Abstract
The ingestion of a foreign body that penetrates the gastric wall and migrates to the liver, where it causes an abscess is uncommon. A case of an ingested rosemary twig perforating the gastric antrum, then migrating to the liver, complicated by hepatic abscess and Staphylococcus aureus sepsis is reported. A 59-year-old man without a history of foreign body ingestion was admitted to our hospital because of sepsis and epigastralgia, which had progressively worsened. No foreign body was identified at preoperative imaging, but a rosemary twig was discovered during laparotomy. The liver abscess and sepsis were controlled successfully with surgery and antibiotics. This unusual condition should be kept in mind when dealing with cases of hepatic abscess, or even sepsis of unknown origin. Despite the improvement of non-surgical techniques such as percutaneous drainage and interventional endoscopy, surgery still remains important in the treatment of hepatic abscess caused by an ingested foreign body.
Keywords: Foreign Body, Gastrointestinal perforation, Hepatic Abscess, Ingestion, Migration
INTRODUCTION
The first case of hepatic abscess as a result of gastro-intestinal tract (GIT) perforation caused by a foreign body was published by Lambert in 1898[1]. Most foreign bodies pass through the GIT without causing any damage once they pass the lower esophageal sphincter[2]. It is not unusual to come across patients in clinical practice with GIT perforation due to ingested foreign bodies, but the development of a secondary hepatic abscess due to foreign body perforation of the gastric wall is a rare condition[1-4]. In the majority of cases, an early diagnosis is difficult to make because of the non-specific clinical presentation[3].
CASE REPORT
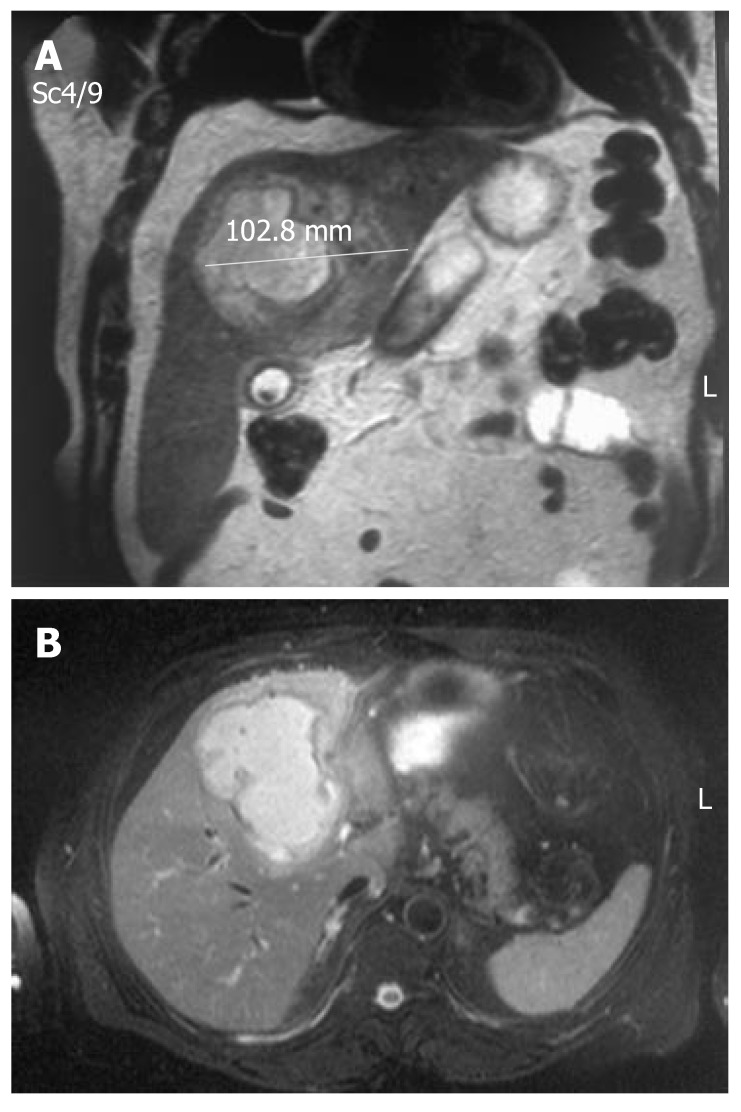
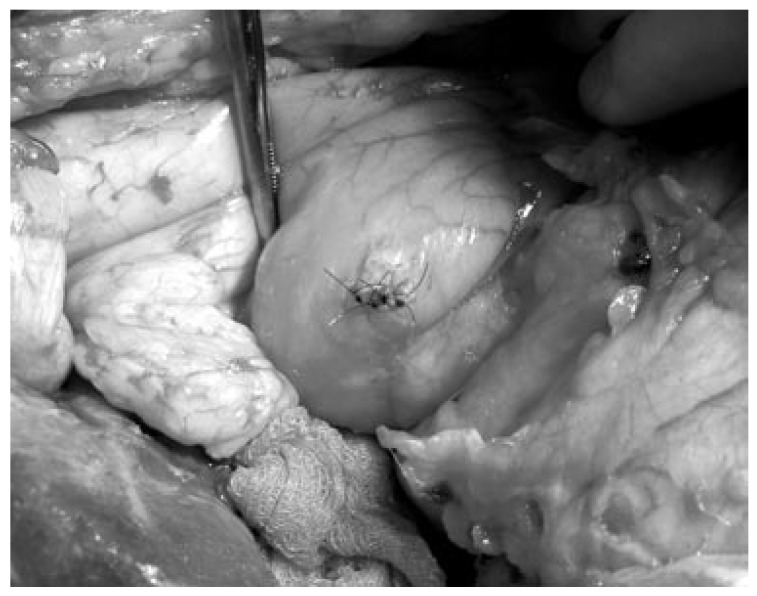
