Abstract
Endoscopic biliary stent insertion is a well-established procedure. It is especially successful in treating postoperative biliary leaks, and may prevent surgical intervention. A routine change of endoprostheses after 3 mo is a common practice but this can be prolonged to 6 mo. We reported a colonic perforation due to biliary stent dislocation and migration to the rectosigmoid colon, and reviewed the literature.
Keywords: Biliary endoprostheses, Migrated biliary stent, Colonic perforation, Biliary stent complications
INTRODUCTION
Endoscopic biliary stent insertion is a well-established treatment for hepatic, biliary or pancreatic disorders (e.g., chronic pancreatitis or pancreatic carcinoma). It is especially successful in treating postoperative biliary leaks, and may prevent surgical intervention[1,2]. Stenting of the biliary duct can be performed with a variety of prosthese that can differ by size, design and material[3,4].
The available biliary endoprostheses can be classified by material into two categories: plastic (i.e., polyethylene, polyurethane and "Teflon") and metallic stents. Plastic endoprostheses are less expensive but have a higher risk of clogging and dislocation[5]. On the other hand, they are easier to remove or to change.
A routine change of an endoprosthesis after 3 mo is common practice, but this can be prolonged to 6 mo[6]. To avoid stent migration, the biliary stent should be placed across the sphincter of Oddi[7]. Distal stent migration is an infrequent late complication, but occurs in up to 6% of cases[3,8]. The majority of biliary endoprostheses pass through the intestine without any problems. Infrequently, however, stents get stuck in the bowel, leading to complications.
Endoscopic retrieval is often possible and surgical intervention is rarely necessary[9,10]. The most common site of a migrated biliary stent is the duodenum[11-17], whereas complications in the rest of the small intestine[18,19] or colon[20-30] are rare.
CASE REPORT
A 65-year-old female patient presented with 4 d of persistent diffuse colicky abdominal pain and localized peritonitis in the supra-symphysial area. Normal leukocytes, elevated C-reactive protein (14.5 mg/dL; normal value < 0.5) and simultaneous cystitis (6500 bacteria/μL; normal value < 600) were found. Three months previously, the patient had undergone a laparoscopic cholecystectomy 4 wk after acute cholangitis with choledocholithiasis. The intraoperatively placed easy-flow drainage showed early postoperative biliary secretion. Endoscopic retrograde cholangiography was performed and showed a small peripheral leakage from the liver. A residual bile duct stone that was causing partial obstruction was removed. A 12 French 10 cm plastic stent was placed in the common bile duct without sphincterotomy. Biliary drainage stopped concurrently. The patient was discharged on the ninth postoperative day. A biliary stent extraction was advised at 4-6 wk later, but this was not carried out because of the patient's non-compliance.
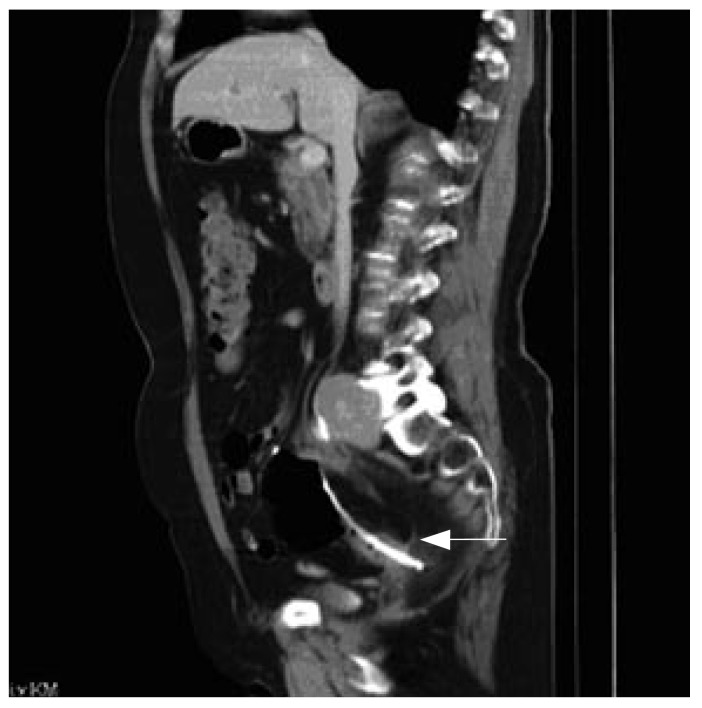
A computed tomography (CT) scan was performed because of extensive pain. A biliary stent dislocation and migration to the rectosigmoid colon was detected. The CT scan showed rectal perforation, and the stent was found in the rectal mesentery (Figure 1). A rectal resection was performed. After an uncomplicated postoperative recuperation, the patient was discharged on the seventh postoperative day.
