Abstract
Background
Preterm prelabour rupture of membranes (PPROM) is associated with increased risk of maternal and neonatal morbidity and mortality. Women with PPROM have been predominantly managed in hospital. It is possible that selected women could be managed at home after a period of observation. The safety, cost and women’s views about home management have not been established.
Objectives
To assess the safety, cost and women’s views about planned home versus hospital care for women with PPROM.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register (January 2010) and the reference lists of all the identified articles.
Selection criteria
Randomised and quasi-randomised trials comparing planned home versus hospital management for women with PPROM before 37 weeks’ gestation.
Data collection and analysis
Two review authors independently assessed clinical trials for eligibility for inclusion, risk of bias, and carried out data extraction.
Main results
We included two trials (116 women) comparing planned home versus hospital management for PPROM. Overall, the number of included women in each trial was too small to allow adequate assessment of pre-specified outcomes. Investigators used strict inclusion criteria and in both studies relatively few of the women presenting with PPROM were eligible for inclusion. Women were monitored for 48 to 72 hours before randomisation. Perinatal mortality was reported in one trial and there was insufficient evidence to determine whether it differed between the two groups (risk ratio (RR) 1.93, 95% confidence interval (CI) 0.19 to 20.05). There was no evidence of differences between groups for serious neonatal morbidity, chorioamnionitis, gestational age at delivery, birthweight and admission to neonatal intensive care.
There was no information on serious maternal morbidity or mortality. There was some evidence that women managed in hospital were more likely to be delivered by caesarean section (RR (random-effects) 0.28, 95% CI 0.07 to 1.15). However, results should be interpreted cautiously as there is a moderate heterogeneity for this outcome (I2 = 35%). Mothers randomised to care at home spent approximately 10 fewer days as inpatients (mean difference −9.60, 95% CI −14.59 to −4.61) and were more satisfied with their care. Furthermore, home care was associated with reduced costs.
Authors’ conclusions
The review included two relatively small studies that did not have sufficient statistical power to detect meaningful differences between groups. Future large and adequately powered randomised controlled trials are required to measure differences between groups for relevant pre-specified outcomes. Special attention should be given to the assessment of maternal satisfaction with care and cost analysis as they will have social and economic implications in both developed and developing countries.
Medical Subject Headings (MeSH): *Home Care Services; *Hospitalization; *Patient Discharge; Chorioamnionitis [epidemiology]; Fetal Membranes, Premature Rupture [mortality; *therapy]; Infant, Newborn; Infant, Newborn, Diseases [diagnosis]; Length of Stay; Patient Satisfaction; Perinatal Mortality
MeSH check words: Female, Humans, Pregnancy
BACKGROUND
Description of the condition
Preterm prelabour rupture of membranes (PPROM) is the spontaneous rupture of the membranes before 37 weeks’ gestation, and where there is at least an hour between membrane rupture and the onset of contractions. It is further classified by gestational age: mid-trimester PPROM (before 24 weeks), early PPROM (24 to 34 weeks), and near-term PPROM (34 to 37 weeks). It occurs in 3% of pregnancies and is responsible for approximately one-third of all preterm births (Bartfield 1998; Goldenberg 1998).
A number of factors increase the risk of PPROM, including history of premature birth, black race, genetic factors, socio-economic status, smoking, low maternal weight, multiple pregnancy, nutritional deficiencies, prior cervical conisation, cervical cerclage, amniocentesis, vaginal bleeding in pregnancy and infection (Mercer 2007). At the same time, PPROM often occurs in the absence of any known risk factors (Besinger 1993; Medina 2006; Mercer 2007; Mingione 2006). The physiological mechanisms leading to PPROM are poorly understood, but may include excessive stretching of the membranes (due to uterine over-distension, as in multiple pregnancies, or an increase in the amount of fluid around the fetus, i.e. polyhydramnios); membrane defects like decreasing collagen content; placental abruption, or problems arising from infection. Between one-quarter and one-half of women with PPROM will have infection at the time of presentation (Simhan 2005).
PPROM may result in immediate risks such as cord prolapse, cord compression and placental abruption; and later problems such as maternal or neonatal infection, as well as the use of interventions including induction of labour, caesarean section and instrumental vaginal delivery. It is estimated that one-half of women with PPROM will go into labour within a week, and three-quarters within a fortnight (Goldenberg 2008). Premature delivery is the major cause of perinatal morbidity and mortality associated with PPROM, and survival of the baby after PPROM largely depends on gestational age (Mercer 2003). The related morbidities associated with prematurity include respiratory distress syndrome (RDS), intraventricular haemorrhage, necrotising enterocolitis, prolonged stay in the neonatal nursery, difficulty with thermoregulation, difficulty with breastfeeding and infection. Current evidence suggests that fetal complications are directly related to gestational age at delivery. Several investigators observed a decrease in neonatal morbidity associated with birth after 34 weeks’ gestation (Lewis 1996b; Mercer 2003; Neerhof 1999). The incidence of RDS, hyperbilirubinaemia and duration of stay in the neonatal nursery was significantly reduced in infants born after 34 weeks’ gestation, compared with those born earlier (Lewis 1996b;Neerhof 1999). On the other hand, prolonged rupture of membranes with lack of amniotic fluid around the fetus may have an impact on limb movements, causing postural deformities and on lung development, predisposing to pulmonary hypoplasia and severe respiratory distress after delivery. Mothers are at increased risk of placental abruption and antenatal as well as postpartum infection. Serious maternal consequences following PPROM are uncommon, but serious infections occur in approximately 5% of babies. Maternal infection during pregnancy, chorioamnionitis, may lead to serious complications in newborns, including cerebral palsy and septicaemia (Neufeld 2005; Ronnestad 2005; Woldesenbet 2005). Most of the evidence on the consequences of PPROM has come from studies in developed countries; outcomes for babies following PPROM, particularly at low gestational ages, may be very poor in developing countries, and mothers may also face risks of serious infectious morbidity (Obi 2007).
While preterm labour and PPROM are distinct, many of the interventions used to treat the conditions are the same. Management of PPROM varies in different settings and according to facilities, local guidelines and protocols and the approach of individual clinicians (ACOG Committee 2007; Buchanan 2004; Giles 2005;Lumley 1991). In a survey of obstetric units in the United States of America, 30% of the units surveyed had formal management protocols (Ramsey 2004). The management of PPROM is dependent upon the gestational age at which rupture of the membranes occurs. The health benefits for the fetus in continuing a pregnancy after PPROM may be considerable, particularly in the late second and early third trimesters of pregnancy (between 24 and 34 weeks’ gestation). Current evidence suggests that among women with PPROM between 24 and 34 weeks’ gestation, the use of antibiotics significantly improves neonatal and maternal morbidity including prolongation of pregnancy, reduced need for surfactant and oxygen therapy, reduction in neonatal infection, and less risk of abnormal cerebral ultrasound (Kenyon 2003; Kenyon 2007). In addition, antenatal corticosteroids have been shown to reduce the risk of neonatal respiratory distress, intraventricular haemorrhage and neonatal death in the preterm neonate (Crowther 2007;Roberts 2006). However, there is currently no consensus as to the optimal management of PPROM in women in whom the fetus is relatively mature, at gestations near to term (greater than 34 weeks’ gestation), and it is currently the subject of a Cochrane review (Buchanan 2008). The aim of planned expectant management is to maximise the benefits of further fetal maturity while avoiding the potential harms of remaining in utero. It involves observation of the mother and fetus for early signs of fetal or maternal infection while awaiting the spontaneous onset of labour and, if labour does not ensue, planning for delivery at term. There is no evidence to support the best place to carry out this observation. Although clinicians may feel that it is easier to monitor women in a hospital setting, women’s views may be different. Ramsey 2004 et al noted that, in a study of obstetric services in the United States, 43% of respondents would consider outpatient care of women after PPROM where the fetus was of viable gestational age, despite the lack of evidence on this approach.
There are a number of possible interventions for PPROM including the use of steroids (Roberts 2006); antibiotics (Kenyon 2003); amnioinfusion (Hofmeyr 1998); tocolytics (Seibel-Seamon 2008); and planned early birth versus expectant management (Buchanan 2008) which are the subject of other Cochrane reviews, and are outside the scope of this review.