A 59-year-old man presented with epigastric, right upper abdominal pain and intermittent high-grade fever, with chills and rigors for the past 2 mo. There was no history of foreign body ingestion. He had received treatment for his fever of unknown origin at a district hospital in the form of antibiotics (ceftriaxone, 2.0 g daily) and antipyretics. On admission, examination revealed a septic, high-grade febrile patient (38.9°C) with tachycardia (pulse 128 bpm) and tachypnoea (21 breaths/min). The white blood cell count was 28.8 × 109/L, alkaline phosphatase was 180 U/L, bilirubin was normal, and C-reactive protein (CRP) was 320 mg/L. The abdomen was tense with tenderness in the epigastrium and right hypochondrium, without any signs of peritoneal reaction. Chest X-ray revealed a right-sided pleural effusion, but X-ray of the abdomen was normal. Ultrasound (US) examination, contrast-enhanced computerized tomography (CT) (Figure 1) and magnetic resonance imaging (MRI) of the abdomen (Figure 2) revealed a hepatic abscess of 11.7 cm × 10.3 cm × 8.8 cm in the segments S4b-S5. The patient was started on meropenem and subjected to exploratory laparotomy, which revealed a huge abscess occupying the central segments of the liver, and concomitant acute calculous cholecystitis. There was no association between the inflammatory process in the gallbladder and abscess formation. After cholecystectomy, hepatotomy along the gallbladder bed was performed, and about 500 mL of pus was drained and a rosemary twig of 4.5 cm was retrieved from the abscess cavity (Figure 3). Since there was no obvious fistulous communication between the liver and stomach or duodenum, a careful examination of the upper GIT revealed a small covered perforation of the gastric antrum wall. The perforation was repaired by using single-layer interrupted sutures (Figure 4). The abscess was also drained with a triple-tube lavage system. Vancomycin was added postoperatively due to subsequent blood culture that showed Staphylococcus aureus. The patient recovered uneventfully and was discharged on postoperative d 10.
Figure 1.

CT scan of the abdomen demonstrating a liver abscess containing a small amount of gas.
Figure 2.
MRI of the abdomen showing the abscess in liver segments S4b-S5. (A) T2W coronal view; (B) T2W axial view.
Figure 3.
