Abstract
Background
Unemployment rates are high amongst people with severe mental illness, yet surveys show that most want to work. Vocational rehabilitation services exist to help mentally ill people find work. Traditionally, these services have offered a period of preparation (Pre‐vocational Training), before trying to place clients in competitive (i.e. open) employment. More recently, some services have begun placing clients in competitive employment immediately whilst providing on‐the‐job support (Supported Employment). It is unclear which approach is most effective.
Objectives
To assess the effects of Pre‐vocational Training and Supported Employment (for people with severe mental illness) against each other and against standard care (in hospital or community). In addition, to assess the effects of: (a) special varieties of Pre‐vocational Training (Clubhouse model) and Supported Employment (Individual Placement and Support model); and (b) techniques for enhancing either approach, for example payment or psychological intervention.
Search methods
Searches were undertaken of CINAHL (1982‐1998), The Cochrane Library (Issue 2, 1999), EMBASE (1980‐1998), MEDLINE (1966‐1998) and PsycLIT (1887‐1998). Reference lists of eligible studies and reviews were inspected and researchers in the field were approached to identify unpublished studies.
Selection criteria
Randomised controlled trials of approaches to vocational rehabilitation for people with severe mental illness.
Data collection and analysis
Included trials were reliably selected by a team of two raters. Data were extracted separately by two reviewers and cross‐checked. Authors of trials were contacted for additional information. Relative risks (RR) and 95% confidence intervals (CI) of homogeneous dichotomous data were calculated. A random effects model was used for heterogeneous dichotomous data. Continuous data were presented in tables (there were insufficient continuous data for formal meta‐analysis). A sensitivity analysis was performed, excluding poorer quality trials.
Main results
Eighteen randomised controlled trials of reasonable quality were identified. The main finding was that on the primary outcome (number in competitive employment) Supported Employment was significantly more effective than Pre‐vocational Training; for example, at 18 months 34% of people in Supported Employment were employed versus 12% in Pre‐vocational Training (RR random effects (unemployment) 0.76 95% CI 0.64 to 0.89, NNT 4.5). Clients in Supported Employment also earned more and worked more hours per month than those in Pre‐vocational Training. There was no evidence that Pre‐vocational Training was more effective in helping clients to obtain competitive employment than standard community care.
Authors' conclusions
Supported employment is more effective than Pre‐vocational Training in helping severely mentally ill people to obtain competitive employment. There is no clear evidence that Pre‐vocational Training is effective.
Plain language summary
Vocational rehabilitation for people with severe mental illness
A majority of severely mentally ill people would like to work and there are compelling ethical, social and clinical reasons for helping them to achieve this goal. Pre‐vocational Training and Supported Employment are two different approaches to helping severely mentally ill people obtain employment. The key principle of Pre‐vocational Training is that a period of preparation is necessary before entering competitive employment. In contrast, the key principle of Supported Employment is that placement in competitive employment should occur as quickly as possible, followed by support and training on the job. This systematic review found that people who received Supported Employment were significantly more likely to be in competitive employment than those who received Pre‐vocational Training (at 12 months 34% employed in Supported Employment compared with 12% in Pre‐vocational Training).
Background
People who suffer from severe mental disorder experience high rates of unemployment. In the United States unemployment rates amongst such people are estimated at 75‐85% (Lehman 1995, Ridgeway 1998), whilst in the UK rates of 61‐73% have been reported (McCreadie 1992, Meltzer 1995). These high rates reflect the disability caused by severe mental illness, but they also reflect discrimination (unemployment rates are higher than in other disabled groups ‐ ONS 1998) and the low priority given to employment by psychiatric services (Lehman 1998). Despite high unemployment rates amongst the severely mentally ill, surveys have consistently shown that most want to work (Hatfield 1992, Lehman 1995, Shepherd 1994).
There are compelling ethical, social and clinical reasons for helping mentally ill people to work. From an ethical standpoint, the right to work is enshrined in the Universal Declaration of Human Rights 1948 and has been incorporated into national disability acts in Europe and America. From a social standpoint, high unemployment rates are an index of the social exclusion of severely mentally ill people, which many governments, including that of the UK, are committed to reducing (DoH 1998). Finally, from a clinical standpoint, employment may lead to improvements in the outcome of severe mental illness, through increasing self‐esteem, alleviating psychiatric symptoms, and reducing dependency and relapse (Lehman 1995).
Helping mentally ill people to work is not a new idea. The value of therapeutic work was recognised by the pioneers of the asylum movement, and in their latter days many large asylums depended on the labour of their inmates in farms, workshops, or work‐crews (Jones 1993). As asylums closed down, work experience played an important role in the preparation of patients for discharge. Patients who performed well on graded tasks within the hospital were gradually reintroduced to working in the community, often through special arrangements with local employers. As community care developed, these arrangements evolved into enterprises or workshops providing sheltered employment within a segregated work setting (Gervey 1994). Such sheltered workshops aimed to place clients in competitive employment after a period of pre‐vocational training, but follow up studies showed a success rate of only five to ten percent (Bond 1988, Connors 1987).
The Clubhouse movement arose in the 1950s as a reaction to traditional sheltered employment and to the lack of emphasis on work within mental health services (Macias 1995). The Clubhouse movement proposed that better employment outcomes could be achieved by fostering patient autonomy in a non‐psychiatric setting (known as a Clubhouse). The Clubhouse is a building run by clients and staff along egalitarian lines, where clients meet for social activity, mutual support and graded work experience. Like traditional pre‐vocational training, the Clubhouse approach involves a period of preparation before clients attempt to return to competitive employment. This period of preparation consists of two stages: the work ordered day and Transitional Employment (Beard 1982). The work‐ordered day refers to a process whereby clients join work crews (working side‐by‐side with staff) that take responsibility for managing and maintaining the Clubhouse. Work crews are seen as a means of preparing for Transitional Employment. Transitional Employment refers to the placement of clients in a series of paid but temporary jobs controlled by the Clubhouse, in order to help them develop the skills and confidence required to cope with competitive employment (Bond 1998a). Whilst there are no rigid guidelines for length of time on work crews, clients are discouraged from seeking competitive employment until they have achieved success in Transitional Employment, and are free to return to work crews at any time (Bilby 1992). Cross‐fertilisation between the Clubhouse and traditional approaches led to a number of hybrid approaches (or stepwise eclectic approaches), combining for example, transitional employment with pre‐employment training (Bond 1998a).
In the mid‐1980s a new approach to vocational rehabilitation emerged, known as Supported Employment. Supported Employment involved trying to place clients in competitive jobs without any extended preparation (Bond 1992). Originally developed for people with learning disabilities, Supported Employment has been defined as paid work that takes place in normal work settings with provision for ongoing support services (Becker 1994, Bond 1998a). Proponents of Supported Employment had two objections to Pre‐vocational Training (Bilby 1992, Bond 1997a). First, they argued that it promoted dependency and deterred clients from finding competitive employment. Second, they argued that Pre‐vocational Training was not effective in developing work skills. Instead of Pre‐vocational Training, they proposed trying to place clients as quickly as possible in competitive employment positions, where they would receive intensive on‐the‐job support and training from personnel known as Job Coaches (Anthony 1987).
Individual Placement and Support is a carefully specified variant of Supported Employment distinguished by six key principles: (1) the goal is competitive employment in work settings integrated into a community's economy; (2) clients are expected to obtain jobs directly, rather than following lengthy pre‐employment training (rapid job search); (3) rehabilitation is an integral component of mental health treatment rather than a separate service; (4) services are based on clients' preferences and choices; (5) assessment is continuous and based on real work experiences; and (6) follow‐on support is continued indefinitely (Bond 1998b). Adherence to Individual Placement and Support guidelines may be measured using a fidelity scale (Bond 1997b).
Natural experiments have suggested that Supported Employment is an acceptable intervention that helps sustain people in work. For example, Drake‐New Hampshire2 studied a Community Mental Health Centre that was forced to eliminate its day care program because of budget cuts. As a replacement for the day care services, a small Supported Employment program was started. Drake‐New Hampshire2 compared the day centre conversion site to a second site, which continued to offer day care alongside traditional Pre‐vocational services. Clients at the Supported Employment site showed increased rates of competitive employment, whilst no change was found for the site not converting. After the completion of the initial conversion, the second site subsequently converted to Supported Employment, with similarly favourable results (Clark 1996). Favourable results have been reported from a third day care centre, which made a partial transition to the Individual Placement and Support model of Supported Employment (Bailey‐New Hampshire).
Both Pre‐vocational Training (traditional, Clubhouse) and Supported Employment are widely practiced. In the US there are 3,000 'psychiatric rehabilitation providers' offering traditional pre‐vocational training and about 230 Clubhouses. There are also around 36,000 mentally ill people in Supported Employment schemes (Bond 1998a, Wehman 1997). In the UK there are around 135 organisations offering Pre‐vocational Training and 77 offering Supported Employment (ERMIS 1998). It remains unclear if Pre‐vocational Training and Supported Employment are equally effective.
Objectives
The main objective was to determine how far Pre‐vocational Training and Supported Employment were effective in helping people with severe mental illness to obtain competitive (i.e. open) employment. The review also examined how far Pre‐vocational Training and Supported Employment affected other work and clinical outcomes. The main comparisons in the review were as follows:
1. Pre‐vocational Training versus standard hospital care; 2. Pre‐vocational Training (in addition to standard community care) versus standard community care; 3. Supported Employment (in addition to standard community care) versus standard community care; 4. Pre‐vocational Training versus Supported Employment.
In addition, the review examined the effectiveness of modifications designed to enhance approaches to vocational rehabilitation (e.g. payment or psychological intervention) and the effectiveness of well‐characterised sub‐types of Pre‐vocational Training (Clubhouse model) and Supported Employment (Individual Placement and Support model). The review did not consider the effectiveness of Assertive Community Treatment or other forms of case management in improving employment outcomes, as these general approaches to enhancing community care have been reviewed elsewhere (Marshall 1999a, Marshall 1999b).
Methods
Criteria for considering studies for this review
Types of studies
Relevant randomised controlled trials that provided data which could be analysed on an intention‐to‐treat basis.
Types of participants
Vocational rehabilitation approaches were not designed for a specific diagnostic group nor are they applied in a diagnostic‐specific way in everyday practice. Therefore, for the purpose of this review, the main requirements of participants were that they were similar to those who typically present to vocational rehabilitation services. Specific inclusion criteria were that a majority of clients in the trial were: (a) aged 18‐65; and (b) suffering from severe mental disorder defined as: schizophrenia and schizophrenia‐like disorders; bipolar disorder; or depression with psychotic features. Substance abuse was not considered a severe mental disorder, but trials were eligible if participants had a problem with substance abuse in addition to a mental disorder. Trials were excluded where a majority of participants were suffering from a learning disability.
Types of interventions
Four interventions were defined: Pre‐vocational Training, Supported Employment, enhanced approaches, and standard care.
1. Pre‐vocational Training Pre‐vocational Training was defined as any approach to vocational rehabilitation in which participants were expected to undergo a period of preparation, before being encouraged to seek competitive employment. This preparation could involve either work in a sheltered environment (such as a workshop or work unit), or some form of pre‐employment training or transitional employment. Both the traditional (sheltered workshop) and Clubhouse approaches were classified as Pre‐vocational Training.
2. Supported Employment Supported employment was defined as any approach to vocational rehabilitation that attempted to place clients immediately in competitive employment. It was acceptable for Supported Employment to begin with a short period of preparation, but this had to be of less than one month duration and not involve work placement in a sheltered setting, or training, or transitional employment. Individual Placement and Support was defined as Supported Employment that adhered to the six principles outlined in the Background (see above).
3. Modifications of vocational rehabilitation programs Modified programs were defined as either Pre‐vocational Training or Supported Employment that had been enhanced by some technique to increase participants' motivation. Typically such techniques consisted of payment for participation in the program, or some form of psychological intervention.
4. Standard care was defined as usual psychiatric care for patients in the trial, without any specific vocational component. In all trials where an intervention is compared against standard care, unless otherwise stated clients will have received the intervention in addition to standard care. Thus, for example, in a trial comparing Pre‐vocational Training against standard community care, patients in the Pre‐vocational Training group will also be in receipt of standard community services, such as out‐patient appointments.
Types of outcome measures
The primary outcome was number of clients in competitive employment at various time points (defined as a full or part time position held by the client in an ordinary work setting, for which they were receiving payment at the market rate).
Secondary outcome measures were grouped into three main categories.
1. Other employment outcomes: 1.1 in any form of employment (defined as competitive employment, transitional employment, sheltered employment or voluntary work); 1.2 in any form of employment or education (defined as above but including people on training courses or full or part‐time education); 1.3 mean hours per month in competitive employment; 1.4 mean monthly earnings.
2. Clinical outcomes: 2.1 numbers lost to follow up (for trials with community or hospital controls only) or numbers not participating in program (for trials comparing different VR approaches); 2.2 admitted to hospital (for trials with a community control) or number living in community at end of study (if a hospital control); 2.3 other clinical outcomes (e.g. symptoms, quality of life and social functioning).
3. Costs: 3.1 mean monthly program costs (direct costs of experimental program versus direct costs of control program); 3.2 mean monthly healthcare costs (including costs of all psychiatric/medical care and program costs, but excluding earnings or transfer costs i.e. benefits obtained).
Search methods for identification of studies
1. Electronic searching The search began by deriving a list of search terms from reading overviews of the field and consulting experts in vocational rehabilitation.
1.1 CINAHL (January 1982‐December 1998) was searched using the Cochrane Schizophrenia Group's search strategy for randomised controlled trials combined with the phrase:
[(SUPP* EMPLOY*) or (EMPLOYMENT) or (PSYCHOSOCIAL REHAB*) or (PSYCHIATRIC REHAB*) or (OCCUPATIONAL REHAB*) or (SOC* REHAB*) or (WORK REHAB*) or (JOB REHAB*) or (SHELTERED WORK*) or (TRANSITIONAL EMP*) or (REHABILITATION COUNSELLING) or (VOCATION*) or (FOUNTAIN HOUSE*) or (FOUNTAIN‐HOUSE*) or (CLUBHOUSE*) or (CLUB‐HOUSE*). The results of this search were then combined with a search using the major indexing term MENTAL‐DISORDERS.
1.2 The Cochrane Library (Issue 2, 1999) was searched using the phrases:
[(SUPP* EMPLOY*) or (EMPLOYMENT) or (PSYCHOSOCIAL REHAB*) or (PSYCHIATRIC REHAB*) or (OCCUPATIONAL REHAB*) or (SOC* REHAB*) or (WORK REHAB*) or (JOB REHAB*) or (SHELTERED WORK*) or (TRANSITIONAL EMP*) or (REHABILITATION COUNSELLING) or (VOCATION*) or (FOUNTAIN HOUSE*) or (FOUNTAIN‐HOUSE*) or (CLUBHOUSE*) or (CLUB‐HOUSE*) and (MENTAL ILLNESS or SCHIZOPHRENIA)]
1.3 EMBASE (January 1980‐December 1998) was searched using the Cochrane Schizophrenia Group's search strategy for randomised controlled trials combined with the phrase:
[(SUPP* EMPLOY*) or (EMPLOYMENT) or (PSYCHOSOCIAL REHAB*) or (PSYCHIATRIC REHAB*) or (OCCUPATIONAL REHAB*) or (SOC* REHAB*) or (WORK REHAB*) or (JOB REHAB*) or (SHELTERED WORK*) or (TRANSITIONAL EMP*) or (REHABILITATION COUNSELLING) or (VOCATION*) or (FOUNTAIN HOUSE*) or (FOUNTAIN‐HOUSE*) or (CLUBHOUSE*) or (CLUB‐HOUSE*). The results of this search were then combined with a search exploding all sub‐headings of the indexing term MENTAL DISEASE.
1.4 MEDLINE (January 1966‐December 1998) was searched using the Cochrane Schizophrenia Group's search strategy for randomised controlled trials combined with the phrase:
[(SUPP* EMPLOY*) or (EMPLOYMENT) or (PSYCHOSOCIAL REHAB*) or (PSYCHIATRIC REHAB*) or (OCCUPATIONAL REHAB*) or (SOC* REHAB*) or (WORK REHAB*) or (JOB REHAB*) or (SHELTERED WORK*) or (TRANSITIONAL EMP*) or (REHABILITATION COUNSELLING) or (VOCATION*) or (FOUNTAIN HOUSE*) or (FOUNTAIN‐HOUSE*) or (CLUBHOUSE*) or (CLUB‐HOUSE*). The results of this search were then combined with a search exploding all sub‐headings of the indexing term MENTAL DISORDERS.
1.5 PsycLIT (January 1887‐December 1998) was searched using the Cochrane Schizophrenia Group's search strategy for randomised controlled trials combined with the phrase:
[(SUPP* EMPLOY*) or (EMPLOYMENT) or (PSYCHOSOCIAL REHAB*) or (PSYCHIATRIC REHAB*) or (OCCUPATIONAL REHAB*) or (SOC* REHAB*) or (WORK REHAB*) or (JOB REHAB*) or (SHELTERED WORK*) or (TRANSITIONAL EMP*) or (REHABILITATION COUNSELLING) or (VOCATION*) or (FOUNTAIN HOUSE*) or (FOUNTAIN‐HOUSE*) or (CLUBHOUSE*) or (CLUB‐HOUSE*).
This search strategy identified 40 confirmed trials and 13 review articles.
