Abstract
Digital whole slide imaging (WSI) is an emerging technology for pathology interpretation; however, little is known about pathologists’ practice patterns or perceptions regarding WSI. A national sample (N = 252) of pathologists from New Hampshire, Vermont, Washington, Oregon, Arizona, Alaska, Maine, and Minnesota were surveyed in this cross-sectional study (2011–2013). The survey included questions on pathologists’ experience, WSI practice patterns, and perceptions using a six-point Likert scale. Agreement was summarized with descriptive statistics to characterize pathologists’ use and perceptions of WSI. The majority of participating pathologists were males (63 %) between 40 and 59 years of age (70 %) and not affiliated with an academic medical center (72 %). Experience with WSI was reported by 49 %. Types of use reported included CME/board exams/teaching (28 %), tumor board/clinical conference (22 %), archival purposes (6 %), consultative diagnosis (4 %), research (4 %), and other uses (12 %). Most respondents (79 %) agreed that accurate diagnoses can be made with this technology, and that WSI is useful for obtaining a second opinion (88 %). However, 78 % of pathologists agreed that digital slides are too slow for routine clinical interpretation. Fifty-nine percent agreed that the benefits of WSI outweigh concerns. The respondents were equally split as to whether they would like to adopt WSI (51 %) or not (49 %). About half of pathologists reported experience with the WSI technology, largely for CME, licensure/board exams, and teaching. Positive perceptions regarding WSI slightly outweigh negative perceptions. Understanding practice patterns with WSI as dissemination advances may facilitate concordance of perceptions with adoption of the technology.
Keywords: Digital whole slide imaging, Pathology
Introduction
Digital whole slide imaging (WSI), sometimes referred to as “virtual microscopy,” is a technology that allows glass slides of pathology specimens to be scanned (digitized) and viewed on a computer screen [1]. Digital WSI is intended to simulate, or even enhance, the viewing experienced with standard microscopy techniques, and is introducing major changes into the clinical practice and teaching of pathology [2–10]. While health information technology is diffusing rapidly into clinical practice, the broad use of WSI has slowed after a 2011 ruling by the US Food and Drug Administration (FDA) regulating use the of WSI for primary diagnosis as a class III medical device [11], which are devices with insufficient information to assure safety and effectiveness through sets of controls [12]. Nevertheless, WSI technologies and applications are expanding, as is their adoption [13]. The European Union and Canada have approved WSI for primary diagnosis, leaving the US as the only industrialized Western country where this technology is not currently approved [13]. The rate at which use of WSI continues to expand in the near term depends largely on the course of FDA regulation, but also on clinicians’ perceptions. Our understanding of the adoption of WSI in the US is limited by the lack of knowledge of the extent, and type of WSI use by pathologists, and their perceptions regarding this technology [3].
Digital WSI has roots in telepathology and so is not entirely new to the field of pathology. However, digital WSI is also thought to fill—or potentially fill—other distinct roles, such as reducing logistical demands of physical specimens (transport, storage) [4–10], integrating into electronic health records [11], improve routine diagnostics [14, 15], validation studies [15, 16], and teaching/training [17].
Despite the purported benefits of WSI, several factors currently limit widespread adoption, such as concerns about image quality, workflow, and expense [18, 19]. Although the methods for evaluating image quality of WSI are being developed [19], comparative studies of image and interpretive quality of WSI and glass slides are lacking. Image analysis algorithms are being developed to help improve interpretive accuracy while reducing the length of viewing time for WSI, which may be greater than for glass slides [3]. Finally, high throughput scanners and the staff time required to scan each slide can be expensive, a disincentive for widespread use.
Considering the advantages and disadvantages of WSI, the shift towards health technology is inevitable, and diffusion and improvement of WSI will continue. In fact, the trend among medical schools is to use digital images and digital slide libraries instead of light microscopes for pathology courses, thus potentially creating a new generation of digitally-trained pathologists [20]. Despite the 2011 FDA ruling, WSI continues to be used for a variety of purposes, but there is very little known about the patterns of use among pathologists or their perceptions of WSI for pathology interpretation.
The purpose of this study was to characterize the use of WSI among a national sample of pathologists who interpret breast specimens. Specifically, we describe (1) pathologists’ use of digital WSI in relation to demographic and professional characteristics, and (2) pathologists’ perceptions about digital WSI. This study provides new information about the current use of WSI and perceived barriers to uptake among pathologists.
