Abstract
AIM: To investigate differences in the effects of biliary drainage procedures in patients with inoperable Klatskin’s tumor based on Bismuth type, considering endoscopic retrograde biliary drainage (ERBD), external percutaneous transhepatic biliary drainage (EPTBD) and internal biliary stenting via the PTBD tract (IPTBD).
METHODS: The initial success rate, cumulative patency rate, and complication rate were compared retrospectively, according to the Bismuth type and ERBD, EPTBD, and IPTBD. Patency was defined as the duration for adequate initial bile drainage or to the point of the patient’s death associated with inadequate drainage.
RESULTS: One hundred thirty-four patients (93 men, 41 women; 21 Bismuth type II, 47 III, 66 IV; 34 ERBD, 66 EPTBD, 34 IPTBD) were recruited. There were no differences in demographics among the groups. Adequate initial relief of jaundice was achieved in 91% of patients without a significant difference in the results among different procedures or Bismuth types. The cumulative patency rates for ERBD and IPTBD were better than those for EPTBD with Bismuth type III. IPTBD provided an excellent response for Bismuth type IV. However, there was no difference in the patency rate among drainage procedures for Bismuth type II. Procedure-related cholangitis occurred less frequently with EPTBD than with ERBD and IPTBD.
CONCLUSION: ERBD is recommended as the first-line drainage procedure for the palliation of jaundice in patients with inoperable Klatskin’s tumor of Bismuth type II or III, but IPTBD is the best option for Bismuth type IV.
Keywords: Klatskin's tumor, Palliation, Drainage, Bile ducts, Intervention
INTRODUCTION
Primary cholangiocarcinoma is an uncommon malignancy with a poor prognosis in the West[1-3] and Klatskin’s tumor (Hilar cholangiocarcinoma) accounts for 15%-53% of primary cholangiocarcinoma[4]. In Asia, however, Klatskin’s tumor is a common cause of malignant biliary obstruction[5]. Furthermore, the incidence and mortality from cholangiocarcinoma are increasing worldwide[6,7]. Because of the absence of early symptoms, Klatskin’s tumor is often diagnosed at an advanced stage, when jaundice is the most important clinical symptom[2]. Klatskin’s tumor is classified according to the type of involvement with the hepatic ducts, as described by Bismuth[8]. This classification is clinically important because the resectability of tumors, and the methods of biliary drainage, depends on Bismuth type. Complete resection of the tumor, with negative resection margins, offers the best possibility for long-term survival[2,9]. However, only 10% to 20% of patients are candidates for such curative resection. The majority of patients, therefore, can only be offered palliative drainage treatment[3,8].
Advances in interventional radiology and therapeutic endoscopy have facilitated nonsurgical management for patients with advanced types of the disease as well as those with high operative risks[10-12]. Endoscopic or percutaneous drainage has therefore become established as effective and relatively noninvasive alternatives for palliation of jaundice[13]. Currently, endoscopic retrograde biliary drainage (ERBD), external percutaneous transhepatic biliary drainage (EPTBD), and internal biliary stenting via the PTBD tract (IPTBD) are being used for the palliation of jaundice in patients with unresectable Klatskin’s tumor. Although it is expected that certain drainage procedures are more effective for a given Bismuth type of Klatskin’s tumor, there has been no study comparing the effects of diverse drainage methods based on the Bismuth type of Klatskin’s tumor. Only one study compared the complication rate associated with ERBD and EPTBD in a small number of patients[13]. Therefore, we conducted a study to evaluate the efficacy of the drainage procedures ERBD, EPTBD, and IPTBD based on the Bismuth type in patients with inoperable Klatskin’s tumor. In addition, we determined whether stent type or stent number (unilateral or bilateral) can affect the patency of biliary drainage.
MATERIALS AND METHODS
Patients
The clinical records of patients with inoperable Klatskin’s tumor, who were treated with ERBD, PTBD, or PTBDS at Seoul National University Hospital from January 1999 to December 2005, were reviewed retrospectively. Institutional review board approval was obtained for this retrospective study. We evaluated demographic variables, clinical symptoms, and laboratory values, as well as imaging with ultrasonography, computerized tomography, magnetic resonance imaging, endoscopic retrograde cholangiopancreatography (ERCP), and percutaneous cholangiography. Follow-up and survival data were obtained from the Korean Central Cancer Registry, as well as direct telephone contact with patients or with relatives if the patient had died or had been lost to follow-up during the intervening period.
The diagnosis of malignancy as the etiology of biliary obstruction was made by histologic or cytologic examinations with tissue samples obtained during ERCP, PTBD, or percutaneous needle biopsy. The patients with hilar stenosis, due to metastatic tumor, gallbladder cancer, liver cancer, or Klatskin’s tumor for which radical or palliative surgery had been done previously, were excluded from this study. Bilateral stents or tubes were inserted if one stent could not drain more than 30% of the volume of liver segment or jaundice has progressed just immediately after the unilateral drainage.
ERCP was performed with a therapeutic duodenoscopy (TJF-240, JF-240, TJF-200, and JF-200; Olympus Optical Co., Ltd, Tokyo, Japan). The 10-mm diameter uncovered self-expandable metallic stent (Wallstent®; Boston Scientific, MA, USA), and 10-Fr polyethylene stent (MTW Endoscopie, Wesel, Germany) were used for ERBD. For EPTBD, visualization of the biliary system was achieved with a Chiba needle under radiologic control. A 5-Fr puncture needle catheter was introduced into the biliary system and an 8.5-Fr or 10-Fr external drainage catheter (Ultrathane®; Cook Inc., Bloomington, USA) was inserted percutaneously into an appropriate intrahepatic duct. The patients were allowed to maintain EPTBD if they refused to undergo IPTBD. IPTBD was performed as a staged procedure. The endoprosthesis was inserted at the second stage, a few days after the first percutaneous transhepatic biliary drainage procedure. Endoprosthesis used for PTBDS was a 10-mm diameter self-expandable metal stent (Wallstent®; Boston Scientific, MA, USA or Niti-S® Biliary Stent; Taewoong Medical Co. Ltd., Kyunggi-do, Korea). An endoscopic approach was preferred as an initial drainage procedure when experienced endoscopists were available (two or three days per week) in our institute, however, a percutaneous approach was performed in other situations. The procedure was explained to all patients and informed consent was obtained in all cases. All authors carried out this research in accordance with the Helsinki Declaration.
