Abstract
AIM: To study the value of biochemical and ultraso-nographic parameters in prediction of presence and size of esophageal varices.
METHODS: The study includes selected cirrhotic patients who underwent a complete biochemical workup, upper digestive endoscopic and ultrasonographic examinations. Albumin/right liver lobe diameter and platelet count/spleen diameter ratios were calculated. The correlation between calculated ratio and the presence and degree of esophageal varices was evaluated.
RESULTS: Ninety-four subjects (62 males, 32 females), with a mean age of 52.32 ± 13.60 years, were studied. Child-Pugh class A accounted for 42.6%, class B 37.2%, whereas class C 20.2%. Esophageal varices (OE) were not demonstrated by upper digestive endoscopy in 24.5%, while OE gradeIwas found in 22.3% patients, grade II in 33.0%, grade III in 16.0%, and grade IV in 4.3%. The mean value of right liver lobe diameter/albumin ratio was 5.51 ± 1.82 (range from 2.76 to 11.44), while the mean platelet count/spleen diameter ratio was 1017.75 ± 729.36 (range from 117.39 to 3362.50), respectively. Statistically significant correlation was proved by Spearman's test between OE grade and calculated ratios. The P values were 0.481 and -0.686, respectively.
CONCLUSION: The right liver lobe diameter/albumin and platelet count/spleen diameter ratios are non-invasive parameters providing accurate information pertinent to determination of presence of esophageal varices, and their grading in patients with liver cirrhosis.
Keywords: Liver cirrhosis, Esophageal varices, Portal hypertension, Ultrasonography
INTRODUCTION
Esophageal varices development is among the major complications of liver cirrhosis, with an estimated prevalence of approximately 50%. The risk of bleeding from varices is 25%-35% with majority of the initial bleeding occurring within 1 year from varices detection[1]. The mortality from each episode of variceal bleeding is 17%-57%[2-4]. Bleeding episodes can be predicted by the presence of red signs ("red cherry spots") on the varices, and by the variceal size[5,6]. The incidence of bleeding can be reduced with nonselective beta-blockers[7,8]. It is also suggested that prophylactic endoscopic variceal ligation can decrease the incidence of first variceal bleeding and mortality in patients with liver cirrhosis who have large varices[9,10]. Therefore, annual endoscopic screening is highly recommended for patients with small esophageal varices while the procedure should be conducted once every two years for patients suffering from liver cirrhosis without diagnosed varices[11,12]. Nevertheless, repeated endoscopic examinations are unpleasant for patients, and have cost impact on health care insurance, while only half of cirrhotic patients have esophageal varices, and up to 30% have large varices. Therefore, the sensitivity and specificity of numerous non-invasive parameters have been investigated for assessment of presence and size of esophageal varices, and risk prediction for bleeding.
We aim to identify non-invasive parameters based on ultrasonographic measurement and laboratory test that have a potential in assessment of presence and size of esophageal varices in patients with liver cirrhosis.
MATERIALS AND METHODS
This study includes 94 patients treated for liver cirrhosis in Clinic for Gastroenterology and Hepatology, Clinical Centre of Serbia in 2006. The diagnosis of cirrhosis was based on clinical features, laboratory test, imaging diagnostics, and liver histology whenever possible.
The following information was collected for each patient: age, gender, etiology of cirrhosis, biochemical parameters (aspartate aminotransferase, alanine aminotransferase, total bilirubin, serum albumin, prothrombin activity, and platelet count), presence and degree of esophageal varices and degree of liver function impairment by Child-Pugh classes. Cirrhosis etiology was determined as viral if hepatitis B surface antigen or hepatitis C serum markers were positive. If viral markers were negative, and the history obtained indicated alcohol consumption of at least 50 g per day in the past five years, liver cirrhosis was considered as alcoholic. Positive immunological markers were characteristic for immunological liver disease. The other studied cases had liver cirrhosis of different etiology (Wilson's disease, α1 antitrypsin deficiency, hemochromatosis, etc.).
All studied subjects underwent ultrasonographic examination of the upper abdomen. The right lobe diameter in the medioclavicular line, as well as the spleen bipolar diameter were measured for three times and the mean value was recorded. One investigator performed all measurements (TA) in order to reduce the inter- and intra-observer errors in assessing the diameters.