2. Reference searching The sensitivity of the search strategy was examined by comparing the results of the search with the reference lists of the identified reviews and trials to determine how many cited trials had not been detected. Of three undetected trials cited in the reviews, two were not listed on any of the databases, whilst the third trial was indexed under the term 'DELIVERY OF HEALTH CARE/INTEGRATED'. This term was then added to the search strategy and the search was re‐run, but no further trials were detected. Finally the results of the search were compared against bibliographies from two unpublished PhD theses (Kim 1998, Schneider 1998) but no further trials were detected.
3. Personal contact Researchers in the field were approached to identify unpublished studies.
Data collection and analysis
1. Selection of studies The initial electronic search was performed by one reviewer (RC). The list of publications identified by the search strategy was examined by two reviewers working independently (MM, RC). Each reviewer discarded irrelevant publications and retained only those trials in which some form of vocational rehabilitation had been compared against a control treatment. The reviewers then obtained copies of all papers relating to relevant trials. Once these papers had been obtained they were read independently by the two reviewers who decided whether the trials were eligible for the study and allocated them to one of six possible comparisons (Pre‐vocational Training versus hospital control; Pre‐vocational Training versus community control; Supported Employment versus Pre‐vocational Training; Supported Employment versus community control; modifications of vocational rehabilitation programs). Inter‐rater agreement was assessed for overall eligibility and for allocation of trials to comparisons.
2. Quality assessment MM and RC rated each trial according to the three categories of allocation concealment described in the Cochrane Collaboration Handbook (Clarke 1999): A ‐ adequate (i.e. the method for assigning participants to interventions was robust against patient and clinician bias and clearly described); B ‐ method of allocation concealment unclear; C ‐ inadequate (i.e. the method of assignment was not robust to patient and clinician bias). When the method of allocation concealment was unclear, trialists were contacted for further details. Blinding of patients and treating clinicians is not possible in trials of vocational rehabilitation. It is also difficult for those evaluating outcome to remain blind to group allocation, as they are obliged to collect data that indicate group allocation (such as days in different types of employment). However, trials were rated on independence of evaluators from those providing the intervention.
3. Data extraction All data were extracted by the two reviewers working alone and then cross‐checked to ensure reliability.
4. Data management 4.1 Missing data 4.1.1 Unacceptable loss to follow‐up: a sensitivity analysis was performed excluding trials where the loss to follow up was greater than 80%. Additionally, amongst included studies, the review did not report data on outcomes where less than 50% of those assessed at baseline failed to be reassessed on the same outcome at follow‐up.
4.1.2 Intention‐to‐treat analysis: it was assumed that patients who were lost to follow up remained unemployed, as suggested by previous research (Bond 1984).
4.2 Dichotomous (i.e. yes/no data) The relative risk and 95% confidence interval (CI), as well as the number needed to treat (NNT) were calculated for relevant outcomes. The relative risk was chosen over the odds ratio because the latter tends to overestimate effect size when event rates are high (Clarke 1999). The NNT was calculated as the inverse of the absolute risk reduction, and confidence intervals were calculated using the Arcus Quickstat(c) Program.
4.3 Continuous data Continuous data were reported on MetaView when normally distributed, and when available on the same variable from more than one trial. Otherwise continuous data, including skewed data (see below 4.3.2) and data analysed using non‐parametric methods, were reported in tables or in the text.
4.3.1 Intention‐to‐treat analysis: in the case of continuous data a completer analysis was presented.
4.3.2 Rating scales: data from rating scales were excluded if collected using an unpublished scale, or based on a subset of items from a scale (see Marshall 2000 for justification).
4.3.2 Skewed data: continuous data on mental health outcomes are often not normally distributed (i.e. skewed). It may not be appropriate to analyse such data using parametric methods, such as those used by MetaView. In this review the degree of skew of continuous data was assessed by multiplying the standard deviation by 1.96. If the result was less than the mean then the data were entered on MetaView, otherwise they were reported in the text or in tables (Altman 1996). Data analysed using non‐parametric statistics were also reported in tables.
4.3.3 Conversion of data: data were reported as presented in the original studies, with two exceptions. First, continuous variables such as costs or days in employment were converted to a single common scale (such as mean days in employment per month or mean monthly costs) in order to facilitate comparisons. Second, number of clients not participating in the program was estimated by taking the number of clients who were not re‐interviewed at the final follow‐up assessment, or by taking actual non‐participation rates (where these were given in the trial report and were greater than the number not re‐interviewed). Clients were not counted as not participating if the reason for non‐participation was that they were in an alternative work or educational placement.
5. Sub‐analyses Two sub‐types of Pre‐vocational Training and Supported Employment (the Clubhouse and IPS models, respectively) have been sufficiently specified to be regarded as approaches in their own right (see above for details). Data from trials using these approaches were included in the main Pre‐vocational Training and Supported Employment comparisons, but were also presented separately as sub‐analyses.
6. Heterogeneity Heterogeneity between trial results was assessed by inspection of graphical presentations and by calculating a Chi squared test of heterogeneity. If heterogeneity was present (p value of Chi squared <0.1) the data were re‐analysed using a random effects model. If heterogeneity was still present, the summary relative risk was interpreted cautiously, and efforts were made to identify the source of the heterogeneity.
7. Addressing publication bias Data from all identified and selected trials were entered into a funnel graph (trial effect versus trial size) in an attempt to investigate overt publication bias.
8. Tables and figures The data were recorded on RevMan so that the area to the left of the 'line of no effect' indicated a 'favourable' outcome for the first intervention mentioned in the title of the comparison. For example, in trials comparing Supported employment to Pre‐vocational Training, an outcome to the left of the 'line of no effect' would indicate a favourable outcome for Supported Employment, whereas an outcome to the right would indicate a favourable outcome for Pre‐vocational Training .
Results
Description of studies
1. Excluded studies Thirty‐one studies were excluded (please see 'Table of excluded studies'); seventeen of these were not randomised, but fourteen were classified as randomised controlled trials. The non‐randomised studies consisted of: one survey (without comparison group); three cross‐sectional comparisons; five uncontrolled 'before and after' comparisons, and eight quasi‐experimental designs (i.e. comparative trials where no attempt was made to randomise). The excluded randomised controlled trials consisted of: five trials of Pre‐vocational Training versus standard care (in two the number of participants with mental illness was unclear, and in three the data could not be analysed on an intention‐to‐treat basis); four trials of modifications of Pre‐vocational Training versus Pre‐vocational Training (in three the number of participants was unclear, whilst the remaining trial was concerned with increasing productivity rather than helping patients find work); and five trials of approaches to community care that did not involve any specific vocational interventions (three of assertive community treatment and two others), although the trials happened to report employment rates. Of the trials where data could not be analysed on an intention‐to‐treat basis: in Briggs‐Minnesota the number of participants was unclear; in Kaufman‐Pittsburgh the numbers randomised to treatment and control groups were not given; and in Ryan‐Connecticut there was substantial exclusion of treatment group participants post‐randomisation (for example, any client who failed to complete three months in the Pre‐vocational Training group was excluded).
2. Ongoing studies Two ongoing studies were identified, including one substantial multi‐centre study of Supported Employment versus Pre‐vocational Training (Carey‐US 8 site).
3. Awaiting assessment There were four studies awaiting assessment: three were published in books that were difficult to obtain (one of which was in Dutch) and one was unpublished.
4. Included studies Eighteen trials met inclusion criteria for the review (see 'Table of included studies' for full details).
4.1 Participants People with schizophrenia are well represented in the trials of Pre‐vocational Training versus Supported Employment (weighted means of 52.4 and 78.7%). Women were well represented. There were insufficient data to assess representation of people from ethnic minorities. Women, people from ethnic minorities, and people with schizophrenia were well represented in the trials of Supported Employment versus Pre‐vocational Training (weighted means of 49.8%, 37.9% and 60.2% respectively).
4.2 Interventions 4.2.1 Pre‐vocational training: Becker‐Fort Worth compared care on a specialised rehabilitation ward with an integral vocational program against continuing in‐patient rehabilitation. Kuldau‐California compared a rehabilitation program involving sheltered work, an in‐patient therapeutic community and transitional housing against a control involving standard hospital care with rapid discharge planning. Walker‐Massachusetts compared day placement in an out‐of‐hospital industrial therapy unit with standard hospital care. Beard‐NewYork compared the 'Clubhouse' model of vocational rehabilitation to standard community care. Dincin‐Chicago compared the 'Thresholds' program, involving work crews and transitional employment to standard community care, including six hours of supportive psychotherapy and fortnightly consultations with a psychiatrist. Griffiths‐London compared a rehabilitation programme involving day hospital and industrial workshops against standard community care involving home support and day centres. Okpaku‐Nashville compared employment‐oriented case management involving work assessment and employment preparation against standard case management. Wolkon‐Cleveland compared individual counselling and transitional work to standard community care.
4.2.2 Modifications of pre‐vocational training: Bell‐Connecticut modified pre‐vocational training and examined the effect of payment on uptake of sheltered set‐aside jobs in a hospital. Blankertz‐Philadelph and Kline‐Philadelphia examined the effects of psychological interventions (designed to increase motivation) on the uptake of community vocational rehabilitation services. Control groups received vocational rehabilitation services but no psychological intervention. Bond‐Chicago1 compared a graded approach (of experience in work crews leading to transitional employment), with an accelerated approach involving immediate placement in transitional employment.
4.2.3 Supported employment: Chandler‐LongBeach compared Assertive Community Treatment combined with Supported Employment against standard community care (not involving Assertive Community Treatment). In the studies of Supported Employment versus Pre‐vocational Training, Bond‐Indiana compared Supported Employment with Pre‐vocational work‐readiness training. Drake‐New Hampshire1 compared the Individual Placement and Support model of Supported Employment with a brokered model of Pre‐vocational Training. Drake‐Washington compared the Individual Placement and Support Model with Pre‐vocational counselling and work adjustment training in a sheltered workshop. Gervey‐New York compared Supported Employment with employment training in a sheltered workshop. McFarlane‐New York compared Family‐aided Assertive Community Treatment plus Supported Employment with conventional Pre‐vocational Training from the local vocational rehabilitation service.
4.3 Outcome Scales Rating scales used to measure clinical outcomes are listed below.
4.3.1 Global Outcome GAS (Endicott 1976). A clinician rated scale of overall functioning on a scale of 1‐100. Lower scores indicate poorer functioning.
4.3.2 Mental State The Positive and Negative Symptom Scale ‐ PANSS (Kay 1987) This schizophrenia scale has 30 items, each of which can be defined on a seven‐point scoring system varying from one ‐ absent to seven ‐ extreme. This scale can be divided into three sub‐scales for measuring the severity of general psychopathology, positive symptoms (PANSS‐P), and negative symptoms (PANSS‐N). A low score indicates lesser severity.
The Brief Psychiatric Rating Scale ‐ BPRS (Lukoff 1986) This is used to assess the severity of abnormal mental state. The original scale has 16 items, but a revised 18‐item scale is commonly used. Each item is defined on a seven‐point scale varying from 'not present' to 'extremely severe', scoring from 0‐6 or 1‐7. Scores can range from 0‐126, with high scores indicating more severe symptoms.
4.3.2 Others Self‐confidence scale (Wing 1966) No details were available on this scale, and the original reference was difficult to obtain.
Self‐esteem (Rosenberg 1969) This scale is a 10‐item self‐report measure. Each item involves a statement about how the respondent feels about him or herself ('I feel that I have a number of good qualities') or aspects of his or her functioning ('I feel that I can't do anything right'). Respondents rate each item on a Likert scale from 'almost always true' to 'never true'. Lower scores indicate higher self‐esteem.
Quality of Life Scale (Lehman 1983) This standardised assessment includes areas such as living situation, leisure activities, relationships and finances. Rated on a seven‐point scale, with higher scores indicating a better quality of life.
Risk of bias in included studies
1. Randomisation The quality of allocation concealment in included trials was as follows: seven trials were in randomisation category A (adequate) (Bond‐Chicago1, Bond‐Indiana, Dincin‐Chicago, Drake‐New Hampshire1, Drake‐Washington, Kuldau‐California, Walker‐Massachusetts); nine were in category B (unclear) (Becker‐Fort Worth, Bell‐Connecticut, Blankertz‐Philadelph, Chandler‐LongBeach, Griffiths‐London, Kline‐Philadelphia, McFarlane‐New York, Okpaku‐Nashville, Wolkon‐Cleveland); and two were category C (inadequate) (Beard‐NewYork, Gervey‐New York). Of the trials in category C: in Beard‐NewYork allocation was by day of referral and in Gervey‐New York allocation was by drawing lots from a hat.
2. Objectivity of rating of outcome In eight trials outcome was assessed by raters who were not involved in providing the treatment or control interventions (Bell‐Connecticut, Chandler‐LongBeach, Drake‐New Hampshire1, Drake‐Washington, Gervey‐New York, McFarlane‐New York, Okpaku‐Nashville, Wolkon‐Cleveland). In ten trials it was either unclear how far raters were independent (Becker‐Fort Worth, Griffiths‐London, Kline‐Philadelphia, Kuldau‐California), or it was clear that they were not independent (Beard‐NewYork, Blankertz‐Philadelph, Bond‐Chicago1, Bond‐Indiana, Dincin‐Chicago, Walker‐Massachusetts).
3. Description of loss to follow up Follow up rates were generally good: 16 trials had loss to follow up rates of 20% or less (Beard‐NewYork, Becker‐Fort Worth, Bell‐Connecticut, Blankertz‐Philadelph, Bond‐Chicago1, Bond‐Indiana, Drake‐New Hampshire1, Drake‐Washington, Gervey‐New York, Griffiths‐London, Kline‐Philadelphia, Kuldau‐California, McFarlane‐New York, Okpaku‐Nashville, Walker‐Massachusetts, Wolkon‐Cleveland). Loss to follow up rates of greater than 20% were found in the following trials: Chandler‐LongBeach (21% at one year); Dincin‐Chicago (37% at nine months);
4. Confounding of interventions There was confounding of the intervention in two trials. In Chandler‐LongBeach experimental patients received Assertive Community Treatment in addition to Supported Employment, whilst in McFarlane‐New York experimental patients received Family‐aided Assertive Community Treatment in addition to Supported Employment.
5. Sensitivity analysis In the initial analyses data from all included trials, regardless of quality, were analysed within the relevant comparisons. Subsequently, these analyses were repeated excluding data from trials with: (a) allocation concealment in categories B or C; (b) non‐independent evaluators; (c) follow up rates of less than 80%; (d) confounding of interventions. As it turned out, only two trials, both of Supported Employment versus Pre‐vocational Training (Drake‐New Hampshire1, Drake‐Washington), met criteria for inclusion in the sensitivity analysis.
Effects of interventions
1. Reliability of data extraction and funnel plot There were no disagreements between the raters on which trials should be discarded on the basis of abstracts obtained from the electronic search. Inter‐rater reliability for inclusion of trials in the review, once full text had been obtained, based on a sample of 20 trials, was 0.89. There was full agreement between raters on categorisation of included trials. There were insufficient data to draw funnel plots in most comparisons, however it was possible to draw a funnel plot for the variable 'not in competitive employment at 12 months' in the comparison: 'Supported Employment versus Pre‐vocational Training'. This plot showed evidence of asymmetry attributable to Gervey‐New York, which found a large effect size in favour of Supported Employment. It was not clear whether the asymmetry in the funnel plot indicated publication bias or whether it was due to inadequate allocation concealment in this trial. Gervey‐New York was not eligible for the sensitivity analysis.
2. PRE‐VOCATIONAL TRAINING versus STANDARD HOSPITAL CARE Three trials, with a total of 200 patients, contributed data to this comparison (Becker‐Fort Worth, Kuldau‐California, Walker‐Massachusetts).
2.1 Not in competitive employment Few data were available on the primary outcome. One small trial (Becker‐Fort Worth) reported data at eight month follow up which showed a non‐significant trend in favour of clients in Pre‐vocational Training (n=50, RR 0.79 CI 0.63 to 1.00).
2.2 Secondary employment outcomes Becker‐Fort Worth reported that at eight months, a significantly larger number of clients in Pre‐vocational Training had obtained any form of employment (n=50, RR 0.42 CI 0.26 to 0.68, NNT 1.8). Walker‐Massachusetts, however, reported no difference in hours/month in competitive employment (n=28, Pre‐vocational Training mean 36.8, control 31.6, p=0.92, Mann Whitney). Kuldau‐California reported that Pre‐vocational Training clients earned significantly more dollars per month than controls (Pre‐vocational Training mean $176.2, control mean $97.3, p <.01). There was a non‐significant trend towards better participation amongst Pre‐vocational Training clients (n=78, RR 0.5 CI 0.05 to 5.25).
2.3 Clinical outcomes The limited data available suggested that clients in Pre‐vocational Training were not more likely to be discharged from hospital (n=50, RR 0.95 CI 0.76 to 1.19).
2.4 Sensitivity analysis No trials met criteria for inclusion in the sensitivity analysis (see Methodological Quality of Included Studies, section 5 above).
3. PRE‐VOCATIONAL TRAINING (ALL APPROACHES) versus COMMUNITY CARE Five trials involving a total of 1204 patients contributed data to this comparison (Beard‐NewYork, Dincin‐Chicago, Griffiths‐London, Okpaku‐Nashville, Wolkon‐Cleveland).
3.1 Not in competitive employment Some limited data (Griffiths‐London and Beard‐NewYork) were available on the primary outcome at 18 and 24 months. These showed no difference between Pre‐vocational Training and control (18 months n=28, RR 1.18 CI 0.87 to 1.61; 24 months n=215, RR 0.95 CI 0.77 to 1.17).
3.2 Secondary employment outcomes Three trials reported data on number in any form of employment. These data showed no difference between Pre‐vocational Training and control at three, six, nine, 12 and 18 months.