Description of the intervention
For women with mid-trimester PPROM, before fetal viability has been established, discharge home has been one of the traditional mainstays of management. Where the fetus is viable, discharge home (as opposed to hospital care) has been more controversial. The advantages of home management may include convenience to women and their families, and reduced costs for healthcare providers. Set against this are the disadvantages associated with any increased risk which may arise from distance from facilities for delivery or emergency care.
In some circumstances, outpatient care after PPROM may not be suitable: for example, where either the mother or the fetus required continuous monitoring or where treatment is required that it would not be feasible to provide at home. Hospital care has also been used to enforce bed rest, which, in the past has formed part of management of PPROM, although there is no evidence that bed rest is helpful, and no evidence that women at home, advised to rest, are less likely to comply.
Some conditions preclude the use of outpatient care including symptomatic infection, fetal compromise or the onset of labour (Ellestad 2008; Lewis 1996). There is, however, concern that, irrespective of the condition of the mother or baby following PPROM, outpatient management could place women at serious risk of infection or fetal distress that requires rapid intervention.
Women considered suitable for possible home management following PPROM include those living within easy travelling distance of hospital and with access to reliable transportation. Planned home management can be initiated after a period of monitoring in hospital and, when appropriate, treatment with antibiotics has commenced. Ideally women should not be in labour and there would be no evidence of infection or oligohydramnios (Ayres 2002; Bartfield 1998). It is not clear what proportion of women with PPROM would meet these criteria.
Why it is important to do this review
Women with PPROM have been predominantly managed in hospital. It is possible that selected women could be discharged home after a period of observation. The safety of home management has not been established, neither is it known whether women prefer this approach, nor whether it would offer potential for reduced costs for health service providers.
OBJECTIVES
The objective of this review is to assess the effects of planned home versus hospital care for women with preterm prelabour rupture of the membranes (PPROM) prior to 37 weeks’ gestation on fetal, infant and maternal wellbeing. We will also examine acceptability to women and costs of planned home versus hospital care for women with PPROM.
METHODS
Criteria for considering studies for this review
Types of studies
Published and unpublished randomised and quasi-randomised trials including cluster randomised trials. Crossover trials are not an appropriate study design for this intervention and we have not included them.
Types of participants
Women with preterm prelabour rupture of the membranes (PPROM) before 37 weeks’ gestation with no specific maternal or fetal contraindications to expectant management (defined by trialists).
Types of interventions
Studies comparing management of PPROM at home versus hospital. We envisaged that women in the home care groups would have received assessment, monitoring and possibly treatment in hospital according to gestational age before discharge home.
Types of outcome measures
Primary outcomes
We have chosen four primary outcomes as being the most representative of the clinically important measures of effectiveness.
Perinatal mortality (only includes deaths between fetal viability (24 weeks’ gestation) and the end of the 7th day after delivery, or as defined by trial authors).
Neonatal infection/sepsis (proven neonatal infection with positive blood culture within 48 hours or more after birth, or culture proven neonatal pneumonia or meningitis).
Maternal mortality.
Serious maternal morbidity (including septicaemia, admission to intensive care unit, organ failure, major postpartum haemorrhage, hysterectomy).
Secondary outcomes
Maternal
Maternal chorioamnionitis (variously defined by authors).
Maternal endometritis (variously defined by authors).
Vaginal birth/caesarean section.
Induction of labour.
Postpartum maternal pyrexia (variously defined by authors).
Days of antenatal hospitalisation.
Days of postnatal hospitalisation.
Breastfeeding initiated in hospital.
Breastfeeding at hospital discharge.
Views of care.
Preferences of care.
Fetal
Gestational age at birth.
Days from randomisation to birth.
Birth within 48 hours after rupture membranes.
Birth within seven days of rupture of membranes.
Birth before 37 weeks’ gestation.
Stillbirth (only includes deaths between the fetal viability (24 weeks’ gestation) and delivery or as defined by trial authors).
Neonatal
Neonatal mortality only includes deaths in the first 28 days of life.
Postneonatal mortality only includes deaths after 28 days of life but before one year.
Infant death (at 12 months of age).
Respiratory distress syndrome.
Use of surfactant.
Use of mechanical ventilation.
Days of mechanical ventilation.
Days of oxygen therapy.
Oxygen treatment greater than 28 days.
Oxygen therapy at 36 weeks’ postmenstrual age.
Birthweight.
Birthweight less than 2500 grams.
Birthweight less than 1500 grams.
Admission to neonatal intensive care unit.
Length of stay in neonatal intensive care unit.
Days from birth to discharge home from hospital.
Major cerebral abnormalities on ultrasound prior to discharge.
Necrotising enterocolitis.
Neonatal encephalopathy (as described by authors).
Presumed neonatal infection up to 48 hours of birth.
Presumed neonatal infection 48 hours or more after birth.
Postural deformities (as defined by authors).
Disability at time of childhood follow up (as defined by authors).
Serious disability (as defined by authors) after two years.
Other
Cost analysis (according to authors).
Search methods for identification of studies
Electronic searches
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register by contacting the Trials Search Co-ordinator (January 2010).
The Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Trials Search Co-ordinator and contains trials identified from:
quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE;
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL and MEDLINE, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service can be found in the ‘Specialized Register’ section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
Trials identified through the searching activities described above are each assigned to a review topic (or topics). The Trials Search Co-ordinator searches the register for each review using the topic list rather than keywords.
Searching other resources
We examined the reference lists of all the articles identified by the search strategy to try to identify any further trials.
We did not apply any language restrictions.
Data collection and analysis
Selection of studies
Two review authors (T Dowswell (TD) and G El Senoun (GE)) independently assessed for inclusion all the identified studies. We resolved any disagreement through discussion or, if required we consulted the third author (HA Mousa (HAM)).
In view of the limited amount of research carried out in this topic area, we planned to include studies where results were reported in abstracts provided that there was sufficient information to allow us to assess eligibility and to make some assessment of risk of bias. Where abstracts were identified by the search strategy and there was insufficient information on methods or results, we contacted study authors for more information.
Data extraction and management
We designed a form to extract data. For eligible studies, two review authors (TD and GE) extracted the data using the agreed form. We resolved discrepancies through discussion or, if required, we consulted the third author (HAM). TD entered data into Review Manager software (RevMan 2008) and GE checked for accuracy. When information regarding any of the above was unclear, we attempted to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
We independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008). We resolved any disagreement by discussion or by involving a third assessor.
(1) Sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
adequate (any truly random process, e.g. random number table; computer random number generator);
inadequate (any non-random process, e.g. odd or even date of birth; hospital or clinic record number); or
unclear.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal the allocation sequence in sufficient detail and determined whether allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
adequate (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
inadequate (open random allocation; unsealed or non-opaque envelopes; alternation; date of birth);
unclear.
(3) Blinding (checking for possible performance bias)
We described for each included study the methods used, if any, to blind study personnel from knowledge of which intervention a participant received. With interventions involving different care management, e.g. home versus hospital care, it is generally not feasible to blind participants and clinical staff to group allocation. So we did not formally assess blinding, but we noted if there had been any attempt to blind outcome assessors and considered whether the lack of blinding was likely to affect results.
(4) Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, protocol deviations)
We have described for each included study, and for each outcome or class of outcomes, the completeness of data, including attrition and exclusions from the analysis. We have stated whether attrition and exclusions were reported, the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or supplied by the trial authors, we planned to re-include missing data in the analyses. We assessed methods as:
adequate;
inadequate;
unclear.
(5) Selective reporting bias
We have described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
adequate (where it is clear that all of the study’s prespecified outcomes and all expected outcomes of interest to the review have been reported);
inadequate (where not all the study’s pre-specified outcomes have been reported; one or more reported primary outcomes were not pre-specified; outcomes of interest were reported incompletely and so could not be used; study failed to include results of a key outcome that would have been expected to have been reported);
unclear.
(6) Other sources of bias
We have described for each included study any important concerns we had about other possible sources of bias such as baseline imbalance between groups.
(7) Overall risk of bias
We have made explicit judgements about whether studies are at high risk of bias, according to the criteria given in the Handbook (Higgins 2008). With reference to (1) to (6) above, we have assessed the likely magnitude and direction of the bias and whether we considered it likely to impact on the findings. We have included only two studies in this version of the review. In updates of the review, as more studies are added we will explore the impact of the level of bias through undertaking sensitivity analyses - see ’ Sensitivity analysis’.
Measures of treatment effect
Dichotomous data
For dichotomous data, we have presented results as summary risk ratio (RR) with 95% confidence intervals (CI).
