Abstract
We report a case of a patient presenting with clinical, radiological and endoscopic features of colitis due to a compressive left para-aortic mass. Total open surgical excision was performed, which resulted in complete resolution of colitis. Histopathology and immunohistochemistry revealed benign retroperitoneal schwannoma. These neural sheath tumors rarely occur in the retroperitoneum. They are usually asymptomatic but as they enlarge they may compress adjacent structures, which leads to a wide spectrum of non-specific symptoms, including lumbar pain, headache, secondary hypertension, abdominal pain and renal colicky pain. CT and MR findings show characteristic features, but none are specific. Schwannoma can be isolated sporadic lesions, or associated with schwannomatosis or neurofibromatosis type II (NF2). Although they vary in biological and clinical behavior, their presence is, in nearly every case, due to alterations or absence of the NF2 gene, which is involved in the growth regulation of Schwann cells. Both conditions were excluded by thorough mutation analysis. Diagnosis is based on histopathological examination and immunohistochemistry. Total excision is therapeutic and has a good prognosis. Schwannomatosis and NF2 should be excluded through clinical diagnostic criteria. Genetic testing of NF2 is probably not justified in the presence of a solitary retroperitoneal schwannoma.
Keywords: Colitis, Neurofibromatosis, Retroperitoneum, Schwannoma
INTRODUCTION
Schwannomas or neurilemmomas are encapsulated tumors arising from the neural sheath of peripheral nerves. They are usually present in the head and neck or in the upper extremities, but may appear in the posterior mediastinum and more rarely in the retroperitoneum. The latter are often found incidentally or may present with vague, non-specific symptoms if the tumor is large enough to compress surrounding structures.
We report a case of a benign retroperitoneal schwannoma with an unusual clinical presentation, its radiological, histopathological and genetic features, and its subsequent management.
CASE REPORT
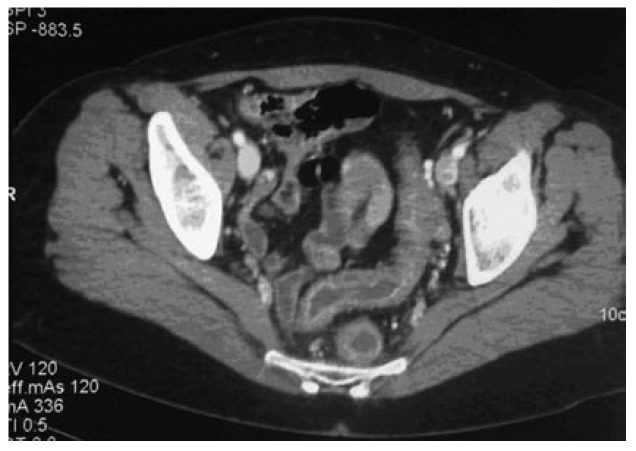
A 45-year-old woman was admitted to our emergency department for severe colicky abdominal pain with nausea and vomiting that started about 15 min after her last meal. She had no relevant medical history but mentioned having had back pain for the last 2 mo, which she thought was due to her increasing workload and stress at work. She denied having any abdominal problems until that day. On clinical examination, the patient was afebrile, pale and uncomfortable. Blood pressure and heart rate were normal. Abdominal examination showed a diffusely tender abdomen, more pronounced in the left lower quadrant. She had no guarding or rebound. Deep palpation of the abdomen revealed a non-tender, non-pulsatile mass left of the umbilicus. Rectal examination was unremarkable, except for the presence of a little blood. Within the first hour after admission, the patient suffered one episode of diarrhea stained with a moderate amount of fresh blood. Laboratory tests showed an increased white blood cell count (WBC) of 18000 cells/mm³ and C-reactive protein (CRP) of 1.1 mg/dL. Other values were within the normal range. At this point our differential diagnosis included diverticulitis and a contrast-enhanced computed tomodensitometry (CT) of the abdomen was performed. It revealed a diffuse infiltration around the rectum and the sigmoid colon, and a thickening of their walls (Figure 1). No diverticula were found. It also showed a well-demarcated, homogeneous, left para-aortic mass lying between the lumbar vertebrae and the left psoas muscle, which measured 60 × 50 mm (Figure 2). With few specific findings, the scan was considered inconclusive.