3.3 Clinical outcomes Data from two trials (Dincin‐Chicago, Okpaku‐Nashville) showed no significant difference in the number of clients participating in the program (n=284, RR random effects 0.95 CI 0.52 to 1.7) between Pre‐vocational Training and control groups. Data from three trials (Beard‐NewYork, Dincin‐Chicago, and Wolkon‐Cleveland) showed that significantly fewer patients were admitted to hospital amongst those receiving Pre‐vocational Training (N= 887, RR 0.79 CI 0.65 to 0.95). However, heterogeneity was present on this outcome and re‐analysis using a random effects model failed to show a significant difference (RR random effects 0.71 CI 0.48 to 1.04). Griffiths‐London reported no difference in self‐esteem (Self‐confidence scale, Wing 1966) between Pre‐vocational Training and control groups (n=28, Pre‐vocational Training mean 25.5, SD 6.6, control mean 23.3, SD 7.3).
3.4 Costs One trial (Dincin‐Chicago) reported mean monthly total healthcare costs of $417.90 for Pre‐vocational Training and $651.50 for controls, but no statistical analysis was reported.
3.5 Sensitivity Analysis No trials met criteria for inclusion in the sensitivity analysis (see Methodological Quality section 5 above).
4. SUB‐ANALYSIS 1: CLUBHOUSE APPROACH (TYPE OF PRE‐VOCATIONAL TRAINING) versus STANDARD COMMUNITY CARE Only one trial (Beard‐NewYork) provided data for this sub‐analysis.
4.1 Not in competitive employment On the primary outcome at 24 months there was no difference between people allocated to Clubhouse approach in addition to standard care and those in the control group (n=215, RR 0.95 CI 0.77 to 1.17).
4.2 Secondary employment outcomes Beard‐NewYork showed no significant difference between the Clubhouse approach and control in numbers obtaining any form of employment at three, six and 12 months.
4.3 Clinical outcomes Beard‐NewYork found significantly fewer admissions to hospital for patients amongst clients in the Clubhouse group (N=215, RR 0.69 CI 0.46 to 0.96, NNT 6.1).
5. MODIFICATION 1. PRE‐VOCATIONAL TRAINING + PAYMENT versus PRE‐VOCATIONAL TRAINING ALONE One trial (Bell‐Connecticut) provided data for this comparison.
5.1 Not in competitive employment No data were available on the primary outcome.
5.2 Secondary employment outcomes At six month follow‐up significantly more clients in the payment group were in any form of employment (n=150, RR 0.40 CI 0.28 to 0.57, NNT 2.2). Clients in the payment group earned significantly more per month (payment group mean $192, non‐payment group mean $32.03, t=7.56, p<0.0001).
5.3 Clinical outcomes Significantly more clients from the payment group participated in the programme (n=150, RR 0.53 CI 0.39 to 0.71, NNT 2.8). There were also significantly fewer admissions to hospital in the payment group (RR 0.55 CI 0.31 to 0.96, NNT 6.4) and they showed significantly better total symptom scores (PANSS, Kay 1987) (payment mean 66.2, SD 15.1, non‐payment mean 72.6, SD 15.0. p<0.02).
6. MODIFICATION 2. PRE‐VOCATIONAL TRAINING + PSYCHOLOGICAL INTERVENTIONS versus PRE‐VOCATIONAL TRAINING ALONE Two trials (Kline‐Philadelphia, Blankertz‐Philadelph) provided data for this comparison.
6.1 Not in competitive employment On the primary outcome at six to nine month follow up there was a difference in favour of Pre‐vocational Training and psychological intervention (n=142, RR 0.86 CI 0.78 to 0.95, NNT 7.1). However, there was evidence of heterogeneity on this variable (Chi squared test 3.12, p=0.077): both trials found an effect in favour of the intervention, but the effect size was larger in the smaller trial (Kline‐Philadelphia n=20, RR 0.56 CI 0.29 to 1.07; Blankertz‐Philadelph n=122, RR 0.90 CI 0.83 to 0.98). Reanalysis using a random effects model found no significant difference (RR 0.76 CI 0.44 to 1.33).
6.2 Secondary employment outcomes One trial (Blankertz‐Philadelph) found that clients receiving psychological intervention were significantly more likely to be in some form of employment (n=122, RR 0.89 CI 0.81 to 0.97, NNT 8.7) or in some form of employment, training or education at the end of the study (n=122, RR 0.63 CI 0.52 to 0.77, NNT 2.8).
6.3 Clinical outcomes Both trials reported data on numbers not participating in the programme, but found no significant difference between intervention and control groups (n=142, RR 0.85 CI 0.33 to 2.18).
6.4 Sensitivity Analysis Neither trial met criteria for inclusion in the sensitivity analysis (see Methodological Quality section 5 above).
7. MODIFICATION 3. ACCELERATED ENTRY TO TRANSITIONAL EMPLOYMENT (A TYPE OF PRE‐VOCATIONAL TRAINING) versus GRADUAL ENTRY TO TRANSITIONAL EMPLOYMENT One trial (Bond‐Chicago1) provided data for this comparison.
7.1 Not in competitive employment On the primary outcome there was no difference between groups at nine and 15 months (although there was a result in favour of accelerated placement, that fell just sort of significance at 15 months, n=131, RR 0.88 CI 0.78 to 1.0).
7.2 Secondary employment outcomes Clients in the accelerated condition were not more likely to be in any form of employment at 15 months (n=131, RR 0.96 CI 0.69 to 1.33), but earned more per month (accelerated condition mean $115.3, control mean $38.9, no statistical analysis).
7.3 Clinical outcomes There was no difference in participation rates between the two groups at nine or 15 months.
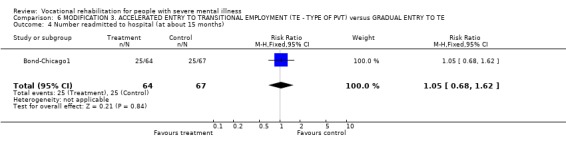
8. SUPPORTED EMPLOYMENT versus STANDARD COMMUNITY CARE One trial, involving 256 patients, contributed data to this comparison (Chandler‐LongBeach).
8.1 Not in competitive employment On the primary outcome there was no difference between Supported Employment and control at 12 months (n=256, RR 1.01 CI 0.93 to 1.09), but there was a significant difference favouring Supported Employment at 24 months (n=256, RR 0.92 CI 0.85 to 0.99, NNT 12.6) and 36 months (n=256, RR 0.88 CI 0.82 to 0.96, NNT 9).
8.2 Secondary employment outcomes Supported Employment clients were significantly more likely to be in any form of employment at 12 months (n=256, RR 0.79 CI 0.70 to 0.90, NNT 5.5) and also earned significantly more per month (Supported Employment mean $60.5, control mean $26.9, p<0.05).
8.3 Clinical outcomes There was no significant difference in participation rates between Supported Employment and control, although there was a result favouring Supported Employment (n=256, RR 0.74, CI 0.55 to 1.01). There was no difference in the number of hospital admissions between Supported Employment and control (n=256, RR 0.83 CI 0.63 to 1.10).
8.4 Costs Mean monthly healthcare costs were significantly higher for clients in Supported Employment (Supported Employment mean $1599, control mean $527.30), but this finding was difficult to interpret as Supported Employment clients were also receiving Assertive Community Treatment.
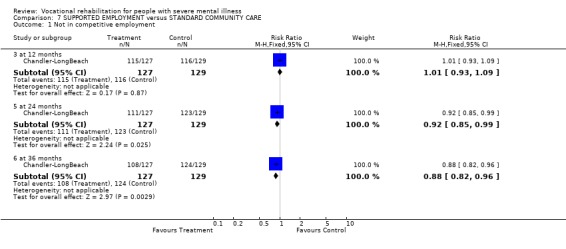
9. SUPPORTED EMPLOYMENT (ALL APPROACHES) versus PRE‐VOCATIONAL TRAINING Five trials, involving 484 patients, contributed data to this comparison (Drake‐New Hampshire1, Drake‐Washington, Bond‐Indiana, Gervey‐New York, McFarlane‐New York).
9.1 Not in competitive employment On the primary outcome there was a difference in favour of supported employment at four, six, nine, 12, 15 and 18 months, e.g. at four months n=364, RR random effects 0.75 CI 0.64 to 0.89, and at 12 months, n=484, RR random effects 0.76 CI 0.64 to 0.89, NNT 4.5 CI 4.48 to 4.63. At 12 months 34% of clients were employed in the Supported Employment group, but only 12% in the Pre‐vocational Training group. There was no significant heterogeneity on this variable at any time point.
9.2 Secondary employment outcomes Three trials found that clients in Supported Employment had significantly more hours per month in competitive employment than those receiving Pre‐vocational Training (Table 01). Three of four trials also found that clients in Supported Employment had higher mean monthly earnings that those in the Pre‐vocational Training (Table 02).
9.3 Clinical outcomes There was no significant difference in participation rates between Supported Employment and control at six, 12, and 18 months (12 month data analysed using random effects model due to heterogeneity). Drake‐New Hampshire1 reported no difference in overall functioning (General Assessment Scale, Endicott 1976), self‐esteem (Rosenberg scale, Rosenberg 1969) or mental state (BPRS scale, Lukoff 1986), but did not report any raw data. Drake‐Washington reported no significant differences at six, 12 and 18 months in: (a) Global outcome (GAS, e.g. at 18 months Supported Employment 45.8 (SE 1.43), control 46.0 (SE 1.78)); (b) Self‐esteem (Rosenberg Scale, e.g. at 18 months Supported Employment 18.5 (SE 0.7), control 18.1 (SE 0.68), (c) Quality of Life (Lehman's scale, Lehman 1983, e.g. at 18 months Supported Employment 5 (SE 0.17), control 4.8 (SE 0.18)) or (d) psychiatric symptoms (BPRS, e.g. at 18 months Supported Employment 39.2 (SE 1.19), control 41.1(SE 1.54)).
9.4 Costs Bond‐Indiana reported that the programme costs of Supported Employment were greater than for Pre‐vocational Training, but that other health care costs were reduced (no statistical analysis), so that overall health care costs were less for Supported Employment. Drake‐New Hampshire1 found no significant difference in program costs or overall health care costs between Supported Employment and Pre‐vocational Training (Table 03).
9.5 Sensitivity Analysis Two trials (Drake‐New Hampshire1, Drake‐Washington) met criteria for inclusion in the sensitivity analysis. As these trials were the only trials included in Sub‐analysis 2 (see item 10, below) the results of the sensitivity analysis were the same as those of Sub‐analysis 2 and were similar to those of the analysis involving all five trials.
10. SUB‐ANALYSIS 2: INDIVIDUAL PLACEMENT & SUPPORT (IPS ‐ TYPE OF SUPPORTED EMPLOYMENT) versus PRE‐VOCATIONAL TRAINING Two trials (Drake‐New Hampshire1, Drake‐Washington) provided data for this comparison.
10.1 Not in competitive employment On the primary outcome there was a difference in favour of IPS clients at four, six, nine, 12, 15 and 18 months. For example, at four months, n=295, RR 0.7 CI 0.6 to 0.8, and at 12 months n=295, RR 0.79 CI 0.70 to 0.89, NNT 5.5. At 12 months 30% of people allocated to IPS were employed as against 12% in Pre‐vocational Training.
10.2 Secondary employment outcomes Both trials reported that IPS clients spent significantly more hours per month in competitive employment (Table 1). One trial (Drake‐New Hampshire1) reported significantly higher mean monthly earnings, but the other (Drake‐Washington) found no difference, (although the IPS grouped earned more from competitive employment ‐ see Table 2).
1. Supported Employment versus PVT: Mean hours in competitive employment.
| Study | Intervention | Mean monthly hrs | t (or F) | p |
| Drake‐NH | IP | 33.7 | 3.7 | <0.001 |
| PVT | 11.4 | |||
| Drake‐Wash | IP | 17.9 | 4.4 | <0.001 |
| PVT | 1.5 | |||
| Gervey | IP | 69 | 3.7 | 0.03 |
| PVT | 9.9 |
2. Supported Employment versus PVT: Mean monthly earnings ($).
| Study | Intervention | Mean earnings | t or F | p |
| Bond‐Indiana | SE | 127.1 | 2.55 | <0.05 |
| PVT | 71.7 | |||
| McFarlane‐New York | SE | 41.9 | 2.35 | 0.019 |
| PVT | 11.8 | |||
| Drake‐NH1 | SE | 188.5 | 3.34 | <0.001 |
| PVT | 59.9 | |||
| Drake‐Wash | SE | 111.1 | 4.29 | NS |
| PVT | 111.4 |
10.3 Clinical outcomes IPS clients were not significantly more likely to participate than control clients, although confidence intervals were wide and there was a trend favouring Supported Employment (n=295, RR 0.52 CI 0.15 to 1.85, random effects model). There were no significant differences between groups on: self‐esteem; mental state; overall functioning; or quality of life at any time point (see 9.3 above).
10.4 Costs Drake‐New Hampshire1 found no significant difference in program costs or overall health care costs between IPS and Pre‐vocational Training (Table 3).
3. Supported Employment versus PVT: Costs of care (mean monthly per patient).
| Study | Group | Program costs | Other health costs | Overall costs |
| Bond‐Indiana | Immediate Placement | $251.6 | $263.0 | $514.6 |
| Control | $132.0 | $586.5 | $718.5 | |
| Drake‐NH1 | Immediate Placement | $313.1 | $801.6 | $1114.7 |
| Control | $307.3 | $928.5 | $1235.8 |
Discussion
1. General 1.1 Methodological limitations affecting the ability to detect improved outcomes The review found little evidence that Supported Employment or Pre‐vocational Training improved symptoms, quality of life or social functioning. This finding is difficult to interpret, however, as only a minority of participants in vocational rehabilitation trials actually find competitive employment (about one third in the most effective Individual Placement and Support trials). Therefore, a large sample would be required to detect clinically significant improvements. There were some indications that this problem was masking symptomatic improvements amongst those people who actually worked. For example, Bell‐Connecticut found a significant improvement in symptoms, after financial inducements had ensured a high participation rate in the treatment group, whilst Drake‐New Hampshire1 reported a sub‐analysis of mental state data showing a significant improvement in clients who obtained competitive work.
1.2 Generalisability There was no evidence that vocational rehabilitation trials were 'cherry‐picking' clients who were likely to be easy to place in employment. Thus a weighted average of participants in Supported Employment versus Pre‐vocational Training trials showed good recruitment of women and ethnic minorities, with a majority of participants suffering from schizophrenia (see Included Studies table). This suggests that the findings of the review can be applied with confidence to the general population of clients with severe mental disorder. The review is however limited by the fact that all trials (bar one) were conducted in the United States. This limitation makes it uncertain how far the findings can be generalised to countries with less dynamic economies, different welfare structures, or dissimilar cultural attitudes to work.
2. PRE‐VOCATIONAL TRAINING versus STANDARD COMMUNITY CARE OR HOSPITAL CARE 2.1 Employment outcomes The review found no evidence to suggest that Pre‐vocational Training was more effective on the primary outcome than standard community care or hospital care. This was supported by findings on other secondary employment outcomes (although Pre‐vocational Training performed slightly better on some secondary outcomes when compared against a hospital control group).
2.2 Clinical outcomes and costs Clients were not more likely to engage in Pre‐vocational Training than standard care. Whilst clients in Pre‐vocational Training programs appeared less likely to be admitted to hospital than clients receiving standard community care, heterogeneity was present on this outcome and reanalysis using a random effects model found no significant difference, although the result is borderline (RR random effects 0.71 CI 0.48 to 1.04). There were only limited data on costs.
2.3 Sub‐analysis This showed that there was insufficient evidence to judge whether the Clubhouse approach was more effective than other approaches to Pre‐vocational Training.
2.4 Modifications of Pre‐vocational Training There was some evidence that payment improved engagement in Pre‐vocational Training and enhanced its effectiveness. The effect of psychological interventions to enhance motivation was less certain, although there were some promising indications.
3. SUPPORTED EMPLOYMENT versus PRE‐VOCATIONAL TRAINING 3.1 Employment outcomes The main finding of the review was that on the primary outcome, finding competitive employment, Supported Employment was superior to Pre‐vocational Training. Evidence supporting this finding was strong: five randomised trials (n=484) showed that people in Supported Employment were significantly more likely to be in competitive employment at six time points across 18 months. There was no evidence of heterogeneity at any time point. A sensitivity analysis excluding all but the two highest quality trials did not substantially alter this finding. Secondary outcomes such as mean hours worked and mean monthly earnings favoured Supported Employment.
3.2 Clinical outcomes and costs Data were inconclusive, but suggested no major differences between Supported Employment and Pre‐vocational Training.
3.3 Sub‐analysis Data suggested that Individual Placement and Support was an effective form of Supported Employment, but were insufficient to say whether it was more effective than other less carefully specified forms of Supported Employment.
Only one trial (Chandler‐LongBeach) compared Supported Employment to standard community care. Although this trial suggested that Supported Employment was superior to standard community care, its findings are difficult to interpret as the intervention group received Assertive Community Treatment in addition to Supported Employment.
Authors' conclusions
Implications for practice.
This review has suggested that Supported Employment is more effective than Pre‐vocational Training in helping mentally ill people obtain competitive employment. Although Supported Employment is growing in popularity, it is still less widely available than Pre‐vocational Training.
Finding competitive employment is a top priority for many mentally ill people, so the vocational rehabilitation agencies that serve them need to consider how to make Supported Employment more widely available. Purchasers, clinicians and clients should encourage vocational rehabilitation agencies to develop and evaluate more US‐style Supported Employment schemes.
