Abstract
Sugimoto, D, Myer, GD, Bush, HM, and Hewett, TE. Effects of compliance on trunk and hip integrative neuromuscular training on hip abductor strength in female athletes. Recent studies demonstrate the link between reduced hip abductor strength and increased risk for knee injury such as patellofemoral pain syndrome in women athletes. Meta-analytic reports indicate that the efficacy of integrative neuromuscular training (INT) is associated with compliance to the prescribed programming. Thus, the purpose was to investigate the compliance effects of a trunk and hip–focused INT exercises on hip abductor strength in young women athletes. In a controlled laboratory study design, 21 high school women volleyball players (mean age = 15.6 ± 1.4 years, weight = 64.0 ± 7.4 kg, height = 171.5 ± 7.0 cm) completed isokinetic hip abductor strength testing in pre- and postintervention, which consisted of 5 phases of supervised progressive trunk and hip–focused INT exercises twice a week for 10 weeks. The compliance effects were analyzed based on the changed hip abductor strength values between pre- and postintervention and 3 different compliance groups using 1-way analysis of variance and Pearson’s correlation coefficients. The participants in the high-compliance group demonstrated significant hip abductor peak torque increases compared with noncompliance group (p = 0.02), but not between moderate-compliance and noncompliance groups (p = 0.27). The moderate correlation coefficient value (r = 0.56) was recorded between the isokinetic hip abductor peak torque changes and the 3 compliance groups. Because of the observed significant effects and moderate linear association, the effectiveness of a trunk and hip–focused INT protocol to improve hip abduction strength seems dependent on compliance. Compliance of trunk and hip–focused INT is an important aspect of increasing hip abductor strength increase in young women athletes.
Keywords: adherence, compliance, exercises, core, women
Introduction
Recent studies demonstrate a mechanistic link between reduced proximal neuromuscular control and increased risk for knee and anterior cruciate ligament (ACL) injuries in the women athletic population. Reduced hip abductor strength has been noted in individuals with patellofemoral pain syndrome (PFPS) compared with non-PFPS individuals (2,4,16). In addition to the weak hip abductor status, a cross-sectional laboratory controlled study found that individuals with PFPS exhibit increased hip adduction angles toward the end of prolonged treadmill running compared with anthro-pometrically matched control individuals (6). Significant associations are found between increased hip adduction angles and elevated knee abduction angles and torques in women, but not in men population (10). The elevated knee abduction loads during a dynamic task is a predictive variable for not only future PFPS development (19) but also a noncontact ACL injury in young women athletes (12).
Because of the influence of the proximal controllers to distal segments particularly in the frontal/coronal plane, recent studies focused on strengthening of hip musculature to improve knee joint mechanics. A randomized clinical-controlled trial implemented 2 different exercise protocols (hip strengthening vs. quadriceps strengthening) to examine the effects of hip strengthening in the women population concluded that the participants in the hip strengthening group had earlier pain relief compared with the participants in the quadriceps group (7). Another study that incorporated a series of proximal stability training aimed to enhance hip and core strength musculature and restore sound movement to a group of womens with PFPS documented a 16.2 N·m less knee abduction moment in running after 8 weeks (8). Along with the alterations in knee kinematics, the study also noted a considerable improvement in patient reported outcome scales including a visual analog scale and a Kujala anterior knee pain scale.
Significant evidence supports rehabilitative and prophylactic benefits of performing hip-strengthening exercises on knee joint and related pathologies (7,8). However, the threshold of training that is necessary to see treatment effects has not yet been determined. One potential measure for the training threshold is the compliance evaluation for a given intervention. Several studies examined the compliance effects of neuromuscular training in women athletes and found significantly different injury rates based on different compliance levels (27,29). One study found that women soccer players who practiced preventive neuromuscular training program with high-compliance level reduced acute soccer injury incidence by 39% compared with those who participated in the same neuromuscular training program with intermediate-compliance group (27). Another study also reported that low-compliance level of neuromuscular training participation resulted in greater number of ACL injuries in women athletes (29). In this study, women athletes who had low compliance to a given preventive neuromuscular training program demonstrated approximately 5 times greater rate of ACL injury compared with those athletes who recorded high compliance of neuromuscular training program (29).