Figure 1.
Contrast-enhanced CT scan of the abdomen showing a diffuse infiltration around the rectum and the sigmoid colon, and thickening of their walls.
Figure 2.
Well-demarcated, homogeneous mass measuring 60×50 mm in close proximity to the left iliac artery, lumbar vertebrae and psoas muscle, on contrast-enhanced CT scanning.
She was hospitalized and received isotonic fluid resuscitation, and intravenous broad-spectrum antibiotics were commenced. Symptoms improved rapidly and disappeared almost completely 3 d after the initial complaints. During her hospital stay, several examinations were performed. First, the patient underwent colonoscopy to exclude inflammatory bowel disease (IBD). It revealed a diffusely edematous, slightly erythematous rectum and sigmoid colon, but no erosive or ulcerative lesions. Histopathological examination of biopsies taken during colonoscopy showed diffuse edema and signs of chronic inflammation, characterized by the presence of mostly lymphocytes and polynuclear granulocytes. Granulomas were absent. A few cryptic abscesses and zones of erosion were also found. The pathologist's diagnosis was chronic colitis, more pronounced in the sigmoid colon than the left colon, and excluded IBD. In laboratory tests, WBC had fallen to a normal value at 9780 cells/mm³ after a rise to 12000. CRP level followed the same course to settle at 1.7 mg/dL, after it had risen to 10.8. Tumor markers CEA and CA 19.9 were within the normal range. Magnetic resonance imaging showed the same features as seen with CT scanning (Figure 3).
Figure 3.
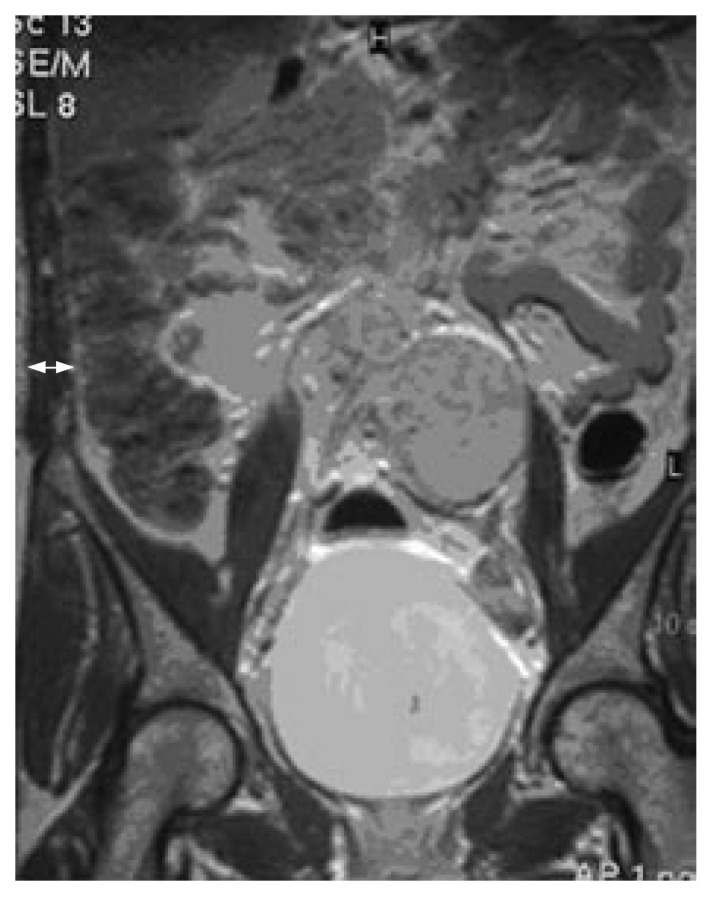
Coronal T1-weighted MR image using gadolinium, showing a solid mass with the same features as seen with CT scanning.
Since we believed that the mass caused the patient's signs and symptoms, we opted for open surgical excision. We approached the retroperitoneal space through a median laparotomy. During exploration and meticulous dissection of the mass, we noticed that it was in close proximity to the aorta and left iliac artery and vein, and seemed to arise from the left para-aortic sympathetic chain. It also adhered partially to the left psoas muscle and to the anterior aspect of the lumbar vertebrae. Complete excision was performed. Perioperative examination of the mass revealed a solid, greyish, spherical tumor with a smooth capsule and a heterogeneous core (Figure 4).
