Abstract
Background
There has been no study carried out to assess health service utilization by people with common mental disorder (CMD) in Malawi.
Aim
The aim of the study was to evaluate health service utilization patterns of patients with CMD in primary health care (PHC) clinics.
Methods
The study was conducted in two PHC clinics in one of the 28 districts in Malawi. Face-to-face interviews with the Self-Reporting Questionnaire (SRQ-20) were conducted in a sample of 323 PHC attendees aged 18 years and older who attended the PHC clinics for any reason.
Results
The prevalence of probable CMD in the sample was 20.1%. People with probable CMD had a higher mean number of health facility visits in the previous three months compared to those without probable CMD (1.6 vs 1.19, p = .02).
Conclusion
The study reveals high utilization of health services for people with CMD in the PHC setting. There is a need for PHC workers to improve skills in diagnosing patients with CMD to make PHC services more effective by reducing re-attendance and improving patient outcomes.
Keywords: Common mental disorder, depression, health service utilization, primary health care, developing countries
Background
Common mental disorders (CMDs) are defined as ‘depressive and anxiety disorders which are classified as neurotic, stress-related, somatoform disorders and mood disorders in the ICD-10′ (Patel & Kleinman, 2003, p. 609). CMDs, according to the World Health Organization (WHO, 2008), are among the leading cause of disability in low-income countries like Malawi. In Malawi, as in other developing countries in sub-Saharan Africa, access to services for people with mental health problems is poor. Mental health care services in Malawi are not yet well integrated into primary health services, but are still largely centralized to the three psychiatric units in the country, with only a small proportion of patients (mostly with severe mental illnesses) accessing the services (Kauye et al., 2011). Furthermore, in Malawi, non-specialized health care workers provide mental health services in the primary care settings, and given the workload at the primary health care (PHC) setting level, little time is available to screen for mental disorders and hence they go unrecognized. Evidence indicates that CMD indeed often goes undetected in primary care (Licht-Strunk, Beekman, de Haan & van Marwijk, 2009). Therefore, there is a possibility that a significant proportion of patients attending PHC services in Malawi may have CMD that goes undetected.
In Malawi, the WHO in 2002 estimated that depression was the fourth-leading cause of disability (Bowie, 2006). The available published data in Malawi show the prevalence to be at 29.9% for maternal CMD (Stewart et al., 2008) and at 28. 8% for CMD of people attending PHC services (Kauye et al., 2011). One study in the northern region of Malawi of people attending antiretroviral therapy clinics found a prevalence rate of 14.4% of psychological distress (Mwale, Stewart & Mathanga, 2007).
Despite mental health problems contributing a significant percentage of the disease burden in Malawi, there is a paucity of research in the area of mental health and in particular a lack of data regarding CMDs in the community and primary care, and health service utilization.
The purpose of this study was to determine the rate of CMDs in a population of PHC users in Zomba, Malawi, and to determine their patterns of health service utilization.
Methods
Ethical approval for this research was obtained from both the Health Research Ethics Committee at Stellenbosch University, South Africa (reference number S12/05/131) and the College of Medicine Research and Ethics Committee, University of Malawi, Malawi (reference number P06/12/1238), and the study was undertaken in accordance with the principles of the Declaration of Helsinki.
The study was a cross-sectional survey conducted in two PHC clinics in Zomba, Malawi. The sample size was calculated using Lwanga and Lameshow (1991)’s formula for cross-sectional surveys. The assumptions made for the sample size determination were a proportion of CMD of 30% (Kauye et al., 2011; Stewart et al., 2008), a 95% confidence interval and margin of error of 5%. This gave us a total sample size of 323. The study included all consecutive patients aged 18 years and older who attended the PHC clinics for any reason. The exclusion criteria were: (1) non-consent; (2) being in an emergency condition needing urgent medical care or admission; and (3) being under 18 years of age.
Interviews
Socio-demographic questionnaire
We collected data on age, gender, marital status, education, employment status, religion and household income.