Implications for research.
The effects of Supported Employment should be examined in larger, multi‐centre trials, both within and outside of the United States. Such research is particularly indicated in countries with high rates of unemployment and more extensive welfare systems. Future trials should involve detailed analyses of the cost‐effectiveness of the various vocational rehabilitation models. The trials should also involve standard care control groups, to establish whether there is an effect on hospital admission rates. Researchers planning future trials of Supported Employment should consider standardising this intervention by adhering to the carefully specified Individual Placement and Support model. Research is also indicated to determine how far Pre‐vocational Training (including the Clubhouse approach) affects readmission/relapse rates under modern conditions. Further research is also required to determine how far mental state and social outcome may be improved by working. Methodological considerations may mean that such research may have to take place outside the framework of randomised controlled trials. Finally, there is a case for countries to survey their existing vocational rehabilitation agencies to determine the extent to which the most effective interventions are being offered.
What's new
| Date | Event | Description |
|---|---|---|
| 6 October 2010 | Amended | Contact details updated. |
History
Protocol first published: Issue 3, 1999 Review first published: Issue 2, 2001
| Date | Event | Description |
|---|---|---|
| 11 November 2009 | Amended | Contact details updated. |
| 20 July 2009 | Amended | Author correction |
| 23 April 2008 | Amended | Converted to new review format. |
| 7 December 2000 | New citation required and conclusions have changed | Substantive amendment |
Notes
The views expressed in this paper are not necessarily those of the NHS Health Technology Assessment Programme.
Cochrane Schizophrenia Group internal peer review complete (see Module). External peer review scheduled.
Acknowledgements
The reviewers acknowledge the support of Guild Community Healthcare NHS Trust, and the Cochrane Schizophrenia Group.
Data and analyses
Comparison 1. PRE‐VOCATIONAL TRAINING versus STANDARD HOSPITAL CARE.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Not in competitive employment (at 8 months) | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.63, 1.00] |
| 2 Not in any form of employment (at 8 months) | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.26, 0.68] |
| 3 Not participating in program (excluding employed) | 2 | 78 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.55] |
| 4 Not discharged from hospital (at 8 months) | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.76, 1.19] |
1.1. Analysis.
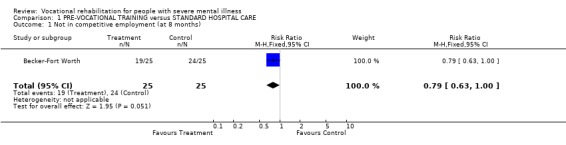
Comparison 1 PRE‐VOCATIONAL TRAINING versus STANDARD HOSPITAL CARE, Outcome 1 Not in competitive employment (at 8 months).
1.2. Analysis.
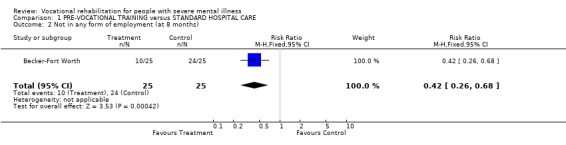
Comparison 1 PRE‐VOCATIONAL TRAINING versus STANDARD HOSPITAL CARE, Outcome 2 Not in any form of employment (at 8 months).
1.3. Analysis.
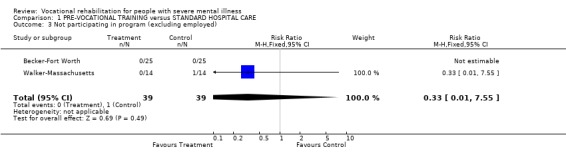
Comparison 1 PRE‐VOCATIONAL TRAINING versus STANDARD HOSPITAL CARE, Outcome 3 Not participating in program (excluding employed).
1.4. Analysis.
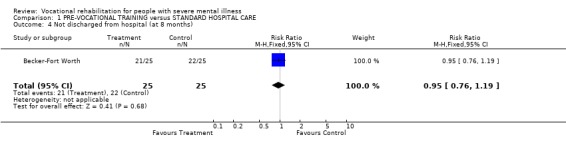
Comparison 1 PRE‐VOCATIONAL TRAINING versus STANDARD HOSPITAL CARE, Outcome 4 Not discharged from hospital (at 8 months).
Comparison 2. PRE‐VOCATIONAL TRAINING (ALL APPROACHES) versus STANDARD COMMUNITY CARE.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Not in competitive employment | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 at 18 months | 1 | 28 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.87, 1.61] |
| 1.2 at 24 months | 1 | 215 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.77, 1.17] |
| 2 Not in any form of employment | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 at 3 months | 1 | 352 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.89, 1.24] |
| 2.2 at 6 months | 1 | 285 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.81, 1.12] |
| 2.3 at 9 months | 1 | 132 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.76, 1.32] |
| 2.4 at 12 months | 1 | 215 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.77, 1.17] |
| 2.5 at 18 months | 1 | 152 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.57, 1.02] |
| 3 Not participating in program (excluding employed) | 2 | 284 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.52, 1.72] |
| 4 Admitted to hospital (by 1 year) | 3 | 887 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.65, 0.95] |
2.1. Analysis.
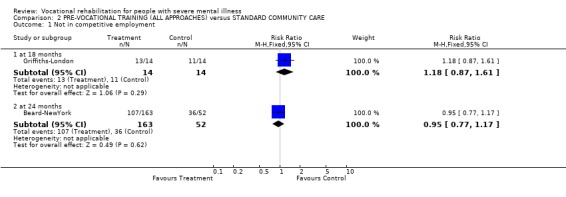
Comparison 2 PRE‐VOCATIONAL TRAINING (ALL APPROACHES) versus STANDARD COMMUNITY CARE, Outcome 1 Not in competitive employment.
2.2. Analysis.
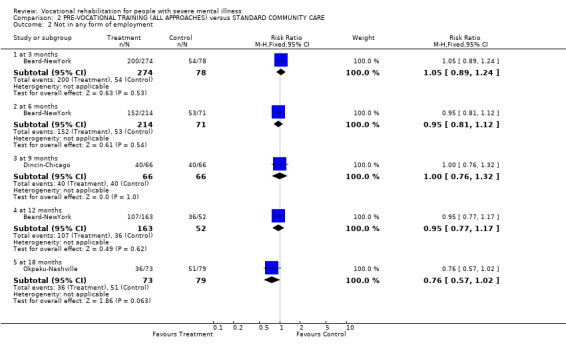
Comparison 2 PRE‐VOCATIONAL TRAINING (ALL APPROACHES) versus STANDARD COMMUNITY CARE, Outcome 2 Not in any form of employment.
2.3. Analysis.
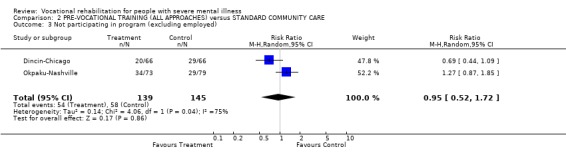
Comparison 2 PRE‐VOCATIONAL TRAINING (ALL APPROACHES) versus STANDARD COMMUNITY CARE, Outcome 3 Not participating in program (excluding employed).
2.4. Analysis.
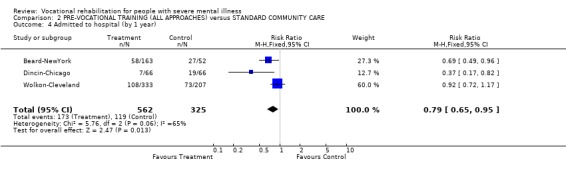
Comparison 2 PRE‐VOCATIONAL TRAINING (ALL APPROACHES) versus STANDARD COMMUNITY CARE, Outcome 4 Admitted to hospital (by 1 year).
Comparison 3. SUB‐ANALYSIS 1: CLUBHOUSE APPROACH (TYPE OF PVT) versus STANDARD COMMUNITY CARE.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Not in competitive employment (at 24 months) | 1 | 215 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.77, 1.17] |
| 2 Not in any form of employment | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 at 3 months | 1 | 352 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.89, 1.24] |
| 2.2 at 6 months | 1 | 285 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.81, 1.12] |
| 2.3 at 12 months | 1 | 215 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.77, 1.17] |
| 3 Admitted to hospital in first year of study | 1 | 215 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.49, 0.96] |
3.1. Analysis.
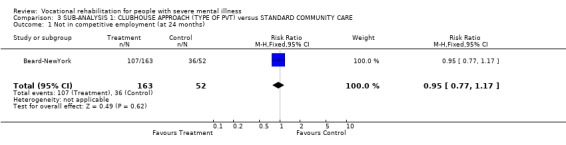
Comparison 3 SUB‐ANALYSIS 1: CLUBHOUSE APPROACH (TYPE OF PVT) versus STANDARD COMMUNITY CARE, Outcome 1 Not in competitive employment (at 24 months).
3.2. Analysis.
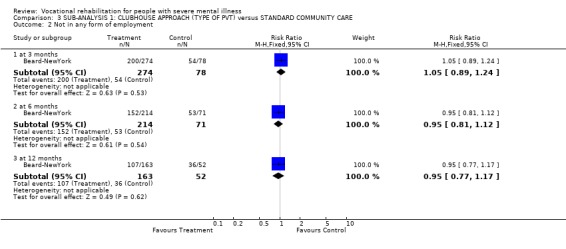
Comparison 3 SUB‐ANALYSIS 1: CLUBHOUSE APPROACH (TYPE OF PVT) versus STANDARD COMMUNITY CARE, Outcome 2 Not in any form of employment.
3.3. Analysis.
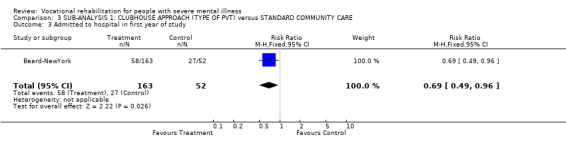
Comparison 3 SUB‐ANALYSIS 1: CLUBHOUSE APPROACH (TYPE OF PVT) versus STANDARD COMMUNITY CARE, Outcome 3 Admitted to hospital in first year of study.
Comparison 4. MODIFICATION 1. PRE‐VOCATIONAL TRAINING + PAYMENT versus PRE‐VOCATIONAL TRAINING ALONE.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Not in any form of employment (at 6 months) | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.28, 0.57] |
| 2 Not participating in program | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.39, 0.71] |
| 3 Admitted to hospital during first year of study | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.31, 0.96] |
4.1. Analysis.
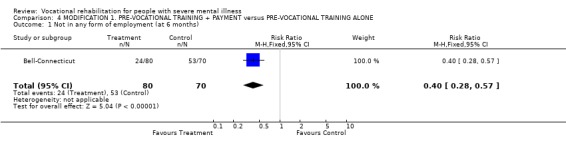
Comparison 4 MODIFICATION 1. PRE‐VOCATIONAL TRAINING + PAYMENT versus PRE‐VOCATIONAL TRAINING ALONE, Outcome 1 Not in any form of employment (at 6 months).
4.2. Analysis.
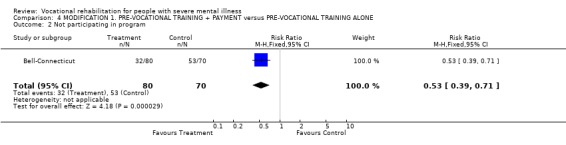
Comparison 4 MODIFICATION 1. PRE‐VOCATIONAL TRAINING + PAYMENT versus PRE‐VOCATIONAL TRAINING ALONE, Outcome 2 Not participating in program.
4.3. Analysis.
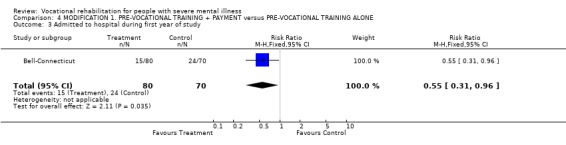
Comparison 4 MODIFICATION 1. PRE‐VOCATIONAL TRAINING + PAYMENT versus PRE‐VOCATIONAL TRAINING ALONE, Outcome 3 Admitted to hospital during first year of study.
Comparison 5. MODIFICATION 2. PRE‐VOCATIONAL TRAINING + PSYCHOLOGICAL INTERVENTIONS versus PRE‐VOCATIONAL TRAINING ALONE.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Not in competitive employment | 2 | 142 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.77, 0.95] |
| 1.1 at 6 months | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.29, 1.07] |
| 1.2 at 9 months | 1 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.83, 0.99] |
| 2 Not in any form of employment | 1 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.81, 0.97] |
| 3 Not in any form or employment or training or education at end of study | 1 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.52, 0.77] |
| 4 Not participating in program | 2 | 142 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.33, 2.18] |
5.1. Analysis.
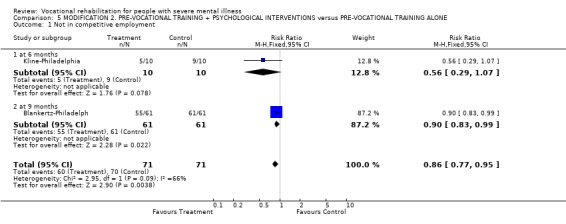
Comparison 5 MODIFICATION 2. PRE‐VOCATIONAL TRAINING + PSYCHOLOGICAL INTERVENTIONS versus PRE‐VOCATIONAL TRAINING ALONE, Outcome 1 Not in competitive employment.
5.2. Analysis.
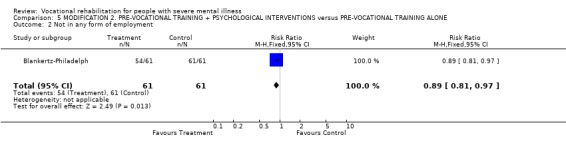
Comparison 5 MODIFICATION 2. PRE‐VOCATIONAL TRAINING + PSYCHOLOGICAL INTERVENTIONS versus PRE‐VOCATIONAL TRAINING ALONE, Outcome 2 Not in any form of employment.
5.3. Analysis.
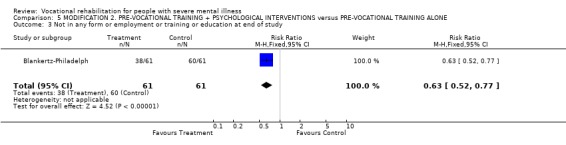
Comparison 5 MODIFICATION 2. PRE‐VOCATIONAL TRAINING + PSYCHOLOGICAL INTERVENTIONS versus PRE‐VOCATIONAL TRAINING ALONE, Outcome 3 Not in any form or employment or training or education at end of study.
5.4. Analysis.
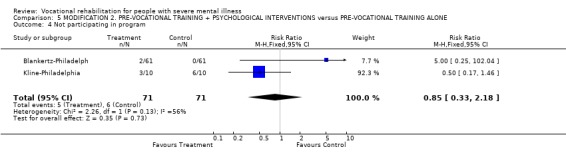
Comparison 5 MODIFICATION 2. PRE‐VOCATIONAL TRAINING + PSYCHOLOGICAL INTERVENTIONS versus PRE‐VOCATIONAL TRAINING ALONE, Outcome 4 Not participating in program.
Comparison 6. MODIFICATION 3. ACCELERATED ENTRY TO TRANSITIONAL EMPLOYMENT (TE ‐ TYPE OF PVT) versus GRADUAL ENTRY TO TE.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Not in competitive employment | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 at 9 months | 1 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.90, 1.10] |
| 1.2 at 15 months | 1 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.78, 1.00] |
| 2 Not in any form of employment (at 15 months) | 1 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.69, 1.33] |
| 3 Numbers not participating in program | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 at 4 months | 1 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.77 [0.98, 3.21] |
| 3.2 at 9 months | 1 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.74, 1.92] |
| 4 Number readmitted to hospital (at about 15 months) | 1 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.68, 1.62] |
6.1. Analysis.
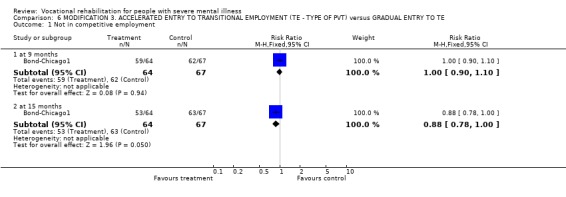
Comparison 6 MODIFICATION 3. ACCELERATED ENTRY TO TRANSITIONAL EMPLOYMENT (TE ‐ TYPE OF PVT) versus GRADUAL ENTRY TO TE, Outcome 1 Not in competitive employment.
6.2. Analysis.
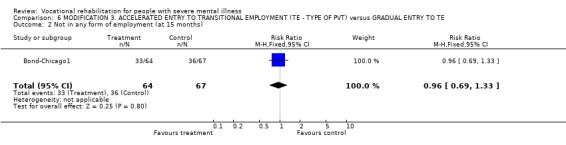
Comparison 6 MODIFICATION 3. ACCELERATED ENTRY TO TRANSITIONAL EMPLOYMENT (TE ‐ TYPE OF PVT) versus GRADUAL ENTRY TO TE, Outcome 2 Not in any form of employment (at 15 months).
6.3. Analysis.
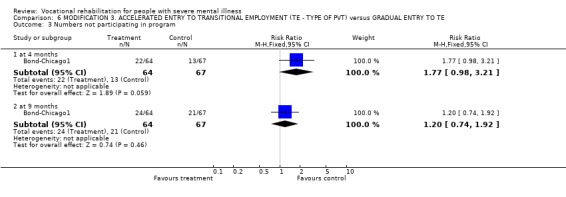
Comparison 6 MODIFICATION 3. ACCELERATED ENTRY TO TRANSITIONAL EMPLOYMENT (TE ‐ TYPE OF PVT) versus GRADUAL ENTRY TO TE, Outcome 3 Numbers not participating in program.