Figure 1.
CT-scan of colonic perforation caused by migrated biliary endo-prosthesis. Arrow marks dislocated stent.
DISCUSSION
The incidence of postoperative biliary fistula is elevated in settings of acute or chronic inflammation[32-34]. Treatment options are surgical biliary leak repair, percutaneous biliary drainage, and endoscopic biliary drainage.
Endoscopic placement of a biliary endoprosthesis is a well-established procedure for treatment of biliary outflow obstruction. The most frequent complication associated with bile duct stents is early occlusion caused by clogging, with resultant cholangitis, or by tumor over-growth. Stent dislocation and proximal or distal migration are uncommon, with an overall incidence of up to 6%[3]. Several complications of stent migration have been reported and can be classified into categories of penetration, intestinal perforation, and obstruction. Other organs are usually unaffected[9,10].
Most ingested foreign bodies pass through the intestine without major problems. Neither size nor shape of the stent predicts the likelihood of successful conservative management. In all patients, a close follow-up after biliary stent placement is mandatory. Patients with diverticular disease, hernia or intra-abdominal adhesions, are especially at risk. Intestinal-wall weakness and increased resistance during bowel movement can produce localized complications[26,39].
Lesions of the intestinal wall due to biliary-stent migration have been reported in the duodenum, and are related to retroperitoneal fixation of this intestinal segment. Penetration requires adherence between the perforated and the penetrated organ, and does not induce intra-abdominal contamination, but eventually causes fistulae (i.e., interenteric or biliocolic[36], colovaginal[25] or colovesicular[27]).
Downstream migration is more frequent in benign than in malignant biliary duct strictures[9,35]. Benign stenoses are not as tight because of regression of inflammatory reactions after placement of the stent. By contrast, tumor growth can anchor a stent in malignant stenoses.
In the case of intestinal perforation, surgical stent removal and drainage of consecutive intra-abdominal or retroperitoneal abscesses is mandatory. A pelvic abscess[28], and colovesicular[27] or colocutaneous[29] fistula are typical consequences (Table 1). A case of necrotizing fasciitis due to colonic perforation has also been reported[31].
Table 1.
Colonic perforation due to biliary stent migration. Review of the literature to January 2007
| Reference | Year | Stent | Material | Type of bile duct lesion | Time to migration | Complication | Therapy |
| Anderson et al[28] | 2006 | Uk | Uk | Benign | 5 mo | Sigmoid diverticula perforation | Endoscopy |
| Wilhelm et al[27] | 2003 | Straight | Uk | Benign | 18 mo | Colovesicular fistula | Surgery |
| Diller et al[19] | 2003 | 7 French, 10 cm | Teflon | Benign | 1 mo | Stuck in sigmiod diverticula | Endoscopy |
| Elliott et al[21] | 2003 | 10 French, 10 cm 10 French, 10 cm | Uk | Benign | 4 mo | Sigmoid perforation | Surgery |
| Figueras et al[29] | 2001 | Straight | Polyethylene | Benign | 3 mo | Colocutaneous fistula | Surgery |
| Klein et al[26] | 2001 | Straight 7 French, 5 cm | Teflon | Benign | 3 yr | Sigmoid diverticular perforation | Surgery |
| Storkson et al[30] | 2000 | Straight | Plastic | Benign | 2 wk | Sigmoid perforation | Surgery |
| Lenzo et al[22] | 1998 | 7 French, 7, 5 cm | Polyethylene | Benign | 1 mo | Sigmoid diverticula perforation | Surgery |
| Baty et al[20] | 1996 | Uk | Polyethylene | Malign | 1 mo | Sigmoid diverticula perforation | Surgery |
| Schaafsma et al[23] | 1996 | Straight | Uk | Benign | 6 mo | Sigmoid perforation | Surgery |
| D´Costa et al[24] | 1994 | Uk | Uk | Malign | Uk | Sigmoid perforation | Surgery |
Uk: unknown.