Self-Reporting Questionnaire (SRQ-20)
The WHO designed the SRQ-20 as a screening tool for CMD (Stewart et al., 2009). The SRQ-20 comprises 20 questions exploring symptoms of depression, anxiety and somatic complaints (Stewart et al., 2009). The SRQ-20 was validated in Malawi and details of the Chichewa version of the questionnaire are published elsewhere (Stewart et al., 2009). We used the SRQ-20 to identify the probable cases of CMD in the PHC attendees. As observed in a previous study, the SRQ-20 is not designed to detect specific mental disorder diagnoses (Havenaar, Geerlings, Vivian, Collinson & Robertson, 2008) and in this study it was used to assess symptoms that were suggestive of possible mental disorder. We used a cut-off point of 7/8 because a previous study carried out in Malawi found this cut-off point to give a good balance between sensitivity, specificity and positive predictive (Stewart et al., 2009). This meant that the participants scoring 8 or above were considered as having probable CMD and those scoring 7 or less as having no probable CMD.
PHC encounter form
The questionnaire generated the clinical diagnostic data. The data included diagnoses, presence of a psychological problem, and management. The PHC encounter form was filled in by the PHC clinicians who saw the service users as part of their regular work. These PHC clinicians had three years’ general training, and six weeks’ training in mental health. The form required the clinician to rate the patient’s level of psychiatric disturbance on a scale of 0 (no disturbance) to 5 (severe disturbance), with a score of 2 or more representing the presence of a psychological problem. This form was similar to that used in previous studies (Boardman, 1987; Liu, Mann, Cheng, Tjung & Hwang, 2004; Maginn et al., 2004; Üstün & Sartorius, 1995). It has shown to be of great utility in efforts to identify clinicians’ detection rate.
Health service utilization encounter questionnaire
This interview elicited information on the use of health care services. This questionnaire on service utilization patterns was adapted and modified from the Canadian Community Health Survey (CCHS 1.2; Vasiliadis, Lesage, Adair & Boyer, 2005). It was divided into two parts: the first was used to elicit the self-perception of mental health and the second to measure for a utilization pattern of health services including PHC and traditional healers.
Procedure
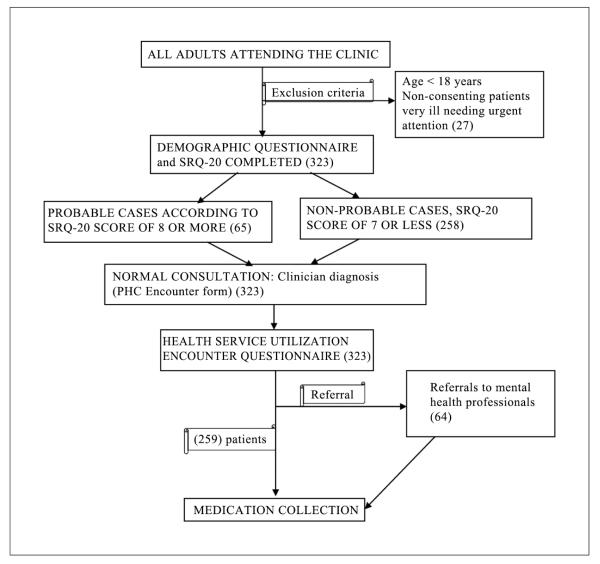
The study was done in one of the 28 districts of Malawi in which 13 public health centres and a convenient sample of two health centres (one urban and one rural) was chosen. All consecutive patients aged 18 years and above attending routine PHC clinics for any reason were asked to take part in the study. Following informed consent, the participants were asked to provide some demographic information and complete the SRQ-20. The research assistant orally administered the SRQ-20 due to low literacy of the study participants. The first research assistant administered the demographic questionnaire and the SRQ-20 to the client. These data were collected before the PHC clinician saw the patient. For each participant completing the SRQ-20, the clinician completed a PHC encounter form. The information collected included the reason for the consultation, diagnoses, rating of the presence of psychiatric disturbance and immediate management plan. Each clinician was unaware of the patient’s responses to the SRQ-20 and their score. Upon exiting the room, the patient met the second research assistant who administered the health service utilization questionnaire to elicit the utilization pattern of health services. The second research assistant was also unaware of the SRQ-20 score (see Figure 1).
Figure 1.
Instruments and study procedure used at clinic level.
