Abstract
Objective:
To review new incidental findings detected on low-resolution CT attenuation correction (CTAC) images acquired during single-photon emission CT (SPECT-CT) myocardial perfusion imaging (MPI) and to determine whether the CTAC images had diagnostic value and warrant reporting.
Methods:
A multicentre study was performed in four UK nuclear medicine departments. CTAC images acquired as part of MPI performed using SPECT were evaluated to identify incidental findings. New findings considered to be clinically significant were evaluated further. Positive predictive value (PPV) was determined at the time of definitive diagnosis.
Results:
Of 1819 patients studied, 497 (27.3%) had a positive CTAC finding. 51 (2.8%) patients had findings that were clinically significant at the time of the CTAC report and had not been previously diagnosed. Only four (0.2%) of these were potentially detrimental to patient outcome.
Conclusion:
One centre had a PPV of 0%, and the study suggests that these CTAC images should not be reported. Two centres with more modern equipment had low PPVs of 0% and 6%, respectively, and further research is suggested prior to drawing a conclusion. The centre with best quality CT had a PPV of 67%, and the study suggests that CTAC images from this equipment should be reported.
Advances in knowledge:
This study is unique compared with previous studies that have reported only the potential to identify incidental findings on low-resolution CT images. This study both identifies and evaluates new clinically significant incidental findings, and it demonstrates that the benefit of reporting the CTAC images depends on the type of equipment used.
Myocardial perfusion imaging (MPI) performed using single-photon emission CT (SPECT) is often subject to artefacts owing to the scatter and absorption of photons prior to detection. These artefacts can mimic myocardial perfusion defects leading to false-positive findings. It has been demonstrated that CT attenuation correction (CTAC) can compensate for these errors in SPECT MPI, resulting in image quality improvement and more accurate diagnosis.1,2 The low-resolution/low-dose CT scan is performed through the area of the chest, which is aligned with the SPECT scan of the heart, so only a limited CT scan of the thorax is acquired. CT images are essentially a by-product of the attenuation correction (AC) process, the CT acquisition being primarily for AC purposes.
Acquisition using a low tube current (mA) and large slice thickness results in images that have low signal-to-noise ratio, poor spatial resolution and an increased potential for partial volume artefacts compared with those of diagnostic CT studies. Motion artefacts may also be evident, as patients are not required to hold their breath during the CT acquisition. The resulting images are adequate for the purpose for which they have been acquired but are often not considered to be of diagnostic quality. The latest guidelines from the British Nuclear Cardiology Society suggest that if the CTAC images are of diagnostic quality, then it is good practice to review them according to a local policy,3 but the guidelines do not specify what constitutes “diagnostic quality”. However, the CTAC images often reveal incidental findings.4,5 This would suggest that whilst the images are of lower quality than a diagnostic CT scan, they could potentially have some diagnostic value.
In the UK, the ionizing radiation (medical exposure) regulations 20006 stipulate that each medical radiation exposure should be evaluated and a record kept of any findings. Although this implies that CTAC images should be reported, this is ambiguous because of the non-diagnostic nature of the images and lack of professional body guidance.3,7
The objectives of this study were:
(1) to review the new incidental findings that were detected on low-resolution CTAC images acquired during SPECT-CT MPI that were thought to be clinically significant at the time of reporting.
(2) to determine whether the CTAC images had diagnostic value and warranted reporting.
In this study, we considered “clinically significant” to mean that there was a high suspicion that the pathology, if any, underlying the incidental radiological finding could impact negatively on patient well being and that further investigation was required.
METHODS AND MATERIALS
A multicentre study of four UK nuclear medicine departments was carried out. Low-resolution CTAC images from all SPECT MPI studies acquired between 1 July 2010 and 30 June 2011 were included in the study and evaluated in order to determine the number of incidental findings. All patients referred for MPI with CTAC whose examination resulted in a written report by a consultant radiologist were included. Their demographics are indicated in Table 1. The mean ages of the patients were similar and typical of patients undergoing CTAC for MPI.
Table 1.
Patient demographics
| Technical specifications | Centre |
||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | All | |
| Male:female | 1:0.8 | 1:0.9 | 1:0.9 | 1:0.5 | 1:0.8 |
| Mean age (years) | 62.6 | 69.6 | 64.9 | 66.5 | 65.9 |
| Age range (years) | 36–85 | 40–91 | 25–89 | 42–83 | 25–91 |
To reduce inter-interpreter reporting bias, studies were reported by a consultant radiologist. A proforma informed by the Royal College of Radiologists guidance8 was used to determine the content and structure of the written consultant report. Each report stated that the images formed part of a low-resolution/low-quality CT that was produced as part of a nuclear medicine myocardial perfusion study. This ensured that it was clear to any clinician reading the report that the CT scan had not been performed for diagnostic purposes. Both non-significant and potentially significant abnormalities were noted in the report and if there was no abnormality detected, this was also noted. Identification of previously unknown significant findings was communicated9 and managed in accordance with the policy of each individual hospital.
The four consultant radiologists held regular case discussion meetings where they were able to share interesting cases and discuss discrepancies. This, in addition to the use of the standard proforma, helped to ensure reporting concurrence and so provide a method of quality assurance.8
As incidental findings were possible in any of the tissues within the thorax, the images were reviewed on a variety of CT window settings in order to adequately visualize lung, bone and soft tissue.
After taking advice from the Health Research Authority, approval for this study was sought locally from each participating hospital and was granted as medical audit from one centre and as service evaluation from the other three centres. Ethical approval was obtained from the University of Salford, Salford, UK.
