem N, Frank E, Reynolds C, Sillowash R. An attachment-based model of complicated grief including the role of avoidance. European Archives of Psychiatry and Clinical Neuroscience. 2007;257:453–461. doi: 10.1007/s00406-007-0745-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shear K, Simon N, Wall M, Zisook S, Neimeyer R, Duan N, Keshaviah A. Complicated grief and related bereavement issues for DSM-5. Depression & Anxiety. 2011;28:103–117. doi: 10.1002/da.20780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon NM, Shear KM, Thompson EH, Zalta AK, Perlman C, Reynolds CF, Silowash R. The prevalence and correlates of psychiatric comorbidity in individuals with complicated grief. Comprehensive Psychiatry. 2007;48:395–399. doi: 10.1016/j.comppsych.2007.05.002. [DOI] [PubMed] [Google Scholar]
- Solomon Z, Dekel R. The contribution of loneliness and posttraumatic stress disorder to marital adjustment following war captivity: A longitudinal study. Family Process. 2008;47:261–275. doi: 10.1111/j.1545-5300.2008.00252.x. [DOI] [PubMed] [Google Scholar]
- Stroebe W, Abakoumkin G, Stroebe M. Beyond depression: Yearning for the loss of a loved one. Omega. 2010;61:85–101. doi: 10.2190/OM.61.2.a. [DOI] [PubMed] [Google Scholar]
- Wegner DM. Ironic Processes of Mental Control. Psychological Review. 1994;101:34–52. doi: 10.1037/0033-295x.101.1.34. [DOI] [PubMed] [Google Scholar]
- Williams J, Barnhofer MG, Crane T, Herman C, Raes D, Watkins F, Dalgleish T. Autobiographical memory specificity and emotional disorders. Psychological Bulletin. 2007;133:122–148. doi: 10.1037/0033-2909.133.1.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson TD, Gilbert DT. Explaining away a model of affective adaptation. Perspectives on Psychological Science. 2008;3:370–386. doi: 10.1111/j.1745-6924.2008.00085.x. [DOI] [PubMed] [Google Scholar]
- Wu MS, Yan XD, Zhou C, Chen YW, Li J, Zhu ZH, Han BX. General Belief in a Just World and Resilience: Evidence from a Collectivistic Culture. European Journal of Personality. 2011;25:431–442. doi: 10.1002/Per.807. [DOI] [Google Scholar]
- Zachar P, Kendler KS. Psychiatric disorders: A conceptual taxonomy. American Journal of Psychiatry. 2007;164:557–565. doi: 10.1176/appi.ajp.164.4.557. [DOI] [PubMed] [Google Scholar]