Data analysis
Data were collated and processed using the SPSS 16.0 statistical package. The statistics included: descriptive statistics (means, standard deviations and frequency analysis); inferential statistics (paired-samples t-test, independent-samples t-test and χ2 test). We used χ2 statistics to test for association and the odds ratio was used to check for the direction of association. To test the relationship between CMD and attendance at each health care service, a logistic model with SRQ-20 cut-off of 7/8 was used. The logistic equation modelled the odds of CMD as an exponential coefficient of number of visit to health care facility or traditional healer. Probable cases for CMD were defined as those people who scored 8 or more on the SRQ-20. During analysis, we re-coded the PHC clinician-rated mental health status into three levels: none to subclinical; mild; and moderate to severe, in which a rating of 2 or more on the five-point scale provided by the PHC clinician indicated that a CMD had been detected (Liu et al., 2004; Maginn et al., 2004). We performed the clinician detection analysis using an identification index. This index was calculated using an adapted version of the method used by Maginn and colleagues (2004). The following equation shows how the two ratings obtained from the SRQ and PHC clinician scales were used to compute the identification index. We used a sensitivity of 59 for the SRQ-20 (Stewart et al., 2009).
Results
Sample description
A total of 323 participants who met the inclusion criteria were interviewed with a response rate of 100%. The socio-demographic profiles of the participants revealed that most of them were in the age group 18–31 (41.8%), female (74%), Christian (67%), married (65%) and unemployed (55%). The socio-demographic profiles also revealed that 22% of the participants had no education at all, 54% had attended primary education, 22% attained secondary education and only 2% had attained tertiary education. Half of the participants (53%) had below-average annual household income status, 33.1% had above-average household income status and only 13.9% had an average annual household income of K50,000 (US$153. 64).
Prevalence of probable CMD among PHC attendees as identified by the SRQ-20
Sixty-five participants (20.1%) were identified as having probable CMD using the SRQ-20 cut-off point of 7/8. The prevalence of probable CMD was 20.7% in women and 18.6% in men. The eight most frequently endorsed SRQ-20 symptoms in the probable cases were poor sleep (66.2%), frequent headaches (83.1%), nervous or worried (72.3%), uncomfortable feelings in stomach (75.4%), trouble thinking (72.3%), tired all the time (73.8%), easily tired (76.9%) and feeling unhappy (83.1%). Of those participants who scored 8 and above, 23.1 % had thought of ending their life.
Socio-demographic characteristics of patients with and without probable CMD
The probable CMD group comprised 65 patients, 24.6% of whom were male and 75.4% female. The non-probable CMD group had 258 patients: 27.1% males and 72.1% female (p = .682). Over half of the participants in both groups were married: 69.2% in the probable CMD group and 64.3% in the non-probable CMD group (p = .655). With regard to employment status, the probable CMD group had 49.2% unemployed participants, while the non-probable CMD group had 56.6% (p = .642). In terms of household income, 47.7% participants in the CMD group and 54.2% in the non-probable CMD group had an average annual household income (p = .570) (Table 1).
Table 1.
Comparison of socio-demographic characteristics between patients with and without probable CMD.
| Variable levels | Probable CMD % (n = 65) | No probable CMD % (n = 258) | p |
|---|---|---|---|
| Age (years) | .226 | ||
| 18–31 | 30.8 | 44.6 | |
| 32–45 | 38.5 | 34.5 | |
| 46–59 | 12.3 | 11.2 | |
| 60–73 | 15.4 | 7.4 | |
| 74–87 | 3.1 | 1.9 | |
| 88–96 | 0 | 0.4 | |
| Gender | .682 | ||
| Female | 75.4 | 72.9 | |
| Male | 24.6 | 27.1 | |
| Education | .456 | ||
| No education | 27.7 | 20.2 | |
| Primary school | 46.2 | 55.8 | |
| Secondary | 24.6 | 21.7 | |
| Tertiary | 1.5 | 2.3 | |
| Marital status | .655 | ||
| Married | 69.2 | 64.3 | |
| Single | 7.7 | 12.0 | |
| Widowed | 12.3 | 10.1 | |
| Separated/divorced | 10.8 | 13.6 | |
| Employment status | .642 | ||
| Unemployed | 49.2 | 56.6 | |
| Student | 6.2 | 7.0 | |
| Employed | 7.7 | 7.8 | |
| Retired | 3.1 | 1.2 | |
| Self-employed | 33.8 | 27.5 | |
| Religious affiliation | .455 | ||
| Christian | 70.8 | 65.9 | |
| Muslim | 29.2 | 34.1 | |
| Economic status | .570 | ||
| Above average | 38.5 | 31.8 | |
| Average | 13.8 | 14.0 | |
| Below average | 47.7 | 54.2 |
Detection rate of CMD
The PHC clinicians recorded at least one diagnosis for the 323 study participants. Many patients had diagnoses of physical conditions. The proportion of patients with probable CMD as identified by SRQ-20 and treated for clinically diagnosed malaria was 15.4%, respiratory tract infection was 16.9%, musculoskeletal pain was 18.5% and dyspepsia was 13.8%. Psychological diagnosis was considered by the PHC clinician in one of the participants. PHC clinicians recognized only 6.2% of the patients who had been detected as having a probable CMD by the SRQ-20 as ‘subclinically ill’. There was no clinician rating of 2 or more (CMD detected) for the patients detected as having probable CMD by the SRQ-20. We found the identification index to be 0.017.
