Abstract
Background
Colorectal cancer (CRC) screening is effective but underutilized. Although physician recommendation is an important predictor of screening, considerable variation in CRC screening completion remains.
Purpose
To characterize the influence of patient trust in care providers on CRC screening behavior.
Methods
Data were collected as part of a cluster–randomized CRC screening intervention trial performed in the San Francisco Community Health Network from March 2007 to January 2012 (analysis, Spring 2012). All study participants received a recommendation to complete CRC screening from their primary care provider (PCP). Included participants were aged 50–79 years, not current with screening, and completed the Wake Forest Trust Scale (WFTS) measuring trust in PCPs and doctors in general. Primary outcome was CRC screening completion (colonoscopy or fecal occult blood testing) within 12 months following enrollment. Multivariable association adjusted for race/ethnicity, language, and other sociodemographics was estimated using generalized estimating equations with logit link and binomial distribution.
Results
WFTS response was 70.3% (701). Most participants (83%) were Latino, Asian, or black. Most had income <$30,000 (96%) and public health insurance (86%). Higher trust in PCP was associated with screening completion (OR=1.11, 95% CI=1.03, 1.17), but trust in doctors was not (OR=1.02, 95% CI=0.82, 1.28). Race, language, and other sociodemographic factors were not significant in multivariable analysis.
Conclusions
After controlling for traditional factors, trust in PCP remained the only significant driver of CRC screening completion in low-income patients. Interventions to promote CRC screening may be improved by including efforts to enhance patient trust in PCP.
Introduction
Colorectal cancer (CRC) is the third leading cause of cancer death in the U.S.1 Despite the presence of multiple effective CRC screening strategies, screening is underutilized, particularly among racial and ethnic minority populations in the U.S.1–8 The decision to complete CRC screening is complex, involving many known and unknown factors, including patient preferences, health beliefs, societal and cultural factors, and relationships with the medical community.9–14
Physician recommendation to undergo CRC screening has been repeatedly identified as an important predictor of CRC screening completion in racial and ethnic minority populations.15–19 Research has shown that patients who self-report receiving a recommendation for screening by their care provider are much more likely to complete screening than those who do not. However, past research testing the effect of physician recommendation on CRC screening behavior has shown that not all patients who receive a recommendation go on to complete CRC screening.20
Trust has long been recognized as an important component of patient–provider relationships, and previous research has shown that increased patient trust is associated with increased use of preventive services; however, few studies have looked at its influence on CRC screening completion specifically.21–24 It is possible that a patient’s trust in their provider may influence the relationship between screening recommendation and completion. Patients who have high levels of trust in their care providers may be more likely to act on a recommendation to complete screening.
Patient trust is a difficult concept to measure. Consequently, little research has been conducted to understand its role. In the past decade, more attempts have been made to create validated measures of patient trust.23,25,26 Given the disparities in completion of CRC screening among racial/ethnic minority and socioeconomically disadvantaged populations in the U.S., a better understanding of the role of patient trust may be particularly important in these populations. The primary objective of this study was to characterize the relationship between patient trust and CRC screening behavior among racially and ethnically diverse, low-income patients who had all received a physician recommendation for screening.
Methods
Overview
This was a secondary analysis of data collected as part of the Colon Cancer Screening Adherence Study.20 The Adherence Study was a prospective, cluster-randomized study that compared competing strategies for recommendation of CRC screening. Study participants were assigned to receive a recommendation from their primary care provider (PCP) for: (1) fecal occult blood testing (FOBT); (2) colonoscopy; or (3) choice of FOBT or colonoscopy. The study was conducted in three clinics of the San Francisco Community Health Network, the safety–net healthcare system in the San Francisco Bay area. Continuity within the Community Health Network is extremely high, and all patients have an assigned PCP (attending physician, resident, fellow, or nurse practitioner). Nearly all participants were seen by their regular PCP on the date of enrollment. The patient’s PCP was responsible for counseling the patient to receive the predetermined intervention (FOBT only, colonoscopy only, or choice of either) during the specific time block. To decrease system-level impediments to screening, participants received an appointment for colonoscopy within 2 weeks of study enrollment, were provided with post-procedure transportation if required, and, in patients who had no insurance or otherwise had an inability to pay, colonoscopies were provided at no cost.
