Abstract
Context
Palliative care patients and their family caregivers may have a foreshortened perspective of time left to live, or the expectation of the patient’s death in the near future. Patients and caregivers may report distress in physical, psychological, or existential/spiritual realms.
Objectives
To conduct a randomized controlled trial examining the effectiveness of retired senior volunteers (RSVs) in delivering a reminiscence and creative activity intervention aimed at alleviating palliative care patient and caregiver distress.
Methods
Of the 45 dyads that completed baseline, 28 completed post-intervention and 24 completed follow-up. The intervention group received three home visits by RSVs; control group families received three supportive telephone calls by research staff. Measures included symptom assessment and associated burden, depression, religiousness/spirituality, and meaning in life.
Results
Patients in the intervention group reported a significantly greater reduction in frequency of emotional symptoms (P = 0.02) and emotional symptom bother (P = 0.04) than the control group, as well as improved spiritual functioning. Family caregivers in the intervention group were more likely than control caregivers to endorse items on the Meaning in Life Scale (P = 0.02). Only improvement in intervention patients’ emotional symptom bother maintained at follow-up after discontinuing RSV contact (P = 0.024).
Conclusion
Delivery of the intervention by RSVs had a positive impact on palliative care patients’ emotional symptoms and burden and caregivers’ meaning in life. Meaningful prolonged engagement with palliative care patients and caregivers, possibly through alternative modes of treatment delivery such as continued RSV contact, may be necessary for maintenance of therapeutic effects.
Keywords: Community-based RCT, palliative care dyads, volunteers, mixed methods
Introduction
Palliative care patients and other vulnerable populations may have a foreshortened perspective of time left to live1 and report distress in multiple realms. Chochinov and colleagues2 found that palliative care patients’ existential distress was associated with patient characteristics, but was even more strongly related to spirituality and a sense of meaning and purpose. Meaning reconstruction,3,4 spirituality and religious coping have been identified as potential therapeutic tools to enhance intervention effects.5,6 For example, Randall and Bishop6 found that the relationship between religion and valuation of life was partially mediated by forgiveness.
Interventions to improve the lives of palliative care patients and caregivers frequently use reminiscence, or the concept of preserving dignity, as a therapeutic tool.7–13 Through focusing individuals’ attention on lifetime accomplishments, relationships and values, techniques such as life review/reminiscence facilitate meaning reconstruction and reduce symptoms of depression.3,14 The most widely studied of these interventions is Chochinov’s Dignity Therapy.10,12 McClement and colleagues13 reported that 95% of bereaved family members perceived their loved one’s participation in Dignity Therapy as beneficial, 78% reported that the “generativity document” helped their grief process, and 95% would recommend Dignity Therapy to others. In a randomized controlled trial (RCT), Chochinov and colleagues12 found that Dignity Therapy improved spiritual well-being and was perceived as more helpful than standard palliative or client-centered care.
A Cochrane review of eleven diverse interventions targeting palliative caregivers15 found weak evidence for therapeutic effect and highlighted the need for greater methodological rigor in future studies. In our prior work,7,8 social work and psychology graduate students with bachelor’s or master’s degrees were trained to deliver a three-session, home-based reminiscence and creative activity intervention to palliative care patients and their family caregivers. The intervention improved palliative patients’ sense of meaning, reduced their physical symptom burden, and improved their family caregivers’ levels of stress relative to a control group. Fidelity data evaluated by a specialist in evidence-based treatment outcomes revealed accuracy of treatment delivery averaged 91.55%.
Although hospice and palliative care social workers frequently use reminiscence and creative activities with their patients,16 such interventions need to be more accessible to patients and families transitioning from community, hospital, and palliative care settings. If hospice or palliative care is not chosen as a treatment option, few means of delivering therapeutic reminiscence-based interventions exist. This represents a significant gap in practice and in the psychosocial palliative care intervention literature. Kazdin and Blase17 argue cogently that the community need for mental health services far outstrips the number of providers available to assist those in distress. They call strongly for new intervention delivery modes targeting prevention and treatment to alleviate suffering. Hence, the purpose of the present study was to evaluate the effectiveness of retired senior volunteers (RSVs), who are available nationally through the national Senior Corps program, to deliver a three-session reminiscence and creative activity intervention previously found effective in improving palliative care patient and caregiver outcomes.7,8 We hypothesized that palliative care patients and their caregivers in the RSV-delivered intervention group would demonstrate improved emotional and spiritual functioning relative to a supportive contact control group. If successful, this mode of treatment delivery (RSV intervention) would represent a significant step toward translation and greater access at earlier disease stages of therapeutic psychosocial interventions for individuals near the end of life and their family members.
Methods
Data were collected between June 2009 and December 2011 with approval from the University of Alabama and the University of Alabama at Birmingham Institutional Review Boards. A variety of methods were used for palliative care patient/caregiver dyad recruitment through physicians/clinical champions at two university medical centers, one home health agency, five assisted living facilities, four congregate apartment sites for older adults and those with low income, one continuing care retirement community, and one rehabilitation unit in a local skilled nursing facility. Sixty-six percent of the dyads were physician-referred. A community recruiter and advertisements in community and university print news media also were used.