Using the laboratory and ultrasonographic values, we calculated two ratios: right lobe diameter/serum albumin concentration and platelet count/spleen diameter.
An experienced endoscopist (SD) who used the gradeI-IV classification[13] did the endoscopies. Varices in the level of mucosa were recognized as grade I, those smaller than 5 mm fulfilling less than 1/3 of the esophageal lumen were recognized as grade II, grade III were varices larger than 5 mm fulfilling more than 1/3 of the esophageal, while grade IV varices occupied more than 2/3 of esophageal lumen. Patients with previous variceal bleeding, porto-systemic shunts and those taking beta-blockers medications and patients with coexistent illness or infection that could influence the liver and spleen size, were excluded.
Child-Pugh score was calculated using five variables (ascites, encephalopathy, bilirubin, albumin, and prothrombin time). Values 1, 2 or 3 were assigned to each of these variables due to increasing abnormality, and the score calculated as sum of the five variables for each patient. A Child-Pugh score less than 7 was considered as class A, from 7 to 9 as class B, while any score greater than 9 was as class C[14]. Laboratory test and ultrasonographic and endoscopic examinations were performed within one week.
The Ethic Committee of our institution approved the study and all patients gave an informed consent prior to inclusion into this investigation.
All collected data were analyzed and correlated. Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS, version 10.0). Basic descriptive statistics included means, standard deviations, ranges and percentages. For correlation analysis, we used Spearman's test. Differences were considered statistically significant if the two-tailed P value was less than 0.05. Sensitivity and specificity, as well as the best cut-off value for the diagnosis of varices were calculated using ROC curves.
RESULTS
Clinical characteristics of the patients are presented in Table 1.
Table 1.
Clinical characteristics of patients
| Sex (M/F) | 62/32 |
| Age (yr; mean ± SD) | 52.32 ± 13.60 |
| Age range (yr) | 17-79 |