CMD and health service utilization
The participants with probable CMD used health centres more than those without CMD (mean number of visits in past three months of 1.6 vs 1.19, p = . 02) (Table 2). Very few people sought health care at the traditional healers. Among those who used traditional healers, the average number of visits was 0.05 for those with probable CMD and 0.08 for those without, but the difference was not statistically significant (p = .565). The average number of visits for those with probable CMD who visited both health centres and traditional healers was higher than in participants without probable CMD. This difference was statistically significant (1.68 vs 1.24, p = .019).
Table 2.
Pattern of use of health services among participants with and without probable CMD.
| Average number of visits in past three months | Probable CMD | No probable CMD | p |
|---|---|---|---|
| To health facility | 1.6 | 1.19 | .02 |
| To traditional healer | 0.05 | 0.08 | .565 |
| Total | 1.68 | 1.24 | .019 |
Association between probable CMD and utilization of health service
A model on the number of times of different health service visits associated with probable CMD was used (Table 3). In the logistic model for the probable CMD sample, the odds of probable CMD increased significantly with each visit to a health facility by 1.27 (p = . 024). At the same time, odds of probable CMD increased with 1.13 on each visit to traditional healer, but this was not significant (p = . 77).
Table 3.
Model on number of visits to health facility or traditional healer associated with probable CMD.
| Variable | Probable CMD |
|||
|---|---|---|---|---|
| Step 1a | B | Wald | OR [exp(B)] | p |
| Number of times for health facility visit | 0.239 | 5.077 | 1. 270 | .024 |
| Number of times for traditional healer visit | 0.130 | 0.085 | 1. 138 | . 770 |
| Constant | −1.718 | 65.857 | 0.179 | < .001 |
Variable(s) entered on step 1: HF: health facility, TH: traditional healer.
Discussion
We found the prevalence of probable CMD in this setting to be 20.1%, which is similar to other findings from developing countries where the prevalence rate of mental CMD ranges from 20% to 30% (Patel & Kleinman, 2003). Gender was not significantly associated with CMD, unlike in a number of other studies where females have been found to be more affected (Cwikel, Zilber, Feinson & Lerner, 2008; Havenaar et al., 2008; Lu et al., 2008; Sawyer, Pfeiffer & Spence, 2009). In this study, poor household income was not significantly associated with CMD, but this is not surprising as the whole sample was of low socio-economic status.
As in other studies, we found a very low detection rate of mental disorder by PHC clinicians (Avasthi et al., 2008; Badamgarav et al., 2003; Licht-Strunk et al., 2009; Ndetei et al., 2009). This could be attributed to both patient and clinician factors: patients may not mention mental disorder symptoms to clinicians, and clinicians may not ask about these symptoms, possibly through lack of knowledge or because of attitudinal issues (Tansella & Thornicroft, 2005), or because of high workload.
A further factor may well be the substantial comorbidity known to exist between mental and physical disorders. In this study, diagnosis of malaria and dyspepsia, among others, were prominent among those who had probable CMD. This finding is similar to a Kenyan study, which found that 46% of the primary care attendees with CMD were unrecognized and misdiagnosed as having malaria, typhoid, amoebiasis and other diagnoses (Jenkins et al., 2010). The diagnosis of malaria in our study was made on clinical assessment; rapid diagnostic tests or microscopy was not used. This observation is similar to findings in Kenya that showed that only 10% of patients who had been clinically diagnosed with malaria actually had it (Jenkins et al., 2010; Zurovac, Midia, Ochola, English & Snow, 2006).