Methods
The obstruction pattern of the bile duct was classified according to Bismuth type[8] on the basis of direct cholangiography, magnetic resonance cholangiography or multi-detector row computed tomographic cholangiography. Clinical data after the drainage procedure, such as success rate of initial palliation of cholestasis, duration of patency of adequate drainage, procedure-related complications, such as cholangitis, pancreatitis, bleeding, immediate mortality, and thirty-day mortality, were compared among the groups that were stratified according to the drainage procedures and Bismuth types.
The initial palliation of cholestasis was defined as successful when the total bilirubin level decreased by more than 30% in one week after the procedure, or to a near-normal level if a later determination was available[14]. The duration of drainage patency was defined as the time interval from the successful drainage procedure either to the point of obstruction or migration of the stent, or to when the tube needed to be replaced using another interventional procedure, or to the point of patient death due to cholangitis. Procedure-related cholangitis was defined as new onset of fever (> 38.2°C) and/or leukocytosis (WBC > 10 000/mm3) with right upper quadrant abdominal pain or tenderness. Pancreatitis was diagnosed when serum amylase levels rose to more than three times the normal limit (60-180 U/L) with notable persistent abdominal pain for more than 24 h after the procedure. Significant bleeding was defined as a requirement for blood transfusions of more than 2 units or hemostatic procedures including surgery being necessary after the drainage procedure. Procedure-related mortality was defined as death directly related to a complication just after the procedure or death within 30 d after the procedure.
Statistical analysis
The variables in the treatment groups were compared, assuming a 95% probability for rejection of the null hypotheses. The Fisher exact test, Pearson’s chi-squared test, and one way analysis of variance were used, when appropriate, to calculate the statistical significance of different demographic and clinical variables. Yates’ correction for continuity would not have removed significance from any findings, so all P values are presented uncorrected for the Yates’ correction. The one way analysis of variance was corrected by the Bonferroni’s method as a multiple comparison test. The cumulative patency rate for each type of drainage procedure was calculated with the Kaplan-Meier method by using the log rank test. To identify independent factors that can be associated with drainage patency, variables such as type of drainage procedure, stent type and stent number were included in a multivariate analysis using the Cox regression analysis. Continuous variables were reported as mean ± standard error. The statistical analysis was performed with software (SPSS 12.0K for windows; SPSS Korea, Seoul, Korea). A P < 0.05 was considered statistically significant.
RESULTS
Between January 1999 and December 2005, 134 patients (93 men, 41 women) underwent nonsurgical palliative treatment for inoperable Klatskin’s tumor, including Bismuth types II-IV. Twenty-one cases were Bismuth type II, 47 patients were Bismuth type III, and 66 patients were Bismuth type IV. Thirty-four patients were treated with ERBD, 66 patients with EPTBD, and 34 patients using IPTBD. Adequate initial relief of jaundice was achieved in 122 patients (91%) after the biliary drainage procedure. Two patients died due to cholangitis within 30 d of the procedure.
Overall patients
When comparing clinical characteristics by Bismuth type, there was no difference in age, sex, serum bilirubin level, success rate of initial palliation of cholestasis, cumulative patency rate of the drainage, and complications after drainage procedures (Table 1). When we compared the clinical characteristics of the patients for each drainage method without further stratification according to Bismuth type, there were no differences in age, sex and Bismuth type (Table 2). However, the initial serum bilirubin level in patients treated with EPTBD was higher than that in patients treated with ERBD or IPTBD (P < 0.01).
Table 1.
Demographics and clinical outcome of patients according to Bismuth type
| Bismuth II | Bismuth III | Bismuth IV | P value | |
| Number of patients | 21 | 47 | 66 | |
| Age (yr)1 | 68.9 ± 2.4 | 67.5 ± 1.4 | 66.6 ± 1.3 | 0.66 |
| Sex (M:F) | 16:5 | 31:16 | 46:20 | 0.74 |
| Serum bilirubin (mg/dL)1 | 9.55 ± 1.66 | 14.06 ± 1.27 | 12.69 ± 0.93 | 0.10 |
| ERBD:EPTBD:IPTBD | 6:8:7 | 12:23:12 | 16:35:15 | 0.74 |
| Palliation of cholestasis | 21 (100%) | 43 (91.5%) | 7 (88%) | 0.30 |
| Patency (d)1 | 103 ± 17 | 98 ± 12 | 113 ± 15 | 0.85 |
| Patency (d)2 | 92 (32-152) | 65 (35-95) | 81 (55-107) | |
| Procedure related cholangitis | 5 (23.8%) | 12 (25.5%) | 12 (18.2%) | 0.58 |
| Procedure related pancreatitis | 0 (0%) | 2 (4.3%) | 0 (0%) | 0.15 |
| Procedure related bleeding | 1 (4.8%) | 5 (10.6%) | 6 (9.1%) | 0.79 |
| Procedure related mortality | 0 | 0 | 0 | 1.00 |
| 30-d mortality | 0 (0%) | 1 (2.1 %) | 1 (1.5%) | 1.00 |
Values expressed as mean ± SE.