| Aetiology of liver disease (alcoholic/infective/autoimmune/other) | 43/19/17/15 |
| Child-Pugh class (A/B/C) | 40/35/19 |
| Mean size of the right liver lobe (mean ± SD) | 157.71 ± 23.37 |
| Mean size of the spleen (mean ± SD) | 148.05 ± 33.73 |
| Mean albumin concentration (g/L; mean ± SD) | 30.79 ± 7.97 |
| Mean thrombocyte number (mean ± SD) | 134 632.98 ± 75937.83 |
| Oesophageal varices grade (0/I/II/III/IV) | 23/21/31/15/4 |
The mean value of the ratio of the platelet count/spleen size was 1017.75 ± 729.36 (range 117.39-3362.50). The mean value of the ratio of the right liver lobe size/serum albumin concentration was 5.51 ± 1.82 (range 2.76-11.44).
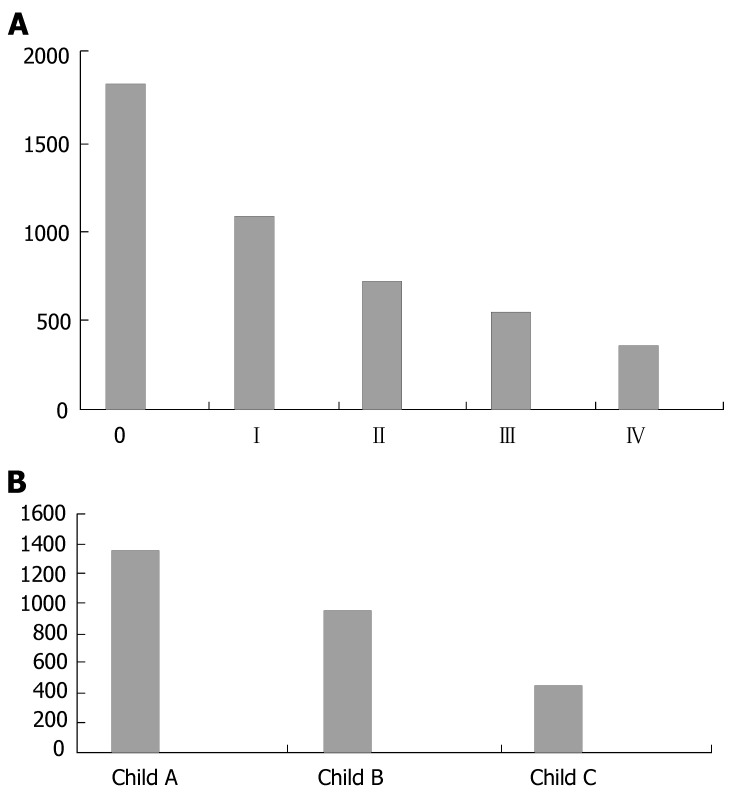
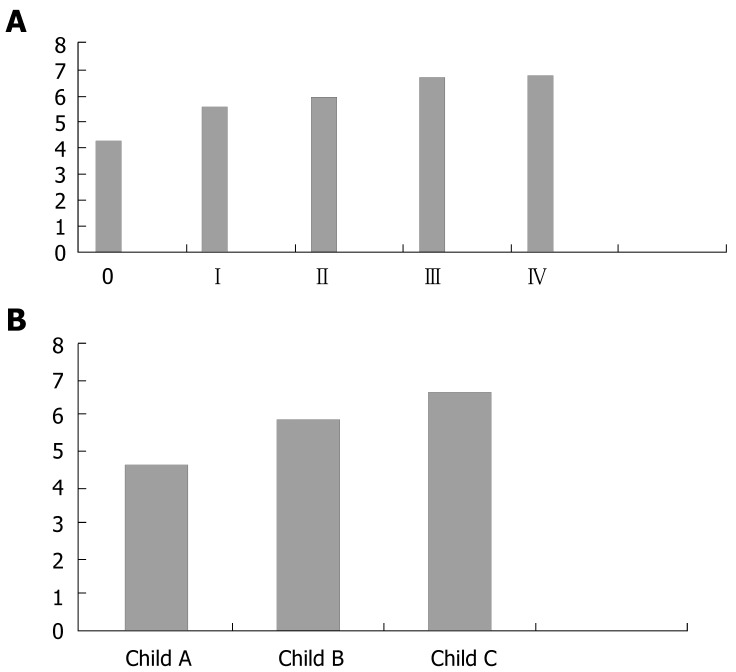
These ratios were correlated with the presence and size of esophageal varices (Table 2, Figure 1A and B). Spearman's test for nonparametric correlation showed that, the platelet count/spleen size ratio significantly correlated with the presence (P = 0.585, P < 0.01) and size (P = 0.686, P < 0.01) of esophageal varices, so does the right liver lobe/serum albumin concentration ratio (P = 0.488, P < 0.01 and P = 0.481, P < 0.01 respectively). We also studied the correlation with Child-Pugh score of liver function impairment (Table 3, Figure 2A and B). These ratios had a highly significant correlation (P < 0.01) with Child Pugh score. For the platelet count/spleen size ratio, P = -0.585, while for the right liver lobe/serum albumin concentration ratio, P = 0.491.
Table 2.
Calculated ratios and varice size
| Varices |
Right lobe/albumin ratio |
Platelet count/spleen ratio |
||
| mean ± SD | Range | mean ± SD | Range | |
| Grade 0 | 4.19 ± 1.36 | 2.76-8.19 | 1822.53 ± 804.06 | 608.70-3362.50 |
| GradeI | 5.43 ± 1.58 | 3.25-9.44 | 1072.86 ± 493.49 | 366.67-2021.05 |
| Grade II | 5.84 ± 1.25 | 3.40-8.48 | 696.46 ± 439.43 | 150.00-2283.33 |
| Grade III | 6.57 ± 2.42 | 4.07-10.00 | 549.14 ± 289.90 | 127.27-1275.00 |
| Grade IV | 6.68 ± 2.52 | 4.07-11.44 | 348.19 ± 231.86 | 117.39-633.33 |
Figure 1.
A: Platelet count/spleen ratio in correlation to varice size; B: Platelet count/spleen ratio in correlation to Child-Pugh score.
Table 3.
