Abstract
Background
Classification schemas for low back pain (LBP), such as the Treatment Based Classification and the Movement System Impairment schemas, use common clinical features to subgroup patients with LBP and are purported to improve treatment outcomes.
Purpose
To assess if providing matched treatments based on patient specific clinical features led to superior treatment outcomes compared to an unmatched treatment for subjects with chronic, recurrent LBP.
Study Design
A randomized controlled trial.
Patient Sample
Subjects (n=124) with LBP (≥ 12 months) with or without recurrences underwent a standardized clinical exam to group them into one of 2 strata: (1) ineligible or (2) eligible for stabilization exercises based on the Treatment Based Classification schema. Subjects underwent additional clinical tests to assign them to one of the 5 possible Movement System Impairment categories.
Outcome Measures
Questionnaires were collected electronically at: Week 0, prior to treatment; Week 7 (following the 6 weekly, one hour treatment sessions); and 12 months. Using the Oswestry Disability Index (0-100) and the Numeric Pain Rating Scale (0-10), the primary analysis was performed using the intention-to-treat principle. Secondary outcomes included fear-avoidance beliefs as well as psychosocial, work related and general health status.
Methods
After subjects were categorized based on their particular clinical features using both the Treatment Based Classification and Movement System Impairment schemas, they were randomized into one of two treatments using a 3:1 ratio for matched or unmatched treatments. The treatments were (1) trunk stabilization exercise, or (2) Movement System Impairment-directed exercises. The study was funded by National Institutes of Health (NCMRR/R01HD040909; $1,485,000). There are no study specific conflicts of interest to report.
Results
Of the patients allocated to treatment for this study, 76 received a matched treatment and 25 received an unmatched treatment. Following treatment, both groups showed a statistically significant improvement in the primary outcome measures and almost all of the secondary measures; however, the matched treatment group did not demonstrate superior outcomes at Week 7 or 12 months, except on one of the secondary measures (Graded Chronic Pain Scale – Disability Scale) (P=0.01).
Conclusion
Providing a matched treatment based on either the Treatment Based Classification or the Movement System Impairment classification schemas did not improve treatment outcomes compared to an unmatched treatment for patients with chronic LBP, except on one secondary disability measure.
Keywords: randomized controlled trial, chronic low back pain, classification, physical therapy, subgroups
Introduction
Low back pain (LBP) remains a public health issue because it is a heterogeneous, musculoskeletal condition that affects up to 80% of all people at some point in their life3. In 85% of persons with LBP, no patho-anatomical cause can be identified27, 48, which makes prescribing treatments for patients difficult. Classification of patients with LBP into homogenous subgroups with relevant clinical features has been identified as a research priority by several groups5, 8, 55 and may be used to direct treatment and improve treatment outcomes.
Two promising classification systems for LBP are the Treatment Based Classification10 and the Movement System Impairment52 approaches. The Treatment Based Classification system uses clusters of clinical features from a patient's medical history and physical examination, to categorize and direct the patient into one of 4 types of treatments16: trunk stabilization exercises, specific exercises, spinal manipulation, or traction. Hicks et al.32 and Fritz et a.16 have identified four clinical features associated with patient improvement following stabilization treatment: (1) age younger than 40 years, (2) a positive score on the prone instability test,11, 32 (3) more than 91° of hip flexion during a passive straight-leg test,11, 32 and (4) aberrant trunk movements with lumbar-spine flexion32. At least any three of the four clinical features, taken together, now comprise a clinical prediction rule used to identify patients likely to improve with stabilization exercises56. Additionally, Fritz et al.15 have identified another clinical feature of patients with LBP who improve with stabilization treatment: lumbar-spine hypermobility. Rater agreement when classifying patients based on shared clinical features using the Treatment Based Classification system ranges from a kappa statistic of 0.52 to 0.62 with a percent agreement ranging from 67% to 81%29, 56.
The Movement System Impairment system classifies types of LBP based on impaired trunk movements and postures associated with the patient's LBP observed during a standardized exam52. The Movement System Impairment system draws on the Kinesiopathologic Model, which assumes that altered precision in spinal movement may result in specific changes in the neuro-musculoskeletal system, such as changes in the activation patterns of trunk muscles. The Kinesiopathologic Model also assumes that, unless persons with LBP modify these repeated, direction-specific trunk movements and postures, they are at risk for persistent or recurrent LBP 52.
In the Movement System Impairment exam, the physical therapist conducts standardized tests52, 60 and assesses for changes in the patient's LBP symptoms. If any test increases the patient's symptoms, the physical therapist modifies the test and has the patient perform this modified test to determine if the patient's movement patterns, trunk posture, and/or symptoms are altered. If the patient reports that the modified test decreases or eliminates the LBP, this response confirms that the direction-specific movement or posture contributes to the patient's LBP61. Results from the initial and modified tests are used to classify the patient into 1 of 5 MSI subgroups (named for the observed lumbar movement or alignment impairments): (1) rotation, (2) extension, (3) flexion, (4) rotation with extension, and (5) rotation with flexion. The 5 MSI subgroups serve to help the PT design a matched treatment to the patient's specific signs and symptoms. The reliability of physical therapists classifying patients based on the Movement System Impairment approach has been examined25,30, 59 and the kappa statistic ranged from 0.61 to 0.81 with a percent agreement ranging from 75% to 87% which reflects moderate to excellent agreement in classification of patients.
The Treatment Based Classification directed trunk stabilization approach focuses on 3 components of spinal stability: (1) motor control of the deep trunk muscles (transversus abdominis, internal oblique and multifidus),7, 32, 51 (2) strengthening of the flexor, extensor, and oblique trunk muscles;32 and (3) incorporating trunk muscle control into activities of daily living. The Movement System Impairment directed approach focuses on (1) direction-specific functional activity modifications to change lumbopelvic movement patterns to patterns that are painfree; (2) exercises to modify lumbopelvic movements and postures in specific directions that are painfree; and (3) patient education on how specific lumbopelvic movement patterns and postures repeated daily might accelerate lumbar-tissue stress as well as education about the importance of modifying the movement patterns throughout the day. The treatments directed by the Treatment Based Classification and Movement System Impairment classification approaches share similar goals of improving the patient's ability to control his trunk and to stabilize his spine during activities of daily living, during isolated and combined trunk movements and during trunk movement that is induced by limb movement.
The purpose of this study was to compare the pain and functional outcomes for patients with chronic LBP who were either matched or unmatched to a treatment that focused on improving their trunk control and ability to stabilize their spine. We hypothesized that patients who were matched to treatment based on particular clinical features would improve their function and decrease their symptoms more over short (7 weeks) and long term (12 months) follow-up periods compared to patients who were not matched to treatment.