Continuous data
For continuous data, we have used the mean difference if outcomes were measured in the same way between trials. We have used the standardised mean difference to combine trials that measured the same outcome, but using different methods.
Unit of analysis issues
Cluster randomised trials
For this version of the review we did not identify any cluster randomised trials but if such trials are conducted in the future we will include them in updates. Cluster trials which are otherwise eligible for inclusion will be in the analyses along with individually-randomised trials. We will adjust the standard error of the effect estimate from cluster trials using the methods described in the Handbook (Higgins 2008). We will carry out meta-analyses using the generic inverse-variance method available in RevMan (RevMan 2008). We will use an estimate of the intracluster correlation co-efficient (ICC) derived from the trial (if possible), or from another source. If ICCs from other sources are used, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC. If we identify both cluster-randomised trials and individually-randomised trials, we plan to synthesise the relevant information. We will consider it reasonable to combine the results from both if there is little heterogeneity between the study designs, and the interaction between the effect of intervention and the choice of randomisation unit is considered to be unlikely. We will also acknowledge heterogeneity in the randomisation unit and perform a separate meta-analysis.
Crossover trials
We did not identify any crossover trials in this topic area. Crossover trials are not an appropriate study design for the intervention considered in this review, and if they are identified in the future, we will exclude them from updates.
Studies including multiple pregnancies
We anticipated that multiple pregnancy was likely to be an exclusion criteria for trials in this area, and if women with multiple pregnancies were included, they were likely to make up only a very small proportion of the trial population. In the included trials, women with multiple pregnancies were excluded. If in the future, we do identify trials including women with multiple pregnancies, we will consider for each review outcome whether the appropriate denominator is the number of babies or the number of women. For most neonatal outcomes, we are aware that babies from multiple pregnancies may be more likely to develop the same outcomes (i.e. non-independence). For analysis of data from trials including multiple pregnancies, we will use methods used to analyse data from cluster-randomised trials and seek the assistance of a statistician.
Dealing with missing data
For included studies, where information was available we have noted levels of attrition. In updates of the review, as more trials are added we will explore the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using sensitivity analysis.
For all outcomes we have carried out analyses, as far as possible, on an intention-to-treat basis: i.e. we have attempted to include all participants randomised to each group in the analyses. The denominator for each outcome in each trial being the number randomised minus any participants whose outcomes are known to be missing.
Assessment of heterogeneity
Where we have pooled data from trials we examined the forest plots from meta-analyses visually to look for any obvious heterogeneity in terms of the size or direction of treatment effect between studies. We examined the I2, T2 and Chi2 statistics to quantify heterogeneity among the trials in each analysis. If we identified moderate or high unexplained heterogeneity (T2 greater than zero and, either I2 greater than 30% or, P = less than 0.1 for the Chi2 test for heterogeneity), we have used a random-effects model if we considered that this was clinically meaningful; we have drawn attention to those outcomes where there are high levels of unexplained heterogeneity and advise caution in the interpretation of results.
Assessment of reporting biases
Where we suspect reporting bias (see ’Selective reporting bias’ above), we attempted to contact study authors asking them to provide missing outcome data. In updates of the review where any missing data are thought to introduce serious bias, we will explore the impact of including such studies in the overall assessment of results by a sensitivity analysis. (In this version of the review, one of the included trials was published in abstract form only and only a small number of results were reported; we have attempted to contact the study author for more information but have had no response.)
If in future updates more trials are included (more than 10), we will explore possible reporting bias by producing funnel plots and visually assessing them for asymmetry.
Data synthesis
We have carried out statistical analysis using the Review Manager software (RevMan 2008). We have used fixed-effect inverse variance meta-analysis for combining data where trials examined the same intervention, and the trials’ populations and methods were judged sufficiently similar. If we suspected clinical or methodological heterogeneity between studies sufficient to suggest that treatment effects may differ between trials, we have used random-effects meta-analysis.
Subgroup analysis and investigation of heterogeneity
We had planned to carry out subgroup analysis for the review’s primary outcomes by:
multiparous versus nulliparous women.
In the included studies separate results by parity were not provided and we were unable to carry out any subgroup analysis. If, in updates of the review, more data become available, for fixed-effect meta-analyses, we will conduct planned subgroup analyses classifying whole trials by interaction tests as described by Deeks 2001. For random-effects meta-analyses, we will assess differences between subgroups by inspection of the subgroups’ confidence intervals; with non-overlapping confidence intervals indicating a statistically significant difference in treatment effect between the subgroups.
Sensitivity analysis
We have included only two trials in this version of the review and have not carried out sensitivity analysis. As more trials become available, in updates of the review, we will explore the impact of removing studies with a high risk of bias (e.g. with poor allocation concealment or with high levels of attrition (greater than 20%)) from the analysis to see whether this changes the size or direction of the treatment effect. We will carry out sensitivity analyses only for the review’s primary outcomes.
RESULTS
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of studies awaiting classification.
Results of the search
The search of the Cochrane Pregnancy and Childbirth Group’s Trials Register found seven reports representing four studies. We have included two trials (Carlan 1993; Ryan 1999) and one is awaiting further assessment (Taghavi 2008). We excluded one study (Jomeen 2002).
Included studies
We have included two studies reporting results for 116 women. One study was carried out in the USA (Carlan 1993) between 1989 and 1991, and the second in Canada in the 1990s (Ryan 1999). Both studies had detailed inclusion criteria and an inpatient surveillance period before randomisation. Women presenting with preterm prelabour rupture of membranes (PPROM) (PROM before 37 weeks’ gestation) underwent 48 to 72 hours of monitoring in hospital before discharge home or routine inpatient management. During monitoring, women were observed for signs of infection or the start of labour, and the wellbeing of the fetus was checked. Both studies had an inclusion criterion relating to the distance women lived from emergency facilities. The Characteristics of included studies tables provide more information on the inclusion and exclusion criteria. In the study by Carlan 1993, all women commenced antibiotic therapy, and in both studies cervical cultures were obtained with subsequent management according to local protocol. The Ryan 1999 study provided very little information on the respective management of women randomised for home versus hospital. In the Carlan 1993 study, women in both groups were encouraged to rest in bed, and fetal movements were recorded daily. Women in both groups were reviewed weekly and those discharged home were advised to contact hospital if there were any signs of labour or decrease in fetal movement.
Excluded studies
We excluded one study as it focused on women with PROM at term rather than before 37 weeks (Jomeen 2002).
Risk of bias in included studies
Allocation
One study provided very little information on study methods (Ryan 1999) and methods used to conceal group allocation were not clear. In the Carlan 1993 study “sealed envelopes” were used to conceal allocation.
Blinding
Blinding women and care providers to group allocation is not feasible with an intervention involving different methods of management. Neither of the included studies provided information on whether or not any outcomes were assessed by blinded investigators.
Incomplete outcome data
Details of sample attrition were not provided; it seems that in both studies all women randomised were accounted for in the analysis, but in neither case were group denominators for all outcomes explicit.
Selective reporting
In one of the included studies, results were not reported in full and we attempted to contact the authors for more information (Ryan 1999).
Other potential sources of bias
One of the included studies was reported in brief abstracts and so we were unable to fully assess risk of bias (Ryan 1999).
Effects of interventions
Home versus hospital management for PPROM: two trials with 116 women
Two randomised controlled trials (Carlan 1993; Ryan 1999), involving 116 women, met our inclusion criteria. Overall, we found insufficient information on the outcomes relevant to the focus of this review, especially on clinical outcomes.
Primary outcomes
One of the included studies reported information on perinatal mortality although it was not clear how this was defined (Carlan 1993). There was no evidence of a statistically significant difference between groups (risk ratio (RR) 1.93, 95% confidence interval (CI) 0.19 to 20.05). This study also provided figures for rates of neonatal pneumonia, and again there was no strong evidence of any difference between groups (RR 0.58, 95% CI 0.15 to 2.19). The second included study reported that there were no significant differences between women managed at home or in hospital in terms of rates of neonatal infection, but did not provide figures. Neither study mentioned maternal mortality or serious maternal morbidity.