Values expressed as median (range).
Table 2.
Demographics and clinical outcome of patients according to drainage procedure
| ERBD | PTBD | PTBDS | P value | |
| Number of patients | 34 | 66 | 34 | |
| Age (yr)1 | 66.8 ± 2.9 | 67.2 ± 1.1 | 67.9 ± 1.8 | 0.91 |
| Sex (M:F) | 23:11 | 46:20 | 24:10 | 0.97 |
| Bismuth type(II:III:IV) | 6:12:16 | 8:23:35 | 7:12:15 | 0.81 |
| Serum bilirubin (mg/L)1 | 9.62 ± 1.14 | 14.89 ± 1.10 | 11.47 ± 1.09 | < 0.01 |
| Palliation of cholestasis | 27 (79.4%) | 62 (93.9%) | 33 (97.1%) | 0.03 |
| Patency (d)1 | 120 ± 16 | 59 ± 6 | 180 ± 20 | < 0.01 |
| Patency (d)2 | 97 (67-127) | 49 (27-71) | 167 (122-217) | |
| Procedure related cholangitis | 10 (29.4%) | 8 (12.1%) | 11 (32.4%) | 0.03 |
| Procedure related pancreatitis | 1 (2.9%) | 0 (0%) | 1 (2.9%) | 0.26 |
| Procedure related bleeding | 2 (5.9%) | 5 (7.6%) | 5 (14.7%) | 0.50 |
| Procedure related mortality | 0 | 0 | 0 | 1.00 |
| 30-d mortality | 0 (0%) | 1 (2.1%) | 1 (1.5%) | 0.26 |
Values expressed as mean ± SE.
Values expressed as median (range).
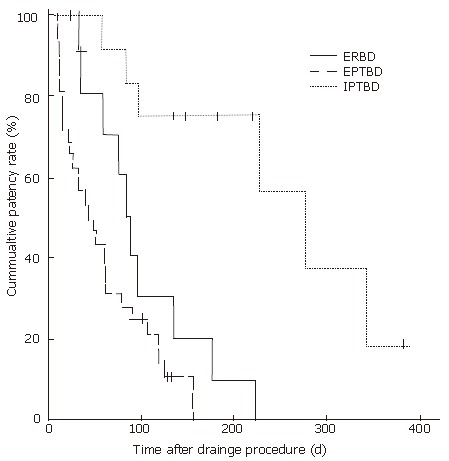
After the drainage procedure, the success rate of initial palliation for cholestasis was higher in either the EPTBD (93.9%) or IPTBD group (97.1%) compared to the ERBD group (79.4%) (P = 0.03) (Table 2). Figure 1 shows the comparison of cumulative patency rates for each drainage procedure. The mean duration of patency was longest in IPTBD followed by ERBD and EPTBD, 180 ± 20, 120 ± 16, and 59 ± 6 d respectively (P = 0.02 for IPTBD vs ERBD, P < 0.01 for ERBD vs EPTBD, P < 0.01 for IPTBD vs EPTBD) (Table 2). Cox regression analysis showed that the type of drainage procedure, such as ERBD (P < 0.01) and IPTBD (P < 0.01), was significantly associated with a longer patency. However, stent type or stent number (bilateral or unilateral) did not affect the patency rate (P = 0.74, P = 0.15, respectively). Procedure-related cholangitis occurred more frequently in ERBD or IPTBD compared to EPTBD (P = 0.03); however, it was usually controlled with antibiotics. There was no difference in other complication rates, such as bleeding, pancreatitis, and procedure-related mortality in comparisons of drainage procedures.
Figure 1.
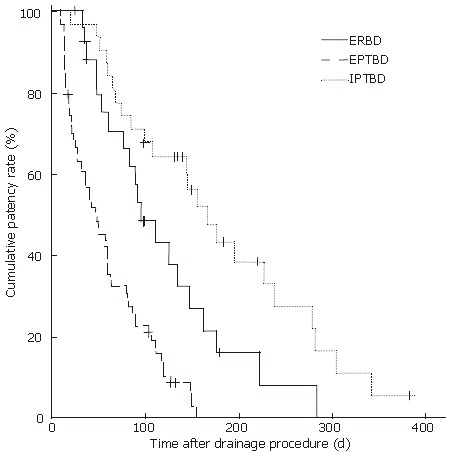
Kaplan-Meier estimation of cumulative patency rates of biliary drainage according to the procedures in all Bismuth types (P = 0.02 for ERBD vs IPTBD, P < 0.01 for ERBD vs EPTBD, P < 0.01 for IPTBD vs EPTBD). ERBD: endoscopic retrograde biliary drainage; EPTBD: external percutaneous transhepatic biliary drainage; IPTBD: internal biliary stenting via PTBD tract.
Bilateral drainage was performed in 45 patients (33.6%) and unilateral drainage in 89 patients (66.4%). There was a statistical difference in the number of inserted stents by the types of drainage procedures used (ERBD; 1.2 ± 0.1, EPTBD; 1.3 ± 0.1 and IPTBD; 1.6 ± 0.1, P < 0.01). Table 3 shows the clinical characteristics and the results comparing unilateral and bilateral drainage. There was no difference in age, sex, Bismuth type, type of stent, serum bilirubin level, success rate of initial palliation of cholestasis, and complication rate between the two groups. However, the IPTBD group received bilateral drainage procedures more frequently than the ERBD or EPTBD group. The mean duration of patency, regardless of stent type, was longer in patients with bilateral drainage than in patients with unilateral drainage (136 ± 16 d vs 88 ± 9 d, P = 0.01) (Table 3, Figure 2). However, Cox regression analysis did not show that the number of stents was an independent factor affecting the patency of the stent (P = 0.74). When duration of drainage patency was compared, between bilateral ERBD and bilateral IPTBD, there was no statistical difference in their mean patency duration between the two groups (110 ± 26 d vs 184 ± 24 d, respectively, P = 0.35).