Figure 4.
Perioperative examination of the mass revealed a solid, greyish, ovoid tumor with a smooth capsule and a homogeneous yellow core.
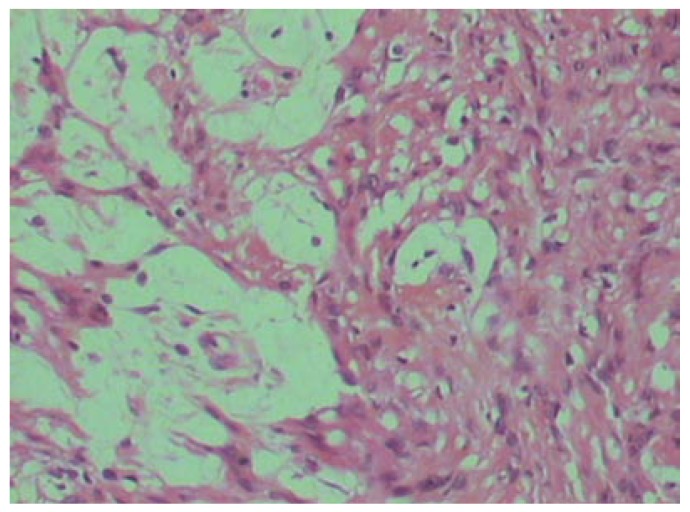
The postoperative course was uneventful. We noticed that the left leg was slightly warmer and dryer than the right, which suggested that we had performed a left lumbar sympathectomy, thus in favor of the excision of a tumor of neural origin. Microscopic histopathological examination revealed strings of spindle cells surrounded by a collagenous stroma that was partially hyalinized and showed cystic degeneration in some regions (Figure 5). There was some nuclear atypia with very limited mitotic activity, but no signs of malignancy. The tumor tested intensely positive for S-100 protein, which confirmed the diagnosis of benign schwannoma. The integrity of the capsule was also noted, which confirmed total excision of the mass. The patient was discharged from the hospital on the fifth postoperative day.
Figure 5.
Antoni A area on the right (well-organised spindle cells in a palisade pattern) and Antoni B area (less cellular, loose pleomorphic cells) on the left (HE, × 200).
Six weeks after surgery, she was still symptom free and signs of sympathectomy persisted. A CT scan and colonoscopy were performed to evaluate the evolution of colitis, which had completely resolved. Further investigations were performed to exclude neurofibromatosis type II (NF2) or schwannomatosis. Thorough physical examination was performed on the patient but no superficial tumors were found. Family history for schwannoma or meningioma was negative. MRI did not show any tumor of the central nervous system. Furthermore, the presence of a germline NF2 mutation was excluded by thorough mutation analysis on DNA extracted from the patient's lymphocytes. We performed direct sequencing of all coding exons of the NF2 gene. Deletion was excluded by multiplex ligation-dependent probe amplification (MLPA). We concluded that the schwannoma was most likely due to a somatic mutation in the NF2 gene.
DISCUSSION
Schwannomas, or neurilemmomas, are tumors arising from the Schwann cells of peripheral nerves[1,2]. They are usually found in the head and neck or in the upper extremities. Only 1% is found in the retroperitoneum, which accounts for 0.5%-1.2% of all retroperitoneal tumors[3,4]. They can be isolated as sporadic lesions or associated with schwannomatosis or NF2. Although they vary in biological and clinical behavior, their presence is in nearly every case due to alterations or absence of the NF2 gene (located on chromosome 22q12), which codes for merlin, a tumor suppressor protein involved in the growth regulation of Schwann cells, but its exact mechanism has not yet been elucidated. Most schwannomas are benign but (although very rarely) malignant degeneration can occur, and is usually associated with NF2[5]. Patients with benign retroperitoneal schwannomas are predominantly in their second to fifth decade, and women are twice as often affected as men[4,6].
