Abstract
Objective
To describe a 10-year proof-of-concept smoking cessation research program evaluating the reach of online health interventions throughout the Americas.
Methods
Recruitment occurred from 2002–2011, primarily using Google.com AdWords. Over 6 million smokers from the Americas entered keywords related to smoking cessation; 57 882 smokers (15 912 English speakers and 41 970 Spanish speakers) were recruited into online self-help automated intervention studies. To examine disparities in utilization of methods to quit smoking, cessation aids used by English speakers and Spanish speakers were compared. To determine whether online interventions reduce disparities, abstinence rates were also compared. Finally, the reach of the intervention was illustrated for three large Spanish-speaking countries of the Americas—Argentina, Mexico, and Peru—and the United States of America.
Results
Few participants had utilized other methods to stop smoking before coming to the Internet site; most reported using no previous smoking cessation aids: 69.2% of Spanish speakers versus 51.8% of English speakers (P < 0.01). The most used method was nicotine gum, 13.9%. Nicotine dependence levels were similar to those reported for in-person smoking cessation trials. Overall observed quit rate for English speakers was 38.1% and for Spanish speakers, 37.0%; quit rates in which participants with missing data were considered to be smoking were 11.1% and 10.6%, respectively. Neither comparison was significantly different.
Conclusions
The systematic use of evidence-based Internet interventions for health problems could have a broad impact throughout the Americas, at little or no cost to individuals or to ministries of health.
Keywords: Internet, smoking cessation, outcome assessment (health care), healthcare disparities, Latin America
Tobacco-related deaths will soon be responsible for 10% of all deaths worldwide, making smoking the leading cause of preventable death in the world (1). The World Health Organization (WHO) released a report stating that, “Unless urgent action is taken, tobacco could kill 1 billion people during this century” (2). These losses would be particularly striking among low- and middle-income countries where 80% of smokers reside (3). Prevalence of smoking in Latin American countries is as high as 40.5% among adults and 37.9% among youths (4). One study of five cities in Latin America (5) found smoking rates among adults 40 years of age and older to be as high as 38.5% (in Santiago, Chile). In Mexico, Uruguay, and Venezuela rates were found to be 25.4%, 28%, and 28.5%, respectively (5). Tobacco use in Spanish-speaking countries is a problem that warrants increased action focused on improving access to and utilization of smoking cessation interventions.
In Latin America, the number of smokers expressing a desire to quit is large; for example, 73.6% of smokers in Argentina, 72.1% in Mexico, and 75.7% in Uruguay. Among those that have attempted to quit, up to 89.9% have attempted to do so without any kind of aid (6). Although many smoking cessation aids are available, they are rarely used among Spanish-speaking populations, perhaps due to cost (not typically reimbursed by public insurance plans) or to a general mistrust of pharmaceuticals (7–9).
Studies confirm that there are disparities between English speakers and Spanish speakers regarding the use of smoking cessation tools; for example, Spanish speakers have significantly lower rates of nicotine gum, patch, inhaler, and/or spray usage (10, 11). This could be due to difficulties with access to tobacco health aids in Latin America (9).
At the same time, the almost exclusive use of consumable health interventions—those that get used up when delivered, e.g., a nicotine patch that gets discarded or time spent by a provider with one patient that can never benefit another—severely limits the ability of public health efforts to reach adequate numbers of individuals throughout the Americas. To reduce health disparities, the health care system must develop, test, and disseminate interventions that can be used repeatedly without losing their therapeutic power; ones that can reach users directly without having to rely on complex and costly service delivery processes that are often difficult to implement and sustain; and ones that can be used simultaneously by many people, anytime and anywhere, without having to travel to distant clinics at specific times and compete for attention with others in need. Mass delivery of scalable health services throughout the Region of the Americas could be greatly accelerated via the use of information and communication technologies (ICTs). Unfortunately, current articles providing recommendations on how to augment smoking cessation interventions do not mention digital health promotion as a potential tool for population-based approaches to smoking cessation (9, 12).
This study reports on the experiences of a small Latino team in San Francisco, California, United States, that developed and tested a stop-smoking Internet site originally intended to serve Latino smokers in California, but that was utilized by Spanish speakers throughout the world over a 10-year period. This work is presented as proof of concept that online evidence-based behavioral health interventions (i) can be tested in randomized controlled trials (RCTs); (ii) can yield outcomes comparable to traditional interventions; and (iii) can be disseminated widely, at no or minimal cost to national health ministries and users. Although this work targeted smoking cessation, the authors believe that self-help internet-based interventions can address other health problems too, such as depression, obesity, and high-risk alcohol use and other drug problems.