Secondary outcomes
Maternal outcomes
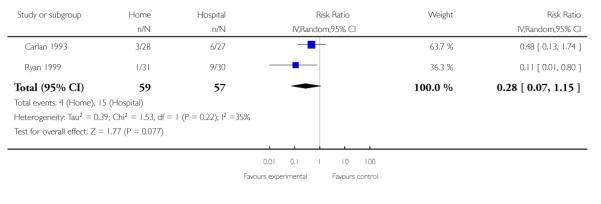
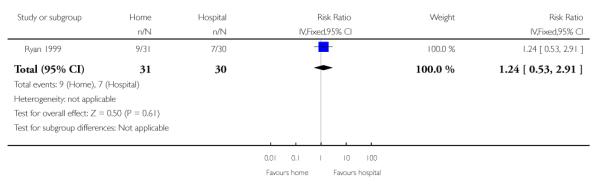
Rates of chorioamnionitis were similar for women in both groups (RR 0.74, 95% CI 0.37 to 1.48). There was some evidence that women managed in hospital were more likely to be delivered by caesarean section although the difference between groups did not reach statistical significance (RR (random-effects) 0.28, 95% CI 0.07 to 1.15, P = 0.08). However, results should be interpreted cautiously as there is moderate heterogeneity for this outcome (heterogeneity: T2 = 0.39, I2 = 35%, Chi2 test for heterogeneity P = 0.22). In the Ryan 1999 study, the number of women undergoing induction of labour was reported, and there was no strong evidence of any difference between groups (Analysis 1.7). Other maternal outcomes including rates of endometritis, postpartum pyrexia or rates of breastfeeding were not reported in either study.
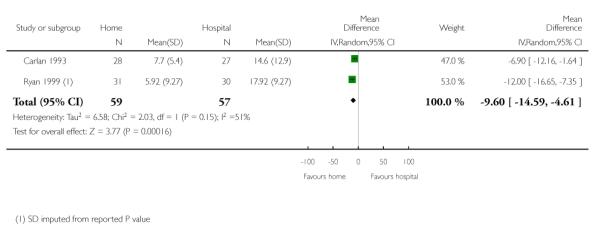
Mothers randomised to care at home were likely to spend less time in hospital. Women randomised to planned home care spent an average of approximately 10 fewer days as inpatients (mean difference (MD) −9.60, 95% CI −14.59 to −4.61 (random-effects)) (heterogeneity: I2 = 51%, T2 = 6.58, Chi2 test for heterogeneity P = 0.15). However, these data should be interpreted with some caution as, while both studies reported means, data may not have been normally distributed, (in one of the studies (Ryan 1999) the standard deviation (SD) was not reported and the values used in the table were imputed from the reported P value; the estimated SDs may not be accurate).
Ryan 1999 reported that more women were more satisfied with home as compared with hospital care (data not shown).
Neonatal outcomes
In the Carlan 1993 study the gestational age at delivery was very similar in both groups (approximately 33 weeks) and there was no evidence of a difference between groups (MD −0.30, 95% CI −2.05 to 1.45). Results in the Ryan 1999 study were not presented in a way in which we could include them in the analysis, but again, it was reported that there was no difference between groups for gestational age at delivery. There was also no significant difference between groups for the latency period (between PPROM and delivery) in either study (outcome data for the Carlan 1993 study are presented in Analysis 1.5; in the Ryan 1999 study results were reported as being not significant).
Rates of respiratory distress syndrome, admissions to neonatal intensive care unit (NICU) and mean birthweight were reported in the Carlan 1993 study, and there was no strong evidence of any differences between groups for any of these outcomes (Analysis 1.9; Analysis 1.10; Analysis 1.11). Data on these outcomes were not reported for the Ryan 1999 study, although the authors state there were no significant differences between groups for five-minute Apgar scores or NICU admissions. Carlan 1993 reports no significant differences between groups for the number of days neonates spent on respirators, the frequency of necrotising enterocolitis, intraventricular haemorrhage, bronchopulmonary dysplasia, and positive neonatal blood culture. In this study three women randomised to the home group delivered in hospitals other than the study hospital, but outcomes for these women and their babies were described as good.
Data were not presented on other neonatal outcomes including cerebral abnormalities and other infant and childhood abnormalities and disabilities.
Costs
The total costs of hospital care were less for those women managed at home. (Again we would advise caution in the interpretation of results in view of some heterogeneity and the imputation of the values for SDs in the Ryan 1999 study.) The total cost of hospital care was less for women managed at home (SMD −0.80, 95% CI −1.41 to −0.19 (random-effects)), (heterogeneity: I2 = 61%, T2 = 0.12, Chi2 test for heterogeneity, P = 0.11). Other costs, including costs to mothers were not reported.
DISCUSSION
The objective of this review was to assess the effects of hospital admission on maternal and neonatal morbidity and mortality, as well as cost implications and maternal satisfaction. The review included only two small randomised trials and in both studies relatively few of the women presenting with PPROM were eligible for inclusion. These two trials addressed many different questions and a broad range of outcomes resulting in limited opportunities to pull any useful data. The paucity of robust studies and reliable information assessing the clinical effects of the intervention make it impossible to balance any benefits or harms of hospital admission for women with preterm prelabour rupture of membranes (PPROM) before 37 weeks’ gestation. Many questions remain open.
The two main arguments against home management for patients with PPROM are the risk of chorioamnionitis and fetal distress. Concerns that planned home management may result in the rise of the rate of chorioamnionitis and shorter latency period (days from PPROM to birth) were not supported by the current review. Irrespective of the intervention used, the rate of chorioamnionitis did not differ between the two groups in the included studies (Carlan 1993; Ryan 1999). Although hospital planned care was not associated with a significant reduction of perinatal mortality, the current rate of chorioamnionitis in the two studies is quite worrying. It is noteworthy that the two trials were presented before the results of the ORACLE trial (Kenyon 2001) became available. The Carlan 1993 study observed no significant difference between the two groups in the frequency of neonatal pneumonia and neonatal positive blood cultures. However, results should be interpreted with caution as the data are from a single trial (Carlan 1993), involving 55 patients, that may not be able to measure differences related to specified outcomes.
Although the incidence of fetal distress in labour in monitored women with PPROM is higher than in pregnancies of equivalent gestational age without premature rupture of membranes, it is nevertheless small (Carlan 1993; Moberg 1984). The higher caesarean section rate among women who had planned hospital care was unexpected. In the Carlan 1993 study the caesarean section rate for fetal distress did not differ between the two groups.
Preterm delivery of infants at home is another limiting factor against the wide use of planned home care among women with PPROM. In the current included two trials, researchers made attempts to include only women who lived within 15 minutes of emergency facilities (Ryan 1999) and women who were resident in the same county (Carlan 1993). There was no significant difference between groups for the latency period (between PPROM and delivery) in either study. The Carlan 1993 study reported delivery in another hospital in three women who were randomised to planned home care. Although the number was small and the outcome was good, results should be taken into consideration in the counselling of women with PPROM. Future randomised controlled trial should address this area.
In the Ryan 1999 trial, women who had planned home care were more likely to be satisfied with their care and had fewer problems. However, it was a small study and authors did not describe the methods used to assess of satisfaction. As there may not be large differences in maternal and neonatal outcomes for planned home versus hospital management, it is vital to have a better understanding of women’s preferences regarding place of care if they have ruptured their membranes.
Investigators in both included studies performed an economic evaluation and found that planned home care was significantly less costly than hospital care. Although the difference in cost may not be an important issue in developed countries, it would have a significant economic impact in developing countries with limited resources.
Summary of main results
The conclusions of this review are limited by the small number of women included in the two trials and rare event rates for important outcomes. For most outcomes including perinatal mortality, neonatal and maternal infection, latency period and neonatal outcomes including birthweight, respiratory distress and admission to the neonatal intensive care unit there was no strong evidence of any differences between groups; clinical outcomes for mothers and babies managed at home and in hospital appear broadly similar. There was some evidence that intervention rates may be increased for women managed in hospital but the evidence was not consistent (caesarean section rates were higher (RR 0.28, 95% CI 0.07 to 1.15) but rates of induction of labour were similar (RR 1.24, 95% CI 0.53 to 2.91)).
The number of days mothers spent in hospital was reduced considerably for the ’home’ group, and this was reflected in reduced costs of care.