Data were collected between March 2007 and January 2012 (analysis, Spring 2012).20 Study participants were aged between 50 and 79 years, at average risk for CRC, and not up to date with recommended CRC screening guidelines (i.e., no FOBT within 1 year, sigmoidoscopy/barium enema within 5 years, or colonoscopy within 10 years). Potential study participants were identified through a computerized database search, and patients’ PCPs confirmed their eligibility for CRC screening. Identified participants were then contacted by research assistants, using patients’ preferred language of English, Spanish, Cantonese, or Mandarin, while waiting for their regularly scheduled appointment with their PCP for routine healthcare maintenance. Patients presenting for acute care visits were not included in this study. Of the 1,072 identified patients, 997 agreed to enter the original study.
Study Participants
Of the 997 subjects participating in the Adherence Study, 701 of these individuals completed the Wake Forest Trust subscales measuring trust in their PCP and in doctors in general, and met inclusion criteria for the analysis. Those who failed to complete one or both of the subscales were excluded. Of these 701 subjects, 252 had been previously assigned to the FOBT-only arm, 203 to the colonoscopy-only arm, and 245 to the choice arm (Figure 1).
Figure 1.
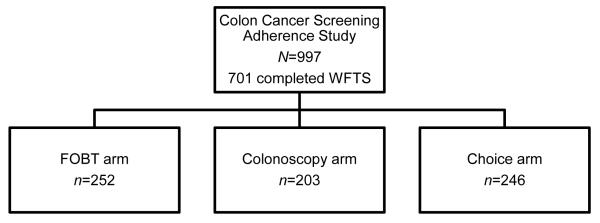
Participant breakdown by study group, Participants were randomized to one of three study arms as part of the Colon Cancer Screening Adherence Study (San Francisco, March 2007–January 2012). System-level barriers (access, cost, and transportation) to screening completion were minimized. FOBT, fecal occult blood testing; WFTS, Wake Forest Trust Scale
Survey Items
The abbreviated Wake Forest Trust Scale (WFTS) is a validated instrument that measures patient trust in three domains: trust in PCPs, trust in health insurers, and trust in doctors in general.25 Each domain (subscale) is measured using five survey items, each on a 5-point Likert scale, with higher scores indicating higher levels of trust in the specified entity. Examples of survey items include I completely trust my PCP’s/doctors’ decisions about which medical treatments are best for me and Sometimes my PCP/doctors care(s) more about what is convenient for him/them than about my medical needs (Appendix figures 1 and 2). This instrument was validated in primarily white populations using telephone participants, and additional research has shown that it performs similarly in minority populations.25,27 Participants who completed the WFTS pre-intervention did so in person, either alone or with assistance from research staff using the participants’ preferred language of English, Spanish, Cantonese, or Mandarin. All foreign-language versions of the subscales were translated and back translated independently and iteratively until consensus with the original English language version was reached. Participants who completed the WFTS during follow-up did so by phone with trained research personnel in English, Spanish, Cantonese, or Mandarin, based on the participants’ preference.
The WFTS questions were added to the pre-intervention survey in February 2008. Participants who enrolled prior to this time completed these questions at a follow-up visit (follow-up respondents). Participants who enrolled after the WFTS was added completed the questions prior to the intervention (pre-intervention respondents). All participants who completed the trust in PCP and trust in doctors general subscales of the WFTS instrument were included in this analysis (Figure 1). All participants in this study had a listed/regular PCP. Regardless of the timing of trust measurement, participants were instructed to rate their trust in the care provider who saw them at the enrollment visit.
Primary Outcome
The primary outcome was completion of CRC screening, defined as either submission of three FOBT test cards, follow-up colonoscopy for positive results, or colonoscopy, each within 12 months following study enrollment. Screening completion was assessed via documentation in the patient’s medical chart. If no documentation was present, the patient was contacted to confirm that they had not undergone screening.