The work reported here was started in 1985 by Pérez-Stable and colleagues with funding from the National Cancer Institute (Bethesda, Maryland, United States), who developed, implemented, and evaluated smoking cessation interventions for Spanish-speaking Latinos in the San Francisco Bay Area. They developed and tested a printed smoking cessation guide, Guía para dejar de fumar (Stop Smoking Guide), that yielded substantial quit rates in outcome studies (13) and in a community-based intervention (14, 15). Muñoz, Pérez-Stable, and colleagues then applied for funds to provide similar interventions via the Internet. The California Tobacco-Related Disease Research Program (University of California, Office of the President, Oakland, California, United States) provided 10 years of funding to carry out the studies described below. Although the target population was Spanish-speaking Latino smokers, the team decided to launch the site in English and Spanish in order to reach English-speaking Latinos in California, and as an added bonus, English-speaking non-Latinos as well.
The present report reviews the results of a 10-year worldwide research program reaching Spanish-speaking smokers online, and discusses the implications of this program for other health interventions.
MATERIALS AND METHODS
From 1998–2012, a team at the University of California, San Francisco, Department of Psychiatry at San Francisco General Hospital conducted several online smoking cessation studies in Spanish and English. The data considered by the present report was collected in 2002–2011. The Internet trials were inspired by a randomized control trial conducted entirely via surface mail (16). In that study, the authors recruited Spanish-speaking smokers in San Francisco to a randomized control trial that compared the printed smoking cessation guide, Guía para dejar de fumar, to the same guide plus a mood management intervention called Tomando control de su vida (Taking Control of Your Life)(16). These studies were designated the TC studies for “Tomando Control.” The study that used the printed material was named TC1. The online studies reported here were designated TC2, TC3, and TC4. All four studies were approved by the University of California, San Francisco Institutional Review Board, Committee on Human Research.
Recruitment
The methods of recruitment and the inclusion criteria varied by study. In the earliest online trial, TC2 (17), Spanish and English-speaking participants were recruited via list serve announcements, registration with commonly used search engines (e.g., Yahoo.com) and a direct e-mail sent from WebMD.com. Participants were deemed eligible if they reported smoking 1 or more cigarettes per day, using email at least once per week, were planning to quit within the next 3 months, and were at least 18 years of age (18).
A Google.com AdWords campaign was employed in TC3 (10, 19) and TC4 (11) as the primary recruiting mechanism. A grant from Google Inc. (Mountain View, California, United States) allowed the placement of bids for ad space that appeared among Google search results following smoking cessation-related queries. When potential participants visited one of the sponsored links, they were directed to either the English or Spanish version of the website (www.stopsmoking.ucsf.edu or www.dejardefumar.ucsf.edu) according to the language of the search term used (11). For the TC3 study, eligibility criteria were being ≥ 18 years of age, smoking ≥ 5 cigarettes/day, using email at least once weekly, and intending to quit in the next month. For the TC4 study, the only eligibility criterion was being over 18 years of age.
Study procedures
In the TC2 study, four distinct trials were conducted. The first and second trials were exploratory studies that tested the smoking cessation guide using a one-condition design. The first trial was conducted with English speakers and the second, with Spanish speakers. Trials 3 and 4, which also differed only by language, were randomized trials comparing the smoking cessation guide plus individually timed educational messages (ITEMS), to the guide plus ITEMs and a Mood Management (MM) intervention (20). ITEMs consisted of email messages sent to participants that were designed to increase the likelihood that participants would return to the website by providing encouragement, and links to relevant intervention elements. Follow-ups for trials 1 and 2 were done at 1 and 6 months, whereas trials 3 and 4 had follow-ups at 1, 3, 6, and 12 months (17, 18).
In the TC3 studies, participants were randomized into one of four intervention conditions, each of which augmented the prior condition with an additional intervention element. Condition 1 solely used the smoking cessation guide (13, 16); Condition 2 added ITEMs to the smoking cessation guide; Condition 3 added the MM intervention to the elements present in Condition 2; and finally, Condition 4 added a “virtual group” (a bulletin board for mutual support and suggestions) to the guide, ITEMs, and MM (10). Follow-up assessments were conducted at 1, 3, 6, and 12 months after enrollment. The first 500 Spanish-speaking and the first 500 English-speaking participants were followed up by telephone if they did not complete the follow-ups online. Thus, the follow-up data for these 1 000 participants is the most complete.