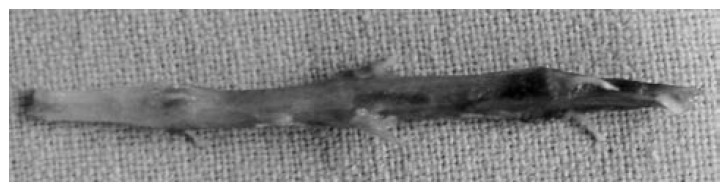
Rosemary twig after retrieval from the hepatic abscess.
Figure 4.
Repair of the perforation site in the gastric antrum.
DISCUSSION
The reported incidence of foreign bodies penetrating the GIT is < 1%[1,2,5], with the objects being pointed or sharp in most cases, such as sewing needles, tooth picks, and chicken and fish bones[5-8], pens, toothbrushes and dental plates[9-11].
The most common sites of perforation of the GIT are the stomach and duodenum[1-3]. Abscess formation occurs more often on the left hemiliver[2,3]. The ingestion of a foreign body that penetrates the GIT wall and migrates to the liver, where it causes an abscess is indeed rare, with 46 cases being reported in the recent literature[3]. No report of hepatic abscess caused by ingestion of a rosemary twig (used for food flavoring), has been found so far in the medical literature.
The classical presenting features of hepatic abscess, such as fever with chills, abdominal pain and discomfort, and jaundice are present in only a small number of patients[1-4]. Most patients have non-specific symptoms such as anorexia, vomiting or weight loss with leucocytosis[6-9], or increased transaminases, bilirubin or alkaline phosphatase[10,11]. The migrating foreign body may remain silent for a long time and may only be discovered if there are features of infection or abscess formation[1]. The presentation of a penetrating foreign body (tooth pick) as a granulomatous liver abscess has been reported 1 mo after ingestion, requiring partial lateral resection of the liver[8]. The prolonged time course of the illness, the lack of history of foreign body ingestion, the relatively non-specific symptoms and signs, and the non-specific results obtained by using conventional radiography have resulted in delayed recognition of this possibly fatal diseas [4]. Deaths caused by missed or delayed diagnosis have been reported, one of which was discovered on autopsy[12-14]. Thus, both a high clinical suspicion index and prompt treatment are necessary for this rare condition[1-3,11-15]. An ingested foreign body may be identified with plain X-rays of the abdomen, if the body is radio-opaque. Other methods of foreign body identification include US, CT, MRI, upper GIT endoscopy, colonoscopy, and laparotomy[8,15-16]. Endoscopy may be helpful when performed early, before the foreign body migration and mucosal healing[3,7].
The recommended treatment is exploratory laparotomy to evacuate the hepatic abscess, remove the foreign body, and repair the perforation site in the GIT[1-3,16]. Since the gastric perforation is small and is probably covered by the omentum or hepatic lobe, minimally invasive treatment such as percutaneous drainage of the pus collection, combined with endoscopic removal of the foreign body, can be employed to reduce open surgery[2,9]. Also, the successful treatment of hepatic abscess and foreign body removal by the percutaneous transhepatic approach has been reported[10].
In conclusion, we report a very rare case of the migration of an ingested rosemary twig into the liver through the stomach, which resulted in hepatic abscess and sepsis. Due to the lack of obvious fistulous communication between the liver and upper GIT, careful exploration of the abscess cavity is of great importance. This condition should be kept in mind when dealing with cases of hepatic abscess, or even sepsis of unknown origin. Therefore, an early diagnosis and prompt intervention are optimal for treatment and necessary to avoid death. Despite the improvement of non-surgical techniques such as percutaneous drainage and interventional endoscopy, surgery still remains important in the treatment of hepatic abscess caused by an ingested foreign body.