Methods
Subjects
Subjects in this study were part of a randomized clinical trial (NCT01362049), funded by the National Institutes of Health (R01HD040909), in which subjects with LBP (n=1022) were assessed for study inclusion through phone and email contact. Subjects who were admitted to the study (1) were between 21 and 55 years old, (2) had a history of chronic LBP (≥ 12 months) with or without recurrences, (3) could stand and walk independently, (4) had a Modified Oswestry Disability Index (ODI) score of ≥ 19%, and/or a score less than 8 on at least one activity from the Patient Specific Functional Scale,58 (5) could understand English, and (6) were currently employed or actively engaged in daily activities. Exclusion criteria included: a structural spinal deformity, spinal fracture, osteoporosis, systemic disease processes, disc herniation with corroborating clinical signs and symptoms, previous spinal surgery, pregnancy or less than 6 months post-partum or post-weaning, magnified symptom behavior,65 and a body-mass index of greater than 30. This study was approved by the Institutional Review Board at the University of Vermont. All subjects provided written, informed consent, and the rights of each subject were protected. There were no adverse events reported during the study and there were no changes to methods after the trial began. Once recruitment goals were met and the questionnaire data were collected across the follow-up time points, the trial was ended Figure 1 gives an outline of subject flow and data-collection procedures in this study.
Figure 1.
Study Flow
Pre-treatment Assessments
Questionnaire Completion
All subjects allocated to treatment for this study (n=102) completed a medical history and demographic form as well as the ODI19, Numeric Pain Rating Scale (NPRS)36, Graded Chronic Pain Scale24,12, 54, Fear Avoidance Behavior Questionnaire23, Patient Specific Functional Scale58, Short Form 36 (SF-36)45,67.
Classification of Subjects
To maximize reliability, one physical therapist examiner (ROM) performed the standardized clinical exam on all subjects in a laboratory setting, and she determined if the subject was eligible or ineligible for stabilization exercises (per the Treatment Based Classification system) and also determined the subject's Movement System Impairment classification. The standardized clinical exam included the following tests that are part of the Treatment Based Classification approach and are used to identify which patients were likely to respond to stabilization exercises: (1) the prone instability test11,32, (2) straight-leg raise test11,32, (3) the lumbar-spine flexion test32, (4) age less than 40 years, and (5) the lumbar-spine hypermobility test28, 32,15. Studies14, 21, 33, 56 have demonstrated these tests to have fair-to-good inter-rater reliability. If a subject was positive on any three of the first four clinical tests listed and/or positive with the lumbar-spine hypermobility test, he was assigned to the ‘eligible’ stratum. If the subject did not meet the Treatment Based Classification-eligible criteria, he was assigned to the ‘ineligible’ stratum. This stratification allowed us to have a non-matched treatment group for comparison to the matched treatment group.
In addition, all subjects underwent a standardized Movement System Impairment clinical exam that allowed the physical therapist examiner to assign a person to one of five possible Movement System Impairment categories25. In a separate pilot study, two physical therapists (SMH and ROM) demonstrated an 80% agreement with a kappa statistic of 0.80 (CI: 0.53, 1.00) when conducting the standardized Movement System Impairment exam and then independently using the clinical data to assign an Movement System Impairment category to each of 20 subjects with LBP. At the completion of the standardized clinical exam, all subjects had been classified using both the Treatment Based Classification and the Movement System Impairment based approaches (Figure 1).
Subject Randomization
After stratifying subjects into either the eligible vs. ineligible strata and then classifying them into one of five Movement System Impairment categories, subjects (n=102) were next randomized to receive one of two treatments: stabilization exercises or Movement System Impairment-based treatment (Figure 1). The statistician used computer generated randomization with centralized allocation concealment to randomize subjects into one of two treatments using a 3:1 ratio for matched to unmatched treatment. Because patients were classified using both the Treatment Based Classification and the Movement System Impairment based approaches, the randomization resulted in the majority of subjects (n=76) receiving a matched treatment (i.e., subjects who were ineligible receiving Movement System Impairment treatment; or were eligible receiving Movement System Impairment treatment; or were eligible receiving stabilization exercises). The other portion of subjects (n=25) received an unmatched treatment (i.e., subjects who were ineligible receiving stabilization) (Figure 1).
Physical therapy treatment
After randomization, the subject was scheduled for his first treatment session as soon as possible in the clinic, usually within 3-6 days of the pre-treatment session. Both the stabilization exercises and Movement System Impairment-based treatment approaches share the common goal of improving the subject's trunk control and the ability to stabilize the spine during activities of daily living as well as during isolated and combined trunk and/or limb movements. Using exercises designed to improve recruitment and strength of trunk muscles, the physical therapy clinicians progressed subjects through the standardized treatment protocols, providing one treatment per week for 6 weeks. All patients were given a home exercise program and turned in their weekly exercise log. Each physical therapy clinician passed a written test to show an acceptable level of knowledge regarding exercise progression for the treatment that she was providing and completed the UVM Human Subject Testing tutorial on ethical treatment of human subjects.
Stabilization treatment protocol
All subjects in both the eligible and ineligible strata who were randomized to stabilization exercises attended physical therapy sessions at one of 4 physical therapy outpatient clinics and were treated by a PT who provided only the stabilization exercises as part of this study (Table 1). The stabilization exercise protocol focused on 3 components of spinal stability: (1) motor control of the deep trunk muscles7, 32,51; (2) strengthening of the flexor, extensor, and oblique trunk muscles32 by focusing on repeated submaximal efforts to mimic the function of these muscles in spine stabilization44, 50 and (3) patient education in the form of an education booklet47 that describes how to use proper body mechanics in order to protect the spine during activities of daily living (see Appendix 1 for protocol details). Subjects were instructed to perform these stabilization exercises daily and to keep an exercise log. The four treating physical therapists received training (from SMH) in how to progress the stabilization exercises and were blinded to the subjects’ strata assignment.
TABLE 1.
Characteristics of the physical therapy clinicians.
| Entry level physical therapy education | BS = 8; MPT or MSPT = 3 |
| Years in practice (mean ± SD; range) | 13.3 ± 6.2; 4- 27 years |
| % FTE of time in physical therapy practice (n) | |
| 0 – 25% | 3 |
| 26 – 50% | 1 |
| 51 – 75% | 1 |
| 76 – 100% | 6 |
| Number of clinicians with previous experience with the Treatment Based Classification system (n) | |
| None | 5 |
| A little | 6 |
| Moderate | 0 |
| A lot | 0 |
| Number of clinicians with previous experience with the Movement System Impairment Classification system (n) | |
| None | 4 |
| A little | 5 |
| Moderate | 2 |
| A lot | 0 |
FTE, full time equivalent
MSI treatment protocol
All subjects in both the eligible and ineligible strata who were randomized to Movement System Impairment treatment attended physical therapy sessions at one of 4 physical therapy outpatient clinics and were treated by a PT who provided only the Movement System Impairment treatment as part of this study (Table 1). With the Movement System Impairment based approach, the PT matches treatment to correspond to the specific Movement System Impairment category. Based on the subject's direction-specific LBP classification, the PT tailored the Movement System Impairment protocol to focus on: (1) education about positions or postures to control his symptoms; (2) ‘Exercises for Precision of Trunk Movement” where patients were taught specific trunk movements and postures that were painfree; and (3) functional activity modifications (based on their Patient Specific Functional Scale) to change his trunk-movement and alignment patterns (see Appendix 2 for protocol details for the Rotation, Rotation with Extension, and Rotation with Flexion categories). The particular exercises that were prescribed depended on the Movement System Impairment classification to which a subject was assigned; however, all PTs used the same set of exercises for a particular Movement System Impairment classification. Subjects were instructed to perform these Movement System Impairment exercises daily and to keep an exercise log. The four treating physical therapists received training (from SMH and LVD) as to how to progress the Movement System Impairment exercises and were blinded to the subjects’ strata assignment.