Calculated ratios and Child score for hepatic insufficiency
| Child- Pugh score |
Right lobe/albumin ratio |
Platelet count/spleen ratio |
||
| mean ± SD | Range | mean ± SD | Range | |
| A | 4.59 ± 1.38 | 2.76-8.19 | 1355.34 ± 796.62 | 365.52-3362.50 |
| B | 5.92 ± 1.60 | 3.25-9.44 | 946.67 ± 612.48 | 127.27-2975.00 |
| C | 6.68 ± 2.12 | 4.07-11.44 | 437.97 ± 215.99 | 117.39-900.00 |
Figure 2.
A: Right lobe/albumin ratio in correlation to varice size; B: Right lobe/albumin ratio in correlation to Child-Pugh score.
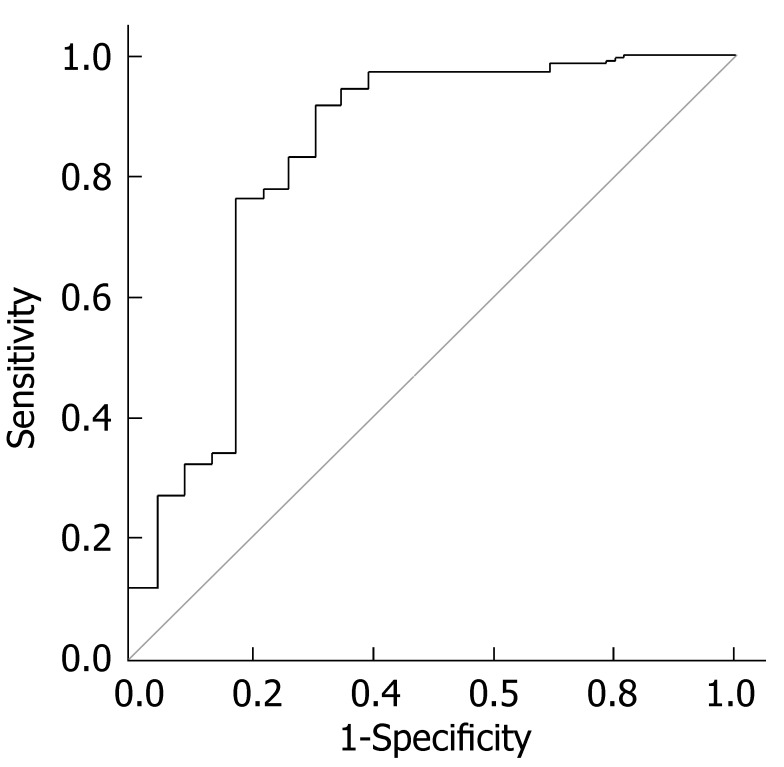
We counted the best cut-off value of the right liver lobe/serum albumin concentration ratio for diagnosis of varices. For the value of 4.425, the sensitivity was 83.1% and the specificity was 73.9% (Figure 3).
Figure 3.
ROC curve for diagnosis of esophageal varices using right lobe/albumin ratio.
DISCUSSION
Incidence of esophageal varices in patients with liver cirrhosis is approximately 90%, but only 9%-35% have been described[15-17]. Variceal bleeding in cirrhotic patients is associated mainly with fatal outcome. Portal hypertension is an essential element of survival in cirrhotic patients[3]. Therefore, regular control and evaluation of esophageal varices with timely introduction of nonselective beta-blockers and variceal ligation play an important role in prevention of bleeding. Endoscopy is an invasive and costly diagnostic procedure. Therefore, introduction of non-invasive parameters for assessment of presence and size of esophageal varices is a major goal of numerous studies.
Platelet count and spleen size were the most frequently explored non-invasive parameters in recent studies. Zaman[15] reported that patients with platelet counts of less than 88000/mm3 have five times greater likelihood of having large esophageal or gastric varices as compared with the patients with higher platelet counts. Ng[16] identified correlation between presence of ascites, thrombocytopenia, hyperbilirubinemia and larger varices in the Chinese population. Similarly, Chalasani[11] concluded that large esophageal varices are predictable in thrombocytopenic patients who have enlarged spleen, while platelet count of less than 88000/mm3 indicates a higher risk for esophageal bleeding. The same study also demonstrated that endoscopy is incrementally cost-effective. Madthora reported that platelet count less than 68000/mm3 have a larger discriminatory value[12].