A review of the literature published to January 2007 has revealed 11 cases of colonic perforation due to biliary stent migration, with the majority being straight plastic endoprostheses[10,17,26,27,29,38,40].
In conclusion, endoscopic insertion of biliary stents is a useful and powerful procedure for short-term decompression of the biliary system. In the case of long-term therapy, stent-migration-associated complications have to be considered as a differential diagnosis that may lead to life-threatening situations. A correct diagnosis is sometimes difficult to make because of the absence of typical symptoms.
A migrated biliary stent, symptomatic or not, should be removed immediately[19]. In cases of intestinal perforation, immediate surgical therapy is required. In cases of benign lesions of the bile duct, the stent should be either removed early to decrease the risk of secondary complications, or replaced regularly to prevent stent obstruction, infection or migration.
Caution should be exercised when straight plastic stents are inserted, and these should be closely followed-up.
Footnotes
S- Editor Liu Y L- Editor Kerr C E- Editor Li JL
References
- 1.Costamagna G, Pandolfi M, Mutignani M, Spada C, Perri V. Long-term results of endoscopic management of postoperative bile duct strictures with increasing numbers of stents. Gastrointest Endosc. 2001;54:162–168. doi: 10.1067/mge.2001.116876. [DOI] [PubMed] [Google Scholar]
- 2.Agarwal N, Sharma BC, Garg S, Kumar R, Sarin SK. Endoscopic management of postoperative bile leaks. Hepatobiliary Pancreat Dis Int. 2006;5:273–277. [PubMed] [Google Scholar]
- 3.Johanson JF, Schmalz MJ, Geenen JE. Incidence and risk factors for biliary and pancreatic stent migration. Gastrointest Endosc. 1992;38:341–346. doi: 10.1016/s0016-5107(92)70429-5. [DOI] [PubMed] [Google Scholar]
- 4.Moesch C, Sautereau D, Cessot F, Berry P, Mounier M, Gainant A, Pillegand B. Physicochemical and bacteriological analysis of the contents of occluded biliary endoprostheses. Hepatology. 1991;14:1142–1146. [PubMed] [Google Scholar]
- 5.Levy MJ, Baron TH, Gostout CJ, Petersen BT, Farnell MB. Palliation of malignant extrahepatic biliary obstruction with plastic versus expandable metal stents: An evidence-based approach. Clin Gastroenterol Hepatol. 2004;2:273–285. doi: 10.1016/s1542-3565(04)00055-2. [DOI] [PubMed] [Google Scholar]
- 6.Frakes JT, Johanson JF, Stake JJ. Optimal timing for stent replacement in malignant biliary tract obstruction. Gastrointest Endosc. 1993;39:164–167. doi: 10.1016/s0016-5107(93)70058-9. [DOI] [PubMed] [Google Scholar]
- 7.Pedersen FM, Lassen AT, Schaffalitzky de Muckadell OB. Randomized trial of stent placed above and across the sphincter of Oddi in malignant bile duct obstruction. Gastrointest Endosc. 1998;48:574–579. doi: 10.1016/s0016-5107(98)70038-0. [DOI] [PubMed] [Google Scholar]
- 8.Mueller PR, Ferrucci JT, Teplick SK, vanSonnenberg E, Haskin PH, Butch RJ, Papanicolaou N. Biliary stent endoprosthesis: analysis of complications in 113 patients. Radiology. 1985;156:637–639. doi: 10.1148/radiology.156.3.4023221. [DOI] [PubMed] [Google Scholar]
- 9.Jendresen MB, Svendsen LB. Proximal displacement of biliary stent with distal perforation and impaction in the pancreas. Endoscopy. 2001;33:195. doi: 10.1055/s-2001-11920. [DOI] [PubMed] [Google Scholar]