The TC4 study was a participant preference trial (11). Participants were presented with a choice of nine intervention elements: (i) a Pre-quit Checklist; (ii) the Stop Smoking Guide; (iii) a nicotine replacement therapy guide; (iv) an electronic version of Taking Control of Your Life materials; (v) individually timed email messages; (vi) an 8-session MM intervention; (vii) a virtual group; (viii) a personal journal; and (ix) a daily cigarette counter. Participants could select any combination of these elements. An individualized homepage contained a navigation bar with only the selected elements. Participants could access these elements throughout the 12-month study. Similar to TC3, participants received emails to complete follow-up assessments at 1, 3, 6, and 12 months after enrolling in the study.
Measures
The first stage of data collection came from information provided by Google. Recruitment via the Google search engine involves a bidding process in which the higher bidder’s ad is placed higher on the search results page. Each ad is called an “impression.” Impressions appear on a user’s screen in response to the user entering a relevant keyword. The search engine reports the number of Internet users who entered keywords related to each ad shown and were provided an “impression,” i.e., shown an ad. A “visit” was defined as a user clicking on the ad to visit the site. Google AdWords began reporting impressions on 17 September 2003; and Google Analytics began reporting impressions and visits by subnational geographic divisions on 26 May 2006. Presented here are the Google reports on number of impressions throughout the Americas and the number of visits by Spanish-speaking users in four selected countries.
After participants entered the website and provided informed consent, a demographic questionnaire was administered to collect age, gender, race/ethnicity, education, income, and marital status. A smoking questionnaire requested age when the person started smoking, age when smoking regularly, number of cigarettes per day, confidence in quitting, smoking exposure, and smoking cessation methods used. The Fagerström Test for Nicotine Dependence (FTND, 21) is a commonly used 6-item test of nicotine dependence, with a range of 0–10.
Self-reported 7-day point prevalence abstinence was defined as a “no” response to “Have you smoked 1 or more cigarettes in the last 7 days?” at 1-, 3-, 6-, and 12-month follow-ups. This is the main measure used in the previously published RCTs (10, 17). Observed quit rates were based solely on participants who completed follow-up measures. Missing = smoking rates assigned participants with missed follow-ups to the smoking category.
Data analysis
Table 1 presents major demographic characteristics of Spanish-speaking participants from all over the world. Table 2 presents rates for utilization of smoking cessation aids prior to entry into these studies. Chi-square tests were used to test the differences in utilization of smoking cessation aids between English-speaking and Spanish-speaking participants. Independent t-tests were used to determine whether the FTND scores are comparable between the two language groups. In addition, chi-square tests were also used to compare the observed and missing = smoking quit rates between English-speaking and Spanish-speaking participants. Data analyses were conducted using IBM SPSS Statistics software, version 20 (SPSS Inc., an IBM company, Chicago, Illinois, United States).
TABLE 1.
Demographic characteristics for Spanish-speaking participants who completed a baseline assessment in three Internet smoking cessation studies (TC2, TC3, TC4), 2002–2011
| Variable | TC2 (2002–2005) | TC3 (2005–2008) | TC4 (2008–2011) |
|---|---|---|---|
| n = 4 904 | n = 14 887 | n = 11 512 | |
| % | % | % | |
| Age (years) | |||
| Mean (Standard deviation) | 34.9 (9.7) | 35.6 (10.5) | 35.7 (10.6) |
| Sex | |||
| Men | 55.2 | 55.8 | 51.4 |
| Women | 44.7 | 44.2 | 48.6 |
| Education | |||
| ≤ 6 years | 0.3 | 2.6 | 2.0 |
| 7 – 11 years | 2.1 | 3.1 | 2.8 |
| High school degree | 20.3 | 18.6 | 20.9 |
| Some college | 24.4 | 37.6 | 39.3 |
| Bachelor degree | 35.7 | 27.5 | 26.6 |
| Graduate degree | 17.2 | 10.6 | 8.3 |
| Marital status | |||
| Single | 36.6 | 34.3 | 32.9 |
| Married | 42.1 | 36.9 | 36.5 |
| Separated | 4.9 | 5.7 | 5.1 |
| Divorced | 4.2 | 6.5 | 5.9 |
| Widowed | 0.8 | 0.8 | 0.9 |
| Living with significant other | 11.4 | 15.8 | 18.7 |
| Ethnicity | |||
| Hispanic/Latino | NA | 93.8 | 93.3 |
| Race | |||
| Asian descent | 0.3 | 0.4 | 0.2 |
| Indigenous descent | 0.0 | 0.2 | 0.4 |
| European/white | 58.6 | 67.7 | 67.9 |
| African descent | 0.2 | 0.3 | 0.1 |
| Latino | 37.9 | See above | See above |
| More than one race | 1.0 | 2.9 | 1.6 |
| Mestizo | NA | 21.5 | 13.6 |
| Other | 2.1 | 7.0 | 16.2 |
TABLE 2.