Based on the prior reports, there seems to be an association between the compliance level in neuromuscular training and the athletic injury incidence. However, a missing link with this association is the evidence of biomechanical and neuromuscular alterations. The high compliance to neuromuscular training may alter biomechanical and neuromuscular profiles of athletes, which may be a mechanism that leads to lower rate of injury incidence. Concurrently, if the compliance level is low, biomechanical and neuromuscular alterations may not occur, which may be resulted in higher rate of injury incidence relative to the athletes with high compliance. To our knowledge, although the effectiveness of proximal neuromuscular training was reported (7,8), the compliance effect of proximal neuromuscular training on muscular strength has not been reported. If a direct association between compliance level of proximal neuromuscular training and muscular strength is observed, it may potentially fill a gap to explain the different injury incidence rates based on the biomechanical and neuromuscular profile alteration. Therefore, the aim of this project was to investigate the compliance effect of proximal neuromuscular training, a trunk and hip–focused integrative neuromuscular training (INT), on isokinetic hip abductor strength in young women athletes. It was hypothesized that the women athletes who demonstrated the higher compliance to a trunk and hip–focused INT would show a greater hip abductor strength enhancement.
Methods
Study Design and Experimental Approach to the Problem
Initial study design was a prospective intervention study with a laboratory-controlled measures with pre- and post-testing sessions. To examine the compliance effects of the trunk and hip–focused INT, all participants’ attendance and completion to the trunk and hip–focused INT were recorded throughout the course of the study duration. Based on the attendance and completion, 3 following compliance cohorts were created: noncompliance, moderate-compliance, and high-compliance groups.
Study Participants
A total of 21 adolescent women volleyball players (height = 171.5 ± 7.0 cm, weight = 64.0 ± 7.4 kg, and age = 15.6 ± 1.4 years) were recruited from a local area high school and agreed to participate in this study. Because they were younger than 18 years and considered minors, signed informed consents were obtained from their parents or legal guardians before the beginning of this study. The informed consent forms were reviewed and approved by the institutional review board.
Instrumentations
Hip abductor peak torque was assessed bilaterally using the Biodex 3 isokinetic dynamometer system (Biodex Medical System, Shirley, NY, USA). The participants were positioned to stand erect, facing the dynamometer head. The participants were then secured with a stabilization strap coming from across their waist above the iliac crest. The dynamometer head was aligned in parallel with the coronal plane of the subject’s body with the axis of rotation of the dynamometer aligned with the center of rotation of the hip. The test limb was secured to the dynamometer head with a custom-made hip attachment with the strap extending from the moving arm positioned immediately superior to the knee. The participants were instructed to grasp the top of the dynamometer head for support, minimize movement of the torso, and abduct their leg with maximal effort. The isokinetic speed was set at 120°s−1.
Testing Procedures
The participants visited the research laboratory as a team, and all of them were tested within 2 days during the team’s off-season in April. Before the participants were actually tested, the participants performed 5–10 repetitions with sub-maximal effort for the purpose of warming-up and familiarizing with the test. Then, the participants were asked to perform 5 repetitions with maximum exertion. The sequence of the testing leg was stratified between the participants to control for a learning effect. A peak torque of the 5 maximum isokinetic hip abduction repetitions was extracted for statistical analysis. This procedure was repeatedly performed in posttesting sessions, which was performed at the end of the 10-week intervention in June.
Training Protocol
The participants were assigned to perform the trunk and hip–focused INT program 2 times per week for 10 weeks. In addition to the 10 weeks of the trunk and hip–focused INT program, the participants performed their standard sport-related resistance training protocol once a week. All participants’ compliance was recorded by a researcher over a course of the study. For the compliance measurement, attendance and completion for the trunk and hip focused–INT exercises were documented. When participants could not perform certain exercises because of injuries or time constrains such as leaving for other extra curriculum activities, being picked up by parent(s), or joining the INT session late, the trunk and hip–focused INT session was marked as an incompletion.