Overall completeness and applicability of evidence
We have included only two small studies and in both studies relatively few of the women presenting with PPROM were eligible for inclusion (11% of women with PPROM in the Ryan 1999 study). As we described in the introduction, women who experience PPROM are at risk of premature delivery and their babies are at risk of a wide range of adverse outcomes. It was noted that in both of the current included studies women were observed in hospital for two or three days before randomisation in an attempt to minimise adverse outcomes including those arising from imminent delivery or infection. Authors of both trials emphasise the need for careful selection of women for possible home management; for the majority of women after PPROM hospital management remains the most appropriate choice.
The review suggests that for most clinical outcomes there was no strong evidence of differences between groups. However, there has been very little research in this area and without further trials it is difficult to come to firm conclusions about the relative safety of home or hospital management for women after PPROM (even if women are carefully selected and their condition is stable at the point of randomisation). Conducting trials in this area is difficult. Women and babies after PPROM constitute high risk groups; women may be reluctant to enter trials if they are anxious about their own and their babies’ well being. At the same time, clinicians may be concerned about randomising this potentially vulnerable group.
Quality of the evidence
We have included only two studies in this review, and in one study there was very little information on research methods. Both studies are likely to be at relatively high risk of bias for some outcomes; blinding was not feasible and some outcomes may have been affected by the lack of blinding.
Some outcomes may be difficult to interpret; for example rates of intervention may be higher for women who remain in hospital due to increased monitoring rather than being a real reflection of different health outcomes, i.e. with increased monitoring in hospital, changes that would go undetected in the home group might lead to intervention in the hospital group.
Potential biases in the review process
We attempted to minimise bias in the reviewing process; two review authors (T Dowswell, G El Senoun) independently carried out data extraction and assessed risk of bias.
Agreements and disagreements with other studies or reviews
The evidence from these trials suggests that outcomes are similar for women and babies managed at home or in hospital, although there is some evidence to suggest that women may prefer being at home. Furthermore, the costs to healthcare providers are reduced for women managed at home. We were able to include only two studies; there is a need for further research in this area.
Some studies have urged caution in the care of women after PPROM, particularly as many women will go into labour within a few days (Goldenberg 2008) and many will require treatment for infection.
Planned early birth versus expectant management for women with preterm prelabour rupture of membranes prior to 37 weeks’ gestation for improving pregnancy outcome is currently the focus of a different review (Buchanan 2008). Studies examining planned early birth versus expectant management (waiting) for prelabour rupture of membranes at term (37 weeks or more) are outside the scope of the current review.
AUTHORS’ CONCLUSIONS
Implications for practice
Most women presenting with preterm prelabour rupture of membranes (PPROM) will require hospital management. We do not have sufficient evidence on the safety of home versus hospital management to make recommendations for clinical practice. Despite the lack of difference between the two groups regarding perinatal mortality and frequency of chorioamnionitis, the results should be interpreted with great caution. Despite the use of strict inclusion criteria in the two included studies, the rate of chorioamnionitis was high irrespective of type of intervention used. Furthermore, the gestational age at delivery was around 33 weeks’ gestation.
Implications for research
There is an urgent need for further research in this area. The limited evidence presented in this review suggests that home management may be preferred by women and it is associated with reduced costs for healthcare providers and that would be useful in both developed and developing countries. Future randomised trials should attempt to blind outcomes such as maternal and neonatal infection and to report these outcomes in a standardised way. Outcomes such as maternal satisfaction, maternal and neonatal infectious morbidity, other neonatal morbidities and long-term child development and disability need to be addressed in any future trials. The current model of randomisation after 48 to 72 hours of observation following PPROM would be useful to consider in any future studies as it will give an opportunity to identify high-risk women who may go into labour or develop chorioamnionitis during that period of observation. The relatively small number of women who were eligible for inclusion in the two included studies is striking and future researchers should take that into consideration. The current two studies were conducted before the results of the ORACLE trial (Kenyon 2001) became available and therefore, future work should take the findings of that trial into consideration.
PLAIN LANGUAGE SUMMARY.
Planned home versus hospital care for rupture of the membranes before 37 weeks’ gestation
Premature rupture of membranes before 37 weeks’ gestation (and where there is at least an hour between membrane rupture and the onset of contractions and labour) can have consequences for both the mother and the baby. It is estimated that after premature rupture of the membranes one-half of women go into labour within a week, and three-quarters within a fortnight. This means that the baby may be born prematurely and both mother and baby are at risk of infection. Where available, the majority of clinicians advise hospital care for the women to allow monitoring and early detection of any problems. It is however possible for some women to go home after a period of observation in hospital. The safety, cost and women’s views about home management have not been established.
We included two randomised controlled studies with 116 women in the review. These studies compared planned home versus hospital management for women with preterm, prelabour rupture of the membranes (PPROM). In both studies there were strict criteria for deciding whether women could be included; for example, women had to live within a certain distance of emergency facilities, and there had to be no signs that mothers and babies had infection or other problems. There was a period of monitoring in hospital for women in both groups.
Results suggested that there were few differences in mothers’ and babies’ health for women cared for at home or in hospital including infant death, serious illness, or admission to intensive care baby units.
There was some evidence that women managed in hospital were more likely to be delivered by caesarean section. Women cared for at home were likely to spend less time in hospital (spending approximately 10 fewer days as inpatients) and were more satisfied with their care. In addition, home care was associated with reduced costs. Overall, the number of women included in the two studies was too small to allow adequate assessment of outcomes.
ACKNOWLEDGEMENTS
As part of the pre-publication editorial process, this review has been commented on by three peers (an editor and two referees who are external to the editorial team), a member of the Pregnancy and Childbirth Group’s international panel of consumers and the Group’s Statistical Adviser.
SOURCES OF SUPPORT
Internal sources
The University of Liverpool, UK.
External sources
National Institute for Health Research (NIHR), UK.
TD is supported by the NIHR NHS Cochrane Collaboration Programme grant scheme award for NHS-prioritised centrally-managed, pregnancy and childbirth systematic reviews: CPGS02
CHARACTERISTICS OF STUDIES
Characteristics of included studies [ordered by study ID]
| Methods | RCT. | |
| Participants | Setting: women attending hospital in Florida, USA. (67 women recruited, 55 included in analyses.) Inclusion criteria: women with PPROM < 37 weeks, singleton. Women observed for 72 hrs and labour not started, no signs of infection, amniotic fluid > 2 cm, cephalic presentation, cervical dilatation < 4 cm, resident in the county. Membrane rupture confirmed by positive fern, or pooling tests and decrease of amniotic fluid on ultrasound Exclusion criteria: labour started during 72 hrs surveillance period, membranes resealed and no further leakage within 72 hrs, oligohydramnios, lived outside county, not consented, maternal condition precluded discharge |
|
| Interventions | Women were evaluated before randomisation and cervical cultures obtained. All women commenced antibiotic treatment according to local protocol. If cultures were negative antibiotics were stopped, if positive then treatment according to local protocol. Testing included fetal lungmaturity with offer of steroids for lungmaturation until 34 weeks. No tocolytic drugs were used. Randomisation was carried out after the surveillance period Intervention group: discharge home after surveillance period with daily charting of fetal movements and weekly review. Women were re-admitted if there was evidence of labour or non-reassuring fetal movements Comparison group: routine care in hospital. Both groups were encouraged to rest in bed. Daily recording of fetal movements. NST and blood count, ultrasound and sterile speculum examination weekly. Women were delivered at 37 weeks’ gestation if the cervix was favourable, and all women by 40 weeks |
|
| Outcomes | Perinatal mortality, neonatal infection, maternal chorioamnionitis, latency period, gestational age at birth, respiratory distress syndrome, NICU admission, birthweight, cost of care | |
| Notes | ||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Not described. |
| Allocation concealment? | Unclear | Described as “sealed envelopes”. |
| Incomplete outcome data addressed? All outcomes |
Unclear | 67 women were recruited but randomisation did not occur until after the surveillance period. Leakage stopped and membranes resealed in 10 women. One woman in each group was described as “non compliant”. 55 women included in the analyses |
| Free of selective reporting? | Yes | None apparent. |
| Free of other bias? | Yes | None apparent. |
| Methods | RCT. | |
| Participants | Setting: hospitals in Ontario, Canada. Inclusion criteria: women with PPROM < 37 weeks, singleton viable pregnancy, cephalic presentation, were admitted and observed for 48-72 hrs. They were included if not in labour, no cervical dilation, no evidence of clinical chorioamnionitis, no evidence of meconium, if less than 34 weeks’ gestation then mother must live within 15 min of emergency care facilities, patient able to self-monitor (Only 11% of women attending study hospitals with PPROM were eligible for inclusion.) |
|
| Interventions | 61 women randomised. Intervention group: discharge home after monitoring period. Comparison group: inpatient care. |
|
| Outcomes | Latency period (PPROM to delivery), gestational age at delivery, induction of labour, CS, chorioamnionitis, time in hospital and costs | |
| Notes | Study was reported in brief abstracts; there was little information on methods or on management | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Not described. |
| Allocation concealment? | Unclear | Not described. |
| Incomplete outcome data addressed? All outcomes |
Unclear | Not described. |
| Free of selective reporting? | Unclear | Study reported in a series of brief abstracts. |
CS: caesarean section
hrs: hours
min: minutes
NICU: neonatal intensive care unit
NST: non-stress test
PPROM: preterm prelabour rupture of membranes
RCT: randomised controlled trial
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Jomeen 2002 | This study examined PROM at term; all women included in the study were over 37 weeks’ gestation. The focus of the review is on PPROM |
PPROM: preterm prelabour rupture of membranes
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | RCT (little information on methods, findings reported in a brief abstract) |
| Participants | 60 women attending an Iranian hospital with PPROM between 26 and 32 weeks’ gestation |
| Interventions | All women were observed in hospital for 1 week before randomisation to inpatient or outpatient management |
| Outcomes | Latency period, 5-min Apgar score, NICU admission, neonatal ventilation, neonatal mortality |
| Notes | This study was reported in a brief abstract. Original data were not set out in the results (P values for statistical tests examining differences between groups were provided). We have attempted to contact the authors for more information on study methods and results but have not been successful so far |
NICU: neonatal intensive care unit
PPROM: preterm prelabour rupture of membranes
RCT: randomised controlled trial
DATA AND ANALYSES
Comparison 1.