Post-treatment Assessments
Within a week after treatment was completed, all subjects returned for the same assessments (questionnaires, standardized clinical exam). The same physical therapist examiner (ROM) conducted the clinical exam.
Masking of Study Personnel
The statistician and recruitment coordinator were not masked to strata and treatment assignment while all other study personnel were masked to both. Physical therapy clinicians who provided the treatment as well as the subjects were masked to strata assignment but not to treatment. Following treatment but prior to post-treatment assessments, the physical therapist examiner (ROM) and the principaI investigator (SMH) guessed which treatment each subject received to test if they had remained masked to treatment assignment. The percent for correct vs. incorrect guesses were: 57%/43% for the physical therapist examiner and 50%/50% for the principaI investigator, indicating that the masking was successful.
Data Analysis
The primary analysis was an intention-to-treat analysis. To investigate our primary hypothesis, repeated measures analyses of variance were performed to examine the primary outcome measures, the ODI and NPRS scores, for subjects in the matched vs. unmatched treatment groups, before and immediately after treatment at Week 7 and at 12 months. A similar procedure was used for the other three questionnaires. Only subjects who were participated in the Week 0 and Week 7 time points were included in the analyses. In addition, a successful treatment outcome was based on changes in the ODI score from pre- to post-treatment such that reduction of 8 percentage points or more on the ODI was called a treatment success22, 41. Less than an 8 percentage point reduction was considered a treatment failure. Baseline patient characteristics and questionnaire responses were compared using t-tests or Chi-Square tests of Independence, depending upon the type of variable being examined. All analyses were completed using a statistical significance of P<0.05 using SAS 9.2 (SAS Inc, Cary, NC) procedures that could accommodate missing data without imputation.
Sample Size
Choosing a power of 80%, a significance level of 0.05 and a subject distribution ratio of 3:1, our power analyses indicated that an overall sample size of 88 subjects was needed to detect a treatment difference over time in the ODI score that was 7 percentage points greater for the matched treatment group compared to the unmatched group. We assumed a standard deviation of 10% for the ODI, which was based on data from our previous work. Thus, we needed 66 subjects in the matched treatment group and 22 subjects in the unmatched group.
Results
In total, 1022 volunteers were screened for inclusion in the study and 898 were excluded because they did not meet the inclusion criteria [prior surgery (n=230), body/mass index > 30 (n=71), age (n=114), pain below the knee (n=56), minimal functional impairment (n=33), LBP< 1 year (n=27), excluded medical diagnosis (n=81), litigation (n=21), other (n=264), declined to participate (n=1)]. Of the 102 subjects allocated to treatment for this study between March 2010 and September 2011, one subject was subsequently excluded on Clinic Visit 1 because he had developed pain below his knee that was not present during the pre-treatment assessment session. Of the 101 subjects included in this study, 76 received a matched treatment (i.e., subjects who were ineligible or eligible receiving Movement System Impairment treatment; or were eligible receiving stabilization exercises) while 25 received an unmatched treatment (i.e., subjects who were ineligible receiving stabilization exercises) (Figure 1). There were no differences in baseline characteristics between the two groups (Table 2).
Table 2.
Patient characteristics prior to treatment. All measures are reported as the mean and standard deviation except where noted.
| Group | Matched | Unmatched |
|---|---|---|
| Number of Subjects | 76 | 25 |
| Sex (number of males/females) | 35/41 | 15/10 |
| Age (y) | 40.15 (11.06) | 45.88 (8.82) |
| Height (m) | 1.72 (0.09) | 1.74 (0.10) |
| Weight (kg) | 70.52 (12.46) | 73.44 (12.62) |
| Body mass index (kg/m2) | 24.07 (3.23) | 24.28 (2.63) |
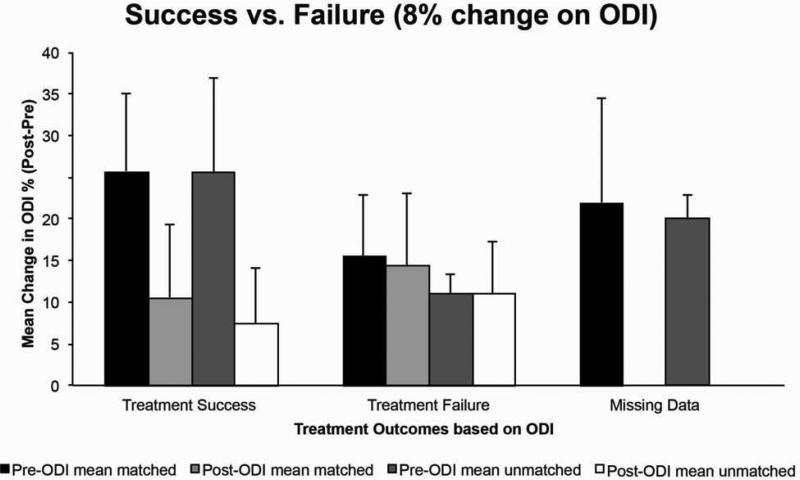
Out of six, one hour planned treatment sessions, the subjects in the match treatment group attended a mean (stdev) of 5.67 (1.03) sessions compared with 5.53 (1.25) sessions for patients allocated to the unmatched treatment group. For both the pain (NPRS) and disability (ODI) scores, there was a visit main effect (P < 0.0001 for both questionnaires) from pre- to post-treatment but no further improvement at 12 months (Table 3). Significant improvements across time were also noted for the other questionnaires for both treatment groups combined (visit main effects, P< 0.0001 to P<0.01) with the exception of the mental component summary score of the SF-36 questionnaire (visit main effect, P = 0.75). There was not a superior treatment effect with either the matched or unmatched treatment as evidenced by the complete lack of the group effects and by the lack of group by visit interactions for most of the questionnaires. The one exception was the Graded Chronic Pain Scale (Disability Scale) which had a significant group by visit interaction (P=0.01); the matched group improved significantly from pre- to immediately post-treatment and continued to improve at the 12 month time point (P< 0.0001) whereas the unmatched group did not improve over time (P=0.14) (Table 3). Results from the per prototcol analysis were similar. Approximately 45% of the matched and 48% of the unmatched group achieved treatment success, defined as a ≥8 percentage point reduction in the ODI score22, 41. The mean ODI scores for the matched vs. unmatched groups that achieved treatment success vs. failure are shown in Figure 2.