Technical scanning parameters
The SPECT-CT equipment installed in the four centres utilized CT scanners with varying capabilities. Scan parameters for each CT system are shown in Table 2. Centre 1 used a GE Infinia™ Hawkeye™ (GE Healthcare, Buckinghamshire, UK) one-slice incremental CT scanner. The parameters available with this scanner were the most limited. The CT images from Centres 2 and 3 were acquired using a GE Infinia Hawkeye 4 System, which had a four-slice multidetector CT (MDCT) scanner. The scan parameters available were still limited, and the available tube currents were 1.0, 1.5, 2.0 and 2.5 mA. Centre 4 utilized a Philips Precedence 16-slice MDCT (Philips Healthcare, Guildford, UK) with the availability for diagnostic parameters to be selected.
Table 2.
Scan parameters of the single-photon emission CT-CT systems
| Technical specifications | Centre |
||
|---|---|---|---|
| 1 | 2 and 3 | 4 | |
| Scanner | GE Infinia Hawkeye 1 one-slice | GE Infinia Hawkeye 4 four-slice | Philips Precedence 16-slice |
| Tube potential (kV) | 120.0 | 120.0 | 120.0 |
| mA | 2.5 | 1.5 | ∼33 |
| Rotation time (s) | 18.0 | 30.0 | 1.5 |
| Effective mAs | 45.0 | 24.0 | 50.0 |
| Acquired slice thickness (mm) | 10.0 | 5.0 | 1.5 |
| Reconstructed slice (mm) | 10.0 | 6.1 | 5.0 |
| Pitch | 1.0 | 1.9 | 0.98 |
| Contrast-to-noise ratio | 2.4 | 2.2 | 0.74 |
| Low-contrast resolution | 3 mm | 4 mm | 4 mm |
| High-contrast resolution | ≥4 lp cm−1 | ≥3 lp cm−1 | ≥24 lp cm−1 |
lp, line pairs.
GE Infinia™ Hawkeye™ (GE Healthcare, Buckinghamshire, UK), Philips Precedence (Philips Healthcare, Guildford, UK).
The GE Infinia Hawkeye 1 used a low tube current of 2.5 mA in axial mode (effective pitch of 1), with a tube rotation time of 30 s. Half-scan mode was utilized, meaning that the X-ray tube was only “on” for 18 s per slice, corresponding to an effective 45 mAs. The GE Infinia Hawkeye 4 scanner used 1.5 mA in helical mode with a pitch of 1.9, which equates to an effective 24 mAs. The Philips Precedence 16-slice scanner used approximately 33 mA with a rotation time of 1.5 s and a pitch of 0.98 to produce 50 mAs. The acquired slice thickness and pitch used with the Philips Precedence was similar to diagnostic MDCT although the reconstructed slice thickness was close to the reconstructed slice thickness of the Infinia Hawkeye 4. The Infinia Hawkeye 4 used a larger acquired slice thickness and pitch and the Infinia Hawkeye 1 had the largest acquired slice thickness of 10 mm.
Acquisition using a large slice thickness and the use of a large pitch both contribute to reduced spatial resolution and the potential for increased partial volume averaging. Also, the Hawkeye acquisitions were performed with the patient free breathing, whereas the Philips Precedence images were acquired with a breath hold. It was therefore expected that the CTAC images produced by the Infinia Hawkeye systems would have reduced quality relative to the CTAC images produced by the Philips Precedence CT. This would be consistent with findings from a lesion detection study performed by Thompson et al,10 using an anthropomorphic phantom to acquire images on different SPECT-CT systems. The SPECT-CT systems were operated with site-specific acquisition parameters and observer performance of lesion detection was found to correlate with variation in CTAC protocols.
Image evaluation
From the four centres, a total of 1819 patients were reported and included in this study. If patients had both stress and rest studies performed, these were considered as one examination for the purpose of this study. The radiologists' written reports were reviewed retrospectively. Reports that identified only previously known pathology were not included in the final evaluation because, if necessary, this pathology would be followed up with diagnostic CT as part of the patient's routine management. Review of the CTAC images would not influence management for these patients. In addition, CTAC images are not suited to longitudinal assessment of pathology and so could not substitute for diagnostic CT as a follow-up tool. Therefore, only findings of previously unknown conditions were considered; we have called these new positive findings.
Patients who had positive findings were noted, and their case history records were then reviewed. New positive findings were classified according to the clinical significance at the time of report. The classification system was adapted from the one used by Goetze et al11 and is shown in Table 3.
Table 3.
Classification of findings
| Classification | Description |
|---|---|
| Major (clinically significant) | Requires further investigation in view of clinical information and history. This includes findings such as pleural effusions or lung nodules |
| Minor | Less significant than major findings; however, they do have clinical significance. For example, cardiomegaly, liver lesions or hiatus hernia |
| Minimal | Less significant than minor findings, minimal or no clinical significance given patient history. These include degenerative changes |
| Equivocal | Findings unclear. These include abnormalities in the liver that cannot be characterized. |
Only findings that were classified as major were considered to be clinically significant and warranted follow-up. Potentially, these findings could affect the clinical management of the patient. For the purposes of this analysis, only major findings of pathology that were not previously known have been considered as significant new incidental findings. All other findings were considered to be insignificant.
The primary outcome was to determine the positive predictive value (PPV) of the CTAC images for patients who had clinically significant new positive findings. These patients all received follow-up procedures (e.g. diagnostic CT, plain radiographs or interventional procedures) over a period of up to 2 years. This enabled assessment of the final diagnostic outcome in these patients, which in turn informed the value of interpreting the CTAC images. It was not possible, either practically or ethically, to follow-up patients who had no positive findings on the CTAC images, and so this study could not determine the number of true- and false-negative results.