Splenomegaly and hypersplenism are prevalent in patients with liver cirrhosis and portal hypertension[11]. Thrombocytopenia is a common and highly specific manifestation of hypersplenism, but with low sensitivity for presence of portal hypertension[18]. It is suggested that the main mechanism of thrombocytopenia is splenic sequestration and pooling[19], and other mechanisms are also involved. Madthora and co-authors reported that 32% of patients had platelet count less than 68000/mm3 without detectable splenomegaly, which might be explained by insufficient synthesis of thrombopoietin. It is also indicated that platelet count and thrombopoietin level are returning to referent values following liver transplantation[20]. Other potential explanations for this phenomenon are presence of antithrombotic antibodies and thrombocyte associated immunoglobulin, which can be found in the sera of patients with liver diseases[21].
Some investigators reported that the use of non-invasive indicators is invalid for avoiding the endoscopic screening in patients with primary biliary cirrhosis and sclerosing cholangitis. The probability of esophageal varices presence is lower in these patients if they have platelet count less than 200000/mm3, possibly due to the fact that thrombopoietin production is preserved in primary biliary cirrhosis and sclerosing cholangitis[22].
It is well documented that the spleen size is correlated with severity of esophageal varices[23-25]. Watanabe[25] calculated the splenic ratio (length × width × height of the spleen size on computed tomography) and showed that patients having a ratio greater than 963 cm3 have esophageal varices, and that a high ratio may predict esophageal bleeding in patients with liver cirrhosis. It is concluded that ultrasonographic measurement of splenic cranio-caudal diameter results in lower inter- and intra-observer variability unlike Doppler sonographic assessment of hepatic flow[26,27]. The value of Doppler sonographic assessment of portal hypertension is controversial. It is indicated that congestive ratio (counted from the cross section area and mean velocity of portal flow)[26,28,29], as well as resistance ratio of the hepatic artery[30] and splenic artery[24] are correlated with portal hypertension. Portal hemodynamic parameters (mean and maximum portal vein velocity) seam to be weak in assessment of portal hypertension[31]. In addition, it is important to keep in mind that performing Doppler sonographic examination requires sophisticated skills and equipment.
The pathophysiologic mechanisms are combined based on the integration of two non-invasive parameters, i.e., platelet count and spleen size into one ratio. Calculation of this ratio is very easy for routine clinical practice. Gianinni and co-authors[32,33] reported the results of a retrospective and prospective study and concluded that this ratio is sensitive for prediction of presence and size of esophageal varices. The same study group suggests as especially important, the use of non-invasive parameters in the diagnostic algorithm for identifying patients without esophageal varices. A cut-off value of 909 has been proposed for platelet count/spleen size ratio[34]. Patient having the ratio greater than cut-off value should not receive nonselective beta-blockers prophylactic therapy because they are less likely to develop esophageal varices. These patients should less frequently undergo endoscopy.
Taking into account the results of previous studies in the field, we also combined laboratory and ultrasonographic parameters and counted an original ratio. For the first time we reported the value of the right liver lobe/serum albumin concentration in assessment of portal hypertension[35]. We used serum albumin concentration as a parameter of liver function in combination with right liver lobe size.
Previously published studies reported that platelet count/spleen size ratios are good predictors of esophageal varices. Despite a good correlation between these ratios and esophageal varices grade, it is unlikely that these ratios could be used to exclude patients from initial endoscopic screening. Nevertheless, these ratios may serve for selection of patients who need more frequent endoscopies. These ratios will help identify patients at higher risks for development of esophageal varices. It will provide insight into the relationship between clinical, biochemical, hematological and imaging abnormalities and development of clinically significant esophageal varices. The right liver lobe diameter/albumin, as well as platelet count/spleen diameter ratios are non-invasive parameters that can provide accurate information pertinent to determination of the presence and grade of esophageal varices in patients with liver cirrhosis. Further validation of the results will be achieved through long-term follow-up of the patients and a larger number of studied subjects.
COMMENTS
Background
Esophageal varices are frequent in patients with liver cirrhosis. There is an increasing mortality rate of cirrhotic patients due to high risk of bleeding. The correlation of varices size and risk of bleeding is well-known, yet non-invasive techniques for variceal size estimation have not been intensively studied.