Patient/Caregiver Screening and Group Assignment
After clinical champions at recruitment sites explained the main components of the project, patients provided verbal consent to have their contact information forwarded to research staff. Next, research staff telephoned patients who had expressed interest, described the project in more detail, and, after getting verbal consent, administered the screening measures (basic demographics, the Vulnerable Elders Survey-13 [VES],18,19 the Telephone Interview for Cognitive Status-modified [TICS-m]20,21) over the telephone. Eligible patients directly nominated a “family” caregiver (related by blood or marriage or fictive kin) for study participation.
Palliative care patients were eligible if they: 1) were age 55 or older; 2) were living in the community or assisted living; 3) had an advanced illness or combination of chronic illnesses; 4) received a score of three or greater on the VES;18,19 5) had no more than mild cognitive impairment as measured by a score of 17 or greater on the TICS-m;20,21 6) received an average of four hours per week of care from a caregiver; and 7) read and spoke English.
Caregivers were eligible if they: 1) were identified by an eligible palliative care patient; 2) were over age 19 (Alabama’s age of majority); 3) were providing an average of four hours per week of care for the patient; 4) were cognitively intact as measured by a score of 28 or greater on the TICS-m;20,21 5) lived nearby; and 6) read and spoke English.
Dyads were excluded if the patient was receiving hospice care or if either individual had schizophrenia or bipolar disorder or had a nursing home admission planned within three months.
Retired Senior Volunteers
Retired senior volunteers (RSVs) were participants in the national Senior Corps program, part of the Corporation for National and Community Service. They were recruited from FOCUS on Senior Citizens in Tuscaloosa, AL, and Positive Maturity in Birmingham, AL. The RSV program is open to all U.S. citizens, nationals, or lawful permanent resident aliens aged 55 or older (http://www.nationalservice.gov/programs/senior-corps/rsvp). Within this program, volunteers receive standard pre-service orientation and training, supplemental insurance while on duty, and, potentially, reimbursement for costs such as travel incurred during service. RSVs receive no pay for the services they perform. In this study, RSVs were included if they: 1) had a high school education; 2) read and spoke English; and 3) had a car and drove independently.
Measures
Other than patient screening instruments, patient and caregiver assessments were completed in the patient’s home at baseline, post-intervention, and follow-up. Demographics included age, race/ethnicity, education and income adequacy, assessing difficulty paying for basic needs with response options ranging from 1 = not at all difficult to 4 = very difficult.
Patient Health and Cognitive Screening by Phone
The VES-1318,19 assesses risk of functional decline and death. Items assess age, self-rated health, limitation in physical function, and functional disabilities, with scores ranging from 0 to 10. Higher scores indicate greater risk. Saliba et al.16 found that 32% of older adults in the nationally representative Medicare Current Beneficiary Survey were considered vulnerable, with a score of three or greater of ten, and this group had 4.2 times the risk of death or functional decline over a two-year period. Further validation of the VES has shown that, among community-dwelling older adults with a VES score of three or higher, the estimated combined risk of death and functional decline within 11 months rose from 23% among older adults with VES = 3 to 60% among older adults with VES = 10.15
The TICS-m20,21 detects cognitive impairment, with scores ranging from 0 to 50. Scores of < 21 have been compared to scores of < 2521 on the Mini-Mental State Examination,22 indicating clinically significant cognitive impairment.
Patient and Caregiver Assessments Administered in Person
The Future Time Perspective Scale23 assesses individual’s motivation and approach to life based on time perspective and was administered to patients and caregivers only at baseline. Ten items with alpha of 0.92, assessed on a 7-point Likert-type scale, are summed; higher scores indicate an increasingly expansive time perspective.
The Center for Epidemiological Studies-Depression Scale (CES-D)24 asks about the frequency of depressive symptoms within the past week, with a score of 16 or greater indicating clinically significant levels of depression. The CES-D has good internal consistency: Cronbach’s alpha = 0.73 to 0.81.25
The Positive and Negative Affect Schedule (PANAS)26 queries participants about their current feelings regarding 10 positive and 10 negative adjectives. Item responses range from very slightly or not at all to extremely, with higher scores indicating more intense affect. The PANAS has good internal consistency for the positive affect (PA; Cronbach’s alpha = 0.84) and negative affect (NA; Cronbach’s alpha = 0.87) scales. The two scales have good discriminant validity, r = −0.09.
Patients and caregivers independently rated the patient’s physical and psychological symptoms and associated distress using the Memorial Symptom Assessment Scale-Short Form (MSAS-SF).27 Higher scores in the symptom category indicate the presence of more patient symptoms whereas higher bother scores indicate greater patient distress related to symptoms. Cronbach’s alpha coefficients for the MSAS-SF subscales range from 0.76 to 0.87.
The Brief Multidimensional Measure of Religiousness and Spirituality (BMMRS)28 was used to examine: 1) patient forgiveness (three items; α = 0.75), asking how often the patient has forgiven themselves, others, or experienced God’s forgiveness. Higher scores indicate greater frequency of forgiveness; 2) religious struggle (one item): “I wonder whether God has abandoned me?” Higher scores indicate greater agreement with the item; and 3) religious meaning (two items): “The events in my life unfold according to a divine or greater plan” and “I have a sense of mission or calling in my own life” (α = 0.64). Higher scores indicate greater agreement with the items.