- 10.Liebich-Bartholain L, Kleinau U, Elsbernd H, Büchsel R. Biliary pneumonitis after proximal stent migration. Gastrointest Endosc. 2001;54:382–384. doi: 10.1067/mge.2001.113646. [DOI] [PubMed] [Google Scholar]
- 11.Miller G, Yim D, Macari M, Harris M, Shamamian P. Retroperitoneal perforation of the duodenum from biliary stent erosion. Curr Surg. 2005;62:512–515. doi: 10.1016/j.cursur.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 12.Bui BT, Oliva VL, Ghattas G, Daloze P, Bourdon F, Carignan L. Percutaneous removal of a biliary stent after acute spontaneous duodenal perforation. Cardiovasc Intervent Radiol. 1995;18:200–202. doi: 10.1007/BF00204152. [DOI] [PubMed] [Google Scholar]
- 13.Elder J, Stevenson G. Delayed perforation of a duodenal diverticulum by a biliary endoprosthesis. Can Assoc Radiol J. 1993;44:45–48. [PubMed] [Google Scholar]
- 14.Gould J, Train JS, Dan SJ, Mitty HA. Duodenal perforation as a delayed complication of placement of a biliary endoprosthesis. Radiology. 1988;167:467–469. doi: 10.1148/radiology.167.2.3282263. [DOI] [PubMed] [Google Scholar]
- 15.Humar A, Barron PT, Sekar AS, Lum A. Pancreatitis and duodenal perforation as complications of an endoscopically placed biliary stent. Gastrointest Endosc. 1994;40:365–366. doi: 10.1016/s0016-5107(94)70075-3. [DOI] [PubMed] [Google Scholar]
- 16.Melita G, Currò G, Iapichino G, Princiotta S, Cucinotta E. Duodenal perforation secondary to biliary stent dislocation: a case report and review of the literature. Chir Ital. 2005;57:385–388. [PubMed] [Google Scholar]
- 17.Basile A, Macri' A, Lamberto S, Caloggero S, Versaci A, Famulari C. Duodenoscrotal fistula secondary to retroperitoneal migration of an endoscopically placed plastic biliary stent. Gastrointest Endosc. 2003;57:136–138. doi: 10.1067/mge.2003.37. [DOI] [PubMed] [Google Scholar]
- 18.Esterl RM, St Laurent M, Bay MK, Speeg KV, Halff GA. Endoscopic biliary stent migration with small bowel perforation in a liver transplant recipient. J Clin Gastroenterol. 1997;24:106–110. doi: 10.1097/00004836-199703000-00014. [DOI] [PubMed] [Google Scholar]
- 19.Diller R, Senninger N, Kautz G, Tübergen D. Stent migration necessitating surgical intervention. Surg Endosc. 2003;17:1803–1807. doi: 10.1007/s00464-002-9163-5. [DOI] [PubMed] [Google Scholar]
- 20.Baty V, Denis B, Bigard MA, Gaucher P. Sigmoid diverticular perforation relating to the migration of a polyethylene endoprosthesis. Endoscopy. 1996;28:781. doi: 10.1055/s-2007-1005606. [DOI] [PubMed] [Google Scholar]
- 21.Elliott M, Boland S. Sigmoid colon perforation following a migrated biliary stent. ANZ J Surg. 2003;73:669–670. doi: 10.1046/j.1445-2197.2003.02698.x. [DOI] [PubMed] [Google Scholar]
- 22.Lenzo NP, Garas G. Biliary stent migration with colonic diverticular perforation. Gastrointest Endosc. 1998;47:543–544. doi: 10.1016/s0016-5107(98)70262-7. [DOI] [PubMed] [Google Scholar]
- 23.Schaafsma RJ, Spoelstra P, Pakan J, Huibregtse K. Sigmoid perforation: a rare complication of a migrated biliary endoprosthesis. Endoscopy. 1996;28:469–470. doi: 10.1055/s-2007-1005523. [DOI] [PubMed] [Google Scholar]
- 24.D'Costa H, Toy E, Dennis MJ, Brown C. Case report: intestinal perforation--an unusual complication of endoscopic biliary stenting. Br J Radiol. 1994;67:1270–1271. doi: 10.1259/0007-1285-67-804-1270. [DOI] [PubMed] [Google Scholar]
- 25.Blake AM, Monga N, Dunn EM. Biliary stent causing colovaginal fistula: case report. JSLS. 2004;8:73–75. [PMC free article] [PubMed] [Google Scholar]
