Abstract
Perivascular epithelioid cell tumor (PEComa) is a rare tumor which arises from mesenchymal tissues. It is predominant in the uterus, but very rare in the liver. To the best of our knowledge, less than 5 cases of PEComa of the liver have been reported. Herein we present two pathologically proven cases of PEComa of the liver, retrospectively analyze their clinical and imaging features, and review the literature.
Keywords: Liver; Neoplasm; Tomography, X-ray computed; Magnetic resonance imaging
INTRODUCTION
Perivascular epithelioid cell tumor (PEComa) is a rare tumor which arises from mesenchymal tissues. The uterus is the predominant site, but it is very rare in the liver[1-3]. To the best of our knowledge, less than 5 cases of PEComa of the liver have been reported[2,3]. Herein we present two pathologically proven cases of PEComa of the liver, retrospectively analyze their clinical and imaging features, and review the literature.
CASE REPORT
Case 1
A 56-year-old woman complained of abdominal distention for a week. The laboratory examinations were normal. Ultrasonography found a mass in the superior segment of left lateral lobe of the liver. Non-enhancement CT showed a round isodense mass in the IV segment of the left liver with ill-demarcated margin. There was no evidence of fatty density, calcification and necrosis in the mass. On contrast enhancement CT, a well demarcated mass, sized 5.1 cm × 4.2 cm, was found with significant and heterogeneous enhancement (Figure 1A). It was more strikingly enhanced on portal venous phase than on arterial phase. Focal nodular hyperplasia (FNH) or adenoma of the left liver was considered before operation. After operation, pathological diagnosis was established as PEComa of the left liver (Figure 1B). Neither primary recurrence nor metastasis was found during the 2-year follow-up.
Figure 1.
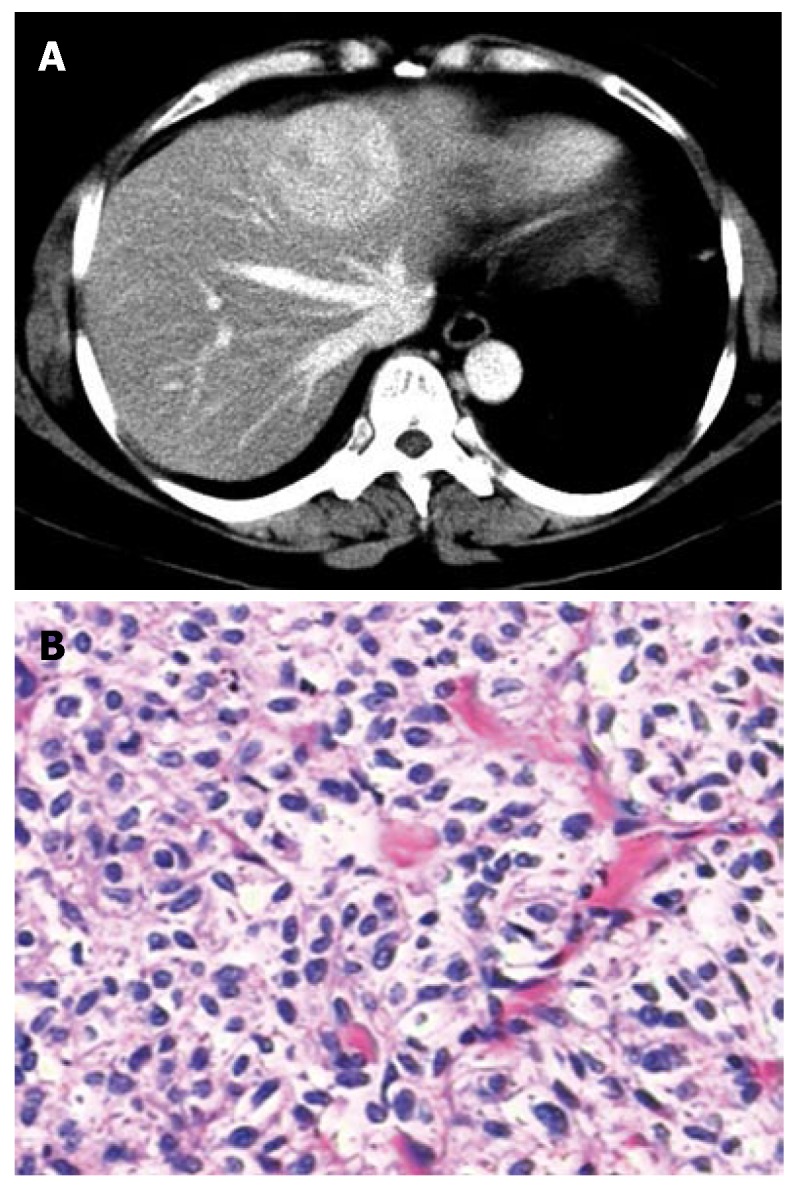
The PEComa of the liver in a 56-year-old woman. A: Contrast-enhanced CT scan shows significant and heterogeneous enhancement of the lesion; B: Photomicrograph shows polygonal or short spindle cells with oval nuclei and clear abundant cytoplasm (HE, × 200).