Table 3.
Comparison of demographics and clinical outcome of patients according to number of stents
| Unilateral | Bilateral | P value | |
| Number of patients | 89 | 45 | |
| Age (yr)1 | 67.3 ± 1.0 | 67.2 ± 1.7 | 0.95 |
| Sex (M:F) | 63:26 | 30:15 | 0.77 |
| Bismuth type (II:III:IV) | 12:30:47 | 9:17:19 | 0.44 |
| Drainage method (ERBD:EPTBD:IPTBD) | 27:48:14 | 7:18:20 | < 0.01 |
| Type of stent (EPTBD:Plastic:Metal) | 48:25:16 | 18:23:04 | 0.03 |
| Serum bilirubin (mg/dL) (mg/L)1 | 12.42 ± 0.90 | 13.22 ± 7.29 | 0.59 |
| Palliation of cholestasis | 80 (89.9%) | 42 (93.3%) | 0.73 |
| Patency (d)1 | 88 ± 9 | 136 ± 16 | 0.01 |
| Patency (d)2 | 68 (45-91) | 112 (35-189) | |
| Procedure related cholangitis | 17 (19.1%) | 12 (26.7%) | 0.43 |
| Procedure related pancreatitis | 1 (1.1%) | 1 (2.3%) | 0.61 |
| Procedure related bleeding | 6 (6.7%) | 6 (13.3%) | 0.34 |
| Procedure related mortality | 0 | 0 | 1.00 |
| 30-d mortality | 2 (2.3%) | 0 (0%) | 0.79 |
Values expressed as mean ± SE.
Values expressed as median (range).
Figure 2.
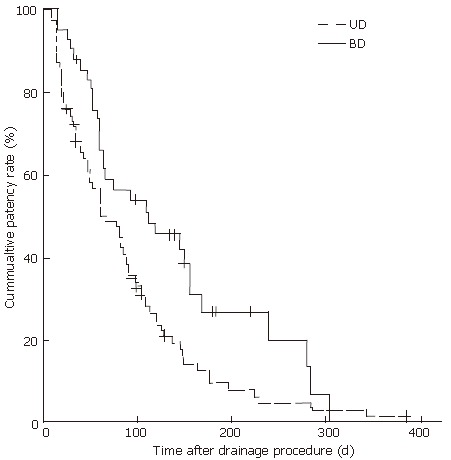
Comparison of cumulative patency rates of biliary drainage according to the number of stents (P = 0.01 between BD and UD). UD: unilateral drainage; BD: bilateral drainage.
A metal stent rather than a plastic stent was used more frequently in the IPTBD group compared to the ERBD group. A metal stent was inserted in all patients treated with IPTBD; however, it was used in 15 patients (44.1%) out of 34 patients treated with ERBD. The mean duration of drainage patency was longer in the metal stent group (168 ± 16 d) compared to the plastic stent group (109 ± 26 d) (P = 0.02). When the mean duration of patency of the metal stent was compared in the ERBD and IPTBD, there was no statistical difference between the two groups (145 ± 24 d vs 180 ± 20 d, respectively, P = 0.28).
Bismuth type II
In 21 patients with Bismuth type II, 6 patients underwent ERBD, 8 patients underwent EPTBD and 7 patients underwent IPTBD. There was no difference in age, sex or serum bilirubin levels among the types of drainage procedures. The success rate of initial palliation for cholestasis, cumulative patency rate of drainage (Figure 3), and complication rate after the procedure were not different based on the type of procedure. Cox regression analysis also showed that the type of drainage procedure (EPTBD vs ERBD P = 0.54, EPTBD vs IPTBD P = 0.66), stent type (P = 0.95) or stent number (P = 0.17) were not related to patency duration in Bismuth type II.
Figure 3.
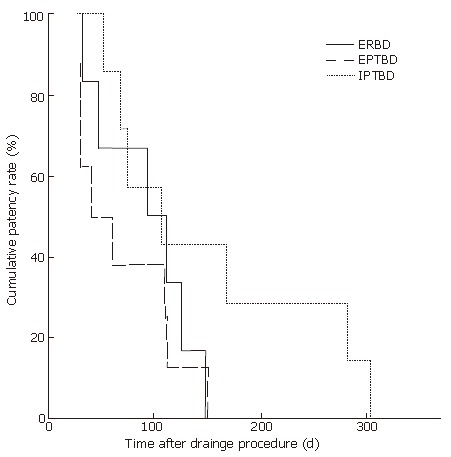
Kaplan-Meier estimation of cumulative patency rates for biliary drainage according to the procedures in patients with Bismuth type II Klatskin's tumor (P > 0.05 between drainage procedures ). ERBD: endoscopic retrograde biliary drainage; EPTBD: external percutaneous transhepatic biliary drainage; IPTBD: internal biliary stenting via PTBD tract.
Bismuth type III
In 47 patients with Bismuth type III, ERBD was performed in 12 patients, EPTBD in 23 patients and IPTBD in 12 patients. The parameters age, sex and serum bilirubin level were not different for different types of procedure. The initial success rate was comparable among all procedures (Table 4). However, the cumulative patency rate of drainage was different among the treatment methods. ERBD and IPTBD showed superior patency rates compared to EPTBD (mean duration of patency; 188 ± 47, 133 ± 21, and 53 ± 8 d respectively, P < 0.01). The cumulative patency rate for drainage in comparisons among procedures is shown in Figure 4. Procedure-related cholangitis occurred more frequently in patients who were treated with ERBD or IPTBD rather than with EPTBD only (P = 0.04) (Table 4). Cox regression analysis also showed that the type of drainage procedure was significantly associated with the duration of patency (ERBD P = 0.01 and IPTBD P < 0.01). However, there was no significant association with stent type (P = 0.60) or stent number (P = 0.07).