Footnotes
S- Editor Zhu LH L- Editor Kerr C E- Editor Liu Y
References
- 1.Chintamani V, Lubhana P, Durkhere R, Bhandari S. Liver abscess secondary to a broken needle migration--a case report. BMC Surg. 2003;3:8. doi: 10.1186/1471-2482-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee KF, Chu W, Wong SW, Lai PB. Hepatic abscess secondary to foreign body perforation of the stomach. Asian J Surg. 2005;28:297–300. doi: 10.1016/S1015-9584(09)60365-1. [DOI] [PubMed] [Google Scholar]
- 3.Santos SA, Alberto SC, Cruz E, Pires E, Figueira T, Coimbra E, Estevez J, Oliveira M, Novais L, Deus JR. Hepatic abscess induced by foreign body: case report and literature review. World J Gastroenterol. 2007;13:1466–1470. doi: 10.3748/wjg.v13.i9.1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Starakis I, Karavias D, Marangos M, Psoni E, Bassaris H. A rooster's revenge: hepatic abscess caused by a chicken bone. Eur J Emerg Med. 2005;12:41–42. doi: 10.1097/00063110-200502000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Theodoropoulou A, Roussomoustakaki M, Michalodimitrakis MN, Kanaki C, Kouroumalis EA. Fatal hepatic abscess caused by a fish bone. Lancet. 2002;359:977. doi: 10.1016/S0140-6736(02)07999-0. [DOI] [PubMed] [Google Scholar]
- 6.Kumar S, Gupta NM. Foreign bodies migrating from gut to liver. Indian J Gastroenterol. 2000;19:42. [PubMed] [Google Scholar]
- 7.Bilimoria KY, Eagan RK, Rex DK. Colonoscopic identification of a foreign body causing an hepatic abscess. J Clin Gastroenterol. 2003;37:82–85. doi: 10.1097/00004836-200307000-00021. [DOI] [PubMed] [Google Scholar]
- 8.Kanazawa S, Ishigaki K, Miyake T, Ishida A, Tabuchi A, Tanemoto K, Tsunoda T. A granulomatous liver abscess which developed after a toothpick penetrated the gastrointestinal tract: report of a case. Surg Today. 2003;33:312–314. doi: 10.1007/s005950300071. [DOI] [PubMed] [Google Scholar]
- 9.Chiang TH, Liu KL, Lee YC, Chiu HM, Lin JT, Wang HP. Sonographic diagnosis of a toothpick traversing the duodenum and penetrating into the liver. J Clin Ultrasound. 2006;34:237–240. doi: 10.1002/jcu.20200. [DOI] [PubMed] [Google Scholar]
- 10.Horii K, Yamazaki O, Matsuyama M, Higaki I, Kawai S, Sakaue Y. Successful treatment of a hepatic abscess that formed secondary to fish bone penetration by percutaneous transhepatic removal of the foreign body: report of a case. Surg Today. 1999;29:922–926. doi: 10.1007/BF02482788. [DOI] [PubMed] [Google Scholar]
- 11.Tsui BC, Mossey J. Occult liver abscess following clinically unsuspected ingestion of foreign bodies. Can J Gastroenterol. 1997;11:445–448. doi: 10.1155/1997/815876. [DOI] [PubMed] [Google Scholar]
- 12.Dugger K, Lebby T, Brus M, Sahgal S, Leikin JB. Hepatic abscess resulting from gastric perforation of a foreign object. Am J Emerg Med. 1990;8:323–325. doi: 10.1016/0735-6757(90)90086-f. [DOI] [PubMed] [Google Scholar]
- 13.de la Vega M, Rivero JC, Ruíz L, Suárez S. A fish bone in the liver. Lancet. 2001;358:982. doi: 10.1016/s0140-6736(01)06106-2. [DOI] [PubMed] [Google Scholar]
- 14.Byard RW, Gilbert JD. Hepatic abscess formation and unexpected death: a delayed complication of occult intraabdominal foreign body. Am J Forensic Med Pathol. 2001;22:88–91. doi: 10.1097/00000433-200103000-00018. [DOI] [PubMed] [Google Scholar]
- 15.Broome CJ, Peck RJ. Hepatic abscess complicating foreign body perforation of the gastric antrum: an ultrasound diagnosis. Clin Radiol. 2000;55:242–243. doi: 10.1053/crad.1999.0339. [DOI] [PubMed] [Google Scholar]
- 16.Drnovsek V, Fontanez-Garcia D, Wakabayashi MN, Plavsic BM. Gastrointestinal case of the day. Pyogenic liver abscess caused by perforation by a swallowed wooden toothpick. Radiographics. 1999;19:820–822. doi: 10.1148/radiographics.19.3.g99ma20820. [DOI] [PubMed] [Google Scholar]