Utilization of other smoking cessation aids before entering an online smoking intervention website among participants worldwide, 2002–2011
| All participants (n = 52 435)
|
English (No. = 13 876)
|
Spanish (No. = 38 559)
|
P value | |
|---|---|---|---|---|
| % | % | % | ||
| Methods used to quit in last 6 months | ||||
| Nicotine gum | 13.9 | 18.7 | 12.1 | < 0.01 |
| Nicotine patch | 10.8 | 19.5 | 7.7 | < 0.01 |
| Nicotine inhaler | 1.3 | 3.0 | 0.7 | < 0.01 |
| Nicotine spray | 0.2 | 0.5 | 0.1 | < 0.01 |
| Bupropion | 4.7 | 7.9 | 3.5 | < 0.01 |
| Other antidepressant | 1.5 | 1.4 | 1.5 | 0.78 |
| Stop smoking group | 1.8 | 2.1 | 1.7 | < 0.01 |
| Hypnosis | 2.2 | 4.9 | 1.3 | < 0.01 |
| Acupuncture | 2.0 | 2.0 | 2.1 | 0.68 |
| Motivational tapes | 2.3 | 4.4 | 1.5 | < 0.01 |
| Other self-help | 4.3 | 5.6 | 3.8 | < 0.01 |
| Other websites | 2.6 | 3.4 | 2.4 | < 0.01 |
| Other | 8.0 | 9.7 | 7.4 | < 0.01 |
| None | 64.6 | 51.8 | 69.2 | < 0.01 |
Source: Baseline survey from San Francisco Stop-Smoking website (http://www.dejardefumar.ucsf.edu).
RESULTS
Sample characteristics
From 2002–2011, a total of 41 970 Spanish-speaking participants provided consent and completed baseline assessment. For the Spanish-speaking participants, over 90% identified themselves as Latino/Hispanic and about 95% reported having at least a high school diploma. The basic demographics of participants from all TC studies were relatively similar (Table 1).
Interest in online smoking cessation resources
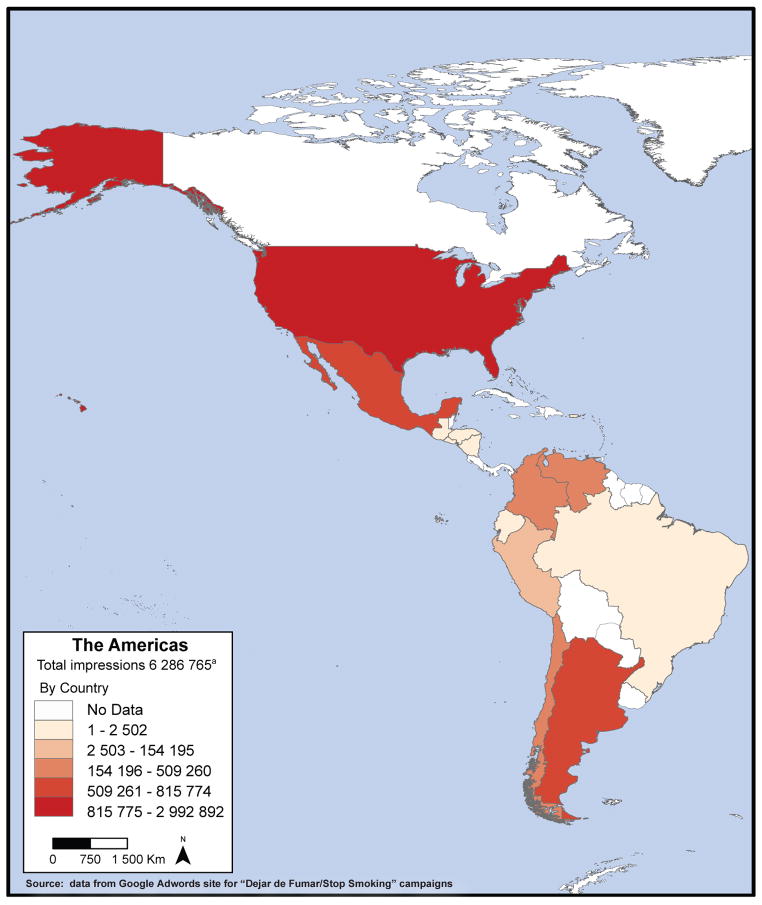
From 2003–2011, Google AdWords recorded a total of 21 201 331 impressions for this stop-smoking intervention. Among those, 6 286 765 impressions were shown to be from Spanish speakers from the Americas (Figure 1). Furthermore, there were a total of 735 458 visits that resulted from the ads and 312 722 visits from Spanish-speaking smokers in the Americas. Since the studies reported here started recruiting individuals using AdWords in September 2003, the numbers of visits and impressions are only available for 8 years. Of those who entered the stopsmoking.ucsf.edu/dejardefumar.ucsf.edu site from 2002–2011, a total of 54 968 consented to participate in the online smoking cessation studies—15 912 English speakers and 41 970 Spanish speakers (including 15 025 participants from Spain and 26 945 from the Americas). Of those who consented, 11 158 English speakers and 18 593 Spanish speakers from the Americas completed baseline assessments.