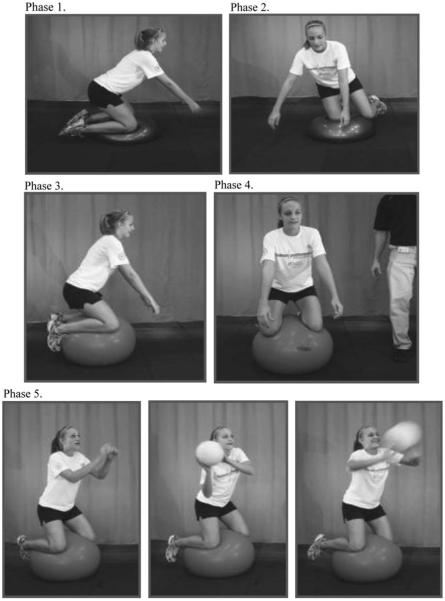
The INT exercises incorporated in this study are described in a previously published study (18). The objective of the INT was to enhance the stability of trunk and hip in their dynamic movements through the progression of each exercise, and the progression was determined based on previous biomechanical studies (20–22). The initial phase of the INT program was adapted from previous studies (13,17,23,26) that demonstrated ACL injury reduction in women subjects. Only exercises that particularly emphasized trunk and hip regions were extracted because the INT was aimed to improve deficits in trunk control and improve hip strength and power in women athletes (Figure 1). Lateral trunk flexion deficits and increased ACL injury risk were reported by several studies in women athletes, but not in men counterparts (14,30). Thus, the INT purposefully incorporated exercises to improve the ability to control the trunk and hip from lateral perturbations at frontal or coronal plane.
Figure 1.
An example of the trunk and hip INT exercises (kneeling trunk stability) and progression (11). Phase 1, Both Side Up (BOSU) ball double-knee hold. Phase 2, BOSU ball single-knee hold. Phase 3, Swiss ball bilateral kneel. Phase 4, Swiss ball bilateral kneel with partner perturbations. Phase 5, Swiss ball bilateral kneel with lateral ball catch. INT, integrative neuromuscular training.
Statistical Analyses
Descriptive statistics of the participants were performed. To analyze the compliance effect, 3 cohorts were created. The 7 participants who demonstrated the highest compliance rate were classified in the high-compliance group. The 7 participants who recorded compliance rate after the top 7 compliant participants were labeled as a moderate-compliance group. Rest of the 7 participants who did not perform the trunk and hip–focused INT were labeled as noncompliance group. To examine the compliance effects on the hip abductor peak torque development, changed hip abductor peak torque values (posttesting values minus pretesting values) were calculated and 1-way analysis of variance (ANOVA) was employed to find significantly different hip abductor peak torque changes among the 3 compliance groups. When a statistical difference was detected, a post hoc test (Boneferroni) was used to avoid type 1 error. Alpha level was set at 0.05 priori. Furthermore, a Pearson’s correlation coefficient value (r) was analyzed with the trunk and hip–focused INT exercise compliance and the hip abductor peak torque changes. Assumption of linearity including outlier and normality was checked priori. Both analyses were performed using SPSS version 18 (SPSS, Inc, Chicago, IL, USA).
Results
All participants’ data including mean and SD of height, mass, age, and pre- and posthip abductor peak torque values were calculated (Table 1). The mean compliance rates of the high and moderate groups were 86.4% and 71.4% (Table 1). For the hip abductor peak torque changes, the participants in the high- and moderate-compliance group demonstrated 16.2% and 9.7% of increases; however, the participants in the control group showed 1.1% decreases of hip abductor peak torque over the change of this study (Table 2).
Table 1.
Mean and SD of the participants’ height, weight, age, compliance rates, and hip abductor peak torque values in pretesting and posttesting.
| Noncompliance (N = 7) |
Moderate-compliance group (N = 7) |
High-compliance group (N = 7) |
|
|---|---|---|---|
| Height, cm | 173.4 ± 10.0 | 170.3 ± 5.0 | 171.6 ± 4.9 |
| Weight, kg | 63.9 ± 5.3 | 59.4 ± 4.5 | 68.8 ± 8.3 |
| Age, y | 16.0 ± 1.7 | 15.5 ± 1.4 | 15.5 ± 1.3 |
| Compliance rate, % |
NA* | 71.4 ± 3.8 | 86.4 ± 6.3 |
Not applicable.
Table 2.