Research frontiers
Valuable laboratory tests and clinical examination may help predict the risk of esophageal varices bleeding. This study shows that excellent correlation exists between platelet count/spleen size and size of esophageal varices, so does the right liver lobe/serum albumin concentration ratio. In addition, the authors suggest that the use of non-invasive and less expensive methods may be of benefit for patients and consumers.
Innovations and breakthroughs
Accumulated literature shows that it is necessary to investigate non-invasive parameters in liver cirrhosis for prediction of the size of esophageal varices. Development of these methods may decrease the exposure of cirrhotic patients to repeated endoscopic procedures.
Applications
Thet can be used for non-invasive estimation of esophageal varice size in cirrhotic patients.
Peer review
The manuscript reports the results from an investigation of non-invasive parameters in estimation of variceal size and risk for bleeding. The authors conclude that combination of laboratory and ultrasonographic parameters such as right liver lobe/serum albumin concentration may be useful in assessment of portal hypertension. The appropriate figures and tables are supporting the results.
Footnotes
S- Editor Liu Y L- Editor Ma JY E- Editor Yin DH
References
- 1.Prediction of the first variceal hemorrhage in patients with cirrhosis of the liver and esophageal varices. A prospective multicenter study. N Engl J Med. 1988;319:983–989. doi: 10.1056/NEJM198810133191505. [DOI] [PubMed] [Google Scholar]
- 2.Graham DY, Smith JL. The course of patients after variceal hemorrhage. Gastroenterology. 1981;80:800–809. [PubMed] [Google Scholar]
- 3.D'Amico G, Luca A. Natural history. Clinical-haemodynamic correlations. Prediction of the risk of bleeding. Baillieres Clin Gastroenterol. 1997;11:243–256. doi: 10.1016/s0950-3528(97)90038-5. [DOI] [PubMed] [Google Scholar]
- 4.Jensen DM. Endoscopic screening for varices in cirrhosis: findings, implications, and outcomes. Gastroenterology. 2002;122:1620–1630. doi: 10.1053/gast.2002.33419. [DOI] [PubMed] [Google Scholar]
- 5.Bhasin DK, Malhi NJ. Variceal bleeding and portal hypertension: much to learn, much to explore. Endoscopy. 2002;34:119–128. doi: 10.1055/s-2002-19845. [DOI] [PubMed] [Google Scholar]
- 6.Merkel C, Zoli M, Siringo S, van Buuren H, Magalotti D, Angeli P, Sacerdoti D, Bolondi L, Gatta A. Prognostic indicators of risk for first variceal bleeding in cirrhosis: a multicenter study in 711 patients to validate and improve the North Italian Endoscopic Club (NIEC) index. Am J Gastroenterol. 2000;95:2915–2920. doi: 10.1111/j.1572-0241.2000.03204.x. [DOI] [PubMed] [Google Scholar]
- 7.D'Amico G, Pagliaro L, Bosch J. The treatment of portal hypertension: a meta-analytic review. Hepatology. 1995;22:332–354. doi: 10.1002/hep.1840220145. [DOI] [PubMed] [Google Scholar]
- 8.Tripathi D, Hayes PC. Review article: a drug therapy for the prevention of variceal haemorrhage. Aliment Pharmacol Ther. 2001;15:291–310. doi: 10.1046/j.1365-2036.2001.00920.x. [DOI] [PubMed] [Google Scholar]
- 9.Khuroo MS, Khuroo NS, Farahat KL, Khuroo YS, Sofi AA, Dahab ST. Meta-analysis: endoscopic variceal ligation for primary prophylaxis of oesophageal variceal bleeding. Aliment Pharmacol Ther. 2005;21:347–361. doi: 10.1111/j.1365-2036.2005.02346.x. [DOI] [PubMed] [Google Scholar]
- 10.Psilopoulos D, Galanis P, Goulas S, Papanikolaou IS, Elefsiniotis I, Liatsos C, Sparos L, Mavrogiannis C. Endoscopic variceal ligation vs. propranolol for prevention of first variceal bleeding: a randomized controlled trial. Eur J Gastroenterol Hepatol. 2005;17:1111–1117. doi: 10.1097/00042737-200510000-00016. [DOI] [PubMed] [Google Scholar]