FIGURE 1.
Number of impressions (Google AdWords) triggered by people searching for smoking cessation information in English and Spanish throughout the Americas (2003–2011)
a A total of 338 916 impressions came from nonspecified Latin American countries; countries with no data were not specifically targeted by Google AdWords campaigns.
As an added bonus, the effort reached Spanish-speaking smokers in Spain, evidenced by the 2 531 926 impressions and 139 151 visits from Spanish users. In addition, 11 872 Spanish users consented and completed the baseline survey.
Nicotine dependence in the online sample
FTND was used to measure participants’ nicotine dependence at baseline. A total of 12 785 English-speaking and 36 489 Spanish speaking participants (including those from Spain) completed the FTND measure. On the 10-point scale, both groups reported a mean FTND score of 5.8, which fell in the medium range. English-speaking and Spanish-speaking participants had a comparable level of nicotine dependence before using the online intervention (t = 1.29, P > 0.05).
Utilization of other smoking cessation methods
Table 2 presents utilization rates of smoking cessation aids by language. Chi-square tests showed that 69.2% of Spanish-speaking smokers reported never having tried other methods to quit smoking, compared to 51.8% of English-speaking smokers (P < 0.01). In addition, Spanish-speaking smokers consistently reported lower percentages of using specific methods to quit smoking, compared to English smokers. For example, compared to 19.5% of English-speaking smokers, only 7.7% of Spanish-speaking smokers reported trying the nicotine patch before entering this study.
7-day abstinence rates at 1 month
A total of 9 875 (31%) Spanish- speaking smokers and 3 579 (32%) English-speaking smokers answered the 7-day abstinence question at 1 month. Among those who provided this data, 37% of Spanish-speaking smokers reported quitting smoking for at least 7 days, while 38% of English-speaking smokers reported doing so (χ2 = 1.30, P > 0.05) (Table 3). In addition, there were no significant differences on the missing = smoking quit rate between the two language groups, with the Spanish-speaking smokers reporting a 10.6% quit rate and English-speaking smokers an 11.1% quit rate (χ2 = 2.62, P > 0.05).
TABLE 3.
Seven-day abstinence rate for English-speaking and Spanish-speaking participants in Internet smoking cessation studies at 1-month follow-up, 2002–2011
| All participants | English-speaking | Spanish-speaking | χ2 | P value | |
|---|---|---|---|---|---|
| Total individuals who received follow-up emails | 43 965 | 11 742 | 32 222 | ||
| Observed quit ratea | 37.3% | 38.1% | 37.0% | 1.30 | 0.26 |
| Missing = smokingb | 10.7% | 11.1% | 10.6% | 2.62 | 0.11 |
Source: 1-month follow-up survey from San Francisco Stop-Smoking website (http://www.dejardefumar.ucsf.edu).
Number reporting being abstinent/number providing data.
Number reporting being abstinent/total number of people receiving follow-up emails.
DISCUSSION
There is a substantial amount of interest in online interventions by Spanish-speaking users. Over 6 million Spanish speakers from the Americas entered search terms, over 735 000 visited the dejardefumar.ucsf.edu site, and 41 970 consented to participate in a smoking cessation study online. Note that all who clicked on the ads and landed on the home page were able to immediately download the Guía para dejar de fumar (Stop Smoking Guide), without entering any further data. Printing and mailing over 735 000 smoking cessation guides (the number of visits recorded by Google Ads) would have been very costly.
In this study, participants reported a level of nicotine dependence (FTND mean = 5.8) comparable to participants recruited for face-to-face smoking cessation RCTs (16, 17). This suggests that online interventions are not recruiting less-addicted smokers, and thus alternative content needs to be developed to target Spanish-speaking current smokers who are very light or not daily smokers.