Statistical Analyses
Primary analyses
Initial descriptive analyses of all variables were performed using means and proportions. For bivariate analysis of screening completion, chi-square tests and t-tests were used to describe the unadjusted relationship between patient trust and sociodemographic and other variables (race/ethnicity, gender, SES, insurance status, and PCP type) with CRC screening completion. These variables were chosen a priori based on literature about predictors of CRC screening behavior in similar populations.28 Adjusted analyses were measured using generalized estimating equations with logit link and binomial distribution to account for clustering by study group (physician recommendation strategy) with jackknifed SEs to account for few clusters. Clustering by PCP was not controlled for because the majority of providers had fewer than five total patients participating in the study. The significance of independent variables of interest was examined using Wald tests.
Sensitivity analyses
Because the responses to the WFTS questions completed pre-intervention and those completed at follow-up were combined, two sensitivity analyses were completed. To ensure that no bias was introduced by using trust scale responses collected at different time periods, t-tests and chi-square tests were used to assess differences in sociodemographic characteristics and trust scores between the pre-intervention and follow-up trust respondent groups. A regression analysis identical to the primary analysis was also conducted separately to determine whether CRC screening completion differed between these groups.
Results
A total of 701 participants were included in this analysis (Table 1), the majority of whom were Latino (36%) or Asian (29%). Fifty-four percent were female, the mean age was 58 years, and half were patients of an attending physician or nurse practitioner. Fifty-five percent preferred to speak English, 28% Spanish, and 17% Chinese (predominantly Cantonese). The majority of participants were of lower SES, with 62% attaining a high school diploma or less, 55% with a family income of less than $10,000, and 64% unemployed. Trust was generally high; the mean score on the trust in PCP subscale was 20.9, and the mean score on the doctors in general subscale was 18.5 (possible maximum of 25 for both subscales), among all participants. Trust in PCP was higher for patients who saw an attending physician or nurse practitioner rather than a medical fellow or resident physician (21.4 vs 20.4, p<0.001). Among those excluded from the study (n=296), the mean age was 59 years (vs 58 years, p=0.04), 48% were men (vs 46%, p=0.55), and 55% completed screening (vs 69%, p<0.001).
Table 1.
Baseline sociodemographic characteristics of participants (n=701)
| Screened | Unscreened | |
|---|---|---|
| Age, M years | 58.7 | 56.8 |
| Sex, n (%) | ||
| Female | 259 (53.9) | 120 (54.6) |
| Male | 222 (46.2) | 100 (45.5) |
|
Wake Forest Trust Scale,
M (SD) |
||
| Trust in PCP | 21.03 (2.38) | 20.60 (3.05) |
| Trust in doctors in general | 18.63 (2.84) | 18.16 (3.16) |
| Race/ethnicity, n (%) | ||
| Latino | 184 (38.3) | 65 (29.6) |
| Asian | 152 (31.6) | 54 (24.6) |
| Black | 68 (14.1) | 57 (25.9) |
| White | 77 (16.0) | 44 (20.0) |
| Language, n (%) | ||
| English | 238 (49.5) | 146 (66.4) |
| Spanish | 150 (31.2) | 48 (21.8) |
| Chinese | 93 (19.3) | 26 (11.8) |
| Education level, n (%) | ||
| <HS degree/GED | 173 (36.0) | 59 (26.8) |
| HS degree/GED | 129 (26.8) | 73 (33.2) |
| Some college | 87 (18.1) | 51(23.2) |
| ≥College degree | 92 (19.1) | 37 (16.8) |
| Employed, n (%) | ||
| No | 302 (62.8) | 151 (68.6) |
| Yes | 179 (37.2) | 69 (31.4) |
|
Annual household income,
n (%) |
||
| <$10,000 | 263 (54.7) | 125 (56.8) |
| $10,000–$19,999 | 162 (33.7) | 68 (30.9) |
| ≥20,000 | 56 (11.6) | 27 (12.3) |
| Insurance, n (%) | ||
| None | 60 (12.5) | 33 (15.0) |
| Public | 414 (86.1) | 185 (84.1) |
| Private | 7 (1.5) | 2 (0.9) |
GED, General Educational Development; HS, high school
Bivariate analyses showed significant strong relationships between age, race/ethnicity, language, and education and completion of CRC screening (Table 2). Health insurance and trust measures were also marginally significantly associated with CRC screening completion. Multivariable analysis revealed that after controlling for age, race, gender, SES, preferred language, insurance status, and type of PCP (attending physician, fellow, or nurse practitioner), only trust in one’s PCP was associated with CRC screening completion. For every point increase in the trust in PCP subscale of the WFTS, odds of completing CRC screening increased 1.11 times (95% CI=1.03, 1.17). Trust in doctors in general was not significantly associated with screening completion (OR=1.02, 95% CI=0.82, 1.28). Age, race/ethnicity, language, health insurance, provider type, and education were no longer significantly associated with screening completion.