- 11.Chalasani N, Imperiale TF, Ismail A, Sood G, Carey M, Wilcox CM, Madichetty H, Kwo PY, Boyer TD. Predictors of large esophageal varices in patients with cirrhosis. Am J Gastroenterol. 1999;94:3285–3291. doi: 10.1111/j.1572-0241.1999.1539_a.x. [DOI] [PubMed] [Google Scholar]
- 12.Madhotra R, Mulcahy HE, Willner I, Reuben A. Prediction of esophageal varices in patients with cirrhosis. J Clin Gastroenterol. 2002;34:81–85. doi: 10.1097/00004836-200201000-00016. [DOI] [PubMed] [Google Scholar]
- 13.Wehrmann T. Öseophagus Diagnostisch und therapeutisch. In: Lembcke B, Wehrmann T, editors. Die gastroenterologische Endoskopie. Reinbeck: Einhorn-Presse Verlag; 1999. pp. 56–83. [Google Scholar]
- 14.Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646–649. doi: 10.1002/bjs.1800600817. [DOI] [PubMed] [Google Scholar]
- 15.Zaman A, Hapke R, Flora K, Rosen HR, Benner K. Factors predicting the presence of esophageal or gastric varices in patients with advanced liver disease. Am J Gastroenterol. 1999;94:3292–3296. doi: 10.1111/j.1572-0241.1999.01540.x. [DOI] [PubMed] [Google Scholar]
- 16.Ng FH, Wong SY, Loo CK, Lam KM, Lai CW, Cheng CS. Prediction of oesophagogastric varices in patients with liver cirrhosis. J Gastroenterol Hepatol. 1999;14:785–790. doi: 10.1046/j.1440-1746.1999.01949.x. [DOI] [PubMed] [Google Scholar]
- 17.Pagliaro L, D'Amico G, Pasta F. Portal hypertension in cirrhosis: natural history. In: Bosch J, Groszmann RJ, editors. Portal hypertension: pathophysiology and treatment. London: Blackwell Scientific; 1994. pp. 72–92. [Google Scholar]
- 18.Thomopoulos KC, Labropoulou-Karatza C, Mimidis KP, Katsakoulis EC, Iconomou G, Nikolopoulou VN. Non-invasive predictors of the presence of large oesophageal varices in patients with cirrhosis. Dig Liver Dis. 2003;35:473–478. doi: 10.1016/s1590-8658(03)00219-6. [DOI] [PubMed] [Google Scholar]
- 19.Mc Cormick PA. The spleen, hypersplenism, and other relationships between the liver and spleen. In: Bircher J, Benhamou J-P, McIntyre N, Rizzetto M, Rodés J, et al., editors. Oxford textbook of clinical hepatology. Oxford: Oxford University Press; 1999. pp. 787–795. [Google Scholar]
- 20.Goulis J, Chau TN, Jordan S, Mehta AB, Watkinson A, Rolles K, Burroughs AK. Thrombopoietin concentrations are low in patients with cirrhosis and thrombocytopenia and are restored after orthotopic liver transplantation. Gut. 1999;44:754–758. doi: 10.1136/gut.44.5.754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Winkfield B, Aubé C, Burtin P, Calès P. Inter-observer and intra-observer variability in hepatology. Eur J Gastroenterol Hepatol. 2003;15:959–966. doi: 10.1097/00042737-200309000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Bressler B, Pinto R, El-Ashry D, Heathcote EJ. Which patients with primary biliary cirrhosis or primary sclerosing cholangitis should undergo endoscopic screening for oesophageal varices detection? Gut. 2005;54:407–410. doi: 10.1136/gut.2004.040832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pilette C, Oberti F, Aubé C, Rousselet MC, Bedossa P, Gallois Y, Rifflet H, Calès P. Non-invasive diagnosis of esophageal varices in chronic liver diseases. J Hepatol. 1999;31:867–873. doi: 10.1016/s0168-8278(99)80288-8. [DOI] [PubMed] [Google Scholar]