Planned home versus hospital care after PPROM
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Perinatal mortality (up to 7 days) | 1 | 55 | Risk Ratio (IV, Fixed, 95% CI) | 1.93 [0.19, 20.05] |
| 2 Neonatal infection | 1 | 55 | Risk Ratio (IV, Fixed, 95% CI) | 0.58 [0.15, 2.19] |
| 3 Chorioamnionitis | 2 | 116 | Risk Ratio (IV, Fixed, 95% CI) | 0.74 [0.37, 1.48] |
| 4 Gestational age at birth (weeks) | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | −0.30 [−2.05, 1.45] |
| 5 Latency period (days from PPROM to birth) | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | 6.00 [−3.51, 15.51] |
| 6 Caesarean section rate | 2 | 116 | Risk Ratio (IV, Random, 95% CI) | 0.28 [0.07, 1.15] |
| 7 Induction of labour | 1 | 61 | Risk Ratio (IV, Fixed, 95% CI) | 1.24 [0.53, 2.91] |
| 8 Maternal days in hospital | 2 | 116 | Mean Difference (IV, Random, 95% CI) | −9.60 [−14.59, −4.61] |
| 9 Respiratory distress syndrome | 1 | 55 | Risk Ratio (IV, Fixed, 95% CI) | 0.48 [0.05, 5.01] |
| 10 Mean birthweight (grams) | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | −170.0 [−558.30, 218.30] |
| 11 NICU admission | 1 | 55 | Risk Ratio (IV, Fixed, 95% CI) | 1.39 [0.72, 2.71] |
| 12 Mean total cost (US and Canadian $s) | 2 | 116 | Std. Mean Difference (IV, Random, 95% CI) | −0.80 [−1.41, −0.19] |
Analysis 1.1. Comparison 1 Planned home versus hospital care after PPROM, Outcome 1 Perinatal mortality (up to 7 days)
Review: Planned home versus hospital care for preterm prelabour rupture of the membranes (PPROM) prior to 37 weeks’ gestation
Comparison: 1 Planned home versus hospital care after PPROM
Outcome: 1 Perinatal mortality (up to 7 days)
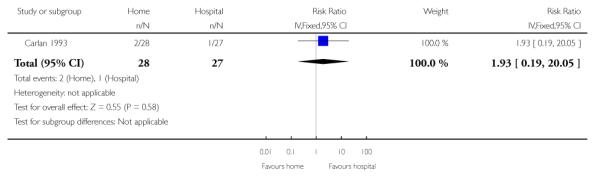 |
Analysis 1.2. Comparison 1 Planned home versus hospital care after PPROM, Outcome 2 Neonatal infection
Review: Planned home versus hospital care for preterm prelabour rupture of the membranes (PPROM) prior to 37 weeks’ gestation
Comparison: 1 Planned home versus hospital care after PPROM
Outcome: 2 Neonatal infection
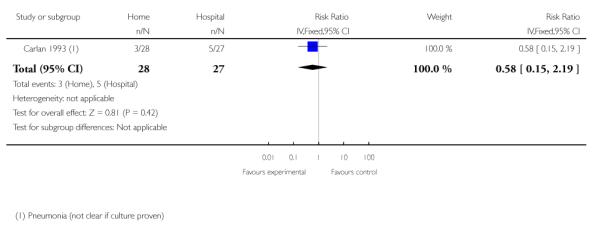 |
Analysis 1.3. Comparison 1 Planned home versus hospital care after PPROM, Outcome 3 Chorioamnionitis
Review: Planned home versus hospital care for preterm prelabour rupture of the membranes (PPROM) prior to 37 weeks’ gestation
Comparison: 1 Planned home versus hospital care after PPROM
Outcome: 3 Chorioamnionitis
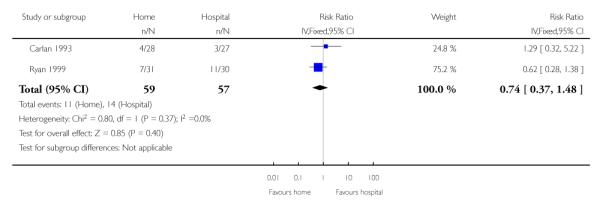 |
Analysis 1.4. Comparison 1 Planned home versus hospital care after PPROM, Outcome 4 Gestational age at birth (weeks)
Review: Planned home versus hospital care for preterm prelabour rupture of the membranes (PPROM) prior to 37 weeks’ gestation
Comparison: 1 Planned home versus hospital care after PPROM
Outcome: 4 Gestational age at birth (weeks)
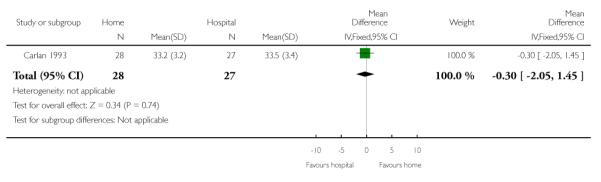 |
Analysis 1.5. Comparison 1 Planned home versus hospital care after PPROM, Outcome 5 Latency period (days from PPROM to birth)
Review: Planned home versus hospital care for preterm prelabour rupture of the membranes (PPROM) prior to 37 weeks’ gestation
Comparison: 1 Planned home versus hospital care after PPROM
Outcome: 5 Latency period (days from PPROM to birth)
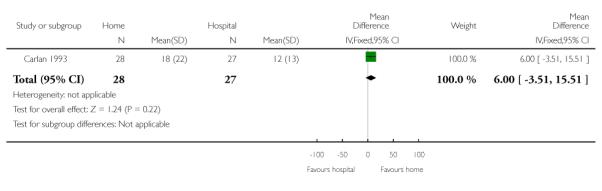 |
Analysis 1.6. Comparison 1 Planned home versus hospital care after PPROM, Outcome 6 Caesarean section rate
Review: Planned home versus hospital care for preterm prelabour rupture of the membranes (PPROM) prior to 37 weeks’ gestation
Comparison: 1 Planned home versus hospital care after PPROM
Outcome: 6 Caesarean section rate
 |
Analysis 1.7. Comparison 1 Planned home versus hospital care after PPROM, Outcome 7 Induction of labour
Review: Planned home versus hospital care for preterm prelabour rupture of the membranes (PPROM) prior to 37 weeks’ gestation
Comparison: 1 Planned home versus hospital care after PPROM
Outcome: 7 Induction of labour
 |
Analysis 1.8. Comparison 1 Planned home versus hospital care after PPROM, Outcome 8 Maternal days in hospital
Review: Planned home versus hospital care for preterm prelabour rupture of the membranes (PPROM) prior to 37 weeks’ gestation
Comparison: 1 Planned home versus hospital care after PPROM
Outcome: 8 Maternal days in hospital
 |
Analysis 1.9. Comparison 1 Planned home versus hospital care after PPROM, Outcome 9 Respiratory distress syndrome
Review: Planned home versus hospital care for preterm prelabour rupture of the membranes (PPROM) prior to 37 weeks’ gestation
Comparison: 1 Planned home versus hospital care after PPROM
Outcome: 9 Respiratory distress syndrome
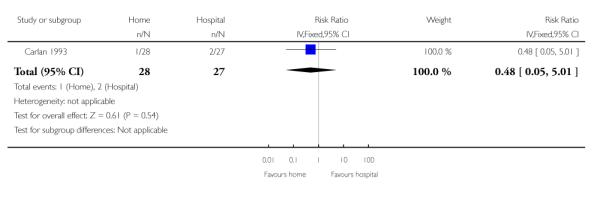 |
Analysis 1.10. Comparison 1 Planned home versus hospital care after PPROM, Outcome 10 Mean birthweight (grams)
Review: Planned home versus hospital care for preterm prelabour rupture of the membranes (PPROM) prior to 37 weeks’ gestation
Comparison: 1 Planned home versus hospital care after PPROM
Outcome: 10 Mean birthweight (grams)
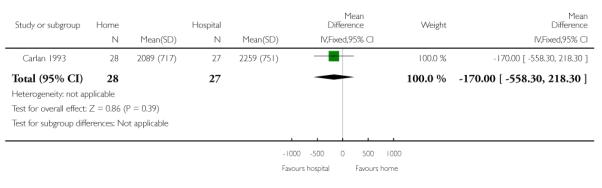 |
Analysis 1.11. Comparison 1 Planned home versus hospital care after PPROM, Outcome 11 NICU admission
Review: Planned home versus hospital care for preterm prelabour rupture of the membranes (PPROM) prior to 37 weeks’ gestation
Comparison: 1 Planned home versus hospital care after PPROM
Outcome: 11 NICU admission
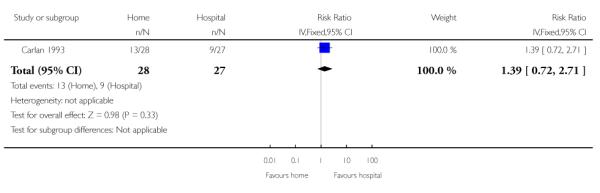 |
Analysis 1.12. Comparison 1 Planned home versus hospital care after PPROM, Outcome 12 Mean total cost (US and Canadian $s)
Review: Planned home versus hospital care for preterm prelabour rupture of the membranes (PPROM) prior to 37 weeks’ gestation
Comparison: 1 Planned home versus hospital care after PPROM
Outcome: 12 Mean total cost (US and Canadian $s)
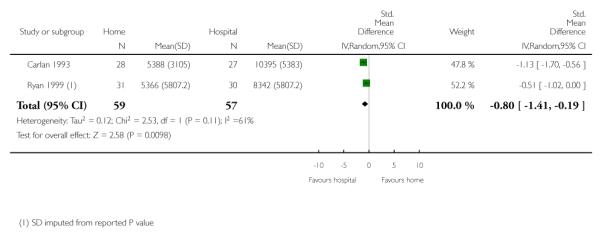 |