In the same vein, the finding of dyspepsia in this study is similar to a previous study by Mujakovic and colleagues (2009), who found that PHC patients consulting for dyspepsia had higher levels of depression and somatization. In the present study, it is not clear whether dyspepsia is proxy for expressing CMD or a vague feeling of indigestion that would suggest somatization. A similar argument may be made for pain symptoms, which were also common. It may be the case that PHC clinicians record dyspepsia and pain as the cause for consultation because these terms are less stigmatizing than are diagnoses of mental disorder, a possibility that requires further examination in subsequent studies.
Under-diagnosis of mental disorders results in lack of treatment for such disorders, and is a serious issue. The question of under-diagnosis will need to be investigated in further studies, preferably including a component that observes clinical practices.
A number of studies have established a relationship between frequent PHC visits and CMD (Jacobi, Klose & Wittchen, 2004; Kramer & Garralda, 2000; Tansella & Thornicroft, 2005). The present study found that people with probable CMD had a higher average number of health facility visits in the previous three months compared to those without probable CMD. However, there was no significant difference in the average number of traditional healer visits in the previous three months between those with and without probable CMD.
Strengths and limitations
The strengths of this study were the use of a validated measure for probable CMD and conducting the study in the PHC setting, which allowed us to examine the prevalence of probable CMD and the utilization of health services. One limitation is that since the study design was cross-sectional, it is difficult to draw causal inferences from the findings. The findings can be generalized to health centres that have the same clinic characteristics as those in Zomba district, but they cannot be generalized to the community. On the other hand, the findings reflect areas for further research. Another limitation is that the use of self-reported data for health care utilization in the preceding three months was prone to recall bias; however, we considered this by limiting it to three months and minimizing the length of the health care service utilization instrument.
Implications for research
This study can act as a platform from which further research may be conducted. The evidence from this study has demonstrated the need for further research to determine the nature and prevalence of CMD in the community and in attendees of traditional healers. Future research should also investigate the awareness of mental health, the help-seeking behaviour of patients with mental health problems in the community and the use of health care service in the community, in order to come up with evidence-based mental health strategies. Given the likely influence of physical symptoms on the misdiagnosis of CMD, a qualitative study is imperative to explore whether dyspepsia or musculoskeletal pain may constitute proxies for expressing CMD, or whether they may be indicative of somatization. As part of this study, diagnostic practices of clinicians could also be explored, examining whether clinicians use these categories to avoid diagnosing stigmatized CMD.
Implications for policy and practice
Improving patient outcomes and reducing re-attendance can be achieved through improved recognition of psychological symptoms. Therefore, there is a need for PHC workers to be refreshed periodically on identifying and treating CMD through continuing professional development (CPD) programmes. Intervention on patient disclosure could also be effective in helping to improve clinician recognition, hence there is a need to direct efforts towards creating awareness about mental health and to encourage patient disclosure of psychological or mental health issues.
Conclusion
This study has revealed the magnitude of CMD that is prevalent in PHC centres that goes unrecognized and untreated. The high utilization of health services suggests that there may be a large treatment gap in terms of mental health care in the PHC setting. The study also shows that the screening questionnaire for mental disorders could identify PHC patients who are at risk for CMD and higher utilization. We therefore conclude that there might be high unmet need of mental health services in the PHC setting. These findings suggest that despite the fact that CMD seems prevalent among PHC attendees, the majority of them may not aware that psychological factors contribute to their symptoms. Considering the fact that the participants in this study did not mainly seek help at the health centre for mental health problems but for a general medical condition, in order to assist in making a correct diagnosis there is a need to ask screening questions about CMD to those patients with medically unexplained symptoms and to those with an increased number of visits. We therefore recommend that PHC workers should improve their skills in diagnosing CMD.
Acknowledgement
We thank Chitsanzo Mafuta and Benson Kampapa for their assistance with the screening, interviews and data management, and Ereshia Benjamin, Crick Lund, Mark Tomlinson and Ashraf Kagee for technical support. We also thank the clinical officers and patients at the two PHC clinics.