Table 3.
Patient outcomes following matched vs. unmatched treatment at Week 7 and 12 months.
| Group (n) | PRE 0 Weeks (Mean/SE) | POST 7 Weeks (Mean/SE) | POST 12 Months (Mean/SE) | P-Group | P-Visit | P-interaction | |
|---|---|---|---|---|---|---|---|
| Overall Statistics → | 0.20 | <0.0001 | 0.46 | ||||
| Oswestry Disability Index (0-100%) | Matched (69) | 20.58 (1.14) | 12.55 (1.14) | 9.36 (1.23) | |||
| Differences (CI) | 8.03 (4.84, 11.22) | 3.19 (−0.12, 6.51) | |||||
| Unmatched (23) | 18.70 (1.98) | 9.22 (1.98) | 10.20 (2.12) | ||||
| Differences (CI) | 9.48 (3.96, 15.00) | −0.98 (−6.70, 4.74) | |||||
| Overall Statistics → | 0.56 | < 0.0001 | 0.12 | ||||
| NPRS (0-10) | Matched (68) | 2.76 (0.22) | 1.59 (0.18) | 1.79 (0.25) | |||
| Differences (CI) | 1.17 (0.76, 1.59) | −0.20 (−0.66, 0.25) | |||||
| Unmatched (24) | 2.42 (0.36) | 1.42 (0.29) | 1.24 (0.41) | ||||
| Differences (CI) | 1.00 (0.31, 1.69) | 0.18 (−0.56, 0.91) | |||||
| Overall Statistics → | 0.73 | < 0.0001 | 0.06 | ||||
| GCPS – CPI (0 - 100) | Matched (69) | 48.61 (1.63) | 38.26 (1.84) | 30.28 (2.26) | |||
| Differences (CI) | 10.35 (7.88, 12.81) | 7.98 (4.54, 11.42) | |||||
| Unmatched (23) | 45.07 (2.82) | 34.01 (3.21) | 34.61 (3.92) | ||||
| Differences (CI) | 11.06 (6.74, 15.39) | −0.60 (−6.62, 5.42) | |||||
| Overall Statistics → | 0.27 | < 0.0001 | 0.01 | ||||
| GCPS – DS (0 - 100) | Matched (69) | 33.71 (2.40) | 26.91 (2.27) | 14.26 (2.16) | < 0.0001 | ||
| Differences (CI) | 6.80 (2.66, 10.93) | 12.65 (8.35, 16.94) | |||||
| Unmatched (23) | 25.07 (4.13) | 18.56 (3.99) | 18.53 (3.75) | 0.14 | |||
| Differences (CI) | 6.51 (−0.72, 13.75) | 0.03 (−7.53, 7.59) | |||||
| Overall Statistics → | 0.63 | 0.01 | 0.82 | ||||
| FABQ-PA (0 – 24) | Matched (69) | 13.39 (0.51) | 12.81 (0.58) | 11.04 (0.70) | |||
| Differences (CI) | 0.58 (−0.51, 1.66) | 1.77 (0.52, 3.03) | |||||
| Unmatched (24) | 13.04 (0.86) | 11.96 (0.99) | 10.86 (1.18) | ||||
| Differences (CI) | 1.08 (−0.75, 2.91) | 1.10 (−1.01, 3.20) | |||||
| Overall Statistics → | 0.59 | 0.01 | 0.42 | ||||
| FABQ-W (0 – 42) | Matched (69) | 10.69 (0.93) | 9.74 (0.93) | 8.29 (0.89) | |||
| Differences (CI) | 0.95 (−0.36, 2.25) | 1.45 (−0.13, 3.03) | |||||
| Unmatched (24) | 10.50 (1.57) | 7.92 (1.58) | 7.76 (1.49) | ||||
| Differences (CI) | 2.58 (0.38, 4.79) | 0.16 (−2.50, 2.81) | |||||
| Overall Statistics → | 0.32 | 0.01 | 0.53 | ||||
| SF36 Physical (0 - 100) | Matched (69) | 46.67 (0.81) | 50.51 (0.79) | 50.56 (0.86) | |||
| Differences (CI) | −3.83 (−6.08, −1.59) | −0.05 (−2.36, 2.26) | |||||
| Unmatched (24) | 48.89 (1.35) | 50.21 (1.35) | 51.42 (1.48) | ||||
| Differences (CI) | −1.32 (−5.08, 2.44) | −1.21 (−5.15, 2.73) | |||||
| Overall Statistics → | 0.69 | 0.75 | 0.87 | ||||
| SF36 Mental (0 - 100) | Matched (69) | 52.76 (1.02) | 53.14 (1.00) | 52.78 (1.08) | |||
| Differences (CI) | 0.48 (−3.73, 4.09) | −0.14 (−4.03, 3.75) | |||||
| Unmatched (24) | 52.57 (1.70) | 53.28 (1.70) | 51.42 (1.86) | ||||
| Differences (CI) | −0.71 (−5.44, 4.02) | 1.36 (−2.88, 5.61) | |||||
NPRS: Numeric Pain Rating Scale
GCPS – CPI: Graded Chronic Pain Scale - Characteristic Pain Index
GCPS – DS: Graded Chronic Pain Scale – Disability Scale
FABQ: Fear Avoidance Behavior Questionnaire; -PA: Physical Activity subscale; -W: work subscale
SF36 Physical: Physical component summary score of the Short Form 36
SF36 Mental: Mental component summary score of the Short Form 36
Figure 2.
The pre- and post-treatment mean Oswestry Disability Scores (%) of subjects grouped as a ‘treatment success’ (matched n=34, unmatched n=12) vs. ‘treatment failure’ (matched n=35, unmatched n=11). For the missing post-treatment data, there were 7 matched subjects and 2 unmatched subjects.
Discussion
By identifying each subject's particular clinical features defined by the Treatment Based Classification and Movement System Impairment classification schemas, we provided either a classification matched treatment based on clinical features or provided a classification unmatched treatment for 6 weeks and then compared the subjects’ pain and functional outcomes up to 12 months post-treatment. Using the primary outcome measures, we found a reduction in both pain (NPRS) and disability (ODI) scores following both the matched and unmatched treatments; however, superior outcomes were not achieved for subjects who received a matched treatment compared to subjects who received an unmatched treatment over this one year follow-up period. One of the secondary measures, the Graded Chronic Pain Scale (Disability Scale), did reveal a greater reduction in disability for the matched treatment group, compared to the unmatched group, immediately post-treatment and at the 12 month time point.