In order to indicate the performance of detecting pathology on the CTAC images that would be detrimental to the patient if undetected, the PPV has been calculated at the time the definitive diagnosis was made, rather than at the time of the CTAC report. Therefore, PPV was calculated as the percentage of new significant findings, which ultimately affected patient outcome.
RESULTS
Table 4 summarizes the results. Out of 1819 patients studied, 497 (27%) had a positive finding of any type, of which 423 (23%) were new findings. 51 (2.8%) patients had findings that were considered clinically significant at the time of CTAC report and which had not been previously diagnosed. However, only 4 (0.2%) of these findings had the potential to be detrimental to patient outcome.
Table 4.
Number of incidental CT attenuation correction findings
| Technical specifications | Centre |
||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | Total | |
| Total number of patients in study | 322 | 1011 | 275 | 211 | 1819 |
| Number with positive findings | 212 | 190 | 71 | 24 | 497 |
| Number with new positive findings | 202 | 158 | 43 | 20 | 423 |
| Clinically significant findings | 12 | 31 | 5 | 3 | 51 |
| Minor findings | 62 | 66 | 31 | 2 | 161 |
| Minimal findings | 126 | 48 | 7 | 14 | 195 |
| Equivocal findings | 2 | 13 | 0 | 1 | 16 |
| Confirmed clinically significant | 0 | 2 | 0 | 2 | 4 |
| Positive predictive value | 0% | 6% | 0% | 67% | 8% |
Although there was a much higher number of findings that were considered to be significant new incidental findings at the time of the CTAC scan, many of these pathologies resolved, remained stable (no change in size or appearance that might otherwise suggest malignancy) or proved to be insignificant when the patient was followed up.
Location and characterization of new significant incidental findings
Only 51 out of 497 (10%) positive findings were both new and clinically significant. The location of these findings fell into three categories: pulmonary (7.8%), cardiovascular (1.8%) and paraspinal (0.4%) (Table 5). The most common lesions detected on CTAC were pulmonary in nature and included pulmonary nodules (2.2%), effusion (2.0%), consolidation (1.6%), pulmonary mass (0.6%), lung metastases (0.4%), ground glass opacities (GGO) (0.2%), atelectasis (0.2%), pneumonia (0.2%) and lobar collapse (0.2%). Findings within the cardiovascular system were predominantly coronary artery calcifications (1.6%), but there was also one aortic aneurysm detected (0.2%). The two paraspinal lesions were masses located adjacent to the thoracic vertebrae (0.4%).
Table 5.
Characterization of significant new CT attenuation correction findings
| Lesion type | Technical specifications | Centre |
||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | Total | ||
| Pulmonary | Nodules | 3 | 3 | 2 | 3 (2) | 11 |
| Mass | 3 (1) | 3 | ||||
| Lung metastases | 2 (1) | 2 | ||||
| Ground glass opacities | 1 | 1 | ||||
| Atelectasis | 1 | 1 | ||||
| Effusion | 1 | 8 | 1 | 10 | ||
| Consolidation | 6 | 2 | 8 | |||
| Ill defined | 2 | 2 | ||||
| Pneumonia | 1 | 1 | ||||
| Lobar collapse | 1 | 1 | ||||
| Total | 10 (0) | 22 (2) | 5 (0) | 3 (2) | 40 (4) | |
| Cardiovascular | Aortic aneurysm | 1 | 1 | |||
| Coronary artery calcification | 8 | 8 | ||||
| Total | 1 (0) | 8 (0) | 9 (0) | |||
| Paraspinal | Mass | 1 | 1 | 2 | ||
| Total | 1 (0) | 1 (0) | 2 (0) | |||
Numbers in parentheses represent the number of patients whose outcome was affected by the significant new finding.
DISCUSSION
Out of 1819 patients undergoing SPECT-CT MPI studies, 423 patients (23%) had some abnormality found on the CT image that was not previously known. Of these, 51 (2.8%) were serious enough to require further investigation. However, after follow-up, the significance of the diagnosis for 47 of these patients was downgraded, leaving only 4 (0.2%) with confirmed clinically significant pathology. Three patients (0.16%) had life-threatening pathologies that were treated as a result of their detection on CTAC images. One patient (0.05%) was diagnosed with a condition that had advanced beyond curative treatment.
Centre 1 used an Infinia Hawkeye 1-slice CT system. Out of 322 patients, they found 12 who were considered to have new significant incidental findings at the time of the report. However, on follow-up, none of these findings was considered to be significant. Six patients had consolidation that resolved over time, and one had a pleural effusion that also resolved. Three patients were reported to have pulmonary nodules, but on follow-up, two cases were found to be owing to fibrotic changes or atelectasis, and in the third case the lesion was benign rheumatoid in nature (Figure 1). This was confirmed on diagnostic MDCT (Figure 2) along with a further lesion in the left upper lobe (Figure 3), which was not within the area of the CTAC acquisition. The lesions were surgically resected before a diagnosis of a benign condition was made. There was also a paraspinal mass that was considered insignificant when followed up and an aortic aneurysm that did not warrant follow-up.