6.4. Analysis.
Comparison 6 MODIFICATION 3. ACCELERATED ENTRY TO TRANSITIONAL EMPLOYMENT (TE ‐ TYPE OF PVT) versus GRADUAL ENTRY TO TE, Outcome 4 Number readmitted to hospital (at about 15 months).
Comparison 7. SUPPORTED EMPLOYMENT versus STANDARD COMMUNITY CARE.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Not in competitive employment | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.3 at 12 months | 1 | 256 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.93, 1.09] |
| 1.5 at 24 months | 1 | 256 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.85, 0.99] |
| 1.6 at 36 months | 1 | 256 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.82, 0.96] |
| 2 Not in any form of employment | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3 Numbers not participating in program | 1 | 256 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.55, 1.01] |
| 4 Numbers admitted to hospital during study | 1 | 256 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.63, 1.10] |
7.1. Analysis.
Comparison 7 SUPPORTED EMPLOYMENT versus STANDARD COMMUNITY CARE, Outcome 1 Not in competitive employment.
7.2. Analysis.
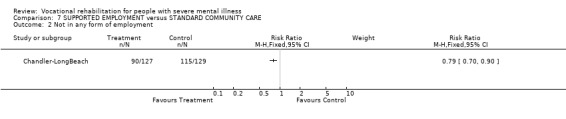
Comparison 7 SUPPORTED EMPLOYMENT versus STANDARD COMMUNITY CARE, Outcome 2 Not in any form of employment.
7.3. Analysis.
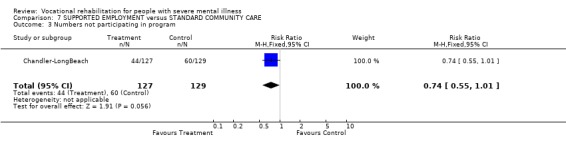
Comparison 7 SUPPORTED EMPLOYMENT versus STANDARD COMMUNITY CARE, Outcome 3 Numbers not participating in program.
7.4. Analysis.
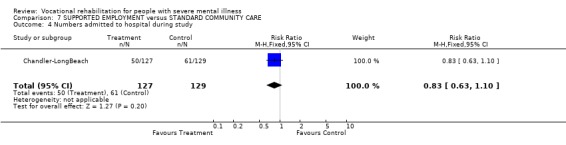
Comparison 7 SUPPORTED EMPLOYMENT versus STANDARD COMMUNITY CARE, Outcome 4 Numbers admitted to hospital during study.
Comparison 8. SUPPORTED EMPLOYMENT (ALL APPROACHES) versus PRE‐VOCATIONAL TRAINING.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Not in competitive employment | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 at about 4 months | 3 | 364 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.66, 0.81] |
| 1.2 at 6 months | 3 | 364 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.67, 0.82] |
| 1.3 at 9 months | 3 | 364 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.60, 0.76] |
| 1.4 at 12 months | 5 | 484 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.69, 0.84] |
| 1.5 at 15 months | 3 | 364 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.73, 0.91] |
| 1.6 at 18 months | 3 | 364 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.71, 0.87] |
| 1.7 at 24 months | 2 | 155 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.81, 1.00] |
| 2 Not in any form of employment | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 at 6 months | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.62, 1.78] |
| 2.2 at 9 months | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.35, 1.08] |
| 2.3 at 12 months | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.40, 1.12] |
| 2.4 at 15 months | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.53, 1.61] |
| 2.5 at 18 months | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.50, 1.33] |
| 3 Numbers not participating in program | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 at 6 months | 1 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.58, 1.54] |
| 3.2 at 12 months | 2 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.48, 0.96] |
| 3.3 at 18 months | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.10, 1.32] |
8.1. Analysis.
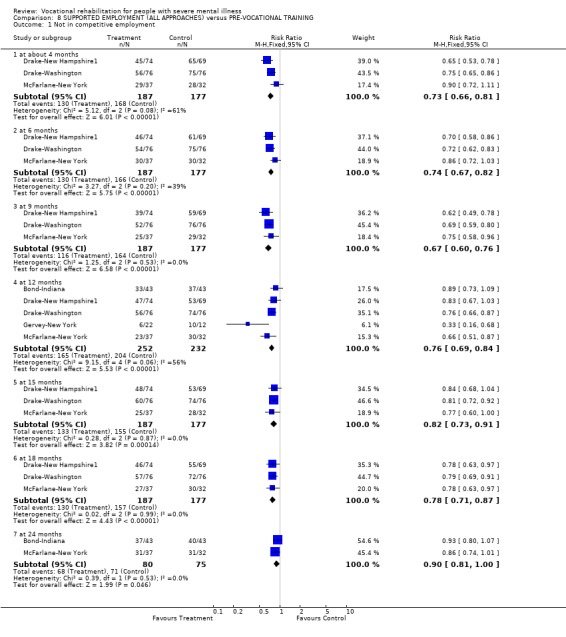
Comparison 8 SUPPORTED EMPLOYMENT (ALL APPROACHES) versus PRE‐VOCATIONAL TRAINING, Outcome 1 Not in competitive employment.
8.2. Analysis.
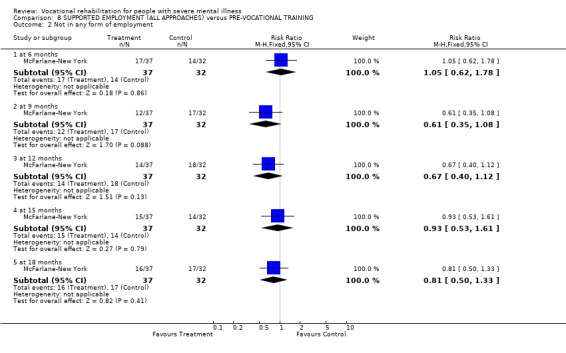
Comparison 8 SUPPORTED EMPLOYMENT (ALL APPROACHES) versus PRE‐VOCATIONAL TRAINING, Outcome 2 Not in any form of employment.
8.3. Analysis.
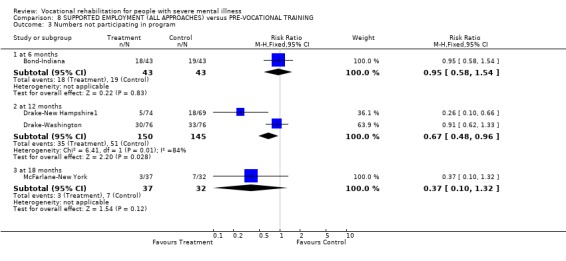
Comparison 8 SUPPORTED EMPLOYMENT (ALL APPROACHES) versus PRE‐VOCATIONAL TRAINING, Outcome 3 Numbers not participating in program.
Comparison 9. SUB‐ANALYSIS 2: INDIVIDUAL PLACEMENT & SUPPORT (TYPE OF SUPPORTED EMPLOYMENT) versus PRE‐VOCATIONAL TRAINING.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Not in competitive employment | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 at 4 months | 2 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.62, 0.78] |
| 1.2 at 6 months | 2 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.63, 0.80] |
| 1.3 at 9 months | 2 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.57, 0.75] |
| 1.4 at 12 months | 2 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.70, 0.89] |
| 1.5 at 15 months | 2 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.74, 0.93] |
| 1.6 at 18 months | 2 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.70, 0.89] |
| 2 Numbers not participating in program | 2 | 295 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.15, 1.85] |
9.1. Analysis.
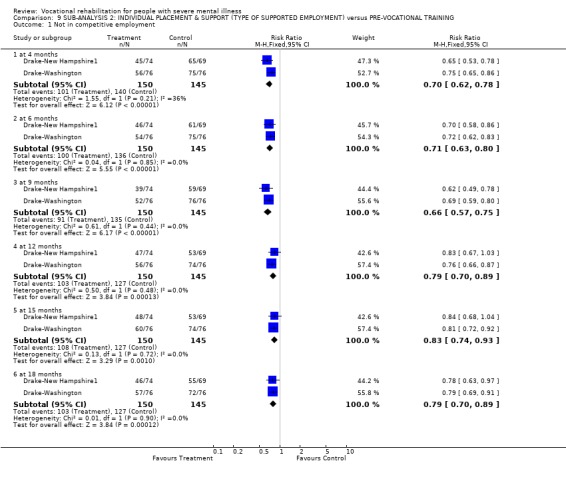
Comparison 9 SUB‐ANALYSIS 2: INDIVIDUAL PLACEMENT & SUPPORT (TYPE OF SUPPORTED EMPLOYMENT) versus PRE‐VOCATIONAL TRAINING, Outcome 1 Not in competitive employment.
9.2. Analysis.
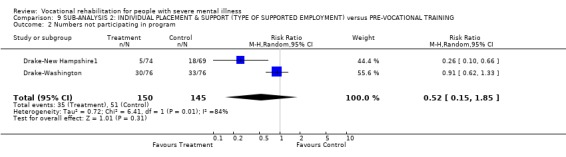
Comparison 9 SUB‐ANALYSIS 2: INDIVIDUAL PLACEMENT & SUPPORT (TYPE OF SUPPORTED EMPLOYMENT) versus PRE‐VOCATIONAL TRAINING, Outcome 2 Numbers not participating in program.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Beard‐NewYork.
| Methods | Allocation: by day of application ‐ patients referred on every fourth day allocated to control group. Follow up: every 3 months for two years.* Lost to follow‐up: 14%, hard to verify from data. Objectivity of rating of outcome: raters not independent. | |
| Participants | Inclusion criteria: i. discharged from in‐patient psychiatric care in last 4 months; ii. in‐patient >2 months; iii. no primary diagnosis of substance abuse, "overt homosexuality", epilepsy, "criminal behaviour"; iv. local resident. Diagnosis: schizophrenia, schizophrenia‐like disorders (82%). N=352. Age: 68% under 35. Sex: 40% women. Race: 12% non‐white. History: ever married 23%, ever employed U/K, time since last employment U/K, previous admissions >1. Setting: urban psychiatric rehabilitation centre, New York, USA. | |
| Interventions | 1. Clubhouse group: i. social activities; ii. "work‐ordered day" on work‐crews; iii. transitional employment for 3‐4 months after completing phases i. + ii.; iv. real job placement with outreach and supported accommodation (mean daily attendance ˜75, 10 F/t staff, mainly psychiatric social workers, emergency psychiatric consultation provided by P/t psychiatrist. N=274. 2. Control: continued to receive community care from other services (not specified). N=78. | |
| Outcomes | In competitive employment.* In any form of employment. Not participating in program. Rehospitalised. | |
| Notes | * Not all patients followed up for a full two years ‐ patients continued to enter the study until the last 3 months. Thus numbers followed up are different at different time points. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Becker‐Fort Worth.
| Methods | Allocation: 'randomly assigned' ‐ no details given. Follow up: 8 months.* Lost to follow‐up: 0%. Objectivity of rating of outcome: unclear. | |
| Participants | Inclusion criteria: i. age <62; ii. in psychiatric hospital >2 years in last 4; iii. no dementa or severe disability; iv. not about to be discharged; v. no unpredictable violence (149/411in‐patients excluded, random sample of 50 selected from remainder). Diagnosis: schizophrenia, schizophrenia‐like disorders (78%). N=50. Age: mean ˜46 years. Sex: not reported. Race: not reported. History: ever married U/K, ever employed >50%, time since last employment >2 years, previous admissions >1, mainly veterans or seamen. Setting: general psychiatric hospital, Texas, USA. | |
| Interventions | 1. Specialised rehabilitation ward: i. intensive multi‐disciplinary input; ii. social skills groups; iii. group and individual vocational assignments; iv. tours of local industrial facilities; v. sheltered workshop; vi. transitional work experience in local community enterprises. N=25. 2. Control: continuing inpatient treatment on rehabilitation wards, option of referral to external vocational rehabilitation services. N=25. | |
| Outcomes | In competitive employment. In any employment. Discharged from hospital. Lost to follow up. | |
| Notes | * The full trial was three phases lasting for total of 20 months ‐ only phase 1 is relevant to this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Bell‐Connecticut.
| Methods | Allocation: 'randomised' ‐ method not specified. Follow up: 5 months. Lost to follow‐up: 4%. Objectivity of rating of outcome: independent raters. | |
| Participants | Inclusion criteria: i. diagnosis of schizophrenia or related disorder; ii. stable (no changes in drugs, housing or treatment status in month); iii. no organic brain disease or physical disability. Diagnosis: schizophrenia, schizophrenia‐like disorders (100%). N=150. Age: mean ˜43 years. Sex: 4% women. Race: 31% non‐white. History: ever married U/K, ever employed U/K, time since last employment U/K, previous admissions ˜8.5. Setting: general hospital, Conneticut, USA. | |
| Interventions | 1. Sheltered set‐aside jobs in the hospital: i. up to 20 hours/week; ii. paid $3.4/hour; iii. worked alongside regular hospital staff in posts ranging from administrative to portering; iv. attended weekly 50 minute support group. N=80. 2. Control: as above but not paid. N=70. Both groups continued to receive benefit entitlement. | |
| Outcomes | In any type of employment.*
Monthly earnings.
Not participating in program.
Rehospitalised.
Mental state: PANSS. Unable to use ‐ Time in any form of employment (not primary or secondary outcome variable). |
|
| Notes | * People lost to follow up treated as not working. 6 patients in control group transferred to half‐way house and excluded because it had its own work program ‐ treated as working and as not dropping out. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Blankertz‐Philadelph.
| Methods | Allocation: random allocation with "oversampling of experimental group" ‐ not clear what this means.* Follow up: 9 months. Lost to follow‐up: 0%. Objectivity of rating of outcome: raters not independent. | |
| Participants | Inclusion criteria: i. severe mental illness (unspecified); ii. unemployed; iii. client of CMHC. Diagnosis: schizophrenia, schizophrenia‐like disorders (72%). N=122. Age: mean 36 years. Sex: 36% women. Race: 20% non‐white. History: ever married 16%, ever employed 82%, time since last employment ˜9 years, previous admissions U/K. Setting: CMHC, Philadelphia, USA. | |
| Interventions | 1. Two employment specialists: using counselling, social learning techniques, group sessions, rewards for passing up a "ladder" of success (making positive changes, setting goals, making transition to state vocational rehabilitation centre, entering the world of work). No specific prevocational training, but some job finding for a few who did not want to enter the VR system, plus usual CMHT. N=61. 2. Control: usual services of CMHT: including partial hospitalisation, outpatient services, therapy and medication management. No specific vocational services, but could have referral to state VR service. N=61. | |
| Outcomes | In competitive employment. Not participating in program. In any form of employment or education. Unable to use ‐ Self‐esteem: Rosenberg's scale (no comparison with control group). Social functioning: Social Level of Functioning Scale (no comparison with control group). | |
| Notes | * Method of randomisation unusual ‐ the paper suggests that a high drop‐out rate after randomisation led to replacement of people in the treatment group ‐ but this is not explicit. It is possible that this is not an intention to treat analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Bond‐Chicago1.
| Methods | Allocation: random assignment ‐ information from trialists indicates that sealed envelope method was used. Follow up: 4,9,15 months. Lost to follow‐up: 18%. Objectivity of rating of outcome: raters not independent. | |
| Participants | Inclusion criteria: i. age >18; ii. no prior participation in program; iii. unemployed; iv. wanting employment; v. attendance of >40 hours in first 4 weeks after admission (drop‐out rate of 20% before screening). Diagnosis: schizophrenia, schizophrenia‐like disorders (55%). N=131. Age:mean ˜25 years. Sex: 31% women. Race: 25% non‐white. History: ever married U/K, ever employed 72%, time since last employment 9 months, previous admissions U/K but 48% >3 admissions. Setting: urban, private psychosocial rehabilitation agency, Chicago, USA. | |
| Interventions | 1. Immediate job placement: i. paid transitional employment (minimum 2 days/week); ii. no prevocational preparation; iii. strong expectation to engage in paid employment; iv. close supervision by staff member. N=64. 2. Control: i. gradual approach to supported employment; ii. remained in unpaid prevocational work crew (minimum 4 months); iii. followed 'standard' schedule; iv. if placement failed returned to work crews before starting again; v. volunteer placements also available. N=67. Both groups could participate in individual and group counselling, evening support groups and a job‐club. | |
| Outcomes | In competitive employment.
In any employment.
Monthly earnings.
Not participating in program.
Rehospitalised.
In any form of employment or education. Unable to use ‐ Time in employment (not primary or secondary outcome). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Bond‐Indiana.
| Methods | Allocation: 'randomly assigned' ‐ information from trialists indicates that randomisation was by an independent co‐ordinator using sealed envelopes. Follow up: 12, 24, 48 months. Lost to follow‐up: 14% at 1 year, 6% at 4 years ‐ only 1 site followed up at 4 years. Objectivity of rating of outcome: raters not independent. | |
| Participants | Inclusion criteria: i. age 18‐60; ii. severe mental disorder (Indiana Department of Mental Health Criteria ‐ based on diagnosis, disability & duration); iii. eligible for disability benefit; iv. enrolled in the CMHC community support program; v. no recent V‐R; vi. unemployed >3 months; vii. wanting to work; viii. consistent attendance at CMHC over preceding 4 weeks. Diagnosis: schizophrenia, schizophrenia‐like disorders (66%). N=86. Age: mean ˜35 years. Sex: 49% women. Race: 20% non‐white. History: ever married 52%, ever employed 82%, time since last employment 38 months, previous admissions 5.3. Setting: 4 CMHTs, 57%:43% urban:rural population, Indiana, USA. | |
| Interventions | 1. Immediate entry into supported employment: >4 months preparation in prevocational work‐readiness training then rural CMHC provided i. 2 employment specialists (employed by CMHC, receiving internal referrals, 1 client at a time, intensive job‐coaching at beginning of placement.); ii. follow‐on staff worker (maintained contact after initial adjustment phase) and urban CMHCs provided 3 employment specialists (liaised with teams, carried individual case loads). N=43. 2. Control: >4 months preparation in prevocational work‐readiness training. N=43. | |
| Outcomes | In competitive employment.