DIFFERENCES BETWEEN PROTOCOL AND REVIEW
Updating of methods relating to the assessment of heterogeneity.
HISTORY
Protocol first published: Issue 4, 2009
Review first published: Issue 4, 2010
Footnotes
DECLARATIONS OF INTEREST None known.
References to studies included in this review
- Carlan 1993 {published data only} .Carlan SJ, O’Brien WF, Parsons M, Schorr S, Lense J. Preterm premature rupture of membranes: home vs hospital management. Proceedings of 40th Annual Clinical Meeting of the American College of Obstetricians and Gynecologists; Washington DC, USA. 1992 April.1992. pp. 15–6. [Google Scholar]; Carlan SJ, O’Brien WF, Parsons MT, Lense JJ. Preterm premature rupture of membranes: a randomized study of home vs hospital management. Obstetrics & Gynecology. 1993;81:61–4. [PubMed] [Google Scholar]; Carlan SJ, Parsons M, O’Brien WF, Lense JJ. Preterm PROM: safety and cost of home vs hospital management. American Journal of Obstetrics and Gynecology. 1991;164:311. [PubMed] [Google Scholar]
- Ryan 1999 {published data only} .Oskamp M, Seaward PGR, Farine D, Ryan G, Kelly E, Ritchie JWK. Eligibility criteria for the outpatient management of preterm premature rupture of membranes (PPROM) American Journal of Obstetrics and Gynecology. 1996;Vol. 174(issue 1 Pt 2):344. [Google Scholar]; Ryan G, Gagnon A, Gratton R, Seaward PGR, Windrim R, Lie K, et al. Randomized controlled trial of outpatient vs. inpatient management of PPROM. Society of Obstetricians and Gynaecologists of Canada, 54th Annual Meeting; Victoria, Canada. 1988 June.1998. [Google Scholar]; Ryan G, Oskamp M, Seaward PGR, Kitch T, Barrett J, Brennan B, et al. Randomized controlled trial of inpatient vs outpatient management of PPROM. American Journal of Obstetrics and Gynecology. 1999;180(1 Pt 1):S95. [Google Scholar]
References to studies excluded from this review
- Jomeen 2002 {published data only} .Jomeen J, Martin CR. The impact of clinical management type on maternal and neo-natal outcome following prelabour rupture of membranes at term. Clinical Effectiveness in Nursing. 2002;6:3–9. [Google Scholar]
References to studies awaiting assessment
- Taghavi 2008 {published data only} .Taghavi S, Abam F, Abbasalizadeh SH. Neonatal outcome of preterm premature rupture of membranes: inpatient versus outpatient management. Journal of Maternal-Fetal and Neonatal Medicine. 2008;21(Suppl 1):185. [Google Scholar]
Additional references
- ACOG Committee 2007 .ACOG Committee on Practice Bulletins-Obstetrics ACOG Practice Bulletin No. 80: premature rupture of membranes. Clinical management guidelines for obstetrician-gynecologists. Obstetrics & Gynecology. 2007;109(4):1007–19. doi: 10.1097/01.AOG.0000263888.69178.1f. [DOI] [PubMed] [Google Scholar]
- Ayres 2002 .Ayres AW. Home management of preterm premature rupture of membranes. International Journal of Gynecology & Obstetrics. 2002;78(2):153–5. doi: 10.1016/s0020-7292(02)00064-4. [DOI] [PubMed] [Google Scholar]
- Bartfield 1998 .Bartfield MC, Carlan SJ. The home management of preterm premature ruptured membranes. Clinical Obstetrics and Gynecology. 1998;41(3):503–14. doi: 10.1097/00003081-199809000-00006. [DOI] [PubMed] [Google Scholar]
- Besinger 1993 .Besinger RE. Preterm labor, premature rupture of membranes, and cervical incompetence. Current Opinion in Obstetrics and Gynecology. 1993;5(1):33–9. [PubMed] [Google Scholar]
- Buchanan 2004 .Buchanan S, Crowther C, Morris J. Preterm prelabour rupture of the membranes: a survey of current practice. Australian and New Zealand Journal of Obstetrics and Gynaecology. 2004;44(5):400–3. doi: 10.1111/j.1479-828X.2004.00256.x. [DOI] [PubMed] [Google Scholar]
- Buchanan 2008 .Buchanan SL, Crowther CA, Levett KM, Middleton P, Morris J. Planned early birth versus expectant management for women with preterm prelabour rupture of membranes prior to 37 weeks’ gestation for improving pregnancy outcome. Cochrane Database of Systematic Reviews. 2008;(Issue 2) doi: 10.1002/14651858.CD004735.pub4. [DOI: 10.1002/14651858.CD004735.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowther 2007 .Crowther CA, Harding JE. Repeat doses of prenatal corticosteroids for women at risk of preterm birth for preventing neonatal respiratory disease. Cochrane Database of Systematic Reviews. 2007;(Issue 3) doi: 10.1002/14651858.CD003935.pub2. [DOI: 10.1002/ 14651858.CD003935.pub2] [DOI] [PubMed] [Google Scholar]
- Deeks 2001 .Deeks JJ, Altman DG, Bradburn MJ. Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. In: Egger M, Davey Smith G, Altman DG, editors. Systematic reviews in health care: meta-analysis in context. BMJ Books; London: 2001. [Google Scholar]
- Ellestad 2008 .Ellestad SC, Swamy GK, Sinclair T, James AH, Heine RP, Murtha AP, et al. Preterm premature rupture of membrane management--inpatient versus outpatient: a retrospective review. American Journal of Perinatology. 2008;25(1):69–73. doi: 10.1055/s-2007-1004830. [DOI] [PubMed] [Google Scholar]
- Giles 2005 .Giles M, Garland S, Oats JJ. Management of preterm prelabour rupture of membranes: an audit. How do the results compare with clinical practice guidelines? Australian and New Zealand Journal of Obstetrics and Gynaecology. 2005;45(3):201–6. doi: 10.1111/j.1479-828X.2005.00389.x. [DOI] [PubMed] [Google Scholar]
- Goldenberg 1998 .Goldenberg RL, Rouse DJ. Prevention of premature birth. New England Journal of Medicine. 1998;339(5):313–20. doi: 10.1056/NEJM199807303390506. [DOI] [PubMed] [Google Scholar]
- Goldenberg 2008 .Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371(9606):75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins 2008 .Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1. The Cochrane Collaboration; [updated September 2008]. 2008. Available from www.cochrane-handbook.org. [Google Scholar]