Table 4.
Comparison of clinical characteristics and clinical outcome according to drainage method in Bismuth type IIIpatients
| ERBD | EPTBD | IPTBD | P value | |
| Number of patients | 12 | 23 | 12 | |
| Age (yr)1 | 67.4 ± 3.1 | 67.0 ± 2.1 | 68.7 ± 2.5 | 0.89 |
| Sex (M:F) | 7:5 | 15:8 | 9:3 | 0.67 |
| Stent number1 | 1.1 ± 0.1 | 1.1 ± 0.1 | 1.7 ± 0.1 | < 0.01 |
| Serum bilirubin (mg/dL)1 | 10.72 ± 1.81 | 16.91 ± 2.14 | 11.13 ± 1.81 | 0.07 |
| Palliation of cholestasis | 9 (75%) | 22 (95.7%) | 12 (100%) | 0.12 |
| Patency (d)1 | 188 ± 47 | 53 ± 8 | 133 ± 21 | < 0.01 |
| Patency (d)2 | 163 (20-306) | 47 (7-87) | 145 (142-148) | |
| Procedure related cholangitis | 5 (41.7%) | 2 (8.7%) | 5 (41.7%) | 0.03 |
| Procedure related pancreatitis | 1 (8.3%) | 0 (0 %) | 1 (8.3%) | 0.26 |
| Procedure related bleeding | 0 (0%) | 2 (8.7%) | 3 (25%) | 0.14 |
| Procedure related mortality | 0 | 0 | 0 | 1.00 |
| 30-d mortality | 1 (8.3%) | 0 (0%) | 0 (0%) | 0.51 |
Values expressed as mean ± SE.
Values expressed as median (range).
Figure 4.
Comparison of cumulative patency rates for biliary drainage according to the procedures in patients with Bismuth type III (P = 0.23 for ERBD vs IPTBD; P < 0.01 for ERBD vs EPTBD; P < 0.01 for IPTBD vs EPTBD). ERBD: endoscopic retrograde biliary drainage; EPTBD: external percutaneous transhepatic biliary drainage; IPTBD: internal biliary stenting via PTBD tract.
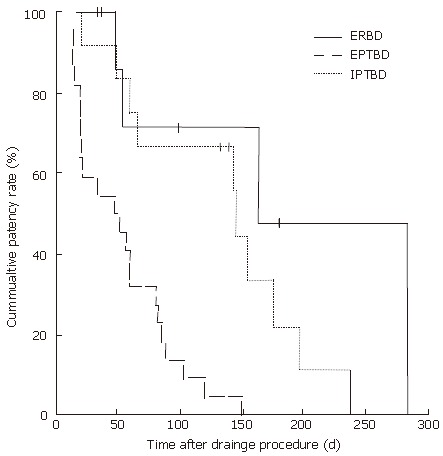
Bismuth type IV
There were 66 patients in the Bismuth type IV group. Sixteen patients were treated with ERBD, 35 patients with EPTBD, and 15 patients with IPTBD. Demographic and clinical characteristics were not different among groups classified by drainage procedures (Table 5). The initial success rate for the procedure or the procedure-related complication rate was not different for different types of procedure (Table 5). The patency rate for drainage was superior in the PTBDS group compared to the ERBD and PTBD groups (Figure 5). The mean duration of patency in patients treated with PTBDS, ERBD, and PTBD was 251 ± 36, 102 ± 19, and 60 ± 9 d, respectively (P < 0.01). Multivariate analysis also revealed that the type of drainage procedure, such as PTBDS, was significantly related to a longer patency (P < 0.01), but stent type (P = 0.55) or number (P = 0.68) was not associated with the duration of patency.
Table 5.
Comparison of demographics and clinical outcome according to drainage method in Bismuth type IV patients
| ERBD | EPTBD | IPTBD | P value | |
| Number of patients | 16 | 35 | 15 | |
| Age (yr)1 | 64.6 ± 3.6 | 67.1 ± 1.5 | 67.6 ± 2.5 | 0.68 |
| Sex (M:F) | 12:4 | 24:11 | 10:5 | 0.88 |
| Stent number1 | 1.1 ± 0.1 | 1.1 ± 0.4 | 1.6 ± 0.6 | 0.01 |
| Serum bilirubin (mg/dL)1 | 10.46 ± 1.75 | 13.99 ± 1.32 | 12.08 ± 1.86 | 0.29 |
| Palliation of cholestasis | 12 (75%) | 32 (93.4%) | 14 (93.3%) | 0.28 |
| Patency (d)1 | 102 ± 19 | 60 ± 9 | 251 ± 36 | < 0.01 |
| Patency (d)2 | 90 (69-111) | 43 (21-65) | 280 (171-389) | |
| Procedure related cholangitis | 3 (18.8%) | 4 (11.4%) | 5 (33.3%) | 0.16 |
| Procedure related pancreatitis | 0 (0%) | 0 (0%) | 0 (0%) | 1.00 |
| Procedure related bleeding | 1 (6.3%) | 3 (8.6%) | 2 (13.3%) | 0.55 |
| Procedure related mortality | 0 | 0 | 0 | 1.00 |
| 30-d mortality | 0 (0%) | 0 (0%) | 1 (1.5%) | 0.23 |
Values expressed as mean ± SE.
Values expressed as median (range).
Figure 5.
Cumulative patency rates for biliary drainage according to the procedures in patients with Bismuth type IV (P < 0.01 for ERBD vs IPTBD; P = 0.06 for ERBD vs EPTBD; P < 0.01 for IPTBD vs EPTBD). ERBD: endoscopic retrograde biliary drainage; EPTBD: external percutaneous transhepatic biliary drainage; IPTBD: internal biliary stenting via PTBD tract.