Mean and SD of the participants’ hip abductor peak torque values in pretesting and posttesting.
| Noncompliance (N = 7) |
Moderate-compliance group (N = 7) |
High-compliance group (N = 7) |
|
|---|---|---|---|
| Hip abductor peak torque at pretesting values (ft-lbs) |
52.2 ± 10.4 | 46.4 ± 9.9 | 46.4 ± 10.4 |
| Hip abductor peak torque at posttesting values (ft-lbs) |
51.6 ± 6.1 | 51.4 ± 7.8 | 55.4 ± 13.1 |
| Hip abductor peak torque changed values (ft-lbs) |
−0.6*† | +5.1*† | +9.0†‡ |
| Hip abductor peak torque changed values, % |
−1.1 | +9.7 | +16.2 |
The change value differences between noncompliance and moderate-compliance groups were not statistically significant (p = 0.68).
The change value differences between the high-compliance and noncompliance groups were statistically significant (p = 0.02).
The change value differences between moderate- and high-compliance groups were not statistically significant (p = 0.27).
One-way ANOVA indicated that there were statistical differences among the 3 compliance cohorts (p = 0.02). Post hoc test (Bonferroni) detected that there was no significant hip abductor peak torque changes between the high-compliance and moderate-compliance groups (p = 0.27) and moderate-compliance and noncompliance groups (p = 0.68) (Table 2). However, a statistically different hip abductor peak torque changes were found between high-compliance and noncompliance groups (p = 0.02). The r-value between the hip abductor peak torque changes based on the 3 compliance groups was recorded as 0.56 (Figure 2).
Figure 2.
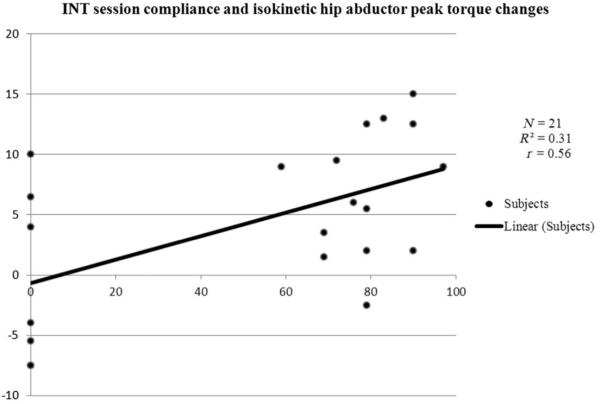
Correlation between the trunk and hip INT compliance and hip abductor peak torque changes (N = 21). INT, integrative neuromuscular training.
Discussion
The purpose of this study was to investigate compliance effect of proximal neuromuscular training, a trunk and hip–focused INT, on isokinetic hip abductor strength in young women athletes. The main finding of this study was that subjects in the moderate compliance group did not demonstrate significantly different hip abductor peak torque changes compared with noncompliance group (Table 2). On the other hand, those subjects who were labeled as a high-compliance group showed significantly greater hip abductor peak torque changes relative to noncompliance group (Table 2). In addition, a moderate linear association was recorded between the hip abductor peak torque changes and the 3 compliance groups (Figure 2). It can be interpreted that attending, performing, and completing the trunk and hip exercises are directly associated with greater increases in isokinetic hip abductor strength. Additionally, this information can be clinically translated to suggest that health care providers need to not only check patients’ attendance for assigned treatment sessions but also emphasize the importance of ensuring actual completion of exercises performed.
Several studies have intervened hip-oriented neuromuscular training in women population for the purpose of achieving hip abductor strength improvement (5,7,9). By implementing trunk and hip neuromuscular training in young adult women population (N = 14, mean age = 20.7 ± 1.7 years) for 8 weeks, a study found an association between eccentric hip abductor strength and knee kinematic improvements (5). The study reported increases of hip abductor strength of 9.7% in posttesting and decreases in knee abduction angles in the single leg squat task (5). Another study with a randomized cohort design that incorporated a set of hip exercises in women (N = 17, mean age = 25 ± 5 years) with PFPS pain for 8 weeks (hip oriented exercises were given in first 4 weeks) documented 21.0% of isometric hip abductor strength improvement (7). Additionally, a study with adult women participants (N = 15, mean age = 35.2 ± 12.2 years) with PFPS reported a 25.6% of isometric hip abductor strength increase (12.9 ± 4.1% body weight [BW] at baseline, 17.1 ± 3.1% BW at posttesting) as a result of 3 weeks of tubing band exercise intervention (9). Although this study demonstrated a significant hip abductor strength increase, knee abduction angles, which were expressed as genu valgum in the original study, during treadmill running did not differ between pre- and postintervention (9).