Baseline assessment measures indicate that most smokers accessing online smoking cessation sites have not used any other method to stop smoking previously. Moreover, Spanish speakers are significantly less likely to have done so than English speakers. This suggests that there are disparities among these two groups in terms of utilization of traditional methods to quit smoking. However, Spanish and English speakers are as likely to quit smoking using the stopsmoking.ucsf.edu/dejardefu-mar.ucsf.edu site. Moreover, missing = smoking 12-month quit rates (20.2% for Spanish speakers and 21.0% for English speakers) obtained in the study with the most strict follow-up methods, that is, TC3 (10) are comparable to quit rates for traditional methods. For example, 6-month quit rates found in RCTs testing the nicotine patch or smoking cessation groups range from 14%–27% (12, 22, 23). The fact that online interventions achieve outcomes very similar to traditional smoking cessation methods, and that they are as effective for English- and Spanish-speakers, suggests that online behavioral health interventions are potentially able to reduce health disparities across large world regions.
Study limitations
An important limitation of this study was that individuals reporting lower levels of education were less likely to use the website; however, about 5% of participants reported less than a high school degree, so some were reached. Future studies should consider creating sites that do not require reading, perhaps using primarily audio and video interventions. In addition, future digital interventions should focus on using media that are widely available, such as mobile devices. Mobile devices have achieved a very high level of penetration, even in very low-income communities.
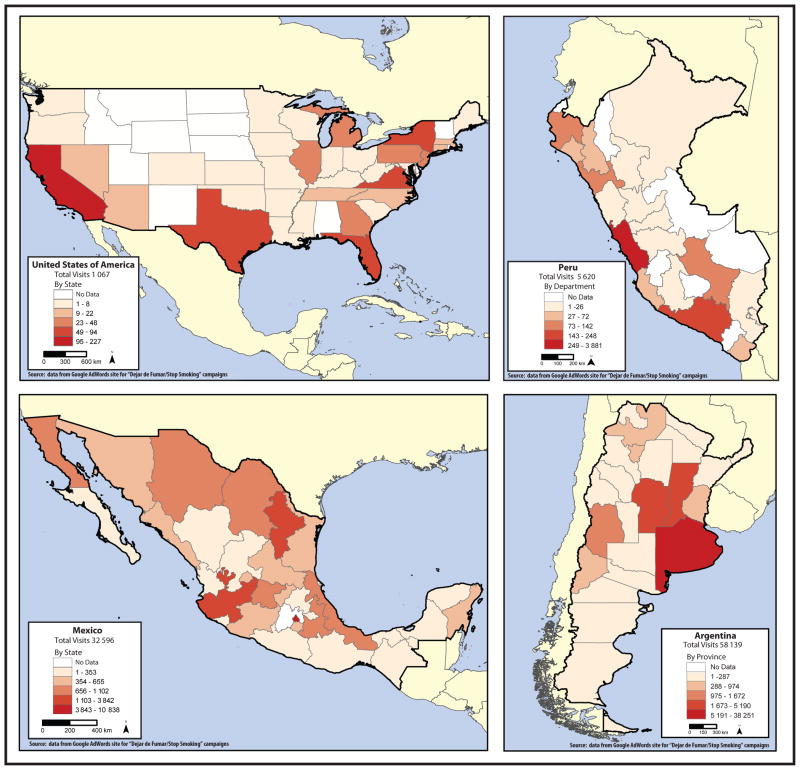
Conclusions
It is notable that the online interventions reported here were created and managed by a small team of Spanish-speaking professionals based at the San Francisco General Hospital, a public sector teaching hospital. With the help of a grant from Google Inc. to present ads on their search engine, this program was able to reach literally millions of people throughout the world. Although the resources were not available to systematically contact the ministries of health of each country in the Americas, this stop-smoking program was able to penetrate remote areas of each (Figure 2).
FIGURE 2.
Number of Spanish speakers who clicked Google AdWords to visit the stop smoking website, four selected countries in the Americas, 2006–2011
It is strongly recommended that the Ministry of Health in every country in the Americas collaborate with an Internet intervention team such as the one described here to widely disseminate the links to these evidence-based interventions. For example, if every pack of cigarettes included the URL to stopsmoking. ucsf.edu/dejardefumar.ucsf.edu, even more smokers could be reached, at no cost to the smoker and at no additional cost to the Ministry of Health. In addition, Spanish-speaking countries could selected countries in the Americas, 2006–2011 collaborate to create and evaluate a state-of-the-science stop-smoking website that could serve Spanish-speaking smokers worldwide. Once a universal stop-smoking site were launched, countries that have the resources to do so could adapt it to their own populations, including linguistic and cultural nuances, as well as native languages spoken by certain segments of their populations.
This proof-of-concept study could be generalized to other health issues that can be targeted with behavioral interventions, issues such as alcohol and drug addiction, obesity and exercise, and even, dizziness. Indeed, several mental health disorders, such as depression (24) and anxiety, are currently being successfully addressed through behavioral Internet interventions with similar outcomes to those of face-to face interventions (25).