DISCUSSION
Successful biliary drainage after endoscopic stent insertion[15] or percutaneous transhepatic endoprostheses[16] can provide useful palliation of jaundice in patients with unresectable Klatskin’s tumor, and can improve the quality of life for these patients[17]. Currently, there is no consensus regarding the best method for jaundice palliation in patients with unresectable Klatskin’s tumor. In many centers, endoscopic stenting is considered as the first line of therapy for these patients because it is less invasive compared to the percutaneous approach. However, some have suggested that patients with Klatskin’s tumor are best treated by percutaneous placement of metallic stents[18]. This is because the endoscopic approach can cause cholangitis, and selective endoscopic stenting into the appropriate bile duct is technically difficult[19]. It is assumed that the relatively low level of biliary obstruction in patients with Klatskin’s tumor of Bismuth typeIor II, can be easily managed by endoscopic stenting. However, the percutaneous approach is more appropriate for patients with a higher level of obstruction; i.e., Bismuth type III or IV. ERCP can cause more frequent cholangitis due to an undrained biliary segment after dye injection. Therefore, the most effective methods of palliative biliary drainage may differ according to the type or level of biliary obstruction in patients with unresectable Klatskin’s tumor. However, there have been no studies investigating this issue to date.
In this study, the initial success rate for palliation of cholestasis in the ERBD group compared with the PTBD or PTBDS group was the same for Bismuth type II; however, it was lower for Bismuth type III or IV. This result might be explained by the difficulty of selective endoscopic stenting in patients with Bismuth type III or IV Klatskin’s tumor. Procedure-related cholangitis occurred more frequently after ERBD or PTBDS compared to PTBD in patients with Bismuth type III and IV. During stent insertion in these patients, cholangitis tends to occur when contrast dye is injected into the peripheral hepatic ducts, which can not be successfully drained subsequently[20]. However, the infection was successfully controlled with antibiotics in this study. The current study showed a similar rate of cholangitis in the ERBD and PTBDS groups and a different retrospective review of 59 patients with unresectable Klatskin’s tumor showed that endoscopically placed stents caused fewer acute complications than percutaneously placed stents (11% vs 33%)[13].
In this study, adequate initial relief of jaundice was achieved in 91% of the patients. The success rate of palliation for cholestasis with ERBD or use of a percutaneous metal stent has been previously reported to be 41%-88%[10,11,14,20-25] and 61%-100%[26-29], respectively, Our findings are consistent with these prior studies; i.e., 79.4% in ERBD and 97.1% in IPTBD. However, there is no prior report on comparisons of success rates with ERBD and IPTBD from the same center; this is the first study on the efficacy of ERBD, EPTBD, and IPTBD.
After the initial intervention for biliary drainage, the duration of patency of ERBD was comparable to IPTBD in Bismuth type II and III, but was not as good as PTBDS in Bismuth type IV. Selective stenting into the most optimal bile duct during ERBD is not difficult for patients with Bismuth type II and III; however, it is difficult in Bismuth type IV. The difference of bile duct accessibility, according to the level of biliary obstruction in ERBD and IPTBD, may contribute to the difference in long-term patency results. The patency rate in IPTBD in Bismuth type IV was much longer than for type II or III, likely due to bilateral metal stents being mainly used in Bismuth type IV.
Although the EPTBD group showed a high initial success rate, and a low infection rate because there were no further interventional procedures in this study, the quality of life with an EPTBD tube was not satisfactory compared to the ERBD or IPTBD. Moreover, the cumulative patency rate of the EPTBD was the shortest compared to ERBD or IPTBD, especially in Bismuth type III or IV of unresectable Klatskin’s tumor. This result might be due to the relatively small caliber of the EPTBD tube, and accidental removal of an EPTBD tube as a result of the difficulty of tube care. In 62 patients treated with EPTBD, 19 patients (30.6%) required an additional drainage procedure within 30 d due to the retracted EPTBD tube. Therefore, for a biliary drainage procedure, EPTBD without internal stent insertion should be considered when patient survival is limited.
IPTBD showed the best result in duration of patency in patients overall. This excellent result for IPTBD, especially in Bismuth type IV, may be explained by relatively easy access for optimal bile duct drainage, and by the use of a large diameter metal stent. Therefore, whenever possible, internal stent insertion through the PTBD tract is recommended after the initial PTBD procedure.
It is generally accepted that a metal stent is better than a plastic stent in patency. Therefore, metal stenting is recommended if long survival is expected. Though the mean duration of drainage patency tended to be longer for the metal stent (168 ± 16 d) compared to the plastic stent (109 ± 26 d) in this study, multivariate analysis revealed that stent type was not an important factor for patency. The mean duration for metal stent patency of ERBD has been reported to range from 103 to 169 d and that for the IPTBD from 126 d to 365 d[11,20,22,23]. However, no prior study has compared the patency of metal stents based on their insertion method. When metal stent patency was compared according to insertion method in this series, there was no difference observed between ERBD and IPTBD (145 ± 24 d and 180 ± 20 d, respectively).
There has been debate on whether bilateral drainage is better than unilateral drainage in unresectable Klatskin’s tumor. One study showed that drainage of 25% of the liver volume can achieve adequate palliation with improvement in biochemical parameters, biliary decompression, and relief of symptoms with improved quality of life[30]. Others have shown that more than one endoprosthesis would not appear to be justified as a routine procedure in patients with malignant hilar biliary obstruction[31]. Therefore, it has been argued that any duct that is technically easiest for drainage, should be selected for stenting[11]. However, another study showed that for the cumulative patency rate, bilateral drainage was superior to unilateral drainage in Bismuth type IV obstruction[26]. The best survival has been reported for patients with bilateral drainage and the worst survival for patients with cholangiographic opacification of both lobes after drainage of only one lobe[20]. However, an advantage for bilateral drainage in survival has not been confirmed in prospective studies to date. In the current study univariate analysis revealed that patency of bilateral stents persists longer than patency of unilateral stents (136± 16 d vs 88 ± 9 d), however, multivariate analysis showed that stent number was not associated with the overall patency rate.