Materials and Methods
Study Population
We surveyed a geographically dispersed sample of US pathologists from eight states as follows: New Hampshire, Vermont, Washington, Oregon, Arizona, Alaska, Maine, and Minnesota in this cross-sectional study. Eligibility criteria included the completion of residency and/or fellowship training more than a year prior, interpreting breast tissue for at least 1 year prior, and planning to continue interpreting breast tissue for the next 2 years. Participants were invited to participate in the survey beginning in November 2011, and all surveys were completed by February 2013. All participants completed an online survey designed and produced as a stand-alone study-based website, for a larger study about pathologists’ interpretations of breast pathology (B-PATH) [21]. Pathologists were identified through their participation in the Breast Cancer Surveillance Consortium (BCSC) or affiliation with Providence Health & Services Oregon, and by lists from professional organizations, internet searches, and telephone calls to pathology facilities. An invitation to the study was sent by email and additional follow-up made by telephone calls. Interested, eligible pathologists were asked to complete a web-based survey that included questions on demographics, training, clinical experience, and perceptions about the diagnosis of breast pathology specimens.
Key Measures
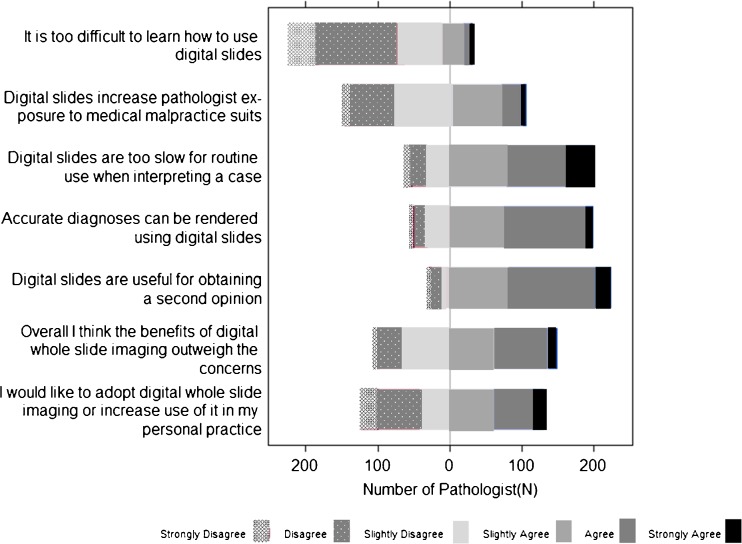
Pathologists reported personal and professional characteristics, such as gender, year of birth, professional affiliation with an academic medical center, fellowship training in surgical or breast pathology, number of years interpreting breast pathology, percentage of caseload that are breast specimens, number of breast cases interpreted in an average week, and whether their colleagues’ consider them an expert in breast pathology. Pathologists also reported WSI practice patterns, including ways in which they use WSI for clinical and educational purposes, use of WSI for providing a primary or secondary diagnosis of breast specimens, length of time using WSI, and use of WSI for IHC tests. They then responded to statements about their perceptions of WSI using a six-point Likert scale (strongly agree, agree, slightly agree, slightly disagree, disagree, and strongly disagree). Statements include the following: (1) accurate diagnoses can be rendered using digital slides; (2) digital slides are useful for obtaining a second opinion; (3) digital slides increase pathologist exposure to medical malpractice suits; (4) it is too difficult to learn how to use digital slides; (5) overall, I think the benefits of digital whole slide imaging outweigh the concerns; (6) digital slides are too slow for routine use when interpreting a case; (7) I would like to adopt digital whole slide imaging or increase use of it in my personal practice.
Analyses
Descriptive statistics were used to characterize participating pathologists and their uses of WSI. Assessments of practice patterns in relation to pathologist characteristics were performed using chi-square. Pathologists’ perceptions of WSI were summarized with frequencies of response categories. For some outcomes, responses were collapsed into binary categories of “agree” and “disagree.” We compared the characteristics of pathologists who agreed that “Overall, I think the benefits of digital whole slide imaging outweigh the concerns,” and “I would like to adopt digital whole slide imaging or increase use of it in my personal practice,” with those who disagreed with this statement. All analyses were performed using Stata v12.0 statistical software. Institutional review boards at the University of Washington, Dartmouth College, the University of Vermont, Fred Hutchinson Cancer Research Center, and Providence Health & Services Oregon approved of all study activities.
Results