Compared with this study, prior studies (7,9) demonstrated greater relative hip abductor strength (21.0% and 25.6%) increases, respectively. However, the association between participants’ compliance and hip abductor strength gains was not clearly shown. From a compliance standpoint, the study gave participants an exercise log to check the home exercise compliance, but the compliance information was not found in the original study (7). In addition, Ferber et al. (9) did not state any compliance information in the study; thus, it is difficult to compare the effect of the given intervention based on compliance alone. In the study by Ferber et al (9), which investigated dosage of the neuromuscular intervention (actual number of exercises performed and session length and frequency), the participants performed 2 types of tubing exercises that took 5–10 minutes daily for 3 weeks. Although the frequency of the intervention sessions was high (daily), the number of exercises performed, length of the intervention session, and the duration of the study were the lowest among all investigations including this study. However, this study demonstrated the greatest hip abductor strength increase (25.6%) compared with the rest of the studies (5,7) including this study. In fact, the study performed by Baldon et al. (5) incorporated more trunk and hip exercises than the study by Feber et al (9) and provided longer intervention sessions (90 minutes per session) and study durations (8 weeks). The study set an inclusion criterion to a minimal compliance rate of participation at least 19 sessions of 24 total sessions (80%) (5). The mean compliance rate of the study was 87%, and no participants dropped out from this study because of the predetermined compliance cutoff. However, the hip abductor strength increase was approximately 10% compared with the prevalue, which is much lower than the increases observed in the study by Ferber et al. In short, the hip abductor strength increases do not correspond to the given neuromuscular training dosage.
An underlying reason for the greater hip abductor strength gains in the prior studies (7,9) may stem from the type of the participants. The study performed by Ferber et al. (9) had patients with PFPS as a subject population. Another study, that also used patients with PFPS, showed a 21.0% hip abductor strength increase as a result of implementing 8 weeks of rehabilitative exercises (a combination of 4 weeks of hip-focused exercise and 4 weeks of functional weight-bearing exercises) (7). However, the study performed by Baldon et al. (5) that examined women individuals did not have a PFPS condition. Recent clinical studies reported lower hip abductor strength in women with PFPS compared with women without PFPS (1,4,16). Therefore, the greater hip abductor strength increases observed in the 2 studies (7,9) may be primarily because of lower hip abductor strength baseline associated with the PFPS condition. In another words, women who have a lower hip abductor strength baseline are more responsive to hip-focused neuromuscular exercises than women who already have an average or within normal level of hip abductor strength.
Because this study demonstrated a strong association between trunk and hip–focused INT compliance and isokinetic hip abductor strength changes, the compliance is imperative for those who have lower hip abductor strength such as women with PFPS. Yet, several previous studies struggled in achieving high neuromuscular compliance and noted it as a limitation (23,28). To successfully incorporate neuromuscular training, the achievement of understanding and acceptance for the training from health care providers, coaching staff, and each athlete was advocated (11). Additionally, it was stated that providing variety and progression to improve neuromuscular training may be a key to enhance neuromuscular training compliance. In this study, a qualified instructor (G.D.M., who holds a certified strength and conditioning specialist certification) supervised every neuromuscular training session. The coaching staff members and the athletes were receptive of his instruction. Additionally, the INT program was designed to offer upto 13 diverse exercises per session and was divided into 5 phases. Each of the INT exercises was individually progressed in phases by increasing the degree of difficulty. Each phase of the progressive INT was designed to bring more challenges, which was intended to enhance the intensity of each exercise throughout the duration of the study. The wide variety of exercise selections and periodized progression may have assisted in maintaining 78.9% of compliance rates of the intervention group in this study.