Case 2
A 63-year-old woman was found to have a mass of liver incidentally in physical examination. Blood, stool and urine routines were normal. Pre-contrast CT scan revealed a lower density mass in the lobus caudatus with a well demarcated margin and homogeneous density. Contrast-enhanced CT showed significantly and heterogeneously patchy enhancement of the lesion on arterial phase (Figure 2A),
Figure 2.
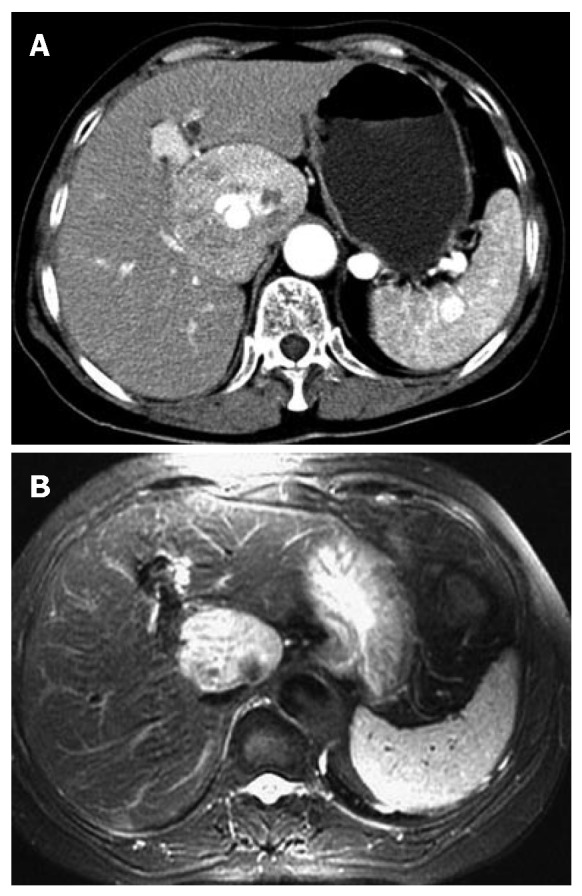
The PEComa in the lobus caudatus of the liver in a 63-year-old woman. A: Contrast-enhanced CT scan demonstrates a tumor in the lobus caudatus; B: Axial T2-weighted (7058/84) MR image shows a hyperintense mass with well-demarcated tumor margins.
being slightly hypodense on delayed CT scan. On T1-weighted images, a round homogeneous hypointense mass in the lobus caudatus was found. On T2-weighted images (Figure 2B), the mass had mildly heterogeneous high-signal intensity with a well-demarcated margin. After contrast enhancement, the mass had striking and homogenous enhancement on arterial phase and venous phase. The diagnosis was FNH or HCC of the liver before operation. The gross appearance of the tumor was a smooth, grey and brown lesion with a capsule. The tumor cells were polygonal with eosinophilic cytoplasm. The final diagnosis was PEComa of the liver. Neither primary recurrence nor metastasis could be found during the 1-year follow-up.
DISCUSSION
The term "PEComa" was introduced by Zamboni et al[4] in 1996. In 2002 and 2003, two monographs published under the auspices of the World Health Organization (WHO) recognized a family of neoplasm with perivascular epithelioid cell differentiation and accepted the designation "PEComa"[5]. In the WHO soft tissue volume, PEComas are defined as "mesenchymal tumors composed of histologically and immunohistochemically distinctive perivascular epithelioid cells (PECs)"[5].
PECs are characterized by perivascular location, often with a radial arrangement of cells around the vascular lumen. Typically, PECs in an immediate perivascular location are most epithelioid and spindle cells resembling smooth muscle are seen away from vessels[5]. The PEC is characterized by positivity with melanocytic markers, such as HMB-45, Melan-A and microphthalmia transcription factor. Desmin is less often positive and cytokeratin and S100 protein are usually absent[5].