Table 2.
Patient trust predicts adherence to CRC screening
| Variable (ref group) | Bivariate analysis | Multivariable analysis* | ||
|---|---|---|---|---|
| OR | p | OR (95% CI) | p | |
| Age, per year increase a | 1.05 | 0.001 | 1.03 (0.95, 1.13) | 0.24 |
| Gender (female) | ||||
| Male | 1.03 | 0.863 | 1.37 (0.59, 3.17) | 0.22 |
| Race/ethnicity (white) | ||||
| Asian | 1.61 | 0.054 | 1.32 (0.35, 4.75) | 0.46 |
| Black | 0.68 | 0.142 | 0.78 (0.16, 3.07) | 0.54 |
| Latino | 1.62 | 0.04 | 1.18 (0.09, 11.92) | 0.80 |
| Language (English) | ||||
| Spanish | 1.92 | 0.001 | 1.95 (0.25, 17.10) | 0.31 |
| Chinese | 2.19 | 0.001 | 1.74 (0.82, 3.30) | 0.08 |
| Income (<$10,000) | ||||
| $10,000–$19,999 | 1.13 | 0.80 | 1.14 (0.20, 6.01) | 0.77 |
| $20,000–$29,999 | 0.95 | 0.86 | 0.92 (0.12, 7.78) | 0.87 |
| ≥$30,000 | 1.11 | 0.84 | 1.09 (0.00, 326.41) | 0.96 |
| Education (<HS) | ||||
| HS degree/GED | 0.60 | 0.016 | 0.76 (0.42, 1.46) | 0.20 |
| Some college | 0.59 | 0.02 | 0.86 (0.30, 2.50) | 0.60 |
| ≥College degree | 0.85 | 0.50 | 1.11 (0.64, 1.85) | 0.49 |
| Insurance (none) | ||||
| Public | 1.23 | 0.38 | 1.22 (0.18, 8.53) | 0.70 |
| Private | 1.93 | 0.43 | 2.22 (0.03, 146.13) | 0.50 |
|
Trust in PCP, per point
increase |
1.06 | 0.046 b | 1.11 (1.04, 1.16) | 0.02 |
|
Trust in doctors in
general, per point increase |
1.05 | 0.69 | 0.05 b | 1.02 (0.83, 1.27) |
Note: Boldface indicates statistical significance.
Controlling for sociodemographic variables.
Per year increase.
Per point increase.
GED, General Educational Development; HS, high school
Comparing the trust scores between the pre-intervention and follow-up respondents, those who completed the questions at follow-up scored 1.4 points lower (p<0.001) on the trust in PCP subscale and 0.64 points lower (p=0.004) on the trust in doctors in general subscale (Appendix Table). In the follow–up trust respondent group, 41% reported having a different PCP than during the intervention. Trust in PCP scores were higher and trust in doctors in general scores were lower among those who had switched PCPs versus those who had not switched PCPs (PCP, 20.6 vs 19.9, p=0.003; doctors in general, 17.7 vs 18.5, p=0.02). Additionally, the pre-intervention group compared to the follow-up group was, on average, 1.5 years younger, less likely to be Latino (40% vs 31%, respectively), and less likely to be poor (62% vs 49% with a family income <$10,000/year). However, comparison of the stratified regression models demonstrated that the estimates of effect of trust in one’s PCP on screening completion did not change appreciably, although the pre-intervention respondents’ OR was no longer statistically significant (pre-intervention OR=1.11, p=0.07; post-intervention OR=1.15, p<0.001). Trust in PCP remained the only significant predictor of CRC screening in multivariable models restricted to the pre-intervention group, the follow-up group, and among those in the follow-up group who changed PCP.