Another interesting discussion point is how long the neuromuscular training effects can be retained. A study was conducted to test the retention of motor movement, which was approximately 15 minutes of balance training to women handball players (15). The balance training was given a minimum of 3 times per week in preseason (5–7 weeks) and once a week during in-season (for ~5 months). This study found that the participants improved balance ability after 8 weeks, and the gained balance ability was maintained approximately ± months after the completion of the program. Furthermore, a recent study evaluated motor learning retention ability of the lower extremity (25) by implementing a 10–15-minutes ACL prevention program for 3–4 times per week. This study assessed jump landing movement patterns in 14-year-old girls and boys in 2 groups as follows: 3-month and 9-month durations. This study reported that the 9-month group retained the learned landing movement patterns for 3 months after post-ACL prevention training program, whereas the landing movement patterns of the participants in the 3-month group returned to their original movements after 3 months. According to this result, it seems that a motor skill is better retained with higher dosage and longer duration training (25). Cumulatively, the current results add to the literature that there seems to be a certain threshold of exercise to influence the desired adaptations for injury risk reduction or reductions in symptoms. Future work focused on the dosage thresholds is warranted in helping guide future intervention design.
The limitations to this study should be stated. The participants in the noncompliance group had higher hip abductor peak torque at pretesting compared with the participants in the moderate- and high-compliance groups, which can be perceived as a confounding variable. However, to minimize the pretesting value differences among the groups, the change values, posttesting values minus pretesting values, were used for the analysis. Additionally, sample size of each compliance group was small; therefore, analysis to detect a difference among each group was not performed in the current analysis. This needs to be addressed in future research. One aspect of neuromuscular training that would influence the magnitude of muscular strength development is intensity. Compliance and dosage (number of exercises, frequency and length of session, and duration of intervention) can be measured objectively. However, it was challenging to measure a level of intensity from the participants although the qualified instructor (G.D.M., who holds a certified strength and conditioning specialist certification) was present for every training session. Furthermore, concentric hip abductor strength measurements were taken instead of eccentric strength. Because ACL injury and PFPS pathologies occurred in closed kinetic chain motions, it was theorized that lower extremity muscles eccentrically contracts (3,24). Thus, an eccentric hip abductor muscle strength measurement was desirable instead of concentric hip abductor peak torque measures. Last, the participants in the intervention group performed routine strength training once a week in addition to the trunk and hip–focused INT. Therefore, the routine strength training might have possibly contributed to the hip abductor peak torque changes.
A significant positive correlation was observed between the hip abductor strength improvement and the trunk and hip–focused INT exercise compliance. The hip abductor strength improvement responses seemed to be directly related to the dosage of the specific trunk and hip–focused INT. In comparison with other studies, it seems that hip abductor strength responses may be sensitive to a subject population. More specifically, the greater hip abductor strength gain may be obtained if the initial hip abductor strength has a deficit. Because those who have hip abductor strength deficit seemr more responsive to neuromuscular training, participation and practice of the trunk and hip–focused INT exercises are believed to be highly beneficial. Adaptations from trunk and hip–focused training that improve hip abductor strength and recruitment may be protective against high knee abduction or valgus loading during dynamic movements and potentially reduce ACL and PFPS risk in young women athletes. Future studies are warranted to include biomechanical measures and injury outcome data along with hip abductor strength changes.
Practical Applications
Ten weeks of trunk and hip–focused INT, a series of exercise programs aiming to improve trunk and hip strength and power and dynamic stabilization, demonstrated the increases in isokinetic hip abductor strength among young women athletes. The participants who complied with the trunk and hip–focused INT with high level demonstrated significant hip abductor peak torque compared with control group, but not between moderate and noncompliance groups. The observed isokinetic hip abductor strength increases were directly associated with compliance of the trunk and hip–focused INT. Therefore, participating in the trunk and hip–focused INT seemed to be an effective neuromuscular training intervention to increase hip abductor strength in young women athletes when compliance with the training program was high. Because the significant difference and strong association between the trunk and hip–focused INT compliance and hip abductor strength changes has been established, health care and strength and conditioning professionals should pay attention to compliance when incorporating a neuromuscular training into their current training program and should consider tracking participation, performance of and completion of given exercises. Because hip abductor weakness is linked to PFPS, hip abductor strength enhancement may potentially help to improve the existing PFPS condition or provide prophylactic effects for future PFPS development.
Acknowledgments
The authors would like to thank Ms. Catherine P. Starnes for her statistical expertise and guidance for this project. The authors would like to acknowledge funding support from National Institutes of Health/NIAMS grants R01-AR049735, R01-AR055563, and R01-AR056259.