On gross appearance, schwannomas are well-demarcated, solid tumors with a smooth surface and have an ovoid or spherical shape[7]. Sometimes, secondary changes such as hemorrhage, cysts and calcification can be present[1]. They are usually solitary and slow-growing tumors[1]. The retroperitoneum is non-restrictive, so that benign tumors are often able to grow to a large size before causing symptoms. These are generally vague and non-specific[7], and range from lumbar pain and neurological symptoms in the lower extremities[8], to renal colicky pain, with or without hematuria, if it involves the urogenital tract[9]. Abdominal complaints can also occur but are mainly vague and poorly localized, with some digestive disturbances[3,10,11]. Our patient's presentation was peculiar, not only because of the abrupt onset of her symptoms, but also because she had colitis. We believe that the tumor was large enough to compromise venous return in the mesocolon, which led to stasis characterized by the infiltration and parietal thickening seen on CT, the edematous and erythematous aspect seen during colonoscopy, and the chronic inflammation with edema seen on histopathological examination. This idea has been strengthened by the fact that those signs disappeared completely after removal of the tumor.
Diagnosis is rarely made preoperatively. The mass seen on the CT scan showed characteristic features of benign schwannoma. It was a well-demarcated, spherical, solitary mass and in a paravertebral position[6]. Contrast enhancement homogeneity was seen because no gross cystic degeneration or calcification had yet occurred. Most authors agree that these features are not diagnostic. Other diagnoses such as paraganglioma, neurofibroma, ganglioneuroma, tumors of mesodermal origin and retroperitoneal malignancies, including malignant fibrous histiocytoma, lymphoma and liposarcoma, should be considered[12,13]. MRI was helpful because it has a better definition, multiplanar capabilities, and the possibility to differentiate the nature of the tumor, such as solid tissue, fibrous tissue, simple or atypical fluid, and blood[14]. It confirmed the presence of a solid, homogeneous mass, and showed its relation to adjacent structures in greater detail[6,15]. No invasive process was revealed and the margins were still regular, convincing us that the mass was benign in nature[16]. Definite diagnosis was made during histopathological examination and immunohistochemistry. Microscopically, the mass showed Antoni A (well-organised spindle cells in a palisade pattern) and B (less cellular, loose pleomorphic cells) areas[1,2], and tested intensely positive for S-100 protein, which is almost exclusively identified within benign nerve sheath tumors[17,18]. CT-guided fine needle aspiration biopsy can be helpful in determining the origin of a mass preoperatively, but is seldom accurate[7]. Since we believed the mass was causing colitis, open surgical excision was performed. Successful laparoscopic removal of retroperitoneal schwannomas has been reported[19], as well as with endoscopic minilaparotomy[20].
Recurrence is rare and probably due to incomplete excision[7,21]. Further investigations were performed to exclude schwannomatosis or NF2. Absence of other schwannomas and lack of family history of schwannoma theoretically excluded both conditions (see diagnostic criteria in Tables 1 and 2). The presence of a germline NF2 mutation was excluded by a thorough genetic analysis. We performed direct sequencing of all coding exons of the NF2 gene. Deletion was excluded by MLPA. This mutation detection strategy, ideally performed on the original tumor specimen, allows the detection of a germline mutation in > 90% of NF2 patients with a family history of the disease, and in > 70% of sporadic cases. However, it is probably only justified in sporadic unilateral vestibular schwannoma in patients aged < 20 years, unless other features of NF2 are present[24].
Table 1.
Diagnostic criteria for NF2[22]
| Definite NF2 | |
| 1 | Bilateral vestibular schwannomas or |
| 2 | Family history of NF2 (first-degree family relative) plus |
| a Unilateral vestibular schwannoma at age < 30 yr, or | |
| b Any two of the following: meningioma, glioma, schwannoma or juvenile posterior subcapsular lenticular opacities/juvenile cortical cataract | |
| Presumptive or probable NF2 | |
| 1 | Unilateral vestibular schwannoma at age < 30 yr plus at least one of the following: meningioma, glioma, schwannoma or juvenile posterior subcapsular lenticular opacities/juvenile cortical cataract |
| 2 | Multiple meningiomas (two or more) plus |
| a Unilateral vestibular schwannoma at age < 30 yr, or | |
| b One of the following: glioma, schwannoma or juvenile posterior subcapsular lenticular opacities/juvenile cortical cataract | |
Table 2.