Meaning in Life Scale:29,30 This eight-item scale assessed four domains: values, purpose, goals, and reflections. Higher scores indicate greater meaning. Cronbach’s alpha = 0.856.31
Caregiver Stressors Scale-Revised.32 Caregivers completed this measure of perceptions of competency, strain, role overload, role captivity, and emotional control, with higher scores indicating greater caregiving stress. Internal consistency estimates range from 0.60 to 0.82, with stability coefficients ranging from 0.61 to 0.74.
Positive Aspects of Caregiving (PAC).33 This scale assesses caregivers’ perceived gains from providing care, with higher scores indicating more positive aspects of caregiving (Cronbach’s alpha = 0.88).
Procedures
This RCT compared the RSV-delivered intervention to a supportive telephone contact control delivered by research staff. Prior experience in dealing with terminal illness was not an eligibility criterion for RSVs or for research staff. However, RSVs indicated if there were any type of advanced chronic illness they would prefer to avoid when being assigned a patient-caregiver dyad. Whereas RSVs were over age 55 and had at least a high school education, all research staff members were under 40 and had completed at least a bachelor’s degree in social/behavioral science or nursing. Our objective in this RCT was to determine whether RSVs could be trained to effectively deliver the reminiscence and creative activity intervention. Thus, the RSVs and research staff did not need to be similar. In translation to the community, there will only be dyads receiving the intervention from RSVs.14
Patient and caregiver written informed consent was obtained at baseline. After baseline, dyads were stratified by race and site and randomly assigned to the intervention or control condition. RSVs were asked to audiorecord the final intervention session for evaluation of treatment acceptability by palliative care patients and caregivers.
Baseline and post-intervention assessments were completed in separate, concurrent interviews with research staff not involved in providing control calls. Post-intervention assessments occurred approximately one week after completion of intervention or control contacts, 15 to 20 weeks post-baseline. Qualitative content analysis was used to examine treatment acceptability. Follow-up assessments for both groups were completed 13 to 14 weeks after the post-intervention assessments. There was no difference between intervention and control groups on timing between baseline, post-intervention, and follow-up assessments. Patients and caregivers each received $20 for completing baseline, post-intervention, and follow-up assessments for a total of $60 for the patient and $60 for the caregiver.
RSV-Delivered LIFE Intervention Group.8
Prior to delivering the manualized intervention, RSVs received intensive training (approximately four to six hours over two sessions), that included reading materials, structured role-play, and practice opportunities observed by a licensed clinical psychologist (R.S.A.). Research staff were on call for consultation with RSVs. The LIFE Volunteer Interventionist Manual and LIFE Participant Notebook have Flesch-Kincaid grade levels of 7.0 with a Flesch Reading Ease rating of 68.7% and were available in 14-point font. The manual and accompanying workbook comprise: 1) instructions about using the steps of problem solving34 to decide on a period of life and creative activity project; 2) constructing a project; 3) evaluation of the activity; and 4) an appendix with life review questions for dyads that find generation of stories more difficult.
With the help of the RSV, in session one the patient-caregiver dyad narrowed the focus to a time period in the patient’s life that could be adequately represented in one tangible project (e.g., scrapbook, cookbook, audiotapes) to represent the patient’s values and achievements in life (see Appendix for question prompts). The RSV and dyad actively brainstormed ways to portray the life story; then the RSV helped the dyad further narrow the focus to one meaningful project, directing the dyad to the LIFE Participant Notebook for tips in project construction. The dyad was asked to gather all necessary materials (such as pictures, recipes, stories from other family members) and actively work on completing a portion of the project between each session with the RSV.
During the second session, RSVs helped the dyad work on the activity and further use problem-solving skills. During the third visit, the patient and caregiver shared their activity with the RSV, who discussed the dyad’s feelings about the process, including a qualitative evaluation of the LIFE project and what the family learned when creating it.
RSVs were carefully trained to monitor dyads’ reactions. If either member of the dyad reacted in a persistently negative manner to the intervention, the activity was discontinued. RSVs were taught to look for depression in the following ways: look for a saddened face, crying, shaky voice, statement from the caregiver that the care recipient seems depressed (e.g., downtrodden, sad, blue). The LIFE Volunteer Interventionist Manual includes “Feelings Checks” in which the RSVs ask, “How does talking about these memories make you feel?” The average treatment fidelity score achieved by RSVs during training was 89.8%.
Patient-caregiver dyads received $25 to offset the costs of purchasing materials (e.g., photo albums, scrapbooks, photograph printing paper, etc.) desired for the project. Research team members purchased and delivered materials to mobility restricted dyads.
Supportive Telephone Contact Control Group
Patients and caregivers each received three separate, structured emotional support telephone calls with research staff (mean±SD duration = 13±6.5 minutes) to minimize differential drop-out with the RSV intervention group. Control callers asked questions of participants and then engaged in supportive conversations using empathic listening and reflection. Topics discussed included family, intergenerational ties, and important aspects of the patient’s life, but structured reminiscence and the creative and therapeutic nature of legacy activities were not discussed.