References
- 1.Baldon Rde M, Nakagawa TH, Muniz TB, Amorim CF, Maciel CD, Serrao FV. Eccentric hip muscle function in females with and without patellofemoral pain syndrome. J Athl Train. 2009;44:490–496. doi: 10.4085/1062-6050-44.5.490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boling MC, Padua DA, Alexander Creighton R. Concentric and eccentric torque of the hip musculature in individuals with and without patellofemoral pain. J Athl Train. 2009;44:7–13. doi: 10.4085/1062-6050-44.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boling MC, Padua DA, Marshall SW, Guskiewicz K, Pyne S, Beutler A. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: The Joint Undertaking to Monitor and Prevent ACL Injury (JUMP-ACL) cohort. Am J Sports Med. 2009;37:2108–2116. doi: 10.1177/0363546509337934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cichanowski HR, Schmitt JS, Johnson RJ, Niemuth PE. Hip strength in collegiate female athletes with patellofemoral pain. Med Sci Sports Exerc. 2007;39:1227–1232. doi: 10.1249/mss.0b013e3180601109. [DOI] [PubMed] [Google Scholar]
- 5.Baldon Rde M, Lobato DF, Carvalho LP, Lam Wun PY, Santiago PR, Serrao FV. Effect of functional stabilization training on lower limb biomechanics in women. Med Sci Sports Exerc. 2012;44:135–142. doi: 10.1249/MSS.0b013e31822a51bb. [DOI] [PubMed] [Google Scholar]
- 6.Dierks TA, Manal KT, Hamill J, Davis IS. Proximal and distal influences on hip and knee kinematics in runners with patellofemoral pain during a prolonged run. J Orthop Sports Phys Ther. 2008;38:448–456. doi: 10.2519/jospt.2008.2490. [DOI] [PubMed] [Google Scholar]
- 7.Dolak KL, Silkman C, Medina McKeon J, Hosey RG, Lattermann C, Uhl TL. Hip strengthening prior to functional exercises reduces pain sooner than quadriceps strengthening in females with patellofemoral pain syndrome: A randomized clinical trial. J Orthop Sports Phys Ther. 2011;41:560–570. doi: 10.2519/jospt.2011.3499. [DOI] [PubMed] [Google Scholar]
- 8.Earl JE, Hoch AZ. A proximal strengthening program improves pain, function, and biomechanics in women with patellofemoral pain syndrome. Am J Sports Med. 2011;39:154–163. doi: 10.1177/0363546510379967. [DOI] [PubMed] [Google Scholar]
- 9.Ferber R, Kendall KD, Farr L. Changes in knee biomechanics after a hip-abductor strengthening protocol for runners with patellofemoral pain syndrome. J Athl Train. 2011;46:142–149. doi: 10.4085/1062-6050-46.2.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ford KR, Myer GD, Smith RL, Vianello RM, Seiwert SL, Hewett TE. A comparison of dynamic coronal plane excursion between matched male and female athletes when performing single leg landings. Clin Biomech (Bristol, Avon) 2006;21:33–40. doi: 10.1016/j.clinbiomech.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 11.Frisch A, Croisier JL, Urhausen A, Seil R, Theisen D. Injuries, risk factors and prevention initiatives in youth sport. Br Med Bull. 2009;92:95–121. doi: 10.1093/bmb/ldp034. [DOI] [PubMed] [Google Scholar]
- 12.Hewett TE, Myer GD, Ford KR, Heidt RS, Colosimo AJ, McLean SG, van den Bogert AJ, Paterno MV, Succop P. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. Am J Sports Med. 2005;33:492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 13.Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes. Decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24:765–773. doi: 10.1177/036354659602400611. [DOI] [PubMed] [Google Scholar]
- 14.Hewett TE, Torg JS, Boden BP. Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: Lateral trunk and knee abduction motion are combined components of the injury mechanism. Br J Sports Med. 2009;43:417–422. doi: 10.1136/bjsm.2009.059162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Holm I, Fosdahl MA, Friis A, Risberg MA, Myklebust G, Steen H. Effect of neuromuscular training on proprioception, balance, muscle strength, and lower limb function in female team handball players. Clin J Sport Med. 2004;14:88–94. doi: 10.1097/00042752-200403000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Ireland ML, Willson JD, Ballantyne BT, Davis IM. Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther. 2003;33:671–676. doi: 10.2519/jospt.2003.33.11.671. [DOI] [PubMed] [Google Scholar]