Discussion
The association between patient trust in their PCP or in doctors in general and completion of CRC screening was examined in a low-income, predominantly minority population. Trust was generally high, and the difference in trust in PCP across screening groups was small. However, the results showed that greater trust in one’s PCP was associated with CRC screening completion. There was no association between trust in doctors in general and screening completion. In addition, race, language, SES, and other sociodemographic characteristics, usually found to be associated with CRC screening behavior, were no longer statistically significant when trust was included in the model. These results imply that the personal relationship between a PCP and a patient, and not how the patient feels about medical professionals in general, may be an important driver for increased screening.
The results of this study suggest that, in a low-SES population, the personal relationship between a PCP and a patient, a factor that is modifiable, may affect CRC screening completion beyond some immutable sociodemographic factors. This is consistent with previous research that has shown a relationship between patient trust and preventive health behaviors.29,30 Similar to the findings of this study, Bonds et al.29 found that, in a population with generally high trust, increased trust was associated with improved diabetes self-care. These results add to a small body of evidence supporting the relationship between trust and cancer screening completion. In some previous qualitative work, investigators found that patients tended to reference a lack of trust in their physician as a reason for not wanting to follow a recommendation for cancer screening.31–33 Other small quantitative studies have also shown a potential statistical relationship between trust and screening.21,34
This study shows strong support for the concept that increased trust in one’s PCP influences CRC screening behaviors. Much of the current research in this field focuses on the relationship of trust and adherence to treatment regimens, yet with the current drive towards enhancing cost-effectiveness and the focus on patient-centeredness in healthcare, emphasis is shifting to the prevention of disease.35–37 The findings of this study may have implications for patient–centered care delivery models, such as the Patient–Centered Medical Home (PCMH).38 The results bolster the importance of patient–care provider relationship continuity, a key feature of PCMH. Further, the results may suggest that focus on not only the continuity of the patient–provider relationship, but also the quality of that relationship, as suggested by patient trust, may have a beneficial effect on participation in preventive care. Specifically for CRC screening, because physician recommendation is so strongly related to screening completion, research regarding trust in physicians may have profound consequences for increasing screening rates.15–19 In particular, the association between trust in one’s PCP and CRC screening completion demonstrated in this study illustrates the importance of developing strong patient–physician relationships to increase CRC screening adherence.
Prior studies have identified a variety of sociodemographic factors that are linked to completion of colorectal cancer screening tests; specifically, non-whites, and those with less education, less continuity of care and lower rates of other preventive care measures are more likely to be nonparticipants.39 Various interventions including decision aid-assisted shared decision making or implementation intentions techniques have been shown to increase screening participation.40-41 However, previous studies were not able to show significant relationships between trust and CRC screening behavior. The results of this study may have differed because of the concerted effort undertaken to reduce system-level barriers to access to screening among the most vulnerable of socioeconomic groups.20 Study participants were provided recommendations and instructions in their language of choice (English, Spanish, Mandarin, or Cantonese), transportation to and from the colonoscopy appointment were provided if necessary, and costs of screening tests were minimized. With fewer barriers to access, the relationship between trust and screening may have been uncovered. In addition, there were differences in the impact of trust in one’s PCP compared with trust in doctors in general on CRC screening completion. In the analysis, it was the trust a patient held in their PCP and not in healthcare providers in general that was important for screening completion. This finding has practical significance because individual providers may more readily undertake measures to augment patient trust than healthcare establishments such as clinics and hospitals. By utilizing personal knowledge of and access to the patient, the clinician may tailor their approach to enhance the patient–provider relationship.
A strength of this study is that the sample consists of predominantly low–income minority patients. However, these findings may not be generalizable to other populations. Further research is necessary to determine whether these results are consistent across different populations and settings. Also, there is a potential for selection bias given that among those excluded from the study because of failure to complete the WFTS, there was a much lower rate of CRC screening completion. The majority of those excluded from this analysis, in whom trust was never measured, were unreachable at follow-up. This could indicate that they were somehow less receptive to engaging in the study or with the healthcare system, which could be reflective of lower trust.