Self-help, automated Internet interventions and mobile-based apps could serve as a basic level of health resource in areas that have few or no health care providers. These digital health tools can be developed and tested with participants from around the globe, and thereby generalized to international populations. Digital tools proven effective for their target health problems can become part of recognized evidence-based prevention and treatment interventions. Dissemination then becomes relatively inexpensive, requiring only that the website continue to operate, or that the app remain available in the online store. Individuals worldwide would be able to access them at any time and any place of their choosing, ideally at no charge to them.
In communities that have adequate health care providers, such digital tools could be adjuncts to traditional care, and be tested to see whether they increase effectiveness. This line of research would have as a goal the systematic filling in of a grid consisting of columns depicting health problems and rows depicting languages. As more of the cells in this grid are filled, more and more health care disparities would be reduced. For a more detailed description of this initiative, see “Using Evidence-Based Internet Interventions to Reduce Health Disparities Worldwide” (26). Systematic efforts to provide universal access to evidence-based non-consumable interventions, such as these, could have a major impact on health among the populations of the Western Hemisphere and beyond.
Acknowledgments
The authors thank the Tobacco-Related Disease Research Program (University of California, Office of the President, Oakland, California, United States) for funding to develop the website (stopsmoking.ucsf.edu/dejardefumar.ucsf.edu) and conduct the outcome studies. The authors also thank Nancy Adler, Director of the Center for Health and Community (University of California, San Francisco, San Francisco, California, United States ), for providing office space and additional resources to target Latino smokers, and Leslie Lenert for major contributions to the development of the initial website. Special thanks to Google, Inc., for the AdWords grant that gave the researchers the ability to recruit smokers worldwide using Google-sponsored links.
The researchers, E. J. Pérez-Stable and R. F. Muñoz, were partly supported by a grant (No. TW05935) from the Tobacco Research Network Program, Fogarty International Center, National Cancer Institute, National Institute of Drug Abuse, National Institutes of Health (Bethesda, Maryland, United States). Thanks also to the Information Services Unit of the University of California (UC) at San Francisco, which hosted the site, and to the UC Office of the President and the Brin Wojcicki Foundation, which provided invaluable additional support once the research grants ended. Finally, the authors want to thank the following staff and collaborators: Carlos Penilla, Veronica Pitbladdo, Omar Contreras, Tom Manley, Alinne Barrera, Leandro Torres, Adrian Aguilera, and Stephen Schueller, and Yan Leykin.
Footnotes
Conflicts of interest. None.
References
- 1.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. [Accessed on 13 May 2014];WHO report on the global tobacco epidemic. 2008 Available from: www.who.int/tobacco/mpower/mpower_report_full_2008.pdf.
- 3.World Health Organization. [Accessed on 13 May 2014];Tobacco fact sheet. 2013 :339. Available from: www.who.int/mediacentre/factsheets/fs339/en/
- 4.Mackay J, Ericksen M. The tobacco atlas. World Health Organization; 2010. [Accessed on 13 May 2014]. Available from: www.who.int/tobacco/media/en/title.pdf. [Google Scholar]
- 5.Menezes AM, Lopez MV, Hallal PC, Muiño A, Perez-Padilla R, Jardim JR, et al. Prevalence of smoking and incidence of initiation in the Latin American adult population: the PLATINO study. BMC Public Health. 2009;9:151. doi: 10.1186/1471-2458-9-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. [Accessed on 13 May 2014];Global adult tobacco survey fact sheets. 2013 Available from: www.who.int/tobacco/surveillance/survey/gats/en/
- 7.Levinson AH, Borrayo EA, Espinoza P, Flores ET, Pérez-Stable EJ. An exploration of Latino smokers and the use of pharmaceutical aids. [Accessed on 13 May 2014];Am J Prev Med. 2006 31(2):167–71. doi: 10.1016/j.amepre.2006.03.022. Available from: www.ncbi.nlm.nih.gov/pubmed/16829334. [DOI] [PubMed] [Google Scholar]