Not participating in program.
Monthly earnings.
Costs: program costs, all heatlh care costs. Unable to use ‐ In competitive employment at 48 months (follow up <50%). Admitted to hospital (no data). Time in any employment (not a primary or secondary outcome variable). |
|
| Notes | Two separate trials described in the reports. Both involve accelerated placement in supported employment. One involves VR team integrated into a CMHC, the other, an independent VR team liaising with 4 different CMHCs. Not possible to report all data separately for the two trials. The integrated site has a slightly better outcome for the accelerated group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Chandler‐LongBeach.
| Methods | Allocation: 'randomised' ‐ no further details. Follow up: 12, 24, 36 months. Lost to follow up: 21% at 1 year, 29% at 3 years. Objectivity of rating of outcome: raters independent. | |
| Participants | Inclusion criteria: i. "serious & persistent mental disorder" (DSM‐III‐R); ii. no primary diagnosis of substance abuse; iii. substantial functional impairment due to mental disorder (not defined); iv. eligible for public assistance as a result of functional impairment. Diagnosis: schizophrenia, schizophrenia‐like disorders (55.2%). N=256. Age: ˜30% over 45 years. Sex: 43% women. Race: ˜32% non‐white. History: ever married 47%, ever employed U/K, time since last employment U/K but 82% >1year, previous admissions U/K. Setting: integrated services agency, California, USA. | |
| Interventions | 1. Village integrated services agency: i. assertive community treatment; ii. employment program based at central site (possible immediate entry into employment opportunities [cafe, store, catering service, client bank, janitor service]); iii. two staff to develop competitive jobs and support clients (supported employment). Finding employment was key value of program. N=127. 2. Control: usual mental health services i. limited case management; ii. limited amount of other rehabilitative services. N=129. | |
| Outcomes | In competitive employment.
In any employment.
Monthly earnings.
Admitted to hospital.
Not participating in program.
Costs: total mental health costs. Unable to use ‐ Other clinical outcomes are available but unclear how far they are attributable to Assertive Community Treatment and how far to supported employment (see text for explanation). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Dincin‐Chicago.
| Methods | Allocation: 'random assignment at intake' ‐ information from trialists indicates randomisation was by independent trial co‐ordinator using sealed envelopes. Follow up: 9 months. Lost to follow‐up: 37%. Objectivity of rating of outcome: raters not independent. | |
| Participants | Inclusion criteria: i. severe mental disorder; ii. accepted by agency for rehabilitation; iii. no primary diagnosis of substance abuse or mental retardation; iv. age >19. Diagnosis: schizophrenia, schizophrenia‐like disorders (86%). N=132. Age: mean ˜25 years. Sex: 47% women. Race: not reported. History: ever married U/K, ever employed U/K, time since last employment U/K, previous admissions ˜3. Setting: urban, privately operated VR centre, Chicago, USA. | |
| Interventions | 1. Threshold rehabilitation program: i. individual case work; ii. work crews leading to transitional employment; iii. problem‐solving and activity groups; iv. linked residential facilities (where suitable); v. special education program; vi. medication and relapse discussion group; vii. staff:patient ratio 1:10. N=66. 2. Control: 6 hours/week supportive treatment "widely used by practitioners who treat severely disturbed clients"; i. referral to existing community services where appropriate; ii. discussion and peer‐support group; iii. visits fortnightly by consulting psychiatrist (prescribed and discussed medication); iv. in nearby church; v. staffed by 2 P/t workers and volunteers; vi. staff:patient ratio 1:20. N=66. | |
| Outcomes | In competitive employment. Admitted to hospital. Not participating in program.* Costs of care. | |
| Notes | *15 people in each group excluded from further analysis after randomisation because they failed to participate in programs ‐ have been added to the denominator for number not participating. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Drake‐New Hampshire1.
| Methods | Allocation: 'randomly assigned' ‐ information from trialists indicated that randomisation was by an off‐site co‐ordinator using computer‐generated random numbers. Follow up: monthly for 2 years (preceded by 4 once‐weekly "informational" meeting). Lost to follow‐up: 2%. Objectivity of rating of outcome: raters independent. | |
| Participants | Inclusion criteria: i. major mental illness with major role dysfunction for past 2 years; ii. in community >1 month; iii. living locally; iv. age 20‐65 years; v. unemployed >1 month, wanting to work; vi. no substance dependence, physical disability, or memory impairment. Diagnosis: schizophrenia, schizophrenia‐like disorders (46.9%). N=143. Age: mean ˜37years. Sex: 52% women. Race: 5% non‐white. History: ever married 50%, ever employed ‐ "relatively good employment history", time since last employment U/K, previous admissions U/K but "many" hospitalised in last year. Setting: urban, New Hampshire, USA. | |
| Interventions | 1. Individual placement and support program: i. integrated team working within mental health services; ii. employment specialists attached directly to clinical teams (helped clients find jobs immediately, provided on‐job training, supportive follow‐up); iii. 3 staff working directly with clients in all phases of supported employment (direct contact time with staff ˜62 hours). N=74. 2. Brokered model (GST) pre‐employment preparation group: i. discussions of skills needed to get and keep jobs; ii. practising these skills; ii. exploration of work‐related values; iii. exploration of clients' strengths and weaknesses as workers; iv. interview skills meetings; v. discussion of job leads and interviews (meetings 2/week); vi. once employed received on job support (liaison with mental health providers, follow‐along support); vii. 3 staff divided functions into job training, job development, and job support roles (direct contact time with staff=74 hours). N=69. | |
| Outcomes | In competitive employment.
Time in competitive employment.
Monthly earnings.
Not participating in program.
Global functioning: GAS scores.
Self‐esteem: Rosenberg's scale
Mental state: BPRS expanded.
Costs: program costs, all heatlh care costs. Unable to use ‐ Quality of life: Lehman's scale (subscales only). |
|
| Notes | Two centre trial but not possible to separate the data by site. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Drake‐Washington.
| Methods | Allocation: by off‐site co‐ordinator using random number tables, stratified according to work history (information from trialists). Follow up: 6, 12 & 18 months. Lost to follow up: 5% at 18 months. Objectivity of rating of outcome: raters independent. | |
| Participants | Inclusion criteria: i. severe mental disorder; ii. unemployed; iii. no memory impairment or medical illness precluding working/participating in job interviews. Diagnosis: schizophrenia, schizophrenia‐like disorders (67%). N=152. Age: mean ˜39 years. Sex: 61% women. Race: 83% non‐white. History: ever married 34%, ever employed U/K, time since last employment U/K, previous admissions U/K. Setting: urban, Washington DC, USA. | |
| Interventions | 1. Individual Placement and Support (IPS): i. rapid job search; ii. follow‐on support after securing work (counselling, transportation, intervening with employer); iii. 3 employment specialists (25 clients each). N=76. 2. Enhanced Vocational Rehabilitation (EVR): i. VR service enhanced by extra VR counselor who monitored clients' satisfaction with service; ii. goal of competitive employment but involved prevocational experiences, work adjustment training in sheltered workshop (primarily paid). N=76. | |
| Outcomes | In competitive employment.
Monthly earnings.
Mental state: BPRS expanded.
Quality of life: Lehman's scale.
Self‐esteem: Rosenberg's scale. Unable to use ‐ In any employment throughout study (not primary or secondary outcome). Satisfaction with leisure/finances/job/housing/town (sub‐scale of Lehman's scale). Time to find employment (not primary or secondary outcome measure). Days in hospital (not primary or secondary outcome measure). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Gervey‐New York.
| Methods | Allocation: 'randomly assigned' ‐ information from trialists indicates this was "lots drawn from a hat". Follow up: 12 months (preceded by assessment and vocational skills training phase). Lost to follow‐up: 0% ‐ difficult to verify. Objectivity of rating of outcome: raters independent. | |
| Participants | Inclusion criteria: i. severely disabled by major mental illness (SCID); ii young (not specified). Diagnosis: schizophrenia, paranoid personality disorder, major affective disorder, attention deficit disorder, oppositional‐defiant disorder (proportions U/K). N=34. Age: mean ˜19 years. Sex: 33% women. Race: 83% non‐white. History: ever married U/K, ever employed 20%, time since last employment U/K, previous admissions U/K, from low‐income families. Setting: densely populated urban centre, New York, USA. | |
| Interventions | 1. Immediate placement in supported employment: support provided through job coaches or a family/peer support group. N=22.* 2. Control: employment training in sheltered workshop setting with weekly individual, family and peer group therapy. N=12. | |
| Outcomes | In competitive employment. Time in competitive employment. | |
| Notes | * Originally 2 groups: a. job placement plus job coaching; and b. job placement with family and peer support. No differences between these 2 groups and are combined into a single experimental group for this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Griffiths‐London.
| Methods | Allocation: 'randomised' ‐ no further details. Follow up: 18 months (mean). Loss to follow up: 0%. Objectivity of rating of outcome: unclear if raters independent. | |
| Participants | Inclusion criteria: i. psychotic illness; ii. in contact with psychiatric services during 12 month period beginning 1968; iii. age range 18‐55 years. Diagnosis: all had a psychotic illness, specific diagnoses U/K. N=28. Age: U/K. Sex: U/K. History: U/K. Setting: urban, London, UK. | |
| Interventions | 1. Rehabilitation program: i. co‐ordinated program involving day hospital and industrial workshops; ii. patients treated by team (psychiatrists, nurses, OTs, psychologists); iii. comprehensive assessment used to plan individual treatment and rehabilitation programs. N=14. 2. Control: i. referred back to doctors; ii. mainly in day centres, at home or in hosptial. N=14. | |
| Outcomes | In competitive employment.
Self esteem: Wing scale. Unable to use ‐ Cognitive functioning: WAIS. Attitude: Attitude Rating Scale (unpublished). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Kline‐Philadelphia.
| Methods | Allocation: "randomly assigned" ‐ no further details. Follow up: 6 months. Lost to follow up: 0%. Objectivity of rating of outcome: unclear if raters were independent. | |
| Participants | Inclusion criteria: i. midway through a 1 year rehabilitation program; ii. psychiatrically disabled (not defined). Diagnosis: schizophrenia, schizophrenia‐like disorders (40%). N=20. Age: mean ˜28 years. Sex: "predominantly male". Race: not reported. History: ever married U/K, ever employed 100%, time since last employment U/K, previous admissions U/K. Setting: psychosocial rehabilitation agency, Philadelphia, USA. | |
| Interventions | 1. Employment group: i. met in group to discuss work values (1.5 hours/week for 12 weeks); ii. VR counsellors were group facilitators; iii. aimed to reduce placement anxiety. N=10. 2. Control: usual VR services. N=10. Both groups received usual services from the VR program including entering a job search workshop. | |
| Outcomes | Obtaining competitive employment. Not participating in program. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Kuldau‐California.
| Methods | Allocation: by sealed envelope method. Follow up: 18 months. Lost to follow‐up: 5%. Objectivity of rating of outcome: unclear if raters were independent. | |
| Participants | Inclusion criteria: i. new admission to VA hospital; ii. residing locally. Diagnosis: schizophrenia, schizophrenia‐like disorders (>27%). N=94. Age: mean ˜41 years. Sex: all men. Race: not reported. History: ever married 74%, ever employed U/K but 12% unemployed for 5 years, time since last employment U/K, previous admissions, mean ˜3. Setting: California, USA. | |
| Interventions | 1. Treatment program: combination of i. inpatient care (in therapeutic community milieu); ii. transitional day hospital care; iii. community housing; iv. supported/sheltered work. An employment co‐ordinator (ex‐patient) i. scanned community for job possibilities; ii. worked with patients to help find employment; iii. placed people in jobs. Patients i. worked through the 'progress and planning group' until a "work‐readiness" committee declared them fit for work; ii. could independently seek work own or through this service. Staff liaision with employers about on‐the‐job problems. N=44. 2. Control: i. 'rapid' discharge with emphasis on discharge planning; ii. no housing or community employment service but emphasised work activities such as unpaid industrial therapy assignments in hospital. N=50. | |
| Outcomes | Monthly earnings. Unable to use ‐ Ever employed during study (not a primary or secondary outcome variable. Time in competitive employment (data unclear). Living in community at end of study (not a primary or secondary outcome variable). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
McFarlane‐New York.
| Methods | Allocation: 'randomly assigned' ‐ no further details. Follow up: 3 monthly for 18 months, partial follow up at 24 + 30 months. Lost to follow‐up: 16% at 18 months. Objectivity of rating of outcome: raters independent. | |
| Participants | Inclusion criteria: i. age 18‐55; ii. family available; iii. interested in obtaining a job; iv. in treatment at site clinics; v. schizophrenia, schizoaffective disorder, bipolar disorder or major depression. Diagnosis: schizophrenia, schizophrenia‐like disorders (65%). N=69. Age: mean ˜33 years. Sex: 30% women. Race: 7% non‐white. History: ever married 26%, ever employed U/K, time since last employment, mean ˜15 months, previous admissions, mean ˜5. Setting: 2 CMHCs, 1 urban, 1 rural, New York State, USA. | |
| Interventions | 1. Family‐aided Assertive Community Treatment: i. ACT; ii. family intervention; iii. vocational specialists: specialists' tasks a. developing contacts with employers; b. case‐specific job development; c. job assessment; d. assessment of patients' cognitive, physical and social capacities; e. setting career goals; f. interview and resume practice and assistance; g. on or near job support; h. intervening with employers; i. close co‐ordination with clinicians. N=37. 2. Control: conventional vocational rehabilitation with referral to state VR service often leading to placement in sheltered workshop. N=32. | |
| Outcomes | Obtaining competitive employment.
Obtaining any form of employment.
Not participating in program
Monthly earnings. Unable to use ‐ Obtaining competitive employment at 30 months (follow up <50%) Admissions to hospital per patient (not a secondary outcome). Mental state (not reported by group). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Okpaku‐Nashville.
| Methods | Allocation: 'randomly assigned' ‐ no further details. Follow up: 7 to 28 months.* Lost to follow‐up: 0% ‐ difficult to verify. Objectivity of rating of outcome: raters independent. | |
| Participants | Inclusion criteria: i. serious mental illness as judged by eligibility for disability benefits; ii. client of CMHC. Diagnosis: schizophrenia, schizophrenia‐like disorders (67%). N=152. Age: mean ˜37 years. Sex: 41% women. Race: 40% non‐white. History: ever married 52%, ever employed U/K, time since last employment U/K, previous admissions ˜3. Setting: urban, Tenessee, USA. | |
| Interventions | 1. Employment oriented case management:** i. multi‐disciplinary team of rehabilitation specialists (case load/specialist ˜10); ii. employment needs assessment; iii. regular review; iv. "aggressively pursued social and rehabilitative services". N=73. 2. Control: standard case management services from CMHC (case load 40‐90). N=79. | |
| Outcomes | Finding any employment
Not participating in program. Unable to use ‐ Cost data (insufficient data). |
|
| Notes | * Variable follow up period ‐ all received 4 month intervention and one 3 month follow up interview, some followed up as long as 24 months. ** Not an assertive community treatment model ‐ not explicit what the intervention was, but not supported employment. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Walker‐Massachusetts.
| Methods | Allocation: by table of random numbers. Follow up: 6 months. Lost to follow‐up: 0%. Objectivity of rating of outcome: raters not independent. | |
| Participants | Inclusion criteria: i. hospital in‐patient + 2 successful weeks in hospital work program; ii. recommended as capable of work by rehabilitation therapist; iii. willing to work; iv. cleared as suitable by psychiatrist. Diagnosis: schizophrenia, schizophrenia‐like disorders (50%). N=28. Age: U/K. Sex: all men. Race: U/K. History: ever married U/K, ever employed U/K, time since last employment U/K, previous admissions U/K. Setting: urban, Massachusetts, USA. | |
| Interventions | 1. Community‐based Hospital Industrial Rehabilitation Placement (CHIRP): i. placements in a regular industrial setting off grounds (˜a form of paid sheltered workshop); ii. supervision by member of rehabilitation staff from hospital; iii. transport; iv. could continue to attend after leaving hospital; v. standard hospital and community care. N=14. 2. Control: standard hospital and community care, could not attend CHIRP. N=14. | |
| Outcomes | Time in competitive employment (excluding CHIRP)
Not participating in program. Unable to use ‐ Obtaining competitive employment (data unclear). Earnings: median monthly (no mean, SD). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Wolkon‐Cleveland.