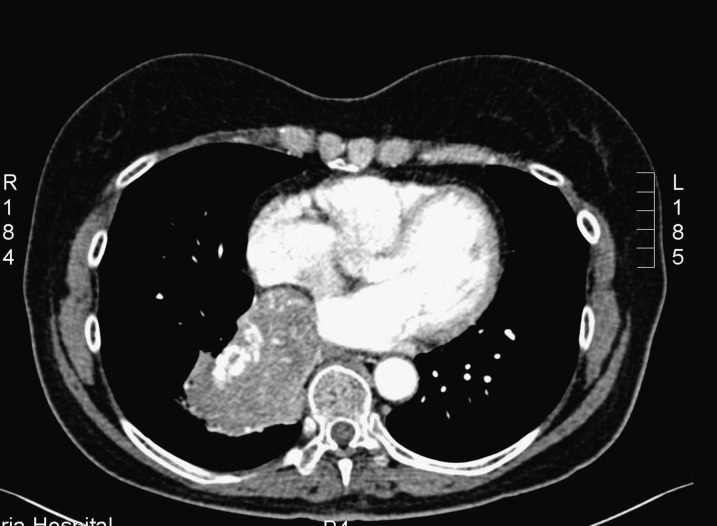
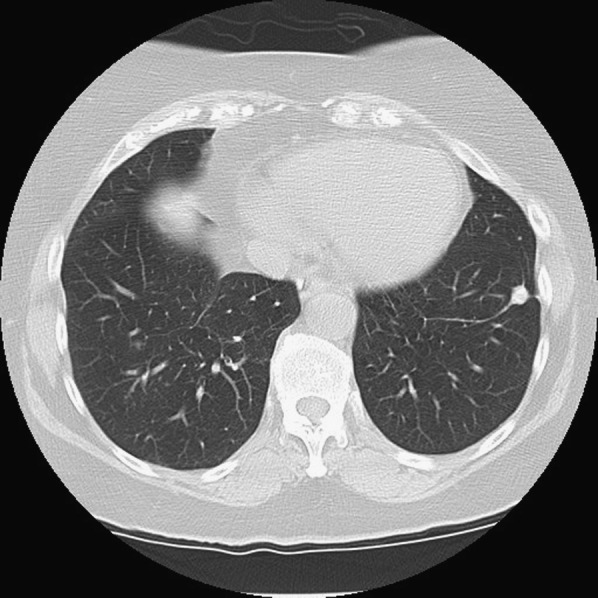
Figure 1.

Patient from Centre 1. CT attenuation correction image acquired using GE Infinia™ Hawkeye™ (GE Healthcare, Buckinghamshire, UK) one-slice single-photon emission CT-CT system, which reveals a single pulmonary nodule in the left lower lobe. This was confirmed by diagnostic CT (Figure 2).
Figure 2.
The same patient as in Figure 1. Diagnostic multidetector CT confirming diagnosis of pulmonary lesion detected on the CT attenuation correction acquisition.
Figure 3.
The same patient as in Figures 1 and 2. Diagnostic multidetector CT demonstrating a further lesion in the left upper lobe.
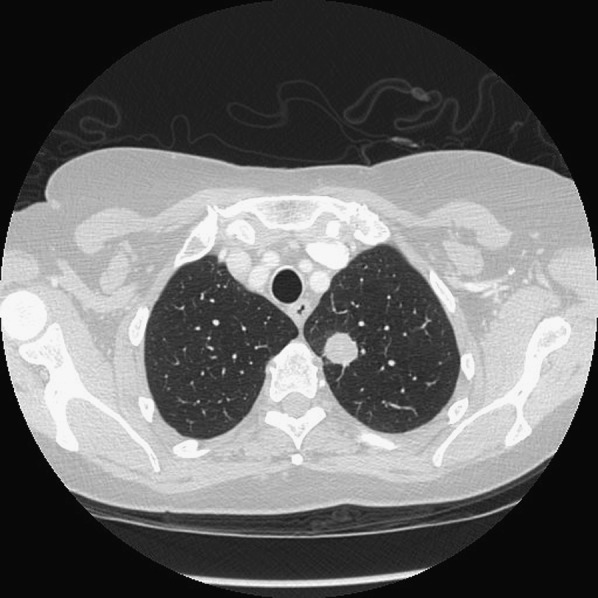
Centre 2 used an Infinia Hawkeye 4-slice CT system. Out of 1011 patients, they found 31 who were considered to have new significant incidental findings at the time of the report. However, only two had clinically significant pathology. One patient was reported to have a pulmonary mass on the initial CTAC images (Figure 4). This was confirmed with diagnostic MDCT (Figure 5) and MR, which demonstrated invasion of the right atrium with involvement of the atrial septum. The mass was resected and confirmed as a 5-cm carcinoid lesion.
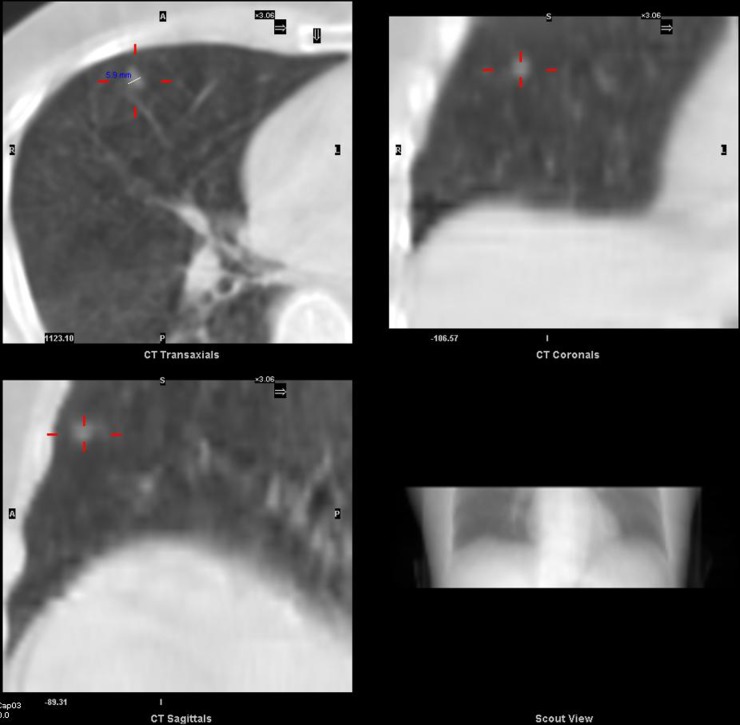
Figure 4.