Diagnostic criteria for schwannomatosis[23]
| Definite schwannomatosis | |
| 1 | Two or more pathologically proved schwannomas, plus |
| 2 | Lack of radiographic evidence of vestibular schwannoma at age > 18 yr |
| Presumptive or probable schwannomatosis | |
| 1 | Two or more pathologically proved schwannomas without symptoms of eighth nerve dysfunction at age > 30 yr or |
| 2 | Two or more pathologically proved schwannomas in an anatomically limited distribution (single limb or segment of the spine), without symptoms of eighth nerve dysfunction, at any age |
In conclusion, benign retroperitoneal schwannomas are rare tumors arising from the neural sheath of peripheral nerves. They are usually incidental findings but may become symptomatic if sufficiently large. Symptoms are usually vague and non-specific and can mimic different diseases. CT and MR findings show characteristic features, but none are specific. Diagnosis is based on histopathological examination and immunohistochemistry. Total excision is therapeutic and has a good prognosis. Genetic testing for NF2 is probably not justified in the presence of a solitary retroperitoneal schwannoma.
Footnotes
S- Editor Liu Y L- Editor Kerr C E- Editor Li JL
References
- 1.Enzinger FM, Weiss SW. Benign tumors of peripheral nerves. In: Enzinger FM, Weiss SW, ediitors , editors. Soft tissue tumors. 3rd ed. St. Louis: Mosby; 1995. pp. 821–888. [Google Scholar]
- 2.Kyriakos ML. Tumors and tumorlike conditions of soft tissues. In: Kissane JM, editor. Anderson's pathology. 8th ed. St. Louis: Mosby; 1985. pp. 1682–1687. [Google Scholar]
- 3.McCarthy S, Duray PH. Giant retroperitoneal neurilemoma: a rare cause of digestive tract symptoms. J Clin Gastroenterol. 1983;5:343–347. [PubMed] [Google Scholar]
- 4.Scanlan DB. Primary retroperitoneal tumors. J Urol. 1959;81:740–745. doi: 10.1016/S0022-5347(17)66103-2. [DOI] [PubMed] [Google Scholar]
- 5.Evans DG, Sainio M, Baser ME. Neurofibromatosis type 2. J Med Genet. 2000;37:897–904. doi: 10.1136/jmg.37.12.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim SH, Choi BI, Han MC, Kim YI. Retroperitoneal neurilemoma: CT and MR findings. AJR Am J Roentgenol. 1992;159:1023–1026. doi: 10.2214/ajr.159.5.1414767. [DOI] [PubMed] [Google Scholar]
- 7.Daneshmand S, Youssefzadeh D, Chamie K, Boswell W, Wu N, Stein JP, Boyd S, Skinner DG. Benign retroperitoneal schwannoma: a case series and review of the literature. Urology. 2003;62:993–997. doi: 10.1016/s0090-4295(03)00792-1. [DOI] [PubMed] [Google Scholar]
- 8.Schindler OS, Dixon JH, Case P. Retroperitoneal giant schwannomas: report on two cases and review of the literature. J Orthop Surg (Hong Kong) 2002;10:77–84. doi: 10.1177/230949900201000114. [DOI] [PubMed] [Google Scholar]
- 9.Singh V, Kapoor R. Atypical presentations of benign retroperitoneal schwannoma: report of three cases with review of literature. Int Urol Nephrol. 2005;37:547–549. doi: 10.1007/s11255-004-4705-5. [DOI] [PubMed] [Google Scholar]
- 10.Hurley L, Smith JJ, Larsen CR, Silverman ML. Multiple retroperitoneal schwannomas: case report and review of the literature. J Urol. 1994;151:413–416. doi: 10.1016/s0022-5347(17)34966-2. [DOI] [PubMed] [Google Scholar]
- 11.Miller PL, Tessler A, Alexander S, Pinck BD. Retroperitoneal neurilemmoma. Urology. 1978;11:619–623. doi: 10.1016/0090-4295(78)90016-x. [DOI] [PubMed] [Google Scholar]