Results
Sample Characteristics
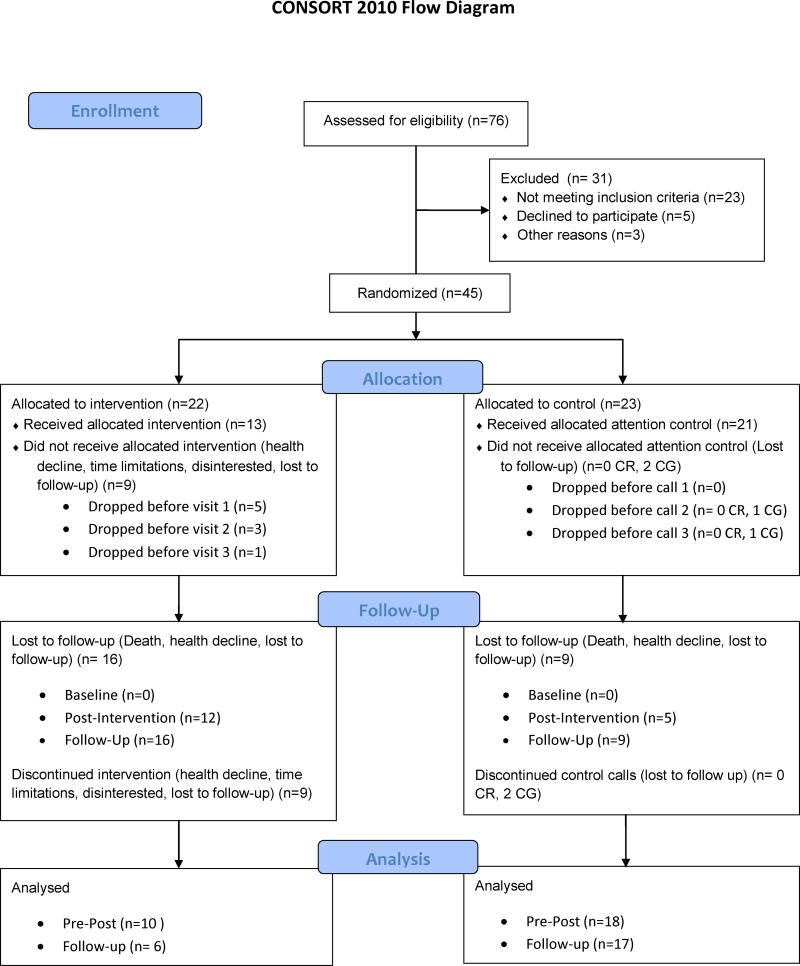
Two hundred fifty-six dyads were referred and received at least a letter or telephone contact to gauge eligibility and interest in participaton. Seventy-six dyads completed screening and were eligible, 45 (59%) completed baseline, 28 completed post-intervention (62% of baseline), and 24 completed follow-up assessments (86% of post-intervention). As shown in Fig. 1, reasons for discontinuation from baseline to post-intervention and follow-up included patient health decline or death (43%), inability to re-contact (24%), caregiver absence (19%), and loss of interest (14%). Demographic characteristics at baseline and post-intervention are presented in Table 1; there were no significant differences between dyads who began the study and completers. Patients reported a median of two chronic illnesses at baseline; 18% reported three or more chronic conditions. The most commonly reported illnesses were central nervous system disorders, pain/arthritis, diabetes, cancer and heart disease.
Fig. 1.
CONSORT flow diagram.
Table 1.
Patient and Caregiver Characteristics (SD) at Baseline (n = 45) and Post-Intervention (n = 28).
| Baseline | Post-Intervention | |||
|---|---|---|---|---|
|
| ||||
| Patient | Caregiver | Patient | Caregiver | |
| Age, yrs | 78.22 (11.59) | 59.85 (11.76) | 77.5 (12.13) | 60.71 (11.02) |
| Gender | ||||
| Women | 82% | 71% | 82% | 68% |
| Race/ethnicity | ||||
| African American | 40% | 44% | 43% | 43% |
| Education, yrs | 12.45 (4.05) | 13.53 (2.74) | 12.48 (4.25) | 13.71 (3.24) |
| Income Adequacy | -- | 2.84 (1.01) | -- | 2.89 (.93) |
| VES | 7.29 (1.95) | -- | 7.0 (2.31) | -- |
| TICS-m | 25.49 (4.85) | 32.51 (4.57) | 26.04 (4.80) | 32.43 (4.20) |
Note: There were no significant differences in baseline and post-intervention patient or caregiver characteristics.
VES = Vulnerable Elders Survey-13; TICS-m = Telephone Interview for Cognitive Status-modified.
Caregivers had varied relationships with patients including adult child (44.4%), spouse (17.8%), other family (i.e., sibling, grandchild, or niece/nephew) (11.1%), friend (4.4%) or paid (2.2%). Nine caregivers (20%) did not report their relationship. Caregivers rated their health as “good,” on average.
Other than patient health (VES-13),18,19 there were no differences based on random assignment to the intervention or control group. Intervention group patients scored higher on the VES than control group patients, t(26) = 2.89, P = 0.008, and were considered more ill. Therefore, patient health was entered as a covariate in outcome analyses. Patient and caregiver scores at baseline and post-intervention assessments appear as Table 2.
Table 2.