Patient from Centre 2. CT attenuation correction image (lung windows) from cardiac single-photon emission CT-CT study using GE Infinia™ Hawkeye™ (GE Healthcare, Buckinghamshire, UK) four-slice demonstrating mass in right lower lobe abutting the heart.
Figure 5.
The same patient as in Figure 4. Contrast-enhanced diagnostic multidetector CT image demonstrating lung mass with serpiginous vessels.
The second case at Centre 2 with clinically significant pathology was confirmed as lung metastases from pancreatic cancer. There was a further case of suspected pulmonary metastases, which was later found to be Wegner's granulomatosis. Three lung nodules at the time of report were considered to be insignificant at follow up. As with Centre 1, pulmonary effusions and consolidations considered to be significant at the time of the report had often resolved on follow-up imaging. One case of lobar collapse was thought to be long standing. There were eight cardiovascular cases that were considered significant in the CTAC report, but this was not thought to be the case subsequently.
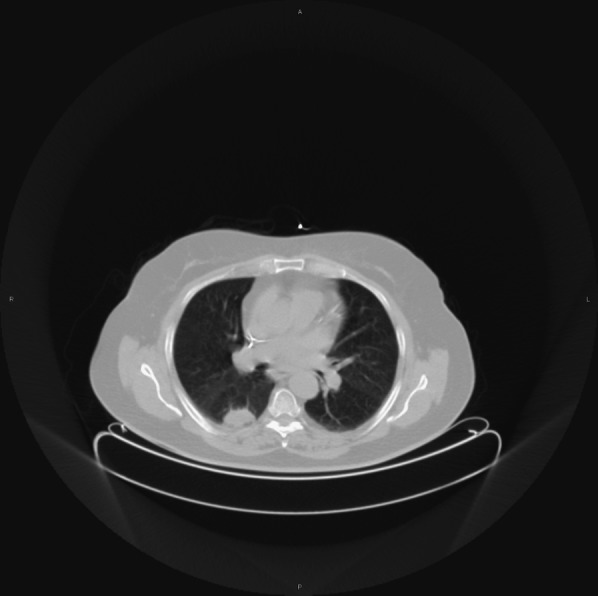
Centre 3 used an Infinia Hawkeye 4-slice CT system. Out of 275 patients, they found 5 who had new significant incidental findings at the time of the report, but none of them had clinically significant pathology. One patient was reported to have a pleural effusion, but when followed up, this was owing to left ventricular failure. Another patient was reported to have GGO, but the appearance 12 weeks later on the follow-up diagnostic MDCT thorax was normal. A further patient was found to have atelectasis. Two pulmonary nodules were identified; one was reclassified as emphysema with fissural thickening on follow-up imaging, and the other (Figure 6) was confirmed as a 6-mm pulmonary nodule by diagnostic MDCT (Figure 7). This was found to be stable over a 24-month follow-up period.
Figure 6.
Patient from Centre 3. CT attenuation correction images using GE Infinia™ Hawkeye™ (GE Healthcare, Buckinghamshire, UK) four-slice. Cross-hairs identify an approximately 6-mm nodule. A, anterior; I, inferior; L, left; P, posterior; R, right; S, superior.
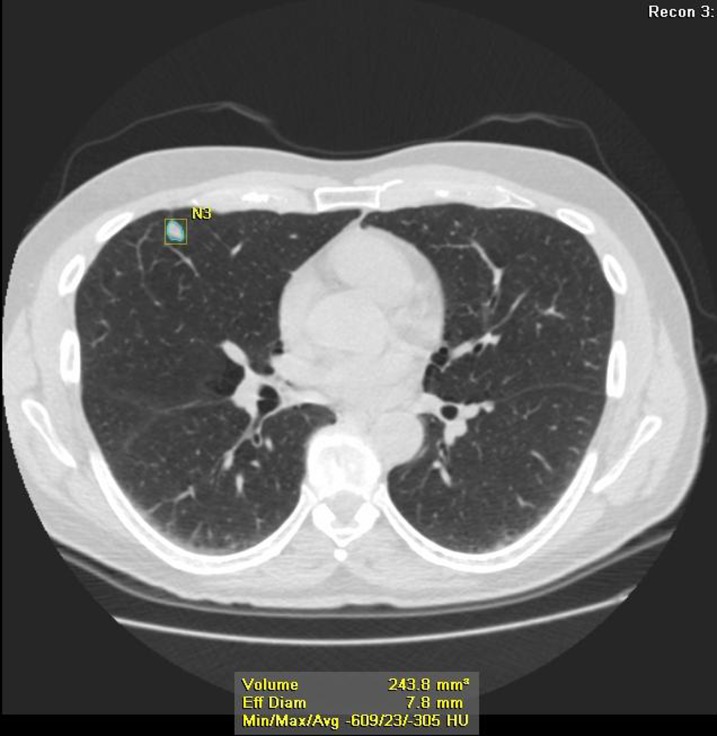
Figure 7.