Additionally, results may have been impacted by the difference in timing of the trust measurement among participants (baseline versus post-intervention). Respondents, regardless of time of measurement, were instructed to rate the provider who saw them at the study index visit, but many in the post-intervention respondent group switched PCPs during the study period. It is possible that some in whom trust was measured post-intervention may not have followed the instruction. Differences also could have arisen because of recall bias: participants responding at post-intervention may not have a good memory of their feelings towards the study provider. In addition, trust was collected in person at baseline and over the telephone at post-intervention. This may have an effect on how the participant reported trust, possibly resulting from social desirability. Despite these possible sources of bias, the sensitivity analyses showed little difference in reported trust across the baseline and post-intervention respondents. Finally, the WFTS has not been formally validated in minority populations. However, an analysis of internal consistency revealed strong internal consistency of the WFTS scales in minority populations.27
These findings, obtained in the unique setting of an urban safety–net population with minimal barriers to access to health care, suggest that variation in CRC screening completion is greatly influenced by trust in one’s PCP rather than by traditional sociodemographic characteristics. Moreover, trust in doctors as a general concept was not associated with screening completion. This suggests that physician recommendation itself is insufficient to increase patient adherence, but the recommendation must originate from a particular physician in whom the patient trusts. Future interventions to increase CRC screening completion should focus on patient trust in their PCP and on enhancing the individual patient–physician relationship.
Supplementary Material
Acknowledgments
The parent study (Colon Cancer Screening Adherence Study) from which the data were extracted was funded by grant no. R01CA106773 from the National Cancer Institute at the NIH, grant no. K24DK080941 from the National Institutes of Diabetes and Digestive and Kidney Diseases at the NIH, and grant no. UL1 RR024131 from the National Center for Research Resources at the NIH. The funding source had no role in the design, conduct, or reporting of this secondary data analysis or in the decision to submit the article for publication. Dr. Brenner was supported by an Agency for Healthcare Research and Quality National Research Service Award Training Grant (previous: grant no. 5T32 HS 13853-9––University of Washington School of Public Health, Department of Health Services; current: grant no. 5T32-HS000032––University of North Carolina at Chapel Hill, Cecil 473 Sheps Center for Health Services Research).
This study was previously presented, in part, at the 2012 Georgia Chapter American College of Physicians Annual Meeting, September 14–16, 2012, Buford, Georgia, and at the American College of Physicians Internal Medicine 2013 Annual Meeting, April 11–13, 2013, San Francisco, California.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.American Cancer Society . Colon/rectum cancer detailed guide. American Cancer Society; Atlanta GA: 2013. www.cancer.org/cancer/colonandrectumcancer/detailedguide/colorectal-cancer-pdf23. [Google Scholar]
- 2.CDC Vital signs: colorectal cancer screening, incidence, and mortality—U.S., 2002–2010. MMWR Morb Mortal Wkly Rep. 2011;60(26):884–9. [PubMed] [Google Scholar]
- 3.Kronborg O, Fenger C, Olsen J, et al. Randomised study of screening for colorectal cancer with faecal-occult-blood test. Lancet. 1996;348(9040):1467–71. doi: 10.1016/S0140-6736(96)03430-7. [DOI] [PubMed] [Google Scholar]
- 4.Mandel JS, Church TR, Bond JH, et al. The effect of fecal occult-blood screening on the incidence of colorectal cancer. N Engl J Med. 2000;343(22):1603–7. doi: 10.1056/NEJM200011303432203. [DOI] [PubMed] [Google Scholar]
- 5.Hardcastle JD, Chamberlain JO, Robinson MH, et al. Randomised controlled trial of faecal-occult-blood screening for colorectal cancer. Lancet. 1996;348(9040):1472–7. doi: 10.1016/S0140-6736(96)03386-7. [DOI] [PubMed] [Google Scholar]