PEComas have been reported in the uterus, falciform ligament, gastrointestinal tract, kidney, pancreas, pelvic sidewall, skull, vulva, prostate, thigh, common bile duct and heart. It now appears that PEComas may potentially arise from any anatomic location, but the uterus is the predominant site. Of the 51 cases of PEComa that have been documented in the literature, 46% (21/51) were described in the uterine corpus and 90% developed in females[5]. The PEComas of the liver are extremely rare, and only 5 cases have been reported to date[6].
Clinical presentation of hepatic PEComa has no specificity. It is often found accidentally in physical examinations. But in other organs, the clinical presentation of PEComa might be significant, for example, uterine PEComa may induce uterine bleeding strikingly. Sometimes, a mass can be touched in the PEComa of the lower digestive system and soft tissues.
It is very difficult to make correct diagnosis of PEComa of the liver preoperatively. It is often misdiagnosed as hepatocellular carcinoma, hemangioma, FNH, adenoma and angiomyolipoma. Imaging modalities may be useful because they can help to differentiate PEComa from hepatocellular carcinoma. But the final diagnosis can only be made by pathology.
Clear criteria for malignancy in PEComas have not been elaborated, due to their rarity[5], but there have been a few reports about the tumor metastases[6,7]. On the basis of prior reports, it appears that PEComas displaying any combination of infiltrative growth, marked hypercellularity, nuclear enlargement and hyperchromasia, high mitotic activity, atypical mitotic figures, and coagulative necrosis should be regarded as malignant[5,8]. Malignant PEComas are aggressive sarcomas that frequently result in the death of affected patients, therefore, a close and long-term clinical follow-up is suggested.
Footnotes
S- Editor Zhu LH L- Editor Ma JY E- Editor Liu Y
References
- 1.Fang S, Dong D, Jin M. Perivascular epithelioid cell tumor (PEComa) of the kidney: MR features. Eur Radiol. 2007;17:1906–1907. doi: 10.1007/s00330-006-0443-7. [DOI] [PubMed] [Google Scholar]
- 2.Rouquie D, Eggenspieler P, Algayres JP, Béchade D, Camparo P, Baranger B. Malignant-like angiomyolipoma of the liver: report of one case and review of the literature. Ann Chir. 2006;131:338–341. doi: 10.1016/j.anchir.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 3.Yamamoto H, Oda Y, Yao T, Oiwa T, Kobayashi C, Tamiya S, Kawaguchi K, Hino O, Tsuneyoshi M. Malignant perivascular epithelioid cell tumor of the colon: report of a case with molecular analysis. Pathol Int. 2006;56:46–50. doi: 10.1111/j.1440-1827.2006.01917.x. [DOI] [PubMed] [Google Scholar]
- 4.Zamboni G, Pea M, Martignoni G, Zancanaro C, Faccioli G, Gilioli E, Pederzoli P, Bonetti F. Clear cell "sugar" tumor of the pancreas. A novel member of the family of lesions characterized by the presence of perivascular epithelioid cells. Am J Surg Pathol. 1996;20:722–730. doi: 10.1097/00000478-199606000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Folpe AL. Neoplasms with perivascular epithelioid differentiation (PEComas) In: Fletcher CDM, Unni KK, Mertens F, editors. Pathology and genetics of tumours of soft tissue and bone. Lyon: IARC Press; 2002. pp. 221–222. [Google Scholar]
- 6.Rigby H, Yu W, Schmidt MH, Fernandez CV. Lack of response of a metastatic renal perivascular epithelial cell tumor (PEComa) to successive courses of DTIC based-therapy and imatinib mesylate. Pediatr Blood Cancer. 2005;45:202–206. doi: 10.1002/pbc.20305. [DOI] [PubMed] [Google Scholar]
- 7.Harris GC, McCulloch TA, Perks G, Fisher C. Malignant perivascular epithelioid cell tumour ("PEComa") of soft tissue: a unique case. Am J Surg Pathol. 2004;28:1655–1658. doi: 10.1097/00000478-200412000-00017. [DOI] [PubMed] [Google Scholar]
- 8.Fadare O, Parkash V, Yilmaz Y, Mariappan MR, Ma L, Hileeto D, Qumsiyeh MB, Hui P. Perivascular epithelioid cell tumor (PEComa) of the uterine cervix associated with intraabdominal "PEComatosis": A clinicopathological study with comparative genomic hybridization analysis. World J Surg Oncol. 2004;2:35. doi: 10.1186/1477-7819-2-35. [DOI] [PMC free article] [PubMed] [Google Scholar]