The same patient as in Figure 6. Diagnostic multidetector CT confirming the presence of a nodule (N3). This was considered stable on subsequent CT images over a period of 24 months. Avg, average; Eff Diam, effective diameter; Max, maximum; Min, minimum.
Centre 4 used a Precedence 16-slice CT system. Out of 211 patients, they found 3 who had previously undiagnosed single pulmonary lung nodules (SPNs) identified at the time of the report. All three SPNs were confirmed with follow-up CT. One nodule remained stable, but the other two were confirmed carcinomas with staging of T3 (two lesions within lobe) (Figure 8) and the other T2a N0 M0 (Figure 9).
Figure 8.
Patient from Centre 4. CT attenuation correction image from Philips Precedence 16-slice multidetector CT (Philips Healthcare, Guildford, UK) demonstrating a right lower lobe nodule in a 77-year-old male patient, which was confirmed as T3 carcinoma at resection.
Figure 9.
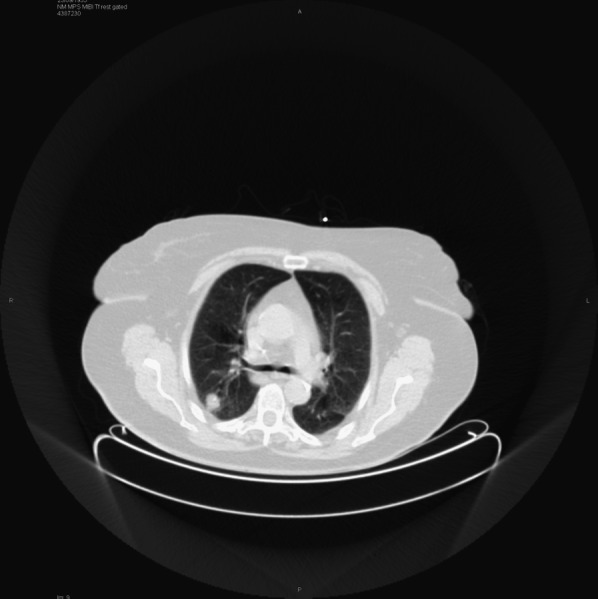
Another patient from Centre 4. CT attenuation correction image from Philips Precedence 16-slice multidetector CT (Philips Healthcare, Guildford, UK) demonstrating single pulmonary nodule in a 77-year-old male patient, which was confirmed as T2a N0 M0.
Implications of the findings
The distinctive feature of this study is that it not only demonstrates the possibility of detecting incidental findings on CTAC, as already reported in current literature, but also goes on to evaluate the significance and value of those findings in relation to the quality of the images on which they have been detected.
There is a common conception that detection of incidental findings will ultimately benefit the patient.12 Detection of pre-clinical disease on CTAC images could potentially lead to early and more effective treatment of the disease with a consequent improvement in patient outcome. This would be consistent with the aim of a screening programme. However, the overall detection rate (4 cancers detected out of 1819 patients) and the low PPV (8%) across all centres means that its value as an investigative procedure appears to be limited.
Incidental findings that are considered to be significant or indeterminate at the time of reporting will warrant further diagnostic follow up, which often carries with it a further risk to the patient.13 Diagnostic imaging usually has an associated radiation burden. Similarly, intervention from biopsy or surgery will also involve associated risk to the patient.
Consideration of clinically relevant findings is important when patient outcome can be improved.14 However, thought needs to be given to the proportion of false-positives detected on the low-resolution CT images and overdiagnosis (where a cancer is detected that would not otherwise have become apparent in that patient's lifetime). These will undoubtedly result in patients having follow-up diagnostic tests, which affect the balance of harms vs benefit to the patient.12,15,16 Benefit exceeding harm is an important aspect of any diagnostic procedure.12,15
The case illustrated in Figures 1–3 shows a good example of this. Here, a pulmonary nodule was detected on CTAC and confirmed with diagnostic MDCT with identification of a further lesion. Both lesions were surgically removed and subsequently found to be benign. Ultimately, the resection of these asymptomatic lesions was found to be unnecessary, so there was no actual benefit to the patient.
A large proportion of incidental findings are pulmonary in nature14 with pulmonary nodules being a frequent finding.13,17 There is considerable controversy surrounding whether CT screening for lung cancer is effective.13,18,19 A suitable screening test with a high enough sensitivity and specificity to reduce mortality from the detection of lung cancer has not yet been established and currently a lung cancer screening programme does not exist in the UK.13,14,18 Given that diagnostic quality images do not reduce mortality in this situation, it has to be questioned whether low-resolution CTAC images are likely to have any net patient benefit.
As well as an increase in morbidity and mortality from follow-up and intervention, there is also the increase in healthcare costs to consider and an inevitable increase in patient anxiety.13,17,20 There is an obvious psychological effect of diagnosing a healthy patient with disease, the effects of which can be long-term even after normal follow-up results.21 Radiological imaging cannot always offer definitive reassurance.20,22 Patient tolerance of further imaging could be affected as a result, which could result in non-compliance with necessary imaging procedures.14
The CTAC images produced during SPECT-CT MPI are of low resolution and taken through a limited area of the thorax. As such, not only will some cancers not be detected on the images but also inevitably pathology outside the scan range will remain undetected. Whilst pathology might be detected on the images, the absence of pathology on the images does not mean that the patient is disease free.