Funding The project described was supported by the Africa Focus on Intervention Research for Mental health (AFFIRM) Collaborative Hub, Grant Number U19MH095699 from the National Institute Of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute Of Mental Health or the National Institutes of Health. The Scotland-Malawi Mental Health Education Project (SMMHEP) and Zomba Mental Hospital also supported this study. Leslie Swartz was supported by the South African National Research Foundation. The work was conducted as part of the activities of the Alan J. Flisher Centre for Public Mental Health based jointly at Stellenbosch University and University of Cape Town. The views expressed in this article are those of the authors and of no other person or organization. This work is based on research supported in part by the National Research Foundation of South Africa (Grant specific unique reference number (UID) 85423). The Grantholder (Leslie Swartz) acknowledges that opinions, findings and conclusions or recommendations expressed in any publication generated by the NRF supported research are that of the author(s), and that the NRF accepts no liability whatsoever in this regard.
Footnotes
Authors’ contributions MU, LS, FK and RS conceptualized and designed the study, and contributed to the conduct of the study. MU participated in the acquisition of data and was responsible for drafting the manuscript. LS, FK and RS reviewed the manuscript for intellectual content and contributed to its revision. All authors read and approved the final manuscript.
Competing interests The authors declare that they have no competing interests.
References
- Avasthi A, Varma SC, Kulhara P, Nehra R, Grover S, Sharma S. Diagnosis of common mental disorders by using PRIME-MD Patient Health Questionnaire. Indian Journal of Medical Research. 2008;127:159–164. [PubMed] [Google Scholar]
- Badamgarav E, Weingarten SR, Henning JM, Knight K, Hasselblad V, Gano A, Jr., Ofman JJ. Effectiveness of disease management programs in depression: A systematic review. American Journal of Psychiatry. 2003;160:2080–2090. doi: 10.1176/appi.ajp.160.12.2080. [DOI] [PubMed] [Google Scholar]
- Boardman AP. The General Health Questionnaire and the detection of emotional disorder by general practitioners: A replicated study. British Journal of Psychiatry. 1987;151:373–381. doi: 10.1192/bjp.151.3.373. [DOI] [PubMed] [Google Scholar]
- Bowie C. The burden of diseases in Malawi. Malawi Medical Journal. 2006;18:103–110. [PMC free article] [PubMed] [Google Scholar]
- Cwikel J, Zilber N, Feinson M, Lerner Y. Prevalence and risk factors of threshold and sub-threshold psychiatric disorders in primary care. Social Psychiatry and Psychiatric Epidemiology. 2008;43:184–191. doi: 10.1007/s00127-007-0286-9. [DOI] [PubMed] [Google Scholar]
- Havenaar JM, Geerlings MI, Vivian L, Collinson M, Robertson B. Common mental health problems in historically disadvantaged urban and rural communities in South Africa: Prevalence and risk factors. Social Psychiatry and Psychiatric Epidemiology. 2008;43:209–215. doi: 10.1007/s00127-007-0294-9. [DOI] [PubMed] [Google Scholar]
- Jacobi F, Klose M, Wittchen HU. Mental disorders in the community: Healthcare utilization and disability days] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2004;47:736–744. doi: 10.1007/s00103-004-0885-5. [DOI] [PubMed] [Google Scholar]
- Jenkins R, Kiima D, Okonji M, Njenga F, Kingora J, Lock S. Integration of mental health into primary care and community health working in Kenya: Context, rationale, coverage and sustainability. Mental Health in Family Medicine. 2010;7:37–47. [PMC free article] [PubMed] [Google Scholar]
- Kauye F, Chiwandira C, Wright J, Common S, Phiri M, Mafuta C, Udedi M. Increasing the capacity of health surveillance assistants in community mental health care in a developing country, Malawi. Malawi Medical Journal. 2011;23:74–103. [PMC free article] [PubMed] [Google Scholar]
- Kramer T, Garralda ME. Child and adolescent mental health problems in primary care. Advances in Psychiatric Treatment. 2000;6:287–294. [Google Scholar]