Our study has some limitations. It is a non-randomized, retrospective study without pre-defined follow-up protocol. However, since each treatment method for biliary drainage was chosen according to availability of experienced endoscopists, regardless of patient’s characteristics, randomization was achieved to a certain degree.
In summary, for the palliation of jaundice in patients with unresectable Klatskin’s tumor, the biliary obstruction pattern, such as Bismuth type, should be considered before selection of an optimal drainage method. ERBD is recommended as the first-line drainage procedure in Bismuth type II or III, considering its efficacy and relative noninvasiveness. However, internal stent insertion through the PTBD tract is the best option for Bismuth type IV.
Footnotes
Supported by a grant No. 2120040320 from the Seoul National University Hospital Research Fund
S- Editor Zhu LH L- Editor Lutze M E- Editor Wang HF
References
- 1.Altaee MY, Johnson PJ, Farrant JM, Williams R. Etiologic and clinical characteristics of peripheral and hilar cholangiocarcinoma. Cancer. 1991;68:2051–2055. doi: 10.1002/1097-0142(19911101)68:9<2051::aid-cncr2820680934>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 2.Jarnagin WR. Cholangiocarcinoma of the extrahepatic bile ducts. Semin Surg Oncol. 2000;19:156–176. doi: 10.1002/1098-2388(200009)19:2<156::aid-ssu8>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 3.Chamberlain RS, Blumgart LH. Hilar cholangiocarcinoma: a review and commentary. Ann Surg Oncol. 2000;7:55–66. doi: 10.1007/s10434-000-0055-4. [DOI] [PubMed] [Google Scholar]
- 4.Van Leeuwen DJ, Huibregtse K, Tytgat GN. Carcinoma of the hepatic confluence 25 years after Klatskin's description: diagnosis and endoscopic management. Semin Liver Dis. 1990;10:102–113. doi: 10.1055/s-2008-1040462. [DOI] [PubMed] [Google Scholar]
- 5.Juttijudata P, Chiemchaisri C, Palavatana C, Churnratanakul S. Causes of cholestasis in Thailand. A study of 276 consecutive patients. Am J Surg. 1984;147:360–366. doi: 10.1016/0002-9610(84)90167-3. [DOI] [PubMed] [Google Scholar]
- 6.Khan SA, Thomas HC, Davidson BR, Taylor-Robinson SD. Cholangiocarcinoma. Lancet. 2005;366:1303–1314. doi: 10.1016/S0140-6736(05)67530-7. [DOI] [PubMed] [Google Scholar]
- 7.McGlynn KA, Tarone RE, El-Serag HB. A comparison of trends in the incidence of hepatocellular carcinoma and intrahepatic cholangiocarcinoma in the United States. Cancer Epidemiol Biomarkers Prev. 2006;15:1198–1203. doi: 10.1158/1055-9965.EPI-05-0811. [DOI] [PubMed] [Google Scholar]
- 8.Bismuth H, Castaing D, Traynor O. Resection or palliation: priority of surgery in the treatment of hilar cancer. World J Surg. 1988;12:39–47. doi: 10.1007/BF01658484. [DOI] [PubMed] [Google Scholar]
- 9.Byrnes V, Afdhal N. Cholangiocarcinoma of the Hepatic Hilum (Klatskin Tumor) Curr Treat Options Gastroenterol. 2002;5:87–94. doi: 10.1007/s11938-002-0055-5. [DOI] [PubMed] [Google Scholar]
- 10.Gerhards MF, den Hartog D, Rauws EA, van Gulik TM, González González D, Lameris JS, de Wit LT, Gouma DJ. Palliative treatment in patients with unresectable hilar cholangiocarcinoma: results of endoscopic drainage in patients with type III and IV hilar cholangiocarcinoma. Eur J Surg. 2001;167:274–280. doi: 10.1080/110241501300091444. [DOI] [PubMed] [Google Scholar]
- 11.De Palma GD, Galloro G, Siciliano S, Iovino P, Catanzano C. Unilateral versus bilateral endoscopic hepatic duct drainage in patients with malignant hilar biliary obstruction: results of a prospective, randomized, and controlled study. Gastrointest Endosc. 2001;53:547–553. doi: 10.1067/mge.2001.113381. [DOI] [PubMed] [Google Scholar]
- 12.Nordback IH, Pitt HA, Coleman J, Venbrux AC, Dooley WC, Yeu NN, Cameron JL. Unresectable hilar cholangiocarcinoma: percutaneous versus operative palliation. Surgery. 1994;115:597–603. [PubMed] [Google Scholar]
- 13.Born P, Rösch T, Brühl K, Sandschin W, Weigert N, Ott R, Frimberger E, Allescher HD, Hoffmann W, Neuhaus H, et al. Long-term outcome in patients with advanced hilar bile duct tumors undergoing palliative endoscopic or percutaneous drainage. Z Gastroenterol. 2000;38:483–489. doi: 10.1055/s-2000-14886. [DOI] [PubMed] [Google Scholar]
- 14.Freeman ML, Overby C. Selective MRCP and CT-targeted drainage of malignant hilar biliary obstruction with self-expanding metallic stents. Gastrointest Endosc. 2003;58:41–49. doi: 10.1067/mge.2003.292. [DOI] [PubMed] [Google Scholar]