The varied CT performance among the centres in this study is an important consideration. Centre 4 (utilizing the Philips Precedence 16-slice) performed considerably better than Centres 2 and 3 (utilizing the GE Infinia Hawkeye 4) and Centre 1 (utilizing GE Infinia Hawkeye 1). This is consistent with the findings of the lesion detection phantom study performed by Thompson et al.10 In our study, the PPV at Centre 4 was 67% compared with 6% for Centre 2 and 0% from Centres 1 and 3. The PPV for Centre 4 was significantly better than for the other three centres combined (p = 0.01 using Fisher's exact test). In previous studies, PPV for detection of pulmonary nodules with contrast-enhanced diagnostic CT was found to be 80%.23
To give this some perspective, from 211 patients imaged with CTAC at Centre 4, 3 (1.42%) had significant new findings of which 2 (0.95%) lives were likely to be saved from lung cancer. This is higher than the detection rate of the breast screening programme (0.8%). Both patients were referred for surgical resection and have survived so far. Of the 1011 patients imaged with CTAC at Centre 2, 31 (3%) had new significant findings of which 1 (0.1%) had their life saved. The 5 (1.8%) patients from Centre 3 and 12 (3.7%) patients from Centre 1 with new significant findings resulted in no improvement in patient outcome in relation to survival rate.
With the equipment used at Centre 4, image quality of the CTAC images would be expected to be closer to diagnostic quality than that of CTAC images acquired at the other three centres. In particular, the short rotation time and overall scan time would greatly reduce the chance of motion artefact on the resultant images from patient respiration. This would be inevitable on the images acquired with the much longer rotation times of the Infinia Hawkeye scanners, which are not designed for diagnostic quality imaging. CTAC images from Centre 4 had also been acquired with a smaller slice thickness and a low pitch factor leading to improved spatial resolution and reduced partial volume effect compared with CTAC images acquired at the other centres.
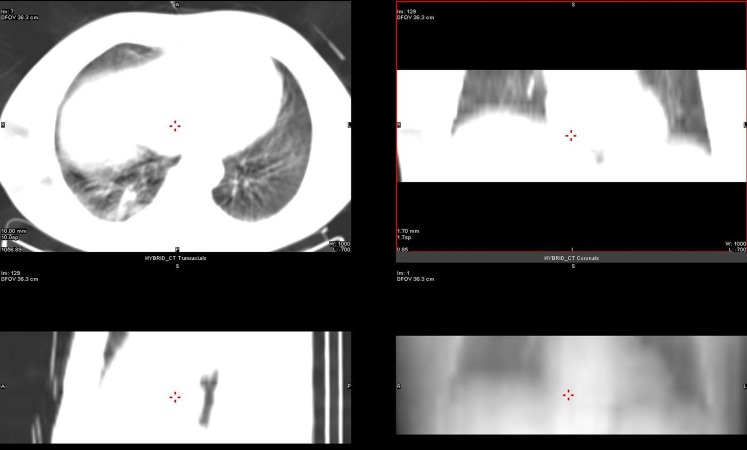
It is likely that improved image quality will lead to improved confidence in reporting. For example, the radiologist from Centre 1 who was used to viewing the CTAC images from the Infinia Hawkeye one-slice system commented on the difficulty of expressing radiopacity in Hounsfield units because a larger slice thickness lead to greater partial volume averaging (Figure 10).
Figure 10.
Illustrating a suspected pulmonary nodule on GE Infinia Hawkeye™ (GE Healthcare, Buckinghamshire, UK) one-slice CT attenuation correction image that was confirmed as pulmonary fibrosis on diagnostic multidetector CT. L, length; DFOV, display field of view; Im, image; W, width.
CONCLUSION
The primary question addressed by this multicentre study was to determine whether low-resolution CTAC images have diagnostic value and would warrant reporting.
Poor-quality CT images were produced by the centre that used the older GE Hawkeye 1 single slice system. This centre had a PPV of 0%, and this study suggests these images do not warrant reporting. Good-quality CT images were produced by the centre using the Philips Precedence system. This centre had a PPV of 67%, and this study suggests that there is merit in reporting these images.
The two centres using the GE Hawkeye 4 system produced medium-quality CT images. These centres had PPVs of 6% and 0%, respectively. The PPVs are extremely low because most of the correctly identified new findings that were thought to be significant at the time of reporting turned out to be clinically insignificant after further investigation. Further research is clearly needed to establish the actual diagnostic value of CT used for AC in MPI, especially in the case of medium-resolution CT subsystems in SPECT-CT scanners.
REFERENCES
- 1.Sharma P, Patel CD, Karunanithi S, Maharjan S, Malhotra A. Comparative accuracy of CT attenuation-corrected and non-attenuation-corrected SPECT myocardial perfusion imaging. Clin Nucl Med 2012; 37: 332–8. doi: 10.1097/RLU.0b013e31823ea16b [DOI] [PubMed] [Google Scholar]
- 2.Pazhenkottil AP, Ghadri JR, Nkoulou RN, Wolfrum M, Buechel RR, Küest SM, et al. Improved outcome prediction by SPECT myocardial perfusion imaging after CT attenuation correction. J Nucl Med 2011; 52: 196–200. doi: 10.2967/jnumed.110.080580 [DOI] [PubMed] [Google Scholar]
- 3.Arumugam P, Harbinson M, Reyes E, Sabharwal N, Tonge C, Underwood R, et al. Procedure guidelines for radionuclide myocardial perfusion imaging with single-photon emission computed tomography. Nucl Med Commun 2013; 34: 813–26. doi: 10.1097/MNM.0b013e32836171eb [DOI] [PubMed] [Google Scholar]
- 4.Pandey A, Rao PPG, Elias M. Should myocardial perfusion CT attenuation correction datasets be reviewed? Presented at the British Nuclear Cardiology Society Annual Meeting, 2009.