- 6.Schoen RE, Pinsky PF, Weissfeld JL, et al. Colorectal-cancer incidence and mortality with screening flexible sigmoidoscopy. N Engl J Med. 2012;366(25):2345–57. doi: 10.1056/NEJMoa1114635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Cancer Society . Cancer facts and figures for African Americans. American Cancer Society; Atlanta GA: 2013. www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-036921.pdf. [Google Scholar]
- 8.American Cancer Society . Cancer facts and figures for Hispanics/Latinos. American Cancer Society; Atlanta GA: 2012. www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-034778.pdf. [Google Scholar]
- 9.Rawl SM, Menon U, Champion VL, et al. Do benefits and barriers differ by stage of adoption for colorectal cancer screening? Health Educ Res. 2005;20(2):137–48. doi: 10.1093/her/cyg110. [DOI] [PubMed] [Google Scholar]
- 10.Rawl SM, Menon U, Champion VL, Foster JL, Skinner CS. Colorectal cancer screening beliefs. Focus groups with first-degree relatives. Cancer Pract. 2000;8(1):32–7. doi: 10.1046/j.1523-5394.2000.81006.x. [DOI] [PubMed] [Google Scholar]
- 11.Sifri R, Rosenthal M, Hyslop T, et al. Factors associated with colorectal cancer screening decision stage. Prev Med. 2010;51(3–4):329–31. doi: 10.1016/j.ypmed.2010.06.015. [DOI] [PubMed] [Google Scholar]
- 12.Pignone MP, Harris R, Kinsinger L. Videotape-based decision aid for colon cancer screening. Ann Intern Med. 2000;133(10):761–9. doi: 10.7326/0003-4819-133-10-200011210-00008. [DOI] [PubMed] [Google Scholar]
- 13.Tu SP, Taylor V, Yasui Y, et al. Promoting culturally appropriate colorectal cancer screening through a health educator: a randomized controlled trial. Cancer. 2006;107(5):959–66. doi: 10.1002/cncr.22091. [DOI] [PubMed] [Google Scholar]
- 14.Tu SP, Yip MP, Li L, et al. Continuity of care and colorectal cancer screening by Vietnamese American patients. Asian Pac J Cancer Prev. 2010;11(4):1125–31. [PMC free article] [PubMed] [Google Scholar]
- 15.Cronan TA, Devoscomby L, Villalta I, Gallagher R. Ethnic differences in colorectal cancer screening. J Psychosoc Oncol. 2008;26(2):63–86. doi: 10.1300/j077v26n02_05. [DOI] [PubMed] [Google Scholar]
- 16.Ferrer RR, Ramirez M, Beckman LJ, Danao LL, Ashing-Giwa KT. The impact of cultural characteristics on colorectal cancer screening adherence among Filipinos in the U.S.: a pilot study. Psychooncology. 2011;20(8):862–70. doi: 10.1002/pon.1793. [DOI] [PubMed] [Google Scholar]
- 17.Jo AM, Maxwell AE, Wong WK, Bastani R. Colorectal cancer screening among underserved Korean Americans in Los Angeles County. J Immigr Minor Heal. 2008;10(2):119–26. doi: 10.1007/s10903-007-9066-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shokar NK, Carlson CA, Weller SC. Factors associated with racial/ethnic differences in colorectal cancer screening. J Am Board Fam Med. 2008;21(5):414–26. doi: 10.3122/jabfm.2008.05.070266. [DOI] [PubMed] [Google Scholar]
- 19.Yepes-Rios M, Reimann JOF, Talavera AC, Ruiz de Esparza A, Talavera G. Colorectal cancer screening among Mexican Americans at a community clinic. Am J Prev Med. 2006;30(3):204–10. doi: 10.1016/j.amepre.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 20.Inadomi JM, Vijan S, Janz NK, et al. Adherence to colorectal cancer screening: a randomized clinical trial of competing strategies. Arch Intern Med. 2012;172(7):575–82. doi: 10.1001/archinternmed.2012.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Born W, Engelman K, Greiner KA, et al. Colorectal cancer screening, perceived discrimination, and low-income and trust in doctors: a survey of minority patients. BMC Public Health. 2009;9:363. doi: 10.1186/1471-2458-9-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.O’Malley AS, Sheppard VB, Schwartz M, Mandelblatt J. The role of trust in use of preventive services among low-income African-American women. Prev Med. 2004;38(6):777–85. doi: 10.1016/j.ypmed.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 23.Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter? Milbank Q. 2001;79(4):613–39. v. doi: 10.1111/1468-0009.00223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pearson SD, Raeke LH. Patients’ trust in physicians: many theories, few measures, and little data. J Gen Intern Med. 2000 Jul;15(7):509–13. doi: 10.1046/j.1525-1497.2000.11002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dugan E, Trachtenberg F, Hall MA. Development of abbreviated measures to assess patient trust in a physician, a health insurer, and the medical profession. BMC Health Serv Res. 2005;5:64. doi: 10.1186/1472-6963-5-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zheng B, Hall MA, Dugan E, Kidd KE, Levine D. Development of a scale to measure patients’ trust in health insurers. Health Serv Res. 2002;37(1):187–202. [PubMed] [Google Scholar]