- 12.Kransdorf MJ. Benign soft-tissue tumors in a large referral population: distribution of specific diagnoses by age, sex, and location. AJR Am J Roentgenol. 1995;164:395–402. doi: 10.2214/ajr.164.2.7839977. [DOI] [PubMed] [Google Scholar]
- 13.Hughes MJ, Thomas JM, Fisher C, Moskovic EC. Imaging features of retroperitoneal and pelvic schwannomas. Clin Radiol. 2005;60:886–893. doi: 10.1016/j.crad.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 14.Hayasaka K, Tanaka Y, Soeda S, Huppert P, Claussen CD. MR findings in primary retroperitoneal schwannoma. Acta Radiol. 1999;40:78–82. doi: 10.1080/02841859909174408. [DOI] [PubMed] [Google Scholar]
- 15.Cretella JP, Rafal RB, McCarron JP, Markisz JA. MR imaging in the diagnosis of a retroperitoneal schwannoma. Comput Med Imaging Graph. 1994;18:209–212. doi: 10.1016/0895-6111(94)90031-0. [DOI] [PubMed] [Google Scholar]
- 16.Nakashima J, Ueno M, Nakamura K, Tachibana M, Baba S, Deguchi N, Tazaki H, Murai M. Differential diagnosis of primary benign and malignant retroperitoneal tumors. Int J Urol. 1997;4:441–446. doi: 10.1111/j.1442-2042.1997.tb00282.x. [DOI] [PubMed] [Google Scholar]
- 17.Weiss SW, Langloss JM, Enzinger FM. Value of S-100 protein in the diagnosis of soft tissue tumors with particular reference to benign and malignant Schwann cell tumors. Lab Invest. 1983;49:299–308. [PubMed] [Google Scholar]
- 18.Kawahara E, Oda Y, Ooi A, Katsuda S, Nakanishi I, Umeda S. Expression of glial fibrillary acidic protein (GFAP) in peripheral nerve sheath tumors. A comparative study of immunoreactivity of GFAP, vimentin, S-100 protein, and neurofilament in 38 schwannomas and 18 neurofibromas. Am J Surg Pathol. 1988;12:115–120. doi: 10.1097/00000478-198802000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Ohigashi T, Nonaka S, Nakanoma T, Ueno M, Deguchi N. Laparoscopic treatment of retroperitoneal benign schwannoma. Int J Urol. 1999;6:100–103. doi: 10.1046/j.1442-2042.1999.06222.x. [DOI] [PubMed] [Google Scholar]
- 20.Kageyama Y, Kihara K, Ishizaka K, Okuno T, Kawakami S, Fujii Y, Masuda H, Suzuki M, Hyochi N, Arai G, et al. Endoscope-assisted minilaparotomy (endoscopic minilaparotomy) for retroperitoneal Schwannoma: experience with three cases. Jpn J Clin Oncol. 2002;32:177–180. doi: 10.1093/jjco/hyf038. [DOI] [PubMed] [Google Scholar]
- 21.Carpenter WB, Kernohan JW. Retroperitoneal ganglioneuromas and neurofibromas. A clinicopathological study. Cancer. 1963;16:788–797. doi: 10.1002/1097-0142(196306)16:6<788::aid-cncr2820160615>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 22.Gutmann DH, Aylsworth A, Carey JC, Korf B, Marks J, Pyeritz RE, Rubenstein A, Viskochil D. The diagnostic evaluation and multidisciplinary management of neurofibromatosis 1 and neurofibromatosis 2. JAMA. 1997;278:51–57. [PubMed] [Google Scholar]
- 23.Jacoby LB, Jones D, Davis K, Kronn D, Short MP, Gusella J, MacCollin M. Molecular analysis of the NF2 tumor-suppressor gene in schwannomatosis. Am J Hum Genet. 1997;61:1293–1302. doi: 10.1086/301633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Evans DG, Ramsden RT, Gokhale C, Bowers N, Huson SM, Wallace A. Should NF2 mutation screening be undertaken in patients with an apparently isolated vestibular schwannoma? Clin Genet. 2007;71:354–358. doi: 10.1111/j.1399-0004.2007.00778.x. [DOI] [PubMed] [Google Scholar]