- 5.Budoff MJ, Fischer H, Gopal A. Incidental findings with cardiac CT evaluation: should we read beyond the heart? Catheter Cardiovasc Interv 2006; 68: 965–73. [DOI] [PubMed] [Google Scholar]
- 6.Department of Health. The ionising radiation (medical exposure) regulations 2000 (together with notes on good practice). London, UK: Department of Health. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22391700 [Google Scholar]
- 7.Hesse B, Lindhardt TB, Acampa W, Anagnostopoulos C, Ballinger J, Bax JJ, et al. EANM/ESC guidelines for radionuclide imaging of cardiac function. Eur J Nucl Med Mol Imaging 2008; 35: 851–85. doi: 10.1007/s00259-007-0694-9 [DOI] [PubMed] [Google Scholar]
- 8.Royal College of Radiologists. Standards for the reporting and interpretation of imaging investigations. London, UK: Royal College of Radiologists; 2006. [Google Scholar]
- 9.Royal College of Radiologists. Standards for the communication of critical, urgent and unexpected significant radiological findings. 2nd edn. London, UK: Royal College of Radiologists; 2012. [Google Scholar]
- 10.Thompson JD, Hogg P, Manning DJ, Szczepura K, Chakraborty DP. A free-response evaluation determining value in the computed tomography attenuation correction image for revealing pulmonary incidental findings: a phantom study. Acad Radiol 2014; 21: 538–45. doi: 10.1016/j.acra.2014.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goetze S, Pannu HK, Wahl RL. Clinically significant abnormal findings on the “nondiagnostic” CT portion of low-amperage-CT attenuation-corrected myocardial perfusion SPECT/CT studies. J Nucl Med 2006; 47: 1312–8. [PubMed] [Google Scholar]
- 12.Glasziou P, Houssami N. The evidence base for breast cancer screening. Prev Med 2011; 53: 100–2. doi: 10.1016/j.ypmed.2011.05.011 [DOI] [PubMed] [Google Scholar]
- 13.MacMahon H, Austin JH, Gamsu G, Herold CJ, Jett JR, Naidich DP, et al. Guidelines for management of small pulmonary nodules detected on CT Scans: a statement from the Fleischner Society. Radiology 2005; 237: 395–400. [DOI] [PubMed] [Google Scholar]
- 14.Machaalany J, Yam Y, Ruddy TD, Abraham A, Chen L, Beanlands RS, et al. Potential clinical and economic consequences of noncardiac incidental findings on cardiac computed tomography. J Am Coll Cardiol 2009; 54: 1533–41. doi: 10.1016/j.jacc.2009.06.026 [DOI] [PubMed] [Google Scholar]
- 15.Harris R, Yeatts J, Kinsinger L. Breast cancer screening for women ages 50 to 69 years; a systematic review of observational evidence. Prev Med 2011; 53: 108–14. doi: 10.1016/j.ypmed.2011.07.004 [DOI] [PubMed] [Google Scholar]
- 16.Bach PB, Mirkin JN, Oliver TK, Azzoli CG, Berry DA, Brawley OW, et al. Benefits and harms of CT screening for lung cancer: a systematic review. J Am Med Assoc 2012; 307: 2418–29. doi: 10.1001/jama.2012.5521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.White CS. The pros and cons of searching for extracardiac findings at cardiac CT: use of a restricted field of view is acceptable. Radiology 2011; 261: 338–41. doi: 10.1148/radiol.11111131 [DOI] [PubMed] [Google Scholar]
- 18.Field JK, Baldwin D, Brain K, Devaraj A, Eisen T, Duffy SW, et al. CT screening for lung cancer in the UK: position statement by UKLS investigators following the NLST report. Thorax 2011; 66: 736–7. doi: 10.1136/thoraxjnl-2011-200351 [DOI] [PubMed] [Google Scholar]
- 19.National Lung Screening Trial Research Team; Aberle DR, Berg CD, Black WC, Church TR, Fagerstrom RM, et al. The National Lung Screening Trial: overview and study design. Radiology 2011; 258: 243–53. doi: 10.1148/radiol.10091808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stone JH. Incidentalomas—clinical correlation and translational science required. N Engl J Med 2006; 354: 2748–9. [DOI] [PubMed] [Google Scholar]
- 21.Dans LF, Silvestre MA, Dans AL. Trade-off between benefit and harm is crucial in health screening recommendations. Part I: general principles. J Clin Epidemiol 2011; 64: 231–9. doi: 10.1016/j.jclinepi.2010.09.009 [DOI] [PubMed] [Google Scholar]
- 22.Laspas F, Roussakis A, Efthimiadou R, Papaioannou D, Papadopoulos S, Andreou J. Percutaneous CT-guided fine-needle aspiration of pulmonary lesions: results and complications in 409 patients. J Med Imaging Radiat Oncol 2008; 52: 458–62. doi: 10.1111/j.1440-1673.2008.01990.x [DOI] [PubMed] [Google Scholar]
- 23.Cronin P, Dwamena BA, Kelly AM, Carlos RC. Solitary pulmonary nodules: meta-analytic comparison of cross-sectional imaging modalities for diagnosis of malignancy. Radiology 2008; 246: 772–82. doi: 10.1148/radiol.2463062148 [DOI] [PubMed] [Google Scholar]