Characteristics of Patients and Caregivers Who Completed LIFE
| Participant Characteristics | Experimental Condition
|
|||
|---|---|---|---|---|
| Intervention Group (n = 10 dyads) | Control Group (n = 18 dyads) | |||
|
| ||||
| Baseline | Post | Baseline | Post | |
| Caregiver | ||||
| MSAS –Symptom Number | ||||
| Physical | 9.86 (4.2) | 10.90 (4.3) | 9.57 (3.2) | 9.00 (4.0) |
| Emotional | 1.86 (1.4) | 1.80 (1.5) | 2.43 (1.2) | 1.83 (1.6) |
| MSAS – Symptom Bother | ||||
| Physical | 0.56 (0.4) | 0.77 (0.6) | 0.54 (0.3) | 0.49 (0.5) |
| Emotional | 0.92 (0.8) | 1.08 (1.2) | 1.27 (0.8) | 1.00 (1.0) |
| Positive Affect | 3.89 (0.6) | 3.26 (0.8) | 3.61 (0.7) | 3.42 (0.7) |
| Negative Affect | 1.67 (0.6) | 1.62 (0.7) | 1.54 (0.5) | 1.48 (0.5) |
| CESD | 9.68 (7.6) | 14.90 (13.5) | 9.70 (7.2) | 8.17 (6.4) |
| Future Time Perspective | 52.94 (8.9) | - | 48.48 (10.8) | - |
| BMMRS - Meaning | 3.36 (0.6) | 3.63 (0.4) | 3.31 (0.6) | 3.43 (0.7) |
| Meaning in Life | 3.42 (0.4) | 3.64 (0.4)a | 3.53 (0.4) | 3.53 (0.4) |
| Caregiver Stress | 2.35 (0.2) | 2.32 (0.2) | 2.34 (0.2) | 2.30 (0.2) |
| PAC | 4.67 (0.3) | 4.67 (0.4) | 4.61 (0.6) | 4.65 (0.5) |
| Patient | ||||
| MSAS –Symptom Number | ||||
| Physical | 9.27 (5.2) | 9.40 (5.7) | 8.30 (2.8) | 9.06 (3.8) |
| Emotional | 2.22 (1.7) | 1.80 (1.1)a | 1.39 (1.3) | 2.00 (1.2) |
| MSAS – Symptom Bother | ||||
| Physical | 0.74 (0.5) | 0.78 (0.6) | 0.61 (0.3) | 0.64 (0.4) |
| Emotional | 1.15 (0.9) | 1.0 (0.8)a | 0.64 (0.7) | 0.97 (0.7) |
| Positive Affect | 3.12 (0.7) | 3.17 (0.8) | 3.38 (0.7) | 3.22 (0.7) |
| Negative Affect | 1.80 (0.6) | 1.80 (0.6) | 1.61 (0.5) | 1.66 (0.6) |
| CESD | 14.27 (8.8) | 18.40 (10.0) | 11.65 (8.0) | 13.50 (9.6) |
| Future Time Perspective | 38.45 (14.1) | - | 44.26 (13.6) | - |
| BMMRS | ||||
| Daily Spiritual Experiences | 5.12 (0.7) | 5.23 (10.0) | 4.85 (1.2) | 4.90 (1.2) |
| Forgiveness | 3.59 (0.3) | 3.80 (0.3)a | 3.54 (0.7) | 3.50 (0.7) |
| Meaning | 3.41 (0.7) | 3.35 (0.7) | 3.24 (0.8) | 3.33 (0.8) |
| Abandonment | 3.73 (0.6) | 3.80 (0.4)a | 3.96 (0.2) | 3.83 (0.5) |
| Meaning in Life | 3.39 (0.5) | 3.43 (0.6) | 3.57 (0.4) | 3.58 (0.4) |
MSAS = Memorial Symptom Assessment Scale; CESD = Center for Epidemiological Studies Depression Scale; BMMRS = Brief Multidimensional Measure of Religiousness and Spirituality.
P<0.05.
Baseline Associations
Among palliative care patients, baseline correlations reveal significant relations between greater future time perspective (i.e., the perception of more time left to live) and better health (VES-13; r = −0.30; P = 0.04), more meaning in life (r = 0.39; P = 0.007), and more positive affect (r = 0.41; P = 0.005). Measures of physical and emotional symptoms and bother were significantly associated with negative affect and depressive symptoms.
Among caregivers, baseline correlations reveal significant relations between greater future time perspective and greater meaning in life (r = 0.41; P = 0.009), more positive affect (r = 0.56; P < 0.0001) and fewer depressive symptoms (r = −0.34; P = 0.02). Greater future time perspective also was significantly associated with lower cognitive functioning (r = −0.31; P = 0.04). Greater caregiving stress at baseline was significantly related to worse palliative care patient health (VES-13; r = 0.36; P = 0.02), and caregiver report of a greater number of patient physical symptoms (r = 0.33; P = 0.03) and physical symptom bother (r = 0.42; P = 0.004), as well as a greater number of patient emotional symptoms (r = 0.35; P = 0.02) and emotional symptom bother (r = 0.39; P = 0.008).
Intervention Effects at Post-Intervention and Maintenance at Follow-Up
Controlling for patient health, patients in the intervention group reported a significantly greater reduction in number of emotional symptoms, F(1, 25) = 6.18, P = 0.02, partial eta-squared = 0.20, and emotional bother, F(1, 25) = 4.81, P = 0.04, partial eta-squared = 0.16, than patients in the control group, whose emotional symptoms and bother increased. Intervention patients expressed more forgiveness than control patients, F(1,25) = 5.24, P = 0.031; partial eta-squared = 0.17, and less negative religious coping (e.g., feelings of abandonment by God), F(1,25) = 4.88, P = 0.037; partial eta-squared = 0.16 from baseline to post-intervention. Thus, delivery of the intervention by RSVs had a positive impact on palliative care patients’ emotional symptoms and burden and spiritual health. Effect sizes observed were similar to those in previous research.8 However, only improvement in intervention patients’ emotional symptom bother was maintained at follow-up, F(2,19) = 4.56, P = 0.024; partial eta-squared = 0.32. It is noteworthy that between post-intervention and follow-up, there was no contact with the RSV.