- 27.Brenner AT, Inadomi JM. Wake Forest trust scale performance and scoring in racial-ethnic minorities in the context of colon cancer screening. Proceedings of the National Research Services Award Trainees 18th Annual Conference; Orlando FL. 2012 Jun 23. [Google Scholar]
- 28.Holden D, Jonas DE, Porterfield D, Reuland D, Harris R. Systematic review: enhancing use and quality of colorectal cancer screening. Ann Intern Med. 2010;152(10):668–76. doi: 10.7326/0003-4819-152-10-201005180-00239. [DOI] [PubMed] [Google Scholar]
- 29.Bonds DE, Camacho F, Bell R, Duren-Winfield VT, Anderson RT, Goff DC. The association of patient trust and self-care among patients with diabetes mellitus. BMC Fam Pract. 2004;5:26. doi: 10.1186/1471-2296-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carpenter WR, Godley PA, Clark JA, et al. Racial differences in trust and regular source of patient care and the implications for prostate cancer screening use. Cancer. 2009;115(21):5048–59. doi: 10.1002/cncr.24539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lasser KE, Kelly B, Maier J. Discussions about preventive services: a qualitative study. BMC Fam Pract. 2008;9:49. doi: 10.1186/1471-2296-9-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gao G, Burke N, Somkin CP, Pasick R. Considering culture in physician–patient communication during colorectal cancer screening. Qual Health Res. 2009;19(6):778–89. doi: 10.1177/1049732309335269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McAlearney AS, Oliveri JM, Post DM, et al. Trust and distrust among Appalachian women regarding cervical cancer screening: a qualitative study. Patient Educ Couns. 2012;86(1):120–6. doi: 10.1016/j.pec.2011.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O’Malley AS, Beaton E, Yabroff KR, Abramson R, Mandelblatt J. Patient and provider barriers to colorectal cancer screening in the primary care safety-net. Prev Med. 2004;39(1):56–63. doi: 10.1016/j.ypmed.2004.02.022. [DOI] [PubMed] [Google Scholar]
- 35.Baker DW, Qaseem A, Reynolds PP, Gardner LA, Schneider EC. Design and use of performance measures to decrease low-value services and achieve cost-conscious care. Ann Intern Med. 2013;158(1):55–60. doi: 10.7326/0003-4819-158-1-201301010-00560. [DOI] [PubMed] [Google Scholar]
- 36.Selby JV, Beal AC, Frank L. The Patient-Centered Outcomes Research Institute (PCORI) national priorities for research and initial research agenda. JAMA. 2012;307(15):1583–4. doi: 10.1001/jama.2012.500. [DOI] [PubMed] [Google Scholar]
- 37.Ratanawongsa N, Karter AJ, Parker MM, et al. Communication and medication refill adherence: the diabetes study of northern california. JAMA Intern Med. 2013;173(3):210–8. doi: 10.1001/jamainternmed.2013.1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kellerman R, Kirk L. Principles of the patient-centered medical home. Am Fam Physician. 2007;76(6):774–5. [PubMed] [Google Scholar]
- 39.Green BB, Bogart A, Chubak J, Vernon SW, Morales LS, Meenan RT, Laing SS, Fuller S, Ko C, Wang CY. Nonparticipation in a population-based trial to increase colorectal cancer screening. Am J Prev Med. 2012;42:390–7. doi: 10.1016/j.amepre.2011.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schroy PC, Emmons KM, Peters E, Glick JT, Robinson PA, Lydotes MA, Mylvaganam SR, Coe AM, Chen CA, Chaisson CE, Pignone MP, Prout MN, Davidson PK, Heeren TC. Aid-assisted decision making and colorectal cancer screening: a randomized controlled trial. Am J Prev Med. 2012;43:573–83. doi: 10.1016/j.amepre.2012.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Neter E, Stein N, Barnett-Griness O, Rennert G, Hagoel L. From the bench to public health: population-level implementation intentions in colorectal cancer screening. Am J Prev Med. 2014;46:273–80. doi: 10.1016/j.amepre.2013.11.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