Using classification schemas to direct treatment
Although the theoretical basis for providing classification directed treatment based on patients’ relevant clinical features is sound, the evidence that supports this assertion is mixed. Some studies demonstrate support for the Treatment Based Classification subgrouping approach when considering the short term (e.g., 4 weeks) but not long term outcomes for patients with acute work-related LBP of less than 3 weeks duration17. Brennan et al (2006)32 reported that patients with acute and subacute LBP (n=123) had a small but significant reduction in disability at 4 weeks if they had received a matched treatment per the Treatment Based Classification schema. However, the long term data at one year were incomplete limiting a definitive conclusion about treatment outcomes. In addition, this study was designed not as a prospective randomized clinical trial but as a study to validate the Treatment Based Classification subgrouping, which limits its direct comparison to our study. Furthermore, the treating therapist was permitted to determine the dosage of treatment in an attempt to reflect clinical practice. This approach may have limited the treatment effect for the matched group that may have been observed had strict protocols been used as in our current study. Other studies with the acute LBP population34, 35 reported positive results following a stabilization exercise approach, thus supporting the notion that clinical outcomes can be improved when the initial treatment provided is matched to the signs and symptoms of patients with acute LPB.
In contrast, a more recent study by Apeldoorn et al.22 reported no differences at 8, 26 and 52 weeks in treatment groups when using the Treatment Based Classification schema for patients with subacute (6-12 wk) and chronic (>12 wk) LBP. The initial baseline characteristics of our subjects were similar to those reported by Apeldoorn et al.22 despite the increased chronicity in our cohort (>1 year of LBP). While their comparison treatment was usual physical therapy care as defined by the current Dutch LBP guidelines4, 41, 53, our comparison treatment was the stabilization exercise provided to subjects who did not meet the clinical prediction rule for stabilization exercises16. Thus, our comparison group (i.e., the unmatched treatment group) should have provided the largest difference in treatment outcomes but we did not observe this result in our study cohort. Similar to Apeldoorn22, we used the decision making algorithm presented by Fritz et al.16 and did not need to use the portion of the algorithm that describes ‘Factors Favoring’ or ‘Factors Against’ for the 3 categories listed there (i.e., ‘manipulation,’ ‘stabilization,’ ‘specific exercise’). Given that we excluded patients with pain below the knee who would likely be managed with traction, we did not need to include the ‘traction’ category which is the fourth category in the Treatment Based Classification schema. In contrast to Apeldorn and colleagues22, we used standardized exercises with progression guidelines for the treating therapists to use.
In addition, the treating therapists in our study gave subjects in the stabilization exercise group general instruction on how to modify a generic list of activities of daily living (from an instructional book) while those receiving matched Movement System Impairment-directed exercises got very specific instruction in how to modify their lumbopelvic coordination (based on their assigned Movement System Impairment category) during their specific daily activities. In another study using similar motor control principles as we did, Costa et al.7 (n= 154 patients with chronic LBP) demonstrated small but significant short term improvements in favor of the motor control group for both patient activity tolerance and global impression of recovery. However, the exercise interventions failed to reduce pain greater than non-therapeutic modalities over the same period. One other study39 did use a chronic LBP population which was subgrouped based on the presence of radiologically confirmed, symptomatic spondylolysis or spondylolisthesis. The authors reported superior treatment outcomes for patients who received the stabilization exercises (n=12) compared to those who received a control treatment (n=15) directed by their medical practitioner that consisted of regular weekly general exercise (e.g., swimming, walking, gym work). These results suggest that the stabilization exercise approach may be indicated for specific subgroups of the chronic LBP population.
The study by Hicks et al.32, from which the clinical prediction rule for stabilization exercise was derived, identified subjects who were successful with stabilization exercise retrospectively whereas for our study these subjects were defined a priori. Furthermore, we used the three of four clinical features identified by Hicks et al.32 to predict treatment success with stabilization exercise as well as lumbar-spine hypermobility which Fritz et al.20 identified as another clinical feature of patients with LBP who improve with stabilization treatment. Hicks et al.32 did not identify lumbar-spine hypermobility as a predictor of improved outcomes following stabilization treatment, likely due to biased recruitment resulting in limited numbers of subjects with lumbar-spine hypermobility. Thus, our cohort was likely more homogeneous based on the Treatment Based Classification schema for stabilization exercises compared to other studies and yet we still did not observe a superior treatment outcome compared to the unmatched treatment group.
Evidence in support of the Movement System Impairment classification directed treatment is similarly mixed. Using case based reports26, 42, 62, patient outcomes following Movement System Impairment directed treatment demonstrate superior improvement (1 year) compared to other classification systems46 and treatment approaches43,40. Results from a larger, randomized clinical trial that compares Movement System Impairment directed treatment and general strengthening and flexibility exercise protocol are not available at this time (NCT00802724).
Are classification schemas ready for clinical use?
Some have suggested that the majority of research to date in defining subgroups of patients with LBP is still in the hypothesis generation stage and that no classification system has demonstrated sufficient evidence to recommend its use in the clinic38, 66. Providing matched interventions to those with acute, first time LBP theoretically has long term implications, including the reduction of chronic LBP. While there has been progress in creating and supporting the decision making algorithm for those with acute LBP9, 17, 32, some have suggested that subgrouping may be less important among patients with more chronic symptoms6. However given that 15-45% of the population currently has LBP with lifetime recurrences in up to 80% of the people2 as well as the high recurrence rate49, there is also a need for treatment algorithms for patients with more mild disability or more chronic symptoms given these patients will likely benefit from alternative decision-making schemes. Given that 85% to 95% of patients with LBP are diagnosed by their general practitioner as having non-specific LBP64, clearly there is a mandate to improve treatment algorithms but perhaps current treatment is ineffective because it is misdirected. Further research is needed as indicated by our study results and may need to include psychosocial measures1, 53, 63 as well as cortical66 and neuromuscular measures 31, 37 and cognitive factors57.
Determining treatment success
Another way to examine the outcomes of matched vs. unmatched treatments is to define treatment outcomes as successful, failed or improved32. Patients with LBP judged to be appropriately matched to their treatment program reported improvements in ODI scores ranging from 57% to 83%, whereas patients receiving unmatched treatments experienced improvements from 20% to 38% over a 1- to 4-week treatment period9, 13, 18. For our study, given our cohort was more chronic than in these previous studies and our subjects had a lower mean ODI at baseline, we were concerned about using these same guidelines. Thus, a successful treatment outcome was based on changes in the ODI score from pre- to post-treatment such that a reduction of 8 percentage points or more on the ODI was called a treatment success22, 41. Less than an 8 percentage point reduction was a treatment failure. The threshold for determining treatment success is less conservative than thresholds used for determining treatment success with a more acute LBP population32 but we believe it is justified based on reports that determine significant changes in the ODI for the chronic LBP population22, 41. The initial ODI scores of those subjects in the ‘treatment failure’ category were lower on average than those in the ‘treatment success’ category which may have contributed to a smaller reduction in the post-treatment ODI score due to a floor effect.