- 24.Piscaglia F, Donati G, Cecilioni L, Celli N, Stagni B, Pini P, Gaiani S, Gherlinzoni F, Bolondi L. Influence of the spleen on portal haemodynamics: a non-invasive study with Doppler ultrasound in chronic liver disease and haematological disorders. Scand J Gastroenterol. 2002;37:1220–1227. doi: 10.1080/003655202760373452. [DOI] [PubMed] [Google Scholar]
- 25.Watanabe S, Hosomi N, Kitade Y, Kurokohchi K, Arima K, Kawabata H, Uchida Y, Nishioka M. Assessment of the presence and severity of esophagogastric varices by splenic index in patients with liver cirrhosis. J Comput Assist Tomogr. 2000;24:788–794. doi: 10.1097/00004728-200009000-00022. [DOI] [PubMed] [Google Scholar]
- 26.Aubé C, Winkfield B, Oberti F, Vuillemin E, Rousselet MC, Caron C, Calès P. New Doppler ultrasound signs improve the non-invasive diagnosis of cirrhosis or severe liver fibrosis. Eur J Gastroenterol Hepatol. 2004;16:743–751. doi: 10.1097/01.meg.0000108357.41221.e5. [DOI] [PubMed] [Google Scholar]
- 27.O'Donohue J, Ng C, Catnach S, Farrant P, Williams R. Diagnostic value of Doppler assessment of the hepatic and portal vessels and ultrasound of the spleen in liver disease. Eur J Gastroenterol Hepatol. 2004;16:147–155. doi: 10.1097/00042737-200402000-00005. [DOI] [PubMed] [Google Scholar]
- 28.Bolondi L, Li Bassi S, Gaiani S, Barbara L. Doppler flowmetry in portal hypertension. J Gastroenterol Hepatol. 1990;5:459–467. doi: 10.1111/j.1440-1746.1990.tb01425.x. [DOI] [PubMed] [Google Scholar]
- 29.Martins RD, Szejnfeld J, Lima FG, Ferrari AP. Endoscopic, ultrasonographic, and US-Doppler parameters as indicators of variceal bleeding in patients with schistosomiasis. Dig Dis Sci. 2000;45:1013–1018. doi: 10.1023/a:1005501930808. [DOI] [PubMed] [Google Scholar]
- 30.Schneider AW, Kalk JF, Klein CP. Hepatic arterial pulsatility index in cirrhosis: correlation with portal pressure. J Hepatol. 1999;30:876–881. doi: 10.1016/s0168-8278(99)80142-1. [DOI] [PubMed] [Google Scholar]
- 31.Schepis F, Cammà C, Niceforo D, Magnano A, Pallio S, Cinquegrani M, D'amico G, Pasta L, Craxì A, Saitta A, et al. Which patients with cirrhosis should undergo endoscopic screening for esophageal varices detection? Hepatology. 2001;33:333–338. doi: 10.1053/jhep.2001.21410. [DOI] [PubMed] [Google Scholar]
- 32.Giannini E, Botta F, Borro P, Risso D, Romagnoli P, Fasoli A, Mele MR, Testa E, Mansi C, Savarino V, et al. Platelet count/spleen diameter ratio: proposal and validation of a non-invasive parameter to predict the presence of oesophageal varices in patients with liver cirrhosis. Gut. 2003;52:1200–1205. doi: 10.1136/gut.52.8.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Giannini EG, Botta F, Borro P, Dulbecco P, Testa E, Mansi C, Savarino V, Testa R. Application of the platelet count/spleen diameter ratio to rule out the presence of oesophageal varices in patients with cirrhosis: a validation study based on follow-up. Dig Liver Dis. 2005;37:779–785. doi: 10.1016/j.dld.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 34.Giannini EG, Zaman A, Kreil A, Floreani A, Dulbecco P, Testa E, Sohaey R, Verhey P, Peck-Radosavljevic M, Mansi C, et al. Platelet count/spleen diameter ratio for the noninvasive diagnosis of esophageal varices: results of a multicenter, prospective, validation study. Am J Gastroenterol. 2006;101:2511–2519. doi: 10.1111/j.1572-0241.2006.00874.x. [DOI] [PubMed] [Google Scholar]
- 35.Alempijevic T, Kovacevic N. Right liver lobe diameter: albumin ratio: a new non-invasive parameter for prediction of oesophageal varices in patients with liver cirrhosis (preliminary report) Gut. 2007;56:1166–1167; author reply 1167. [PMC free article] [PubMed] [Google Scholar]