- Licht-Strunk E, Beekman AT, de Haan M, van Marwijk HW. The prognosis of undetected depression in older general practice patients: A one year follow-up study. Journal of Affective Disorders. 2009;114:310–315. doi: 10.1016/j.jad.2008.06.006. [DOI] [PubMed] [Google Scholar]
- Liu SI, Mann A, Cheng A, Tjung JJ, Hwang LC. Identification of common mental disorders by general medical doctors in Taiwan. General Hospital Psychiatry. 2004;26:282–288. doi: 10.1016/j.genhosppsych.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Lu J, Ruan Y, Huang Y, Yao J, Dang W, Gao C. Major depression in Kunming: Prevalence, correlates and comorbidity in a south-western city of China. Journal of Affective Disorders. 2008;111:221–226. doi: 10.1016/j.jad.2008.02.018. [DOI] [PubMed] [Google Scholar]
- Lwanga SK, Lameshow S. Sample size determination in health studies: A practical manual. World Health Organization; Geneva: 1991. [Google Scholar]
- Maginn S, Boardman AP, Craig TK, Haddad M, Heath G, Stott J. The detection of psychological problems by general practitioners: Influence of ethnicity and other demographic variables. Social Psychiatry and Psychiatric Epidemiology. 2004;39:464–471. doi: 10.1007/s00127-004-0751-7. [DOI] [PubMed] [Google Scholar]
- Mujakovic S, de Wit NJ, van Marrewijk CJ, Fransen GA, Laheij RJ, Muris JW, Numans ME. Psychopathology is associated with dyspeptic symptom severity in primary care patients with a new episode of dyspepsia. Alimentary Pharmacology & Therapeutics. 2009;29:580–588. doi: 10.1111/j.1365-2036.2008.03909.x. [DOI] [PubMed] [Google Scholar]
- Mwale CM, Stewart R, Mathanga D. The prevalence of psychological distress and associated factors among people living with AIDS attending antiretroviral therapy clinics in Mzuzu, Malawi: A cross-sectional descriptive study. Malawi Medical Journal. 2007;19:56. [Google Scholar]
- Ndetei DM, Khasakhala LI, Kuria MW, Mutiso VN, Ongecha-Owuor FA, Kokonya DA. The prevalence of mental disorders in adults in different level general medical facilities in Kenya: A cross-sectional study. Annals of General Psychiatry. 2009;8:1. doi: 10.1186/1744-859X-8-1. doi:10.1186/1744-859X-8-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bulletin of the World Health Organization. 2003;81:609–615. [PMC free article] [PubMed] [Google Scholar]
- Sawyer MG, Pfeiffer S, Spence SH. Life events, coping and depressive symptoms among young adolescents: A one-year prospective study. Journal of Affective Disorders. 2009;117:48–54. doi: 10.1016/j.jad.2008.12.013. [DOI] [PubMed] [Google Scholar]
- Stewart RC, Kauye F, Umar E, Vokhiwa M, Bunn J, Fitzgerald M, Creed F. Validation of a Chichewa version of the self-reporting questionnaire (SRQ) as a brief screening measure for maternal depressive disorder in Malawi, Africa. Journal of Affective Disorders. 2009;112:126–134. doi: 10.1016/j.jad.2008.04.001. [DOI] [PubMed] [Google Scholar]
- Stewart RC, Umar E, Kauye F, Bunn J, Vokhiwa M, Fitzgerald M, Creed F. Maternal common mental disorder and infant growth: A cross-sectional study from Malawi. Maternal & Child Nutrition. 2008;4:209–219. doi: 10.1111/j.1740-8709.2008.00147.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tansella M, Thornicroft G, editors. Common mental disorders in primary care. Taylor & Francis; London: 2005. [Google Scholar]
- Üstün TB, Sartorius N, editors. Mental illness in general health care. John Wiley & Sons; Chichester: 1995. [Google Scholar]
- Vasiliadis HM, Lesage A, Adair C, Boyer R. Service use for mental health reasons: Cross-provincial differences in rates, determinants, and equity of access. Canadian Journal of Psychiatry. 2005;50:614–619. doi: 10.1177/070674370505001007. [DOI] [PubMed] [Google Scholar]
- WHO (World Health Organization) The global burden of disease: 2004 update. WHO Press; Geneva: 2008. [Google Scholar]
- Zurovac D, Midia B, Ochola SA, English M, Snow RW. Microscopy and outpatient malaria case management among older children and adults in Kenya. Tropical Medicine & International Health. 2006;11:432–440. doi: 10.1111/j.1365-3156.2006.01587.x. [DOI] [PubMed] [Google Scholar]