- 15.Lai EC, Chu KM, Lo CY, Fan ST, Lo CM, Wong J. Choice of palliation for malignant hilar biliary obstruction. Am J Surg. 1992;163:208–212. doi: 10.1016/0002-9610(92)90102-w. [DOI] [PubMed] [Google Scholar]
- 16.Magistrelli P, Masetti R, Coppola R, Coco C, Antinori A, Nuzzo G, Picciocchi A. Changing attitudes in the palliation of proximal malignant biliary obstruction. J Surg Oncol Suppl. 1993;3:151–153. doi: 10.1002/jso.2930530539. [DOI] [PubMed] [Google Scholar]
- 17.Abraham NS, Barkun JS, Barkun AN. Palliation of malignant biliary obstruction: a prospective trial examining impact on quality of life. Gastrointest Endosc. 2002;56:835–841. doi: 10.1067/mge.2002.129868. [DOI] [PubMed] [Google Scholar]
- 18.Cowling MG, Adam AN. Internal stenting in malignant biliary obstruction. World J Surg. 2001;25:355–359; discussion 359-361. doi: 10.1007/s002680020384. [DOI] [PubMed] [Google Scholar]
- 19.Deviere J, Baize M, de Toeuf J, Cremer M. Long-term follow-up of patients with hilar malignant stricture treated by endoscopic internal biliary drainage. Gastrointest Endosc. 1988;34:95–101. doi: 10.1016/s0016-5107(88)71271-7. [DOI] [PubMed] [Google Scholar]
- 20.Chang WH, Kortan P, Haber GB. Outcome in patients with bifurcation tumors who undergo unilateral versus bilateral hepatic duct drainage. Gastrointest Endosc. 1998;47:354–362. doi: 10.1016/s0016-5107(98)70218-4. [DOI] [PubMed] [Google Scholar]
- 21.Liu CL, Lo CM, Lai EC, Fan ST. Endoscopic retrograde cholangiopancreatography and endoscopic endoprosthesis insertion in patients with Klatskin tumors. Arch Surg. 1998;133:293–296. doi: 10.1001/archsurg.133.3.293. [DOI] [PubMed] [Google Scholar]
- 22.Cheng JL, Bruno MJ, Bergman JJ, Rauws EA, Tytgat GN, Huibregtse K. Endoscopic palliation of patients with biliary obstruction caused by nonresectable hilar cholangiocarcinoma: efficacy of self-expandable metallic Wallstents. Gastrointest Endosc. 2002;56:33–39. doi: 10.1067/mge.2002.125364. [DOI] [PubMed] [Google Scholar]
- 23.De Palma GD, Pezzullo A, Rega M, Persico M, Patrone F, Mastantuono L, Persico G. Unilateral placement of metallic stents for malignant hilar obstruction: a prospective study. Gastrointest Endosc. 2003;58:50–53. doi: 10.1067/mge.2003.310. [DOI] [PubMed] [Google Scholar]
- 24.Rerknimitr R, Kladcharoen N, Mahachai V, Kullavanijaya P. Result of endoscopic biliary drainage in hilar cholangiocarcinoma. J Clin Gastroenterol. 2004;38:518–523. doi: 10.1097/01.mcg.0000123204.36471.be. [DOI] [PubMed] [Google Scholar]
- 25.Peters RA, Williams SG, Lombard M, Karani J, Westaby D. The management of high-grade hilar strictures by endoscopic insertion of self-expanding metal endoprostheses. Endoscopy. 1997;29:10–16. doi: 10.1055/s-2007-1004054. [DOI] [PubMed] [Google Scholar]
- 26.Inal M, Akgül E, Aksungur E, Seydaoğlu G. Percutaneous placement of biliary metallic stents in patients with malignant hilar obstruction: unilobar versus bilobar drainage. J Vasc Interv Radiol. 2003;14:1409–1416. doi: 10.1097/01.rvi.0000096762.74047.a6. [DOI] [PubMed] [Google Scholar]
- 27.Wagner HJ, Knyrim K, Vakil N, Klose KJ. Plastic endoprostheses versus metal stents in the palliative treatment of malignant hilar biliary obstruction. A prospective and randomized trial. Endoscopy. 1993;25:213–218. doi: 10.1055/s-2007-1010295. [DOI] [PubMed] [Google Scholar]
- 28.Stoker J, Laméris JS, van Blankenstein M. Percutaneous metallic self-expandable endoprostheses in malignant hilar biliary obstruction. Gastrointest Endosc. 1993;39:43–49. doi: 10.1016/s0016-5107(93)70009-7. [DOI] [PubMed] [Google Scholar]
- 29.Lee BH, Choe DH, Lee JH, Kim KH, Chin SY. Metallic stents in malignant biliary obstruction: prospective long-term clinical results. AJR Am J Roentgenol. 1997;168:741–745. doi: 10.2214/ajr.168.3.9057527. [DOI] [PubMed] [Google Scholar]
- 30.Dowsett JF, Vaira D, Hatfield AR, Cairns SR, Polydorou A, Frost R, Croker J, Cotton PB, Russell RC, Mason RR. Endoscopic biliary therapy using the combined percutaneous and endoscopic technique. Gastroenterology. 1989;96:1180–1186. doi: 10.1016/0016-5085(89)91639-9. [DOI] [PubMed] [Google Scholar]
- 31.Polydorou AA, Cairns SR, Dowsett JF, Hatfield AR, Salmon PR, Cotton PB, Russell RC. Palliation of proximal malignant biliary obstruction by endoscopic endoprosthesis insertion. Gut. 1991;32:685–689. doi: 10.1136/gut.32.6.685. [DOI] [PMC free article] [PubMed] [Google Scholar]