Palliative caregivers also experienced initial gains from the RSV-delivered intervention. Controlling for group differences in patient health, caregivers in the intervention group reported increased meaning in life compared with control caregivers, F(1,25) = 6.20, P = 0.02; partial eta-squared = 0.24. Once again, effect sizes were similar to those in previous research.8 No other statistically significant group differences for caregivers were found, and this initial gain was not maintained at follow-up, during which time there was no contact with the RSV.
Qualitative Analysis of Treatment Acceptability
Descriptive qualitative content analysis35 of audiotaped and transcribed intervention session three revealed several themes. Patients and caregivers shared that the intervention had been an enriching, energizing, or valued experience. A family pride theme emerged, with importance placed on “passing down” family history. A theme of patient-caregiver connection emerged, along with the concept of better communication. Patients and caregivers strongly expressed appreciation for the RSV. Some intervention dyads shared that their project was not completed, but expressed the intention of continuing work on it.
Unique to patients, the theme of being thankful for, proud or appreciative of the caregiver arose. One patient stated, “She’s got a different perspective than I do,” to which the caregiver replied, “I base it on… the things that inspire me about you… the qualities you possess.” Patients mentioned the idea of being remembered through creation of the project. One patient stated, “I got some more great-great grans coming along now. And see, they don’t even know me.” Another stated, “I love remembering and talkin’ about all of them…and me. That’s good, too, the part of me.” This theme was occasionally tied to family being geographically distant.
The theme of patient suffering arose. One patient stated, “I see that my stroke was a turning point in my life.” Another said, “I have always worried that I wouldn’t be able to have my whole life flash before my eyes. I’d forget some of it.”
Unique to caregivers, the theme of motivation by the project and the RSV arose. One caregiver stated, “It’s one of those things that you always intend to get around to.” Another said, “I probably would have just stopped had you not come back to see what else I had done.” Caregivers expressed appreciation for the Participant Notebook and brainstorming activity, along with the project’s ability to “keep [the patient’s] mind going a little while.” Negative themes emerged concerning costs of the project in time and money and caregivers feeling overwhelmed.
Discussion
The results of this RCT extend prior research by demonstrating the effective delivery by RSVs of a manualized reminiscence and creative activity intervention with positive emotional outcomes for palliative care patients and caregivers. Effect sizes were similar to prior research wherein graduate students acted as interventionists.8 Palliative care patients experienced fewer emotional symptoms and less emotional symptom bother, greater forgiveness, and less “abandonment by God,” and their caregivers experienced greater meaning in life in comparison with the control group. It is noteworthy that, as in Dignity Therapy,10,12 several intervention effects reflected existential or spiritual realms. Unfortunately, only improvement in intervention patients’ emotional symptom bother was maintained at follow-up after contact with the RSV ceased. This finding suggests that, as recommended by Kazdin and Blase,17 alternative treatment delivery modes such as continued RSV contact, technology, or self-help must be built into translation of interventions to relieve patient and caregiver suffering. Notably, caregivers reported that presence of the RSV motivated continued work on the reminiscence and creative activity project.
Further translation and implementation of this RSV-delivered intervention will necessitate programming for maintenance of therapeutic gains. Perhaps certain RSVs would be interested in “adopting” a family for longer intervention periods. Alternatively, volunteers could be recruited from faith-based or other organizations with which palliative care patients and caregivers are actively involved. Recruiting volunteers from within the palliative care patient or caregiver community to act as interventionists also may be feasible under certain conditions. Finally, technology-assisted delivery methods for such interventions should be explored.17
How time perspective functions near death has been a matter of some debate.36–38 In this study, future time perspective measured at baseline was associated with meaning in life and positive affect among both patients and caregivers. As expected, patients in better health, and hence with lower risk of death or functional decline in the near future, reported a more expansive perspective of future time. Among caregivers, a significant association between an expansive time perspective and fewer depressive symptoms was observed. Caregiver stress was associated with worse patient physical and emotional functioning. Future qualitative studies should explore the experience of time, suffering, forgiveness and meaning among palliative care patients and caregivers39 to clarify situations in which existentially-focused intervention may be therapeutically beneficial.
As with any research, this project had limitations. First, community-based sample recruitment proved difficult, with only 45 of 76 eligible dyads (59%) completing baseline. Moreover, generalizability is limited by the geographic region and racial/ethnic characteristics of the participants. Future research should target dyads of diverse racial/ethnic groups, particularly in rural areas. Third, our patients’ proximity to death varied. Although the community-based, pre-hospice nature of this study is unique, the timing of intervention may be better placed at patient diagnosis or health status change to focus patients and caregivers on prevention of decline and increase motivation.