Study Limitations
The results of this study must be considered in light of several limitations. The sample size was relatively small, providing adequate power for only comparing the matched to unmatched treatments (and not the stabilization vs. Movement System Impairment exercises). While the physical therapy clinicians were trained to provide both treatment approaches (in case of vacation or unexpected absence from the clinic), they only provided one treatment the majority of the time. So although clinicians could not be blinded to treatment, this bias was reduced because each therapist delivered only one treatment. While the number of treatments given to each group was equal, the potential influence of the therapists cannot be discounted. The exclusion criteria used in this study should be taken into account when considering the clinical implications of the results. In particular, it is important to note that patients with signs of nerve root compression or prior surgery to the low back were excluded.
Conclusion
In summary, superior outcomes were not achieved for subjects with chronic LBP who received a matched treatment compared to subjects who received an unmatched treatment over a one year period.
Supplementary Material
Acknowledgments
The authors would like to acknowledge the consultation services of Dr. Julie Fritz on the Treatment Based Classification schema and the related standardized clinical exam items. The authors would also like to acknowledge the Vermont physical therapists that participated in this study: Justine Dee, MS PT, Matthew Odachowski, MPT and Jeffrey Albertson, MPT of Dee Physical Therapy, South Burlington; Janet Carscadden, PT and Andrea Trombley, MPT of Evolution Physical Therapy and Yoga, Burlington; Rose Bernier, PT, Traci Glanz, PT, Lucia Ryan, PT, Diane Stevens, PT and Sonya Worth, PT, PGDipHSc of Fletcher Allen Health Care, Burlington; Candice Brueck, MPT of Timberlane Physical Therapy, South Burlington; Karen Westervelt, PT, PGDipHSc and Jane Eliasson, PT of Copley Hosptial, Morrisville, Vermont. Data assistance was provided by Ms. Jennifer Chennette, Ms. Claire Freson and Ms. Kelsey McLaren.
Supported by NIH/NCMRR/2R01HD040909-07 (PI: SM Henry)
Appendix 1
Stabilization treatment protocol. Treatment included trunk motor control and strengthening exercises.
Appendix 2
Movement System Impairment treatment protocol. Treatment is outlined for three of the five Movement System Impairment categories that were treated in this study: Rotation, Rotation with Extension, and Rotation with Flexion categories. Treatment included positions for control of symptoms, modification of functional activities, and exercises for precision of trunk movement.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Preliminary results of this study were presented at the American Physical Therapy Association Combined Sections Meeting, New Orleans, LA, February 10, 2012.
Clinical Trials Registration: NCT01362049
References
- 1.Al-Obaidi SM, Beattie P, Al-Zoabi B, A-W S. The relationship of anticipated pain and fear avoidance beliefs to outcome in patients with chronic low back pain who are not receiving workers' compensation. Spine. 2005;30:1051–1057. doi: 10.1097/01.brs.0000160848.94706.83. [DOI] [PubMed] [Google Scholar]
- 2.Anderrsen G. Epidemiological features of chronic low-back pain. Lancet. 1999;354:581–585. doi: 10.1016/S0140-6736(99)01312-4. [DOI] [PubMed] [Google Scholar]
- 3.Andersson GBJ, Frymoyer JW. The Adult Spine. Lippincott-Raven Publishers; Philadelphia: 1997. The Epidemiology of Spinal Disorders. p. 93. [Google Scholar]
- 4.Bekkering GE, Hendriks HJM, Koes BW, et al. Dutch physiotherapy guidelines for low back pain. Physiotherapy. 2003;89:82–96. [Google Scholar]
- 5.Borkan JM, Cherkin DC. An agenda for primary care research on low back pain. Spine. 1996;21:2880–2884. doi: 10.1097/00007632-199612150-00019. [DOI] [PubMed] [Google Scholar]
- 6.Brennan GP, Fritz JM, Hunter SJ, Thackeray A, Delitto A, Erhard RE. Identifying subgroups of patients with acute/subacute “nonspecific” low back pain: results of a randomized clinical trial. Spine. 2006;31:623–631. doi: 10.1097/01.brs.0000202807.72292.a8. [DOI] [PubMed] [Google Scholar]
- 7.Costa LO, Maher CG, Latimer J, et al. Motor control exercise for chronic low back pain: a randomized placebo-controlled trial. Phys Ther. 2009;89:1275–1286. doi: 10.2522/ptj.20090218. [DOI] [PubMed] [Google Scholar]
- 8.Croft P. Low back pain. In: Stevens A, Raftery J, editors. Health Care Needs Assessment. Radcliffe Medical Press Oxford; New York, NY: 1997. p. 129. [Google Scholar]
- 9.Delitto A, Cibulka MT, Erhard RE, Bowling RW, Tenhula JA. Evidence for use of an extension-mobilization category in acute low back syndrome: A prescriptive validation pilot study. Phys Ther. 1993;73:216–222. doi: 10.1093/ptj/73.4.216. [DOI] [PubMed] [Google Scholar]
- 10.Delitto A, Erhard RE, Bowling RW. A treatment-based classification approach to low back syndrome: Identifying and staging patients for conservative treatment. Phys Ther. 1995;75:470–485. doi: 10.1093/ptj/75.6.470. [DOI] [PubMed] [Google Scholar]
- 11.Dutton M. Orthopedic examination, evaluation, and intervention. 2nd edition The McGraw-Hill Companies, Inc; 2008. [Google Scholar]
- 12.Elliott AM, Smith BH, Smith WC, WA C. Changes in chronic pain severity over time: the Chronic Pain Grade as a valid measure. Pain. 2000;88:303–308. doi: 10.1016/S0304-3959(00)00337-7. [DOI] [PubMed] [Google Scholar]
- 13.Erhard RE, Delitto A, Cibulka MT. Relative effectiveness of an extension program and a combined program of manipulation and flexion and extension exercises in patients with acute low back syndrome. Phys Ther. 1994;74:1093–1100. doi: 10.1093/ptj/74.12.1093. [DOI] [PubMed] [Google Scholar]
- 14.Fritz JM, Brennan GP, Clifford SN, Hunter SJ, A T. An examination of the reliability of a classification algorithm for subgrouping patients with low back pain. Spine. 2006;31:77–82. doi: 10.1097/01.brs.0000193898.14803.8a. [DOI] [PubMed] [Google Scholar]