- 17.Mandelbaum BR, Silvers HJ, Watanabe DS, Knarr JF, Thomas SD, Griffin LY, Kirkendall DT, Garrett W. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year followup. Am J Sports Med. 2005;33:1003–1010. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 18.Myer GD, Chu DA, Brent JL, Hewett TE. Trunk and hip control neuromuscular training for the prevention of knee joint injury. Clin Sports Med. 2008;27:425–448. doi: 10.1016/j.csm.2008.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Myer GD, Ford KR, Barber Foss KD, Goodman A, Ceasar A, Rauh MJ, Divine JG, Hewett TE. The incidence and potential pathomechanics of patellofemoral pain in female athletes. Clin Biomech (Bristol, Avon) 2010;25:700–707. doi: 10.1016/j.clinbiomech.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Myer GD, Ford KR, Brent JL, Hewett TE. The effects of plyometric vs. dynamic stabilization and balance training on power, balance, and landing force in female athletes. J Strength Cond Res. 2006;20:345–353. doi: 10.1519/R-17955.1. [DOI] [PubMed] [Google Scholar]
- 21.Myer GD, Ford KR, Brent JL, Hewett TE. Differential neuromuscular training effects on ACL injury risk factors in “high-risk” versus “low-risk” athletes. BMC Musculoskelet Disord. 2007;8:39. doi: 10.1186/1471-2474-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Myer GD, Ford KR, Palumbo JP, Hewett TE. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. J Strength Cond Res. 2005;19:51–60. doi: 10.1519/13643.1. [DOI] [PubMed] [Google Scholar]
- 23.Myklebust G, Engebretsen L, Braekken IH, Skjolberg A, Olsen OE, Bahr R. Prevention of anterior cruciate ligament injuries in female team handball players: A prospective intervention study over three seasons. Clin J Sport Med. 2003;13:71–78. doi: 10.1097/00042752-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Nakagawa TH, Baldon Rde M, Muniz TB, Serrao FV. Relationship among eccentric hip and knee torques, symptom severity and functional capacity in females with patellofemoral pain syndrome. Phys Ther Sport. 2011;12:133–139. doi: 10.1016/j.ptsp.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 25.Padua DA, DiStefano LJ, Marshall SW, Beutler AI, de la Motte SJ, DiStefano MJ. Retention of movement pattern changes after a lower extremity injury prevention program is affected by program duration. Am J Sports Med. 2012;40:300–306. doi: 10.1177/0363546511425474. [DOI] [PubMed] [Google Scholar]
- 26.Petersen W, Braun C, Bock W, Schmidt K, Weimann A, Drescher W, Eiling E, Stange R, Fuchs T, Hedderich J, Zantop T. A controlled prospective case control study of a prevention training program in female team handball players: The German experience. Arch Orthop Trauma Surg. 2005;125:614–621. doi: 10.1007/s00402-005-0793-7. [DOI] [PubMed] [Google Scholar]
- 27.Soligard T, Nilstad A, Steffen K, Myklebust G, Holme I, Dvorak J, Bahr R, Andersen T. Compliance with a comprehensive warm-up programme to prevent injuries in youth football. Br J Sports Med. 2010;44:787–793. doi: 10.1136/bjsm.2009.070672. [DOI] [PubMed] [Google Scholar]
- 28.Steffen K, Myklebust G, Olsen OE, Home I, Bahr R. Preventing injuries in female yough football—A cluster-randomized controlled trial. Scand J Med Sci Sports. 2008;18:605–614. doi: 10.1111/j.1600-0838.2007.00703.x. [DOI] [PubMed] [Google Scholar]
- 29.Sugimoto D, Myer GD, Bush HM, Klugman MF, Medina McKeon JM, Hewett TE. Compliance with neuromuscular training and anterior cruciate ligament injury risk reduction in female athletes: A meta-analysis. J Athl Train. 2012;47:714–723. doi: 10.4085/1062-6050-47.6.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zazulak BT, Ponce PL, Straub SJ, Medvecky MJ, Avedisian L, Hewett TE. Gender comparison of hip muscle activity during single-leg landing. J Orthop Sports Phys Ther. 2005;35:292–299. doi: 10.2519/jospt.2005.35.5.292. [DOI] [PubMed] [Google Scholar]