In spite of these limitations, these promising results have practice and policy implications. RSV delivery of effective interventions extends the potential scope of palliative mental health care practice to patient and caregiver dyads that have not yet chosen hospice care.17 Moreover, volunteer efforts reflect a monetary value of $161.7 billion,40 and volunteering affords positive health benefits to the volunteer.41,42 The results of this RCT demonstrate that RSVs can be trained to effectively deliver reminiscence and creative activity interventions with similar patient and caregiver improvements in outcome to that found in previous research.8
Acknowledgments
Special thanks are extended to Drs. Regina Harrell, Richard Sims, Ali Ahmed, Andrew Duxbury, and Kelli Flood, and to Ms. Mary Hardrick and Ms. Starr P. Culpepper for assistance in recruitment. Most especially, the LIFE team extends its thanks to FOCUS on Senior Citizens and Positive Maturity for supporting volunteer recruitment and involvement, and to all of the patients and caregivers who gave generously of their time and energy to this project.
Appendix. Question Prompts Used in Session 1 from the LIFE Volunteer Interventionist Manual
|
Patient Questions – 4 items
|
| “The things I care about and value most in my life are..” |
| “The most important people in my life have been…” |
| “I would like people to remember these things about me…” |
| “The ideas, books, music, and poems that have most influenced my life are…
|
|
Caregiver Questions – 3 items
|
| “My favorite memories of times with my loved one are…” |
| “The things I most want to remember about my loved one are…” |
| “The lessons/values I have learned or most associate with my loved one are…”
|
Tips for Legacy Activities
|
Footnotes
Disclosures
This project was supported by funding from the National Institute of Nursing Research (R21NR011112) to Dr. Allen. Although all authors received financial support for this project, no conflicts of interest were reported and the National Institute of Nursing Research was not involved in the conduct of the study or development of the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Carstensen L, Isaacowitz DM, Charles ST. Taking time seriously. Am Psychol. 1999;54:165–181. doi: 10.1037//0003-066x.54.3.165. [DOI] [PubMed] [Google Scholar]
- 2.Chochinov HM, Hassard T, McClement S, et al. The landscape of distress in the terminally ill. J Pain Symptom Manage. 2009;38:641–649. doi: 10.1016/j.jpainsymman.2009.04.021. [DOI] [PubMed] [Google Scholar]
- 3.Breitbart W, Applebaum A. Meaning-centered group psychotherapy. In: Watson M, Kissane DW, editors. Handbook of psychotherapy in cancer care. New York: Wiley; 2011. [Google Scholar]
- 4.Neimeyer RA, Pennebaker JW, van Dyke JG. Narrative medicine: writing through bereavement. In: Chochinov HM, Breitbart W, editors. Handbook of psychiatry in palliative Medicine. New York: Oxford University Press; 2009. pp. 454–469. [Google Scholar]
- 5.Harris GM, Allen RS, Dunn L, Parmelee P. “Trouble won’t last always”: Religious coping and meaning in the stress process. Qual Health Res. 2013;23:773–781. doi: 10.1177/1049732313482590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Randall GK, Bishop AJ. Direct and indirect effects of religiosity on valuation of life through forgiveness and social provisions among older incarcerated males. Gerontologist. 2013;53:51–59. doi: 10.1093/geront/gns070. [DOI] [PubMed] [Google Scholar]
- 7.Allen RS. The legacy project intervention to enhance meaningful family interactions: case examples. Clin Gerontol. 2009;32:164–176. doi: 10.1080/07317110802677005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Allen RS, Hilgeman MM, Ege MA, Shuster JL, Burgio LD. Legacy activities as interventions approaching the end of life. J Palliat Med. 2008;11:1029–1038. doi: 10.1089/jpm.2007.0294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ando M, Morita T, Akechi T, Okamoto T. Efficacy of short-term life-review interviews on the spiritual well-being of terminally ill cancer patients. J Pain Symptom Manage. 2010;39:993–1002. doi: 10.1016/j.jpainsymman.2009.11.320. [DOI] [PubMed] [Google Scholar]
- 10.Chochinov HM. Dignity Therapy: Final words for final days. New York: Oxford University Press; 2012. [Google Scholar]
- 11.Chochinov HM, Hack T, Hassard T, et al. Dignity therapy: a novel psychotherapeutic intervention for patients near the end of life. J Clin Oncol. 2005;23:5520–5525. doi: 10.1200/JCO.2005.08.391. [DOI] [PubMed] [Google Scholar]
- 12.Chochinov HM, Kristjanson LJ, Breitbart W, et al. Effect of dignity therapy on distress and end-of-life experience in terminally ill patients: a randomised controlled trial. Lancet Oncol. 2011;12:753–762. doi: 10.1016/S1470-2045(11)70153-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McClement S, Chochinov HM, Hack T, et al. Dignity therapy: family member perspectives. J Palliat Med. 2007;10:1076–1082. doi: 10.1089/jpm.2007.0002. [DOI] [PubMed] [Google Scholar]
- 14.Scogin F, Welsh D, Hanson A, Stump J, Coates A. Evidence-based psychotherapies for depression in older adults. Clin Psychol: Science Practice. 2005:222–237. [Google Scholar]