- 15.Fritz JM, Childs JD, Flynn TW. Pragmatic application of a clinical prediction rule in primary care to identify patients with low back pain with a good prognosis following a brief spinal manipulation intervention. BMC Fam Pract. 2005;6:29. doi: 10.1186/1471-2296-6-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fritz JM, Cleland JA, Childs JD. Subgrouping patients with low back pain: evolution of a classification approach to physical therapy. J Orthop Sports Phys Ther. 2007;37:290–302. doi: 10.2519/jospt.2007.2498. [DOI] [PubMed] [Google Scholar]
- 17.Fritz JM, Delitto A, Erhard RE. Comparison of classification-based physical therapy with therapy based on clinical practice guidelines for patients with acute low back pain: a randomized clinical trial. Spine. 2003;28:1363–1371. doi: 10.1097/01.BRS.0000067115.61673.FF. [DOI] [PubMed] [Google Scholar]
- 18.Fritz JM, George S. The use of a classification approach to identify subgroups of patients with acute low back pain. Interrater reliability and short-term treatment outcomes. Spine. 2000;25:106–114. doi: 10.1097/00007632-200001010-00018. [DOI] [PubMed] [Google Scholar]
- 19.Fritz JM, Irrgang JJ. A comparison of a modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale. Phys Ther. 2001;81:776–788. doi: 10.1093/ptj/81.2.776. [DOI] [PubMed] [Google Scholar]
- 20.Fritz JM, Whitman JM, Childs JD. Lumbar spine segmental mobility assessment: an examination of validity for determining intervention strategies in patients with low back pain. Arch Phys Med Rehabil. 2005;86:1745–1752. doi: 10.1016/j.apmr.2005.03.028. [DOI] [PubMed] [Google Scholar]
- 21.Fritz JM, Whitman JM, Childs JD. Lumbar spine segmental mobility assessment: an examination of validity for determining intervention strategies in patients with low back pain. Arch Phys Med Rehabil. 2005;86:1745–1752. doi: 10.1016/j.apmr.2005.03.028. [DOI] [PubMed] [Google Scholar]
- 22.Frost H, Lamb SE, Stewart-Brown S. Responsiveness of a patient specific outcome measure compared with the Oswestry Disability Index v2.1 and Roland and Morris Disability Questionnaire for patients with subacute and chronic low back pain. Spine. 2008;33:2450–2457. doi: 10.1097/BRS.0b013e31818916fd. [DOI] [PubMed] [Google Scholar]
- 23.George SZ, Fritz JM, Childs JD. Investigation of elevated fear-avoidance beliefs for patients with low back pain: a secondary analysis involving patients enrolled in physical therapy clinical trials. J Orthop Sports Phys Ther. Feb. 2008;38:50–58. doi: 10.2519/jospt.2008.2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goubert L, Crombez G, De Bourdeaudhuij I. Low back pain, disability and back pain myths in a community sample: prevalence and interrelationships. Eur J Pain. Aug. 2004;8:385–394. doi: 10.1016/j.ejpain.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 25.Harris-Hayes M, Van Dillen LR. The Inter-Tester Reliability of Physical Therapists Classifying Low Back Pain Problems Based on the Movement System Impairment Classification System. PM&R. 2009;1:117–126. doi: 10.1016/j.pmrj.2008.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harris-Hayes M, Van Dillen LR, Sahrmann SA. Classification, treatment and outcomes of a patient with lumbar extension syndrome. Physiother Theory Pract. 2005;21:181–196. doi: 10.1080/09593980500212987. [DOI] [PubMed] [Google Scholar]
- 27.Hart LG, Deyo RA, Cherkin DC. Physician office visits for low back pain. Frequency, clinical evaluation, and treatment patterns from a U.S. national survey. Spine. 1995;20:11–19. doi: 10.1097/00007632-199501000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Hebert J, Koppenhaver S, Magel J, JM F. The relationship of transversus abdominis and lumbar multifidus activation and prognostic factors for clinical success with a stabilization exercise program: a cross-sectional study. Arch Phys Med Rehabil. 2009;91:78–85. doi: 10.1016/j.apmr.2009.08.146. [DOI] [PubMed] [Google Scholar]
- 29.Henry SM, Fritz JM, Trombley AL, JY B. Reliability of the Treatment Based Classification System for Subgrouping People with Low Back Pain. J Orthop Sports Phys Ther. 2012;42:797–805. doi: 10.2519/jospt.2012.4078. [DOI] [PubMed] [Google Scholar]
- 30.Henry SM, Van Dillen LR, Tromley AL, Dee JM, JY B. Reliability of novice raters in using the movement system impairment approach to classify people with low back pain. Manual Ther. 2013;18:35–40. doi: 10.1016/j.math.2012.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Henry SM, Hitt JR, Jones SL, Bunn JY. Decreased limits of stability in response to postural perturbations in subjects with low back pain. Clin Biomech (Bristol, Avon) 2006;21:881–892. doi: 10.1016/j.clinbiomech.2006.04.016. [DOI] [PubMed] [Google Scholar]
- 32.Hicks GE, Fritz JM, Delitto A, McGill SM. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Arch Phys Med Rehabil. 2005;86:1753–1762. doi: 10.1016/j.apmr.2005.03.033. [DOI] [PubMed] [Google Scholar]
- 33.Hicks GE, Fritz JM, Delitto A, Mishock J. Interrater reliability of clinical examination measures for identification of lumbar segmental instability. Arch Phys Med Rehabil. 2003;84:1858–1864. doi: 10.1016/s0003-9993(03)00365-4. [DOI] [PubMed] [Google Scholar]
- 34.Hides JA, Jull GA, Richardson CA. Long-term effects of specific stabilizing exercises for first-episode low back pain. Spine. 2001;26:E243–248. doi: 10.1097/00007632-200106010-00004. [DOI] [PubMed] [Google Scholar]
- 35.Hides JA, Richardson CA, Jull GA. Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain. Spine. 1996;21:2763–2769. doi: 10.1097/00007632-199612010-00011. [DOI] [PubMed] [Google Scholar]
- 36.Jensen MP, Turner JA, Romano JM. What is the maximum number of levels needed in pain intensity measurement? Pain. 1994;58:387–392. doi: 10.1016/0304-3959(94)90133-3. [DOI] [PubMed] [Google Scholar]
- 37.Jones SL, Henry SM, Raasch CC, JR. H. Individuals with chronic low back pain in an active episode demonstrate temporal but not spatial altered torque responses and directionally-specific enhanced muscle activity following unexpected balance perturbations. Exp Brain Res. 2012;221:413–426. doi: 10.1007/s00221-012-3183-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kamper SJ, Maher CG, Hancock MJ, Koes BW, Croft PR, Hay E. Treatment-based subgroups of low back pain: a guide to appraisal of research studies and a summary of current evidence. Best Pract Res Clin Rheumatol. 2010;24:181–191. doi: 10.1016/j.berh.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 39.Katz J. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006;88:21–24. doi: 10.2106/JBJS.E.01273. [DOI] [PubMed] [Google Scholar]