- 8.Levinson AH, Pérez-Stable EJ, Espinoza P, Flores ET, Byers TE. Latinos report less use of pharmaceutical aids when trying to quit smoking. [Accessed on 13 May 2014];Am J Prev Med. 2004 26(2):105–11. doi: 10.1016/j.amepre.2003.10.012. Available from: linkinghub.elsevier.com/retrieve/pii/S0749379703003222. [DOI] [PubMed] [Google Scholar]
- 9.Sansores RH, Pérez-bautista O, Neumól MC, Ramírez-Venegas A. Guías de atención médica para dejar de fumar. Una propuesta para Latinoamérica. 2010;52(1):355–65. doi: 10.1590/s0036-36342010000800034. [DOI] [PubMed] [Google Scholar]
- 10.Muñoz RF, Barrera AZ, Delucchi K, Penilla C, Torres LD, Pérez-Stable EJ. International Spanish/English Internet smoking cessation trial yields 20% abstinence rates at 1 year. Nicotine Tob Res. 2009;11(9):1025–34. doi: 10.1093/ntr/ntp090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Muñoz RF, Aguilera A, Schueller SM, Leykin Y, Pérez-Stable EJ. From online randomized controlled trials to participant preference studies: morphing the San Francisco Stop Smoking site into a worldwide smoking cessation resource. J Med Internet Res. 2012;14(3):e64. doi: 10.2196/jmir.1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schroeder SA. What to do with a patient who smokes. JAMA. 2005;294(4):482–7. doi: 10.1001/jama.294.4.482. [DOI] [PubMed] [Google Scholar]
- 13.Pérez-Stable EJ, Sabogal F, Marin G, Marin B, Otero-Sabogal R. Evaluation of the Guia para dejar de rumar: a Spanish language self-help guide to quit smoking. Public Health Reports. 1991;106:56–9. [PMC free article] [PubMed] [Google Scholar]
- 14.Marín BV, Pérez-Stable EJ, Marín GHW. Effects of a community intervention to change smoking behavior among Hispanics. Am J Prev Med. 1994;10(6):340–7. [PubMed] [Google Scholar]
- 15.Marín G, Pérez-Stable EJ. Effectiveness of disseminating culturally appropriate smoking-cessation information: Programa Latino Para Dejar de Fumar. Monogr Natl Cancer Inst. 1995;(18):155–63. [PubMed] [Google Scholar]
- 16.Muñoz RF, Marín BV, Posner SF, Pérez-Stable EJ. Mood management mail intervention increases abstinence rates for Spanish-speaking Latino smokers. Am J Community Psychol. 1997;25(3):325–43. doi: 10.1023/a:1024676626955. [DOI] [PubMed] [Google Scholar]
- 17.Muñoz RF, Lenert LL, Delucchi K, Stoddard J, Perez JE, Penilla C, et al. Toward evidence-based Internet interventions: A Spanish/English Web site for international smoking cessation trials. Nicotine Tob Res Off J Soc Res Nicotine Tob. 2006;8(1):77–87. doi: 10.1080/14622200500431940. [DOI] [PubMed] [Google Scholar]
- 18.Stoddard J, Delucchi K, Muñoz RF, Collins N, Pérez-Stable EJ, Augustson E, et al. Smoking cessation research via the internet: a feasibility study. J Health Commun. 2005;10(1):27–41. doi: 10.1080/10810730590904562. [DOI] [PubMed] [Google Scholar]
- 19.Leykin Y, Aguilera A, Torres LD, Pérez-Stable EJ, Muñoz RF. Interpreting the outcomes of automated Internet-based randomized trials: example of an International Smoking Cessation Study. J Med Internet Res. 2012;14(1):e5. doi: 10.2196/jmir.1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lewinsohn PM, Muñoz RF, Youngren MA, Zeiss A. Control your depression. New York: Fireside Books; 1992. [Google Scholar]
- 21.Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86(9):1119–27. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 22.Fiore MC, Smith SS, Jorenby DE, Baker TB. The effectiveness of the nicotine patch for smoking cessation. A meta-analysis. JAMA. 1994;271(24):1940–7. [PubMed] [Google Scholar]
- 23.Lando HA, McGovern PG, Barrios FX, Etringer BD. Comparative evaluation of American Cancer Society and American Lung Association smoking cessation clinics. Am J Public Health. 1990;80(5):554–9. doi: 10.2105/ajph.80.5.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dimidjian S, Barrera M, Martell C, Muñoz RF, Lewinsohn PM. The origins and current status of behavioral activation treatments for depression. Annu Rev Clin Psychol. 2011;7:1–38. doi: 10.1146/annurev-clinpsy-032210-104535. [DOI] [PubMed] [Google Scholar]
- 25.Cuijpers P, Donker T, van Straten a, Li J, Andersson G. Is guided self-help as effective as face-to-face psychotherapy for depression and anxiety disorders? A systematic review and meta-analysis of comparative outcome studies. Psychol Med. 2010;40(12):1943–57. doi: 10.1017/S0033291710000772. [DOI] [PubMed] [Google Scholar]
- 26.Muñoz RF. Using evidence-based inter-net interventions to reduce health disparities worldwide. J Med Internet Res. 2010;12(5):e60. doi: 10.2196/jmir.1463. [DOI] [PMC free article] [PubMed] [Google Scholar]