| Methods | Allocation: 'random assignment' ‐ no further details except randomisation took place before consent was obtained (207 of 333 patients assigned to control group refused to participate). Follow up: 12, 18, 24, 30 months. Lost to follow‐up: 8%. Objectivity of rating of outcome: raters independent. | |
| Participants | Inclusion criteria: i. age 20‐60; ii. >1 month psychiatric hospitalisation + about to be discharged; iii. no primary diagnosis of substance abuse, mental retardation or organic brain disease.* Diagnosis: schizophrenia/schizophrenia‐like disorders (78%). N=540. Age: mean ˜36 years. Sex: 65% women. Race: 43% non‐white. History: Ever married U/K, ever employed U/K, time since last employment U/K, previous admissions >2. Setting: urban, non‐residental, transitional, social rehabilitation centre for adults recently released from psychiatric hospital, Ohio, USA. | |
| Interventions | 1. Rehabilitative treatment: i. social group work; ii. individual counselling; iii. transitional work projects; iv. informed that participation was limited to 1 year (not clear if strictly enforced). N=333. 2. Control: standard aftercare services (not specified). N=207. | |
| Outcomes | Rehospitalised. Unable to use ‐ In competitive employment (no data reported). Psychiatric symptoms (unpublished scale). |
|
| Notes | * A random sample of all patients about to be discharged from 3 state psychiatric hospitals over a 2.5 year period. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
BPRS ‐ Brief Psychiatric Rating Scale. PANSS ‐ Positive and Negative Symptom Scale. ACT ‐ Assertive Community Tretment. CMHC ‐ Community Mental Health Centre SCID U/K ‐ unknown. P/t ‐ part time. F/t ‐ full time. VR ‐ vocational rehabilitation. DSM‐III‐R ‐ Diagnostic Statistical Manual, version 3, revised.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adams‐Shollenberger | Allocation: not randomised, a survey comparing absenteeism rates. |
| Ax‐Salem | Allocation: randomised. Participants: diagnosis unclear, at least one third had alcohol problems only, hence excluded. Intervention: PVT (job club) versus no intervention. |
| Azrin‐Illinois | Allocation: randomised (coin flip). Participants: diagnosis unclear, not all severely mentally ill, many had physical handicaps alone, hence excluded. Intervention: PVT (job club) versus advice on finding work. |
| Bailey‐New Hampshire | Allocation: not randomised, before and after study. |
| Becker‐Boston | Allocation: not randomised, retrospective case series. |
| Bell‐Connecticut2 | Allocation: not randomised (quasi‐experimental study comparing a hospital‐based VR program with two other inpatient treatment units). |
| Block‐Canada | Allocation: not randomised, before and after study. |
| Bond‐Chicago2 | Allocation: randomised. Participants: people with severe mental disorder Interventions: Assertive Community Treatment versus standard care. This trial of Assertive Community Treatment versus standard care happened to report vocational outcomes, but did not involve and any specific vocational rehabilitation intervention ‐ hence excluded. |
| Briggs‐Minnesota | Allocaton: randomised. Participants: people with severe mental disorder Interventions: PVT (vocational counselling) versus standard community care. Outcomes: Excluded as not possible to do an intention‐to‐treat analysis. The number randomised appears to be fewer than the numbers followed up. Two different conflicting figures are given for the number of people recruited ‐ excluded pending clarification. (Even if included, the study does not report any data that could be used in the review). |
| Campbell‐Massachus | Allocation: not randomised ‐ quasi‐experimental design. Participants: people with severe mental disorder Interventions: PVT (sheltered workshop) versus PVT (an "industry‐integrated model"). |
| Chandler‐Stanislaus | (This trial is described in the same paper as the included trial Chandler‐Long Beach.) Allocation: randomised. Participants: people with severe mental disorder Interventions: Assertive Community Treatment versus standard community care. This trial of Assertive Community Treatment versus standard care happened to report vocational outcomes, but did not involve and any specific vocational rehabilitation intervention ‐ hence excluded. |
| Drake‐New Hampshire2 | Allocaton: not randomised, quasi‐experimental design. Participants: people with severe mental disorder attending a two rehabilitative day centres. Intervention: SE (one day centre closed and converted to SE program) versus rehabilitative day centre. |
| Fabian‐Maryland | Allocation: not randomised, a survey comparing employed and unemployed participants. |
| Faulkner‐Virginia | Allocation: not randomised, before and after design. |
| Huxley‐Colorado | Allocation: not randomised, a survey comparing patients attending a Clubhouse program with controls from a neighbouring area. |
| Jennings‐Virginia | Allocation: randomised. Participants: diagnosis unclear, hence excluded. Interventions: PVT enhanced by a psychological group treatment for enhancing participation versus unenhanced PVT. |
| Kaufman‐Pittsburgh | Allocaton: randomised. Participants: people with severe mental disorders referred to a self‐help employment centre. Interventions: PVT approach (self‐help employment centre) versus standard care ‐ control condition unclear ‐ all controls were referred to other VR services, but it is unclear how many (if any) actually engaged. Outcomes: no usable data ‐ numbers randomised to treatment and control groups were not specified, hence it was not possible to report the number in employment on an intention to treat basis. |
| Keith‐Michigan | Allocation: randomised. Participants: not all participants were mentally ill, hence excluded. Interventions: psychological approach for enhancing the effectiveness of vocational rehabilitation versus standard vocational rehabilitation counselling provided by the same agency. |
| Kregel‐Virginia | Allocation: not randomised, a large survey of participants in Supported Employment services. |
| Luo‐Nanjing | Allocation: not randomised, retrospective cohort study. |
| McAlpine‐San Francis | Allocation: not randomised, quasi‐experimental study comparing vocational outcome in patients receiving assertive community treatment with those receiving standard community care. |
| Noble‐New York | Allocation: not randomised, compared clients in a Clubhouse program to those in newly developed Supported Employment Program. |
| Olah‐Ohio | Allocation: not randomised, matched group design, examining effectiveness of a group intervention to increase self efficacy in people with mental disorder versus no intervention. |
| Otero‐Spain | Allocation: not randomised, before and after study of a rehabilitation program for people with chronic schizophrenia. |
| Proudfoot‐London | Allocation: randomised. Participants: not mentally ill, hence excluded. Interventions: occupational training program (incorporating cognitive behavioural therapy) versus a program that emphasised social support. |
| Purvis‐Denver | Allocation: randomised. Participants: discharged psychiatric patients. Interventions: group "community follow‐up" versus individual "community follow‐up" versus a control group ‐ experimental interventions included "vocational counseling" but did not appear to involve any active vocational rehabilitation in the sense of either prevocational training of supported employment. |
| Ryan‐Connecticut | Allocation: randomised. Participants: patients recently discharged from hospital. Interventions: PVT versus standard community care. Outcomes: not an intention to treat analysis ‐ patients randomly assigned whilst inpatients, but any who were judged not ready for discharge within two months were dropped from study. Similarly, any who failed to complete 3 months in the PVT after allocation were dropped. The trial seems to report data only on people who met these conditions after randomisation. |
| Sauter‐New York | Allocation: randomised. Participants: people with chronic schizophrenia attending a sheltered work shop. Interventions: work skills training for sheltered workshop participants verus sheltered workshop alone. Outcomes: increasing productivity rates, not concerned with employment outcomes ‐ hence excluded. |
| Stein‐Madison | Allocation: randomised. Participants: people with severe mental illness requiring admission to hospital. Interventions: Assertive Community Treatment versus hospital admission. Vocational outcomes were reported but excluded as the intervention did not involve any specific vocational rehabilitation component. |
| Tomaras‐Athens | Allocation: not randomised, before and after study. |
| Velasquez‐Minnesota | Allocation: randomised. Participants: young adults with psychotic, neurotic or personality disorder. Interventions: residential milieu therapy versus standard community care. Vocational outcomes were reported, but the intervention did not involve any specific vocational component. |
PVT ‐ Pre‐vocational Training VR ‐ Vocational Rehabilitation
Characteristics of ongoing studies [ordered by study ID]
Bond‐Chicago3.
| Trial name or title | Thresholds DPA/IPS Study |
| Methods | |
| Participants | N=180. History: new admissions to Thresholds organisation in Chicago. Inclusion criteria: i. suffering from severe mental illness; ii. 18 or over; iii. interested in competitive employment; iv. unemployed for previous month; and v. willing to attend 2 informational group sessions to understand project's requirements. |
| Interventions | 1. IPS model. 2. Diversified Placement Approach (DPA ‐ a prevocational approach developed at Thresholds). |
| Outcomes | Employment outcomes. Substance abuse. Costs of care. Compliance. |
| Starting date | Started 09/99 |
| Contact information | Gary Bond gbond@iupui.edu |
| Notes |
Carey‐US 8 site.
| Trial name or title | No details available. |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes |
Contributions of authors
Ruth Crowther ‐ designed the protocol, co‐ordinated the reviewing, developed and ran the search strategy, screened the results, organised the retrieval of papers, appraised papers and extracted data. She entered, analysed and interpreted the data and participated in writing the review.
Max Marshall ‐ conceived the review and obtained funding. He designed the protocol, developed the search strategy, screened search results, appraised papers, extracted, analysed and interpreted data and participated in writing the review.
Peter Huxley ‐ conceived the review and obtained funding. He helped interpret data and provided a methodological, policy and clinical perspective on the data and participated in writing the review.
Gary Bond ‐ assisted in developing the search strategy, provided additional information about papers and helped in obtaining data on unpublished studies. He helped analyse and interpret data and was involved in writing the review. Gary Bond has performed previous reviews in the field that were the foundation of the current study.
Sources of support
Internal sources
Guild Community Healthcare Trust, UK.
External sources
NHS Health Technology Assessment ‐ grant no. 96/41/3, UK.
NHS Executive North West (research fellowship for Ms. Crowther), UK.
Declarations of interest
Ruth Crowther, Max Marshall and Peter Huxley have no conflict of interest. Gary Bond has collaborated with Robert Drake and Debbie Becker (developers of the Individual Placement and Support Model), and their colleagues at Dartmouth on a series of studies and papers related to this model. He is co‐author on one IPS trial (Drake‐Washington) and is currently funded to complete a 5‐year randomised controlled trial comparing IPS to a Pre‐vocational Training model. Bond is also the primary author on two other trials reviewed in this group: Bond‐Chicago1 and Bond‐Indiana.
Edited (no change to conclusions)
References
References to studies included in this review
Beard‐NewYork {published data only}
- Beard JH, Malamud TJ, Rossman E. Psychiatric rehabilitation and long‐term rehospitalisation rates: the findings of two research studies. Schizophrenia Bulletin 1978;4:622‐35. [DOI] [PubMed] [Google Scholar]
- Beard JH, Pitt MA, Fisher SH, Goertzel V. Evaluating the effectiveness of a psychiatric rehabilitation program. American Journal of Orthopsychiatry 1963;33:701‐12. [DOI] [PubMed] [Google Scholar]
Becker‐Fort Worth {published data only}
- Becker RE. An evaluation of a rehabilitation program for chronically hospitalised psychiatric patients. Social Psychiatry 1967;2:32‐8. [Google Scholar]
Bell‐Connecticut {published data only}
- Bell MD, Lysaker PH, Milstein RM. Clinical benefits of paid work activity in schizophrenia. Schizophrenia Bulletin 1996;22:51‐67. [DOI] [PubMed] [Google Scholar]
- Bell MD, Milstein RM, Lysaker PH. Pay and participation in work activity: clinical benefits for clients with schizophrenia. Psychosocial Rehabilitation Journal 1993;17:173‐6. [Google Scholar]
- Bell MD, Milstein RM, Lysaker PH. Pay as an incentive in work participation by patients with severe mental illness. Hospital and Community Psychiatry 1993;44:684‐6. [DOI] [PubMed] [Google Scholar]
Blankertz‐Philadelph {published data only}
- Blankertz L, Robinson S. Adding a vocational focus to mental health rehabilitation. Psychiatric Services 1996;47:1216‐22. [DOI] [PubMed] [Google Scholar]
Bond‐Chicago1 {published data only}
- Bond GR, Dincin J. Accelerating entry into transitional employment in a psychosocial rehabilitation agency. Rehabilitation Psychology 1986;31:143‐55. [Google Scholar]
Bond‐Indiana {published data only}
- Bond GR, Dietzen LL, McGrew JH, Miller LD. Accelerating entry into supported employment for persons with severe psychiatric disabilities. Rehabilitation Psychiatry 1995;40:75‐94. [Google Scholar]
- Bond GR, Dietzen LL, Vogler K, Katuin CH, McGrew JH, Miller D. Toward a framework for evaluating cost and benefits of psychiatric rehabilitation: three case examples. Journal of Vocational Rehabilitation 1995;5:75‐88. [Google Scholar]
Chandler‐LongBeach {published data only}
- Chandler D, Hu T, Meisel J, McGowen M, Madison K. Mental health costs, other public costs, and family burden among mental health clients in capitated integrated service agencies. Journal of Mental Health Administration 1997;24:178‐88. [DOI] [PubMed] [Google Scholar]
- Chandler D, Meisel J, Hu T, McGowen M, Madison K. A capitated model for a cross section of severely mentally ill clients: employment outcomes. Community Mental Health Journal 1997;33:501‐16. [DOI] [PubMed] [Google Scholar]
- Chandler D, Meisel J, Hu T, McGowen M, Madison K. Client outcomes in a three‐year controlled study of an integrated service agency model. Psychiatric Services 1996;47:1337‐43. [DOI] [PubMed] [Google Scholar]
- Chandler D, Meisel J, McGowen M, Mintz J, Madison K. Client outcomes in two model capitated integrated service agencies. Psychiatric Services 1996;47:175‐80. [DOI] [PubMed] [Google Scholar]
Dincin‐Chicago {published data only}
- Bond GR. An economic analysis of psychosocial rehabilitation. Hospital and Community Psychiatry 1984;35:356‐62. [DOI] [PubMed] [Google Scholar]
- Dincin J, Witheridge TF. Psychiatric rehabilitation as a deterrent to recidivism. Hospital and Community Psychiatry 1982;33:645‐50. [DOI] [PubMed] [Google Scholar]
Drake‐New Hampshire1 {published data only}
- Clark RE. Supported employment and managed care: can they coexist?. Psychiatric Rehabilitation Journal 1998;22(1):62‐8. [Google Scholar]
- Clark RE, Xie H, Becker DR, Drake RE. Benefits and costs of supported employment from three perspectives. Journal of Behavioural Health Services and Research 1998;25(1):22‐34. [DOI] [PubMed] [Google Scholar]
- Drake RE, Becker DR, Anthony WA. A research induction group for clients entering a mental health research project. Hospital and Community Psychiatry 1994;45:487‐9. [DOI] [PubMed] [Google Scholar]
- Drake RE, McHugo GJ, Becker DR, Anthony WA, Clark RE. The New Hampshire Study of supported employment for people with severe mental illness. Journal of Consulting and Clinical Psychology 1996;64:391‐9. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Becker DR, Torrey WC, Xie H, Bond GR, Drake RE, Dain BJ. Work and non‐vocational domains of functioning in persons with severe mental illness: a longitudinal analysis. Journal of Nervous and Mental Disease 1997;185:419‐26. [DOI] [PubMed] [Google Scholar]
Drake‐Washington {published data only}
- Drake RE, McHugo GJ, Bebout RR, Becker DR, Harris M, Bond GR, Quimby E. A randomized controlled trial of supported employment for inner‐city patients with severe mental illness. Archives of General Psychiatry 1999;56:627‐33. [DOI] [PubMed] [Google Scholar]
Gervey‐New York {published data only}
- Gervey R, Bedell JR. Psychological assesment and treatment of persons with severe mental disorders. In: Bedell JR editor(s). Supported employment in vocational rehabilitation. Washington DC: Taylor & Francis, 1994:170‐5. [Google Scholar]
Griffiths‐London {published data only}
- Griffiths RD. Rehabilitation of chronic psychotic patients. Psychological Medicine 1974;4:316‐25. [PubMed] [Google Scholar]
Kline‐Philadelphia {published data only}
- Kline MN, Hoisington V. Placing the psychiatrically disabled: a look at work values. Rehabilitation Counseling Bulletin 1981:366‐9. [Google Scholar]
Kuldau‐California {published data only}
- Kuldau JM, Dirks SJ. Controlled evaluation of a hospital originated community transitional system. Archives of General Psychiatry 1977;34:1331‐40. [DOI] [PubMed] [Google Scholar]
McFarlane‐New York {unpublished data only}
- McFarlane WR, Dushay RA, Deakins SM, Stasny P, Lukens EP, Toran J, Link B. Employment outcomes in family‐aided assertive community treatment. Journal of Orthopsychiatry 2000;70(2):203‐14. [DOI] [PubMed] [Google Scholar]
- McFarlane, W. R, Stastny, P, Deakins, S. Dushay, R. Employment outcomes in family‐aided assertive community treatment (FACT). Presented at the Institute on Psychiatric Services, Boston 1995.