- 40.Koumantakis GA, Watson PJ, Oldham JA. Trunk muscle stabilization training plus general exercise versus general exercise only: randomized controlled trial of patients with recurrent low back pain. Phys Ther. 2005;85:206–208. [PubMed] [Google Scholar]
- 41.Lauridsen HH, Hartvigsen J, Manniche C, Korsholm L, Grunnet-Nilsson N. Responsiveness and minimal clinically important difference for pain and disability instruments in low back pain patients. BMC Musculoskelet Disord. 2006;7:82. doi: 10.1186/1471-2474-7-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Maluf KS, Sahrmann SA, Van Dillen LR. Use of a classification system to guide nonsurgical mangement of a patient with chronic low back pain. Phys Ther. 2000;80:1097–1111. [PubMed] [Google Scholar]
- 43.Mannion AF, Muntener M, Taimela S, Dvorak J. Comparison of three active therapies for chronic low back pain: Results of a randomized clinical trial with one-year follow-up. Rheumatology. 2001;40:772. doi: 10.1093/rheumatology/40.7.772. [DOI] [PubMed] [Google Scholar]
- 44.McGill SM. Low back exercises: evidence for improving exercise regimens. Phys Ther. 1998;78:754–765. doi: 10.1093/ptj/78.7.754. [DOI] [PubMed] [Google Scholar]
- 45.McHorney CA, Ware JE, Jr., Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–263. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 46.McKenzie R, May S. The Lumbar Spine: Mechanical Diagnosis & Therapy Volume 1. Spinal Publications New Zealand Ltd; Waikanae, New Zealand: 2003. [Google Scholar]
- 47.Melnick MS, Saunders HD, Saunders R. Self Help Manual: Managing Back Pain; Daily Activities Guide for Back Pain Patients. The Saunders Group, Inc.; St. Paul, MN: 1998. [Google Scholar]
- 48.Nordin M, Weiser S, van Doorn JW, Hiebert R, Rom. WN. Environmental and Occupational Medicine. Lippincott-Raven Publishers; Philadelphia, PA: 1998. Nonspecific low back pain. p. 947. [Google Scholar]
- 49.Pengel LH, Herbert RD, Maher CG, KM R. Acute low back pain: systematic review of its prognosis. Brit Med J. 2003;327:323. doi: 10.1136/bmj.327.7410.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Richardson C, Jull G. An historical perspective on the development of clinical techniques to evaluate and treat the active stabilising system of the lumbar spine. Australian Physiotherapy. 1995;1:5–13. [Google Scholar]
- 51.Richardson C, Jull G, Hodges P, Hides J. Therapeutic exercise for spinal segmental stabilization in low back pain: Scientific basis and clinical approach Edinburgh: Churchill Livingstone. 1999 [Google Scholar]
- 52.Sahrmann SA. Diagnosis and Treatment of Movement Impairment Syndromes. Mosby, Inc; St. Louis, MO: 2002. Movement impairment syndromes of the lumbar spine. p. 5. [Google Scholar]
- 53.Severeijns R, Vlaeyen JW, van den Hout MA, WE W. Pain catastrophizing predicts pain intensity, disability, and psychological distress independent of the level of physical impairment. Clin J Pain. 2001;17:165–172. doi: 10.1097/00002508-200106000-00009. [DOI] [PubMed] [Google Scholar]
- 54.Smith BH, Penny KI, Purves AM, et al. The Chronic Pain Grade questionnaire: validation and reliability in postal research. Pain. 1997;71:141–147. doi: 10.1016/s0304-3959(97)03347-2. [DOI] [PubMed] [Google Scholar]
- 55.Spitzer WO, LeBlanc FE, Dupuis M. Scientific approach to the assessment and management of activity related spinal disorders: A monograph for clinicians. Report of the Quebec Task Force on Spinal Disorders. Spine. 1987;12:S1–S59. [PubMed] [Google Scholar]
- 56.Stanton T, Fritz J, Hancock M, et al. Evaluation of a treatment based classification algorithm for low back pain: a cross-sectional study. Phys Ther. 2011;91:1–14. doi: 10.2522/ptj.20100272. [DOI] [PubMed] [Google Scholar]
- 57.Steiger F, Wirth B, de Bruin ED, AF. M. Is a positive clinical outcome after exercise therapy for chronic non-specific low back pain contingent upon a corresponding improvement in the targeted aspect(s) of performance? A systematic review. Eur Spine J. 2012;21:575–598. doi: 10.1007/s00586-011-2045-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stratford P, Gill C, Westaway M, Binkley J. Assessing disability and change on individual patients: A report of a patient specific measure. Physiotherapy Canada. 1995;47:258–263. [Google Scholar]
- 59.Trudelle-Jackson E, Sarvaiya-Shah SA, SS W. Interrater reliability of a movement impairment-based classification system for lumbar spine syndromes in patients with chronic low back pain. J Ortho Sports Phys Ther. 2008;38:371–376. doi: 10.2519/jospt.2008.2760. [DOI] [PubMed] [Google Scholar]
- 60.Van Dillen LR, Sahrmann SA, Norton BJ, et al. Reliability of physical examination items used for classification of patients with low back pain. PhysTher. 1998;78:979–988. doi: 10.1093/ptj/78.9.979. [DOI] [PubMed] [Google Scholar]
- 61.Van Dillen LR, Sahrmann SA, Norton BJ, Caldwell CA, McDonnell MK, Bloom NJ. The effect of modifying patient-preferred spinal movement and alignment during symptom testing in patients with low back pain: a preliminary report. Arch Phys Med Rehabil. 2003;84:313–322. doi: 10.1053/apmr.2003.50010. [DOI] [PubMed] [Google Scholar]
- 62.Van Dillen LR, Sahrmann SA, Wagner JM. Classification, intervention, and outcomes for a person with lumbar rotation with flexion syndrome. Phys Ther. 2005;85:336–351. [PubMed] [Google Scholar]
- 63.Verkerk K, Luijsterburg PA, Miedema HS, Pool-Goudzwaard A, BW K. Prognostic factors for recovery in chronic nonspecific low back pain: a systematic review. Phys Ther. 2012;92:1093–1108. doi: 10.2522/ptj.20110388. [DOI] [PubMed] [Google Scholar]
- 64.Waddell G. Subgroups within “nonspecific” low back pain. J Rheumatol. 2005;32:395–396. [PubMed] [Google Scholar]
- 65.Waddell G, McCulloch JA, Kummel E, Venner RM. Nonorganic physical signs in low-back pain. Spine. 1980;5:117–125. doi: 10.1097/00007632-198003000-00005. [DOI] [PubMed] [Google Scholar]
- 66.Wand BM, O'Connell NE. Chronic non-specific low back pain - sub-groups or a single mechanism? BMC Musculoskelet Disord. 2008;9:11. doi: 10.1186/1471-2474-9-11. 2266926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ware JE, Kosinski M, JE D. How to score version two of the SF-36 Health Survey. QualityMetric, Inc; Lincoln, RI: 2000. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.