- Hofmeyr 1998 .Hofmeyr GJ. Amnioinfusion for preterm rupture of membranes. Cochrane Database of Systematic Reviews. 1998;(Issue 1) doi: 10.1002/14651858.CD000942. [DOI: 10.1002/14651858.CD000942] [DOI] [PubMed] [Google Scholar]
- Kenyon 2001 .Kenyon SL, Taylor DJ, Tarnow-Mordi W, ORACLE Collaborative Group Broad-spectrum antibiotics for preterm, prelabour rupture of fetal membranes: the ORACLE I randomised trial. ORACLE Collaborative Group. Lancet. 2001;357(9261):979–88. doi: 10.1016/s0140-6736(00)04233-1. [DOI] [PubMed] [Google Scholar]
- Kenyon 2003 .Kenyon S, Boulvain M, Neilson JP. Antibiotics for preterm rupture of membranes. Cochrane Database of Systematic Reviews. 2003;(Issue 2) doi: 10.1002/14651858.CD001058. [DOI: 10.1002/ 14651858.CD001058] [DOI] [PubMed] [Google Scholar]
- Kenyon 2007 .Kenyon S, Ullman R, Mori R, Whittle M. Care of healthy women and their babies during childbirth: summary of NICE guidance. BMJ. 2007;335(7621):667–8. doi: 10.1136/bmj.39322.703380.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis 1996 .Lewis R, Mercer BM. Selected issues in premature rupture of the membranes: herpes, cerclage, twins, tocolysis, and hospitalization. Seminars in Perinatology. 1996;20(5):451–61. doi: 10.1016/s0146-0005(96)80012-7. [DOI] [PubMed] [Google Scholar]
- Lewis 1996b .Lewis DF, Futayyeh S, Towers CV, Asrat T, Edwards MS, Brooks GG. Preterm delivery from 34-37 weeks gestation: Is respiratory distress syndrome a problem? American Journal of Obstetrics and Gynecology. 1996;174(2):525–8. doi: 10.1016/s0002-9378(96)70421-0. [DOI] [PubMed] [Google Scholar]
- Lumley 1991 .Lumley J. Preventing and managing prematurity. International Journal of Technology Assessment in Health Care. 1991;7(4):460–77. doi: 10.1017/s0266462300007030. [DOI] [PubMed] [Google Scholar]
- Medina 2006 .Medina TM, Hill DA, Medina TM, Hill DA. Preterm premature rupture of membranes: diagnosis and management. American Family Physician. 2006;73(4):659–64. [PubMed] [Google Scholar]
- Mercer 2003 .Mercer BM. Preterm premature rupture of the membranes. Obstetrics & Gynecology. 2003;101(1):178–93. doi: 10.1016/s0029-7844(02)02366-9. [DOI] [PubMed] [Google Scholar]
- Mercer 2007 .Mercer BM. Is there a role for tocolytic therapy during conservative management of preterm premature rupture of the membranes? Clinical Obstetrics and Gynecology. 2007;50(2):487–96. doi: 10.1097/GRF.0b013e31804c977d. [DOI] [PubMed] [Google Scholar]
- Mingione 2006 .Mingione MJ, Pressman EK, Woods JR. Prevention of PPROM: current and future strategies. Journal of Maternal-Fetal & Neonatal Medicine. 2006;19(12):783–9. doi: 10.1080/14767050600967797. [DOI] [PubMed] [Google Scholar]
- Moberg 1984 .Moberg LJ, Garite TJ, Freeman RK. Fetal heart rate patterns and fetal distress in patients with preterm premature rupture of membranes. Obstetrics & Gynecology. 1984;64(1):60–4. [PubMed] [Google Scholar]
- Neerhof 1999 .Neerhof MG, Cravello C, Haney EI, Silver RK. Timing of labor induction after premature rupture of membranes between 32 and 36 weeks’ gestation. American Journal of Obstetrics and Gynecology. 1999;180(2):349–52. doi: 10.1016/s0002-9378(99)70212-7. [DOI] [PubMed] [Google Scholar]
- Neufeld 2005 .Neufeld MD, Frigon C, Graham AS, Mueller BA. Maternal infection and risk of cerebral palsy in term and preterm infants. Journal of Perinatology. 2005;25(2):108–13. doi: 10.1038/sj.jp.7211219. [DOI] [PubMed] [Google Scholar]
- Obi 2007 .Obi SN, Ozumba BC. Pre-term premature rupture of fetal membranes: the dilemma of management in a developing nation. Journal of Obstetrics and Gynaecology. 2007;27(1):37–40. doi: 10.1080/01443610601016875. [DOI] [PubMed] [Google Scholar]
- Ramsey 2004 .Ramsey PS, Nuthalapaty FS, Lu G, Ramin S, Nuthalapaty ES, Ramin KD. Contemporary management of preterm premature rupture of membranes (PPROM): a survey of maternal-fetal medicine providers. American Journal of Obstetrics and Gynecology. 2004;191(4):1497–502. doi: 10.1016/j.ajog.2004.08.005. [DOI] [PubMed] [Google Scholar]
- RevMan 2008 .The Nordic Cochrane Centre . The Cochrane Collaboration. Review Manager (RevMan). 5.0. The Nordic Cochrane Centre, The Cochrane Collaboration; Copenhagen: 2008. [Google Scholar]
- Roberts 2006 .Roberts D, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database of Systematic Reviews. 2006;(Issue 3) doi: 10.1002/14651858.CD004454.pub2. [DOI: 10.1002/14651858.CD004454.pub2] [DOI] [PubMed] [Google Scholar]
- Ronnestad 2005 .Ronnestad A, Abrahamsen TG, Medbo S, Reigstad H, Lossius K, Kaaresen PI, et al. Septicemia in the first week of life in a Norwegian national cohort of extremely premature infants. Pediatrics. 2005;115(3):e262–e268. doi: 10.1542/peds.2004-1834. [DOI] [PubMed] [Google Scholar]
- Seibel-Seamon 2008 .Seibel-Seamon J, Berghella V, Baxter J, Grimes-Dennis J. Tocolytics for preterm premature rupture of membranes. Cochrane Database of Systematic Reviews. 2008;(Issue 2) doi: 10.1002/14651858.CD007062.pub2. [DOI: 10.1002/14651858.CD007062] [DOI] [PubMed] [Google Scholar]
- Simhan 2005 .Simhan HN, Canavan TP. Preterm premature rupture of membranes: diagnosis, evaluation and management strategies. BJOG: an international journal of obstetrics and gynaecology. 2005;112(Suppl 1):32–7. doi: 10.1111/j.1471-0528.2005.00582.x. [DOI] [PubMed] [Google Scholar]
- Woldesenbet 2005 .Woldesenbet M, Perlman JM. Histologic chorioamnionitis: an occult marker of severe pulmonary hypertension in the term newborn. Journal of Perinatology. 2005;25(3):189–92. doi: 10.1038/sj.jp.7211240. [DOI] [PubMed] [Google Scholar]
- * Indicates the major publication for the study