- 15.Candy B, Jones L, Drake R, Leurent B, King M. Interventions for supporting informal caregivers of patients in the terminal phase of a disease. Cochrane Database Syst Rev. 2011;6:CD007617. doi: 10.1002/14651858.CD007617.pub2. [DOI] [PubMed] [Google Scholar]
- 16.Csikai EL, Weisenfluh S. Hospice and palliative social workers’ engagement in life review interventions. Am J Hosp Palliat Care. 2013;30:257–263. doi: 10.1177/1049909112449067. [DOI] [PubMed] [Google Scholar]
- 17.Kazdin AE, Blase SL. Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspect Psychol Sci. 2011;6:21–37. doi: 10.1177/1745691610393527. [DOI] [PubMed] [Google Scholar]
- 18.Min LC, Elliott MN, Wenger NS, Saliba D. Higher Vulnerable Elders Survey scores predict death and functional decline in vulnerable older people. J Am Geriatr Soc. 2006;54:507–511. doi: 10.1111/j.1532-5415.2005.00615.x. [DOI] [PubMed] [Google Scholar]
- 19.Saliba D, Elliott M, Rubenstein LZ, et al. The Vulnerable Elders Survey: a tool for identifying vulnerable older people in the community. J Am Geriatr Soc. 2001;49:1691–1699. doi: 10.1046/j.1532-5415.2001.49281.x. [DOI] [PubMed] [Google Scholar]
- 20.van den Berg E, Ruis C, Biessels GJ, Kappelle LJ, van Zandvoort MJ. The Telephone Interview for Cognitive Status (Modified): relation with a comprehensive neuropsychological assessment. J Clin Exp Neuropsychol. 2012;34:598–605. doi: 10.1080/13803395.2012.667066. [DOI] [PubMed] [Google Scholar]
- 21.De Jager CA, Budge MM, Clarke R. Utility of TICS-M for the assessment of cognitive function in older adults. Int J Geriatr Psychiatry. 2003;18:318–324. doi: 10.1002/gps.830. [DOI] [PubMed] [Google Scholar]
- 22.Folstein MF, Folstein S, McHugh P. “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 23.Carstensen LL, Lang FR. Future Orientation Scale. 1996. [Google Scholar]
- 24.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 25.Carpenter JS, Ph D, Andrykowski MA, Wilson J, Rayens MK. Psychometrics for two short forms of the Center for Epidemiologic Studies-Depression Scale. Issues Ment Health Nurs. 1998;19:481–494. doi: 10.1080/016128498248917. [DOI] [PubMed] [Google Scholar]
- 26.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 27.Chang VT, Hwang SS, Feuerman M, Kasimis BS, Thaler HT. The Memorial Symptom Assessment Scale Short Form (MSAS-SF) Cancer. 2000;89:1162–1171. doi: 10.1002/1097-0142(20000901)89:5<1162::aid-cncr26>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 28.Fetzer Institute. Multidimensional measurement of religiousness/spirituality for use in health research. Kalamazoo, MI: John E. Fetzer Institute; 1999. [Google Scholar]
- 29.Krause N. Longitudinal study of social support and meaning in life. Psychol Aging. 2007;22:456–469. doi: 10.1037/0882-7974.22.3.456. [DOI] [PubMed] [Google Scholar]
- 30.Krause N. Evaluating the stress-buffering function of meaning in life among older people. J Aging Health. 2007;19:792–812. doi: 10.1177/0898264307304390. [DOI] [PubMed] [Google Scholar]
- 31.Krause N. Meaning in life and mortality. J Gerontol B Psychol Sci Soc Sci. 2009;64B:517–527. doi: 10.1093/geronb/gbp047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zarit SH, Stephens MA, Townsend A, Greene R. Stress reduction for family caregivers: effects of adult day care use. J Gerontol B Psychol Sci Soc Sci. 1998;53:S267–277. doi: 10.1093/geronb/53b.5.s267. [DOI] [PubMed] [Google Scholar]
- 33.Tarlow BJ, Wisniewski SR, Belle SH, et al. Positive aspects of caregiving: contributions of the REACH project to the development of new measures for Alzheimer’s caregiving. Res Aging. 2004;26:429–453. [Google Scholar]
- 34.D’Zurilla T, Nezu A. Problem-solving therapy: A positive approach to clinical intervention. 3. New York: Springer Publishing Company; 2007. [Google Scholar]
- 35.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23:334–340. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 36.Chochinov HM. Death, time and the theory of relativity. J Pain Symptom Manage. 2011;42:460–463. doi: 10.1016/j.jpainsymman.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 37.Chochinov HM. Relatively speaking. J Pain Symptom Manage. 2012;43:e6–7. doi: 10.1016/j.jpainsymman.2011.12.175. [DOI] [PubMed] [Google Scholar]
- 38.Round J. Death, time, and the theory of relativity: a brief reply? J Pain Symptom Manage. 2012;43:e2–6. doi: 10.1016/j.jpainsymman.2011.12.177. [DOI] [PubMed] [Google Scholar]
- 39.Monin JK, Schulz R. Interpersonal effects of suffering in older adult caregiving relationships. Psychol Aging. 2009;24:681–695. doi: 10.1037/a0016355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Johnson RW, Schaner SG. Value of unpaid activities by older Americans tops $160 billion per year. Washington, DC: The Urban Institute’s Retirement Project; 2005. [Google Scholar]
- 41.Harris AHS, Thoresen CE. Volunteering is associated with delayed mortality in older people: analysis of the longitudinal study of aging. J Health Psychol. 2005;10:739–752. doi: 10.1177/1359105305057310. [DOI] [PubMed] [Google Scholar]
- 42.Martinez IL, Frick K, Glass TA, et al. Engaging older adults in high impact volunteering that enhances health: recruitment and retention in The Experience Corps Baltimore. J Urban Health. 2006;83:941–953. doi: 10.1007/s11524-006-9058-1. [DOI] [PMC free article] [PubMed] [Google Scholar]