- 26.Klein U, Weiss F, Wittkugel O. Migration of a biliary Tannenbaum stent with perforation of sigmoid diverticulum. Rofo. 2001;173:1057. doi: 10.1055/s-2001-18306. [DOI] [PubMed] [Google Scholar]
- 27.Wilhelm A, Langer C, Zoeller G, Nustede R, Becker H. Complex colovesicular fistula: A severe complication caused by biliary stent migration. Gastrointest Endosc. 2003;57:124–126. doi: 10.1067/mge.2003.71. [DOI] [PubMed] [Google Scholar]
- 28.Anderson EM, Phillips-Hughes J, Chapman R. Sigmoid colonic perforation and pelvic abscess complicating biliary stent migration. Abdom Imaging. 2007;32:317–319. doi: 10.1007/s00261-006-9067-2. [DOI] [PubMed] [Google Scholar]
- 29.Figueiras RG, Echart MO, Figueiras AG, González GP. Colocutaneous fistula relating to the migration of a biliary stent. Eur J Gastroenterol Hepatol. 2001;13:1251–1253. doi: 10.1097/00042737-200110000-00021. [DOI] [PubMed] [Google Scholar]
- 30.Størkson RH, Edwin B, Reiertsen O, Faerden AE, Sortland O, Rosseland AR. Gut perforation caused by biliary endoprosthesis. Endoscopy. 2000;32:87–89. doi: 10.1055/s-2000-87. [DOI] [PubMed] [Google Scholar]
- 31.Marsman JW, Hoedemaker HP. Necrotizing fasciitis: fatal complication of migrated biliary stent. Australas Radiol. 1996;40:80–83. doi: 10.1111/j.1440-1673.1996.tb00353.x. [DOI] [PubMed] [Google Scholar]
- 32.Binmoeller KF, Katon RM, Shneidman R. Endoscopic management of postoperative biliary leaks: review of 77 cases and report of two cases with biloma formation. Am J Gastroenterol. 1991;86:227–231. [PubMed] [Google Scholar]
- 33.Peters JH, Gibbons GD, Innes JT, Nichols KE, Front ME, Roby SR, Ellison EC. Complications of laparoscopic cholecystectomy. Surgery. 1991;110:769–777; discussion 777-778. [PubMed] [Google Scholar]
- 34.Deziel DJ, Millikan KW, Economou SG, Doolas A, Ko ST, Airan MC. Complications of laparoscopic cholecystectomy: a national survey of 4,292 hospitals and an analysis of 77,604 cases. Am J Surg. 1993;165:9–14. doi: 10.1016/s0002-9610(05)80397-6. [DOI] [PubMed] [Google Scholar]
- 35.Culp WC, McCowan TC, Lieberman RP, Goertzen TC, LeVeen RF, Heffron TG. Biliary strictures in liver transplant recipients: treatment with metal stents. Radiology. 1996;199:339–346. doi: 10.1148/radiology.199.2.8668775. [DOI] [PubMed] [Google Scholar]
- 36.Fiori E, Mazzoni G, Galati G, Lutzu SE, Cesare A, Bononi M, Bolognese A, Tocchi A. Unusual breakage of a plastic biliary endoprosthesis causing an enterocutaneous fistula. Surg Endosc. 2002;16:870. doi: 10.1007/s004640042021. [DOI] [PubMed] [Google Scholar]
- 37.Levey JM. Intestinal perforation in a parastomal hernia by a migrated plastic biliary stent. Surg Endosc. 2002;16:1636–1637. doi: 10.1007/s00464-002-4506-9. [DOI] [PubMed] [Google Scholar]
- 38.Mistry BM, Memon MA, Silverman R, Burton FR, Varma CR, Solomon H, Garvin PJ. Small bowel perforation from a migrated biliary stent. Surg Endosc. 2001;15:1043. doi: 10.1007/s004640041008. [DOI] [PubMed] [Google Scholar]
- 39.Ruffolo TA, Lehman GA, Sherman S, Aycock R, Hayes A. Biliary stent migration with colonic diverticular impaction. Gastrointest Endosc. 1992;38:81–83. doi: 10.1016/s0016-5107(92)70342-3. [DOI] [PubMed] [Google Scholar]
- 40.Mofidi R, Ahmed K, Mofidi A, Joyce WP, Khan Z. Perforation of ileum: an unusual complication of distal biliary stent migration. Endoscopy. 2000;32:S67. [PubMed] [Google Scholar]