Okpaku‐Nashville {published data only}
- Okpaku SO, Anderson KH, Sibulkin AE, Butler JS, Bickman L. The effectiveness of a multidisciplinary case management intervention on the employment of SSDI applicants and beneficiaries. Psychiatric Rehabilitation Journal 1997;20:34‐41. [Google Scholar]
Walker‐Massachusetts {published data only}
- Walker R, Winick W, Frost ES, Lieberman JM. Social restoration of hospitalised psychiatric patients through a program of special employment in industry. Rehabilitation Literature 1969;30:297‐303. [PubMed] [Google Scholar]
Wolkon‐Cleveland {published data only}
- Wolkon GH, Karmen M, Tanaka HT. Evaluation of a social rehabilitation program for recently released psychiatric patients. Community Mental Health Journal 1971;7:312‐22. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Adams‐Shollenberger {published data only}
- Adams‐Shollenberger GE, Mitchell TE. [A comparison of janitorial workers with mental retardation and their non‐disabled peers on retention and absenteeism]. Journal of Rehabilitation 1996;62:56‐60. [Google Scholar]
Ax‐Salem {unpublished data only}
- Ax RK. A comparison of the efficacy of a group versus individualised "job club" job search training format (Doctoral thesis). Blacksburg: Virginia Polytechnic Institute and State University, 1983. [Google Scholar]
Azrin‐Illinois {published data only}
- Azrin NH, Philip RA. The job club method for the job handicapped: a comparative outcome study. Rehabilitation Counseling Bulletin 1980;23:144‐55. [Google Scholar]
Bailey‐New Hampshire {published data only}
- Bailey E, Ricketts S, Becker DR, Xie H, Drake RE. Conversion of day treatment to supported employment: one‐year outcomes. Psychiatric Rehabilitation Journal 1998;22(1):24‐9. [Google Scholar]
Becker‐Boston {published data only}
- Becker RE, Meisler N, Stormer G, Brondino MJ. Employment outcomes for clients with severe mental illness in a PACT model replication. Psychiatric Services 1999;50:104‐6. [DOI] [PubMed] [Google Scholar]
Bell‐Connecticut2 {published data only}
- Bell MD, Ryan ER. Integrating psychosocial rehabilitation into the hospital psychiatric service. Hospital and Community Psychiatry 1984;35:1017‐23. [DOI] [PubMed] [Google Scholar]
Block‐Canada {published data only}
- Block L. The employment connection: the application of an individual supported employment program for persons with chronic mental health problems. Canadian Journal of Community Mental Health 1992;11:79‐89. [DOI] [PubMed] [Google Scholar]
Bond‐Chicago2 {published data only}
- Bond GR, Witheridge TF, Dincin J, Wasmer D, Webb J, Graaf‐Kaser R. Assertive community treatment for frequent users of psychiatric hospitals in a large city: a controlled study. American Journal of Community Psychology 1990;18:865‐91. [DOI] [PubMed] [Google Scholar]
Briggs‐Minnesota {published data only}
- Briggs PF, Yater AC. Counseling and psychometric signs as determinants in the vocational success of discharged psychiatric patients. Journal of Clinical Psychology 1966;22:100‐4. [DOI] [PubMed] [Google Scholar]
Campbell‐Massachus {unpublished data only}
- Campbell JF. An industrially integrated model versus the sheltered workshop in the vocational rehabilitation of mentally‐disabled persons (Doctoral dissertation). Amherst: University of Massachusetts, 1984. [Google Scholar]
Chandler‐Stanislaus {published data only}
- Chandler D, Meisel J, Hu T, McGowen M, Madison, K. Client outcomes in a three‐year controlled study of an integrated service agency model. Psychiatric Services 1996;47:1337‐43. [DOI] [PubMed] [Google Scholar]
Drake‐New Hampshire2 {published data only}
- Clark RE, Bush PW, Becker DR, Drake RE. A cost‐effectiveness comparison of supported employment and rehabilitative day treatment. Administration and Policy in Mental Health 1996;24:63‐77. [Google Scholar]
- Drake RE, Becker DR, Biesanz JC, Torrey WC, McHugo GJ, Wyzik PF. Rehabilitative day treatment vs. supported employment. I. Vocational outcomes. Community Mental Health Journal 1994;30:519‐32. [DOI] [PubMed] [Google Scholar]
- Torrey WC, Becker DR, Drake RE. Rehabilitative day treatment vs. supported employment. II. Consumer, family and staff reactions to a program change. Psychosocial Rehabilitation Journal 1995;18:67‐75. [Google Scholar]
Fabian‐Maryland {published data only}
- Fabian ES. Supported employment and the quality of life: does a job make a difference?. Rehabilitation Counseling Bulletin 1992;36:84‐97. [Google Scholar]
Faulkner‐Virginia {published data only}
- Faulkner LR, McFarland BH, Larch BB, Wanda JH, Yohe CD. Small group therapy for the chronic mentally ill. Hospital and Community Psychiatry 1986;37:273‐9. [DOI] [PubMed] [Google Scholar]
Huxley‐Colorado {unpublished data only}
Jennings‐Virginia {unpublished data only}
- Jennings JA. The effects of prevocational training on the vocational maturity of outpatients in a community mental health clinic (Doctoral thesis). Charlottesville: University of Virginia, 1981. [Google Scholar]
Kaufman‐Pittsburgh {published data only}
- Kaufman CL. The Self‐Help Employment Center: some outcomes from the first year. Psychosocial Rehabilitation Journal 1995;18:145‐62. [Google Scholar]
Keith‐Michigan {published data only}
- Keith RD, Engelkes JR, Winborn BB. Employment‐seeking preparation and activity: an experimental job‐placement training model for rehabilitation clients. Rehabilitation Counseling Bulletin 1977;21:159‐65. [Google Scholar]
Kregel‐Virginia {published data only}
- Kregel J, Wehman P, Banks RD. The effects of consumer characteristics and types of employment models on individual outcomes in supported employment. Journal of Applied Behaviour Analysis 1989;22(4):407‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Luo‐Nanjing {published data only}
- Luo K, Yu D. Enterprise‐based sheltered workshops in Nanjiing: a new model for the community rehabilitation of mentally ill workers. British Journal of Psychiatry 1994;165:89‐95. [PubMed] [Google Scholar]
McAlpine‐San Francis {unpublished data only}
- McAlpine JK. The effectiveness of the community based outreach model on the community adjustment of the chronically mentally ill (Doctoral thesis). San Francisco, CA: Saybrook Institute, 1991. [Google Scholar]
Noble‐New York {published data only}
- Noble JH. The benefits and costs of supported employment for people with mental illness and with traumatic brain injury in New York. Albany, NY: The Research Foundation of State University of New York, 1991. [Google Scholar]
Olah‐Ohio {unpublished data only}
- Olah RJ. Facilitating the development of self‐efficacy in severely mentally disabled adults: application of a group intervention in a supported employment program (Doctoral thesis). Kent, OH: Kent State University, 1989. [Google Scholar]
Otero‐Spain {published data only}
- Otero V, Rebolledo S. [Evaluation de un programa de rehabilitacion psiquiatrica]. Psiquis 1993;14:273‐80. [Google Scholar]
Proudfoot‐London {published data only}
- Proudfoot J, Guest J, Dunn G, Gray J. Effect of cognitive‐behavioural training on job‐finding among long‐term unemployed people. Lancet 1997;350:96‐100. [DOI] [PubMed] [Google Scholar]
Purvis‐Denver {published data only}
- Purvis SA, Miskimmins RW. Effects of community follow‐up on post‐hospital adjustment of psychiatric patients. Community Mental Health Journal 1970;6:374‐82. [DOI] [PubMed] [Google Scholar]
Ryan‐Connecticut {published data only}
- Ryan ER, Bell MD. Rehabilitation of chronic psychiatric patients: a randomised clinical study. American Psychological Association Convention papers. Los Angeles, 1985.
Sauter‐New York {published data only}
- Sauter AW, Nevid S. Work skills training with chronic schizophrenic sheltered workers. Rehabilitation Psychology 1991;36:255‐64. [Google Scholar]
Stein‐Madison {published data only}
- Stein LI, Test MA. Alternative to mental hospital treatment. I. Conceptual model, treatment program, and clinical evaluation. Archives of General Psychiatry 1980;37:392‐7. [DOI] [PubMed] [Google Scholar]
Tomaras‐Athens {published data only}
- Tomaras V, Vlachonikolis IG, Stefanis CN, Madianos M. The effects of individual psychosocial treatment on the family atmosphere of schizophrenic patients. Social Psychiatry and Psychiatric Epidemiology 1988;23:256‐61. [DOI] [PubMed] [Google Scholar]
Velasquez‐Minnesota {published data only}
- Velasquez JS, McCubbin HI. Towards establishing the effectiveness of community‐based residential treatment: program evaluation by experimental research. Journal of Social Service Research 1980;3:337‐59. [Google Scholar]
References to studies awaiting assessment
Brinkman‐Amsterdam {published data only}
- Brinkman N, Mastboom JCM. Evaluatie van eeen clubhuis voor mensen met languirige psychiatrische problemen. Utrecht: Fountain House De Waterheuvel. NcGv‐reeksnr. 89‐10, 1989. [Google Scholar]
Fairweather‐unknown {published data only}
- Fairweather GW, Samders DH, Maynard H, Cressler DL, Bleck DS. Community life for the mentally ill. Chicago: Aldine, 1969. [Google Scholar]
Field‐Madison {published data only}
- Field G, Allness D, Knoedler W, Test MA. Employment training for chronic patients in the community. Mendota Mental Health Institute, Madison, Wis. 53704. Madison, Wis.
Weinberg‐unknown {published data only}
- Weinberg JL. Lustig P. A workshop experience for post‐hospitalised schizophrenics. In: Wright GN, Trotter AB editor(s). Rehabilitation Research. Madison: University of Wisconsin, 1968:72‐8. [Google Scholar]
References to ongoing studies
Bond‐Chicago3 {unpublished data only}
- Bond GR, Drake R, Becker D, Dincin J, Evans J, Lysaker P, McCoy T, Clark R. [Comparison of two employment models for clients with severe mental illness ‐ the Thresholds DPA/IPS Study]. 2000 (personal communication).
Carey‐US 8 site {published data only}
- Carey MA. The continuing need for research on vocational rehabilitation programs. Psychosocial Rehabilitation Journal 1995;18(4):163‐4. [Google Scholar]
Additional references
Altman 1996
- Altman DG, Bland JM. Detecting skewness from summary information. BMJ 1996;313:1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
Anthony 1987
- Anthony WA, Blanch A. Supported employment for persons who are psychiatrically disabled: an historical and conceptual perspective. Psychosocial Rehabilitation Journal 1987;11:5‐23. [Google Scholar]
Beard 1982
- Beard JH, Propst RN, Malamud TJ. The Fountain House model of rehabilitation. Psychosocial Rehabilitation Journal 1987;5:47‐53. [Google Scholar]
Becker 1994
- Becker DR, Drake RE. Individual Placement & Support: a community mental health center approach to vocational rehabilitation. Community Mental Health Journal 1994;30(2):193‐206. [DOI] [PubMed] [Google Scholar]
Bilby 1992
- Bilby R. A response to the criticisms of transitional employment. Psychosocial Rehabilitation Journal 1992;18:69‐82. [Google Scholar]
Bond 1984
- Bond GR, Dincin J, Setze PJ, Witheridge TF. The effectiveness of psychiatric rehabilitation: a summary of research at Thresholds. Psychosocial Rehabilitation Journal 1984;7:6‐22. [Google Scholar]
Bond 1988
- Bond GR, Boyer SB. Rehabilitation programs and outcomes. In: Ciardiello JA editor(s). Vocational rehabilitation of persons with prolonged mental illness. Baltimore, MD: Johns Hopkins University Press, 1988:231‐63. [Google Scholar]
Bond 1992
- Bond GR. Vocational rehabilitation. In: Liberman RP editor(s). Handbook of psychiatric rehabilitation. New York: Macmillan, 1992:244‐75. [Google Scholar]
Bond 1997a
- Bond GR, Drake RE, Mueser KT, Becker DR. An update on supported employment for people with severe mental illness. Psychiatric Services 1997;48(3):335‐46. [DOI] [PubMed] [Google Scholar]
Bond 1997b
- Bond GR, Becker DR, Drake RE, Vogler KM. A fidelity scale for the Individual Placement and Support model of supported employment. Rehabilitation Counseling Bulletin 1997;40:265‐84. [Google Scholar]
Bond 1998a
- Bond GR, Drake RE, Becker DR, Mueser KT. Effectiveness of psychiatric rehabilitation approaches for employment of people with severe mental illness. Journal of Disability Policy Studies 1998;in press. [Google Scholar]
Bond 1998b
- Bond GR. Principles of the Individual Placement and Support model: empirical support. Psychiatric Rehabilitation Journal 1998;22(1):11‐23. [Google Scholar]
Clark 1996
- Clark RE, Bush PW, Becker DR, Drake RE. A cost‐effectiveness comparison of supported employment and rehabilitative day treatment. Administration and Policy in Mental Health 1996;24:63‐77. [Google Scholar]
Clarke 1999
- Clarke M, Oxman AD. Cochrane Reviewers’ Handbook. 1999, Issue 4.0.
Connors 1987
- Connors KA, Graham RS, Pulso R. Playing the store: where is the vocational in psychiatric rehabilitation?. Psychosocial Rehabilitation Journal 1987;10(3):21‐33. [Google Scholar]
DoH 1998
- DoH. Modernising Mental Health Services. London: Department of Health, 1998. [Google Scholar]
Endicott 1976
- Endicott J, Spitzer RL, Fleiss JL, Cohen J. The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Archives of General Psychiatry 1976;33:766‐71. [DOI] [PubMed] [Google Scholar]
ERMIS 1998 [Computer program]
- Ermis European Economic Interest Grouping. ERMIS, 1998.
Gervey 1994
- Gervey R, Bedell JR. Supported employment in vocational rehabilitation. In: Bedell JR editor(s). Psychological assesment and treatment of persons with severe mental disorders. Washington DC: Taylor & Francis, 1994. [Google Scholar]
Hatfield 1992
- Hatfield B, Huxley P, Mohamad H. Accommodation and employment: a survey into the circumstances and expressed needs of users of mental health services in a northern town. British Journal of Social Work 1992;22:60‐73. [Google Scholar]
Jones 1993
- Jones K. Asylums and after, a revised history of the mental health services: from the early 18th century to the 1990s. London: Athlone, 1993. [DOI] [PubMed] [Google Scholar]
Kay 1987
- Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophrenia Bulletin 1987;13:261‐76. [DOI] [PubMed] [Google Scholar]
Kim 1998
- Kim SH. Persons with severe mental illness: a meta‐analysis of vocational programs (Masters thesis). Indianapolis, IN: Indiana University‐Purdue University Indianapolis, 1998. [Google Scholar]
Lehman 1983
- Lehman A. The well being of chronic mental patients: assessing their quality of life. Archives of General Psychiatry 1983;40:369‐73. [DOI] [PubMed] [Google Scholar]
Lehman 1995
- Lehman AF. Vocational rehabilitation in schizophrenia. Schizophrenia Bulletin 1995;21(4):645‐56. [DOI] [PubMed] [Google Scholar]
Lehman 1998
- Lehman AF, Steinwachs DM, PORT Co‐investigators. Patterns of usual care for schizophrenia: initial survey results from the Schizophrenia Patient Outcomes Research Team (PORT) survey. Schizophrenia Bulletin 1998;24:11‐20. [DOI] [PubMed] [Google Scholar]
Lukoff 1986
- Lukoff K, Liberman RP, Neuchterlein KH. Symptom monitoring in the rehabilitation of schizophrenic patients. Schizophrenia Bulletin 1986;12:578‐602. [DOI] [PubMed] [Google Scholar]
Macias 1995
- Macias C, Kinney R, Rodican C. Transitional employment: an evaluative description of Fountain House Practice. Journal of Vocational Rehabilitation 1995;5:151‐8. [Google Scholar]
Marshall 1999a
- Marshall M, Lockwood A. Assertive community treatment for people with severe mental disorders. The Cochrane Library 1999, Issue 2. [DOI] [PubMed] [Google Scholar]
Marshall 1999b
- Marshall M, Gray A, Lockwood A, Green R. Case management for people with severe mental disorders. The Cochrane Library 1999, Issue 2. [DOI] [PubMed] [Google Scholar]
Marshall 2000
- Marshall M, Lockwood L, Bradley C, Adams C, Joy C, Fenton M. Unpublished rating scales ‐ a major source of bias in randomised controlled trials of treatments for schizophrenia?. British Journal of Psychiatry 2000;176:249‐52. [DOI] [PubMed] [Google Scholar]
McCreadie 1992
- McCreadie RG. The Nithsdale schizophrenia surveys. Social Psychiatry and Psychiatric Epidemiology 1992;27:40‐5. [DOI] [PubMed] [Google Scholar]
Meltzer 1995
- Meltzer H, Gill B, Petticrew M, Hinds K. Economic activity and social functioning of adults with psychiatric disorders. Office of Population Censuses & Surveys, Surveys of psychiatric morbidity in Great Britain. Vol. Report 2, London: HMSO, 1995. [Google Scholar]
ONS 1998
- Office of National Statistics. Labour Force Survey (1997/8). London: Office of National Statistics, 1998. [Google Scholar]
Ridgeway 1998
- Ridgeway P, Rapp C. The active ingredients in achieving competitive employment for people with psychiatric disabilities: a research synthesis. Critical Ingredients Series. Lawrence, Kansas: Kansas Department of Social and Rehabilitation Services, Commission on Mental Health and Developmental Disabilities, 1998. [Google Scholar]
Rosenberg 1969
- Rosenberg M. Society and the adolescent self‐image. Princeton, NJ: Princeton University Press, 1969. [Google Scholar]
Schneider 1998
- Schneider J. A rationale for employment of people with mental health problems (Doctoral thesis). Canterbury: University of Kent at Canterbury, 1998. [Google Scholar]
Shepherd 1994
- Shepherd G, Murray A, Muijen M. Relative values: the different views of users, family carers and professionals on services for people with schizophrenia. London: Sainsbury Centre for Mental Health, 1994. [Google Scholar]
Wehman 1997
- Wehman P, Revell WG, Kregel J. Supported Employment: a decade of rapid growth and impact. In: Wehman P, Revell WG, West M editor(s). Supported employment research: expanding competitive employment opportunities for persons with significant disabilities. Richmond, VA: VCU Rehabilitation Research and Training Center on Supported Employment, 1997:1‐18. [Google Scholar]
Wing 1966
- Wing JK. Social and psychological changes in a rehabilitation unit. Social Psychiatry 1966;1:21‐8. [Google Scholar]
References to other published versions of this review
Crowther 2001
- Crowther RE, Marshall M, Bond GR, Huxley P. Helping people with severe mental illness to obtain work: systematic review. BMJ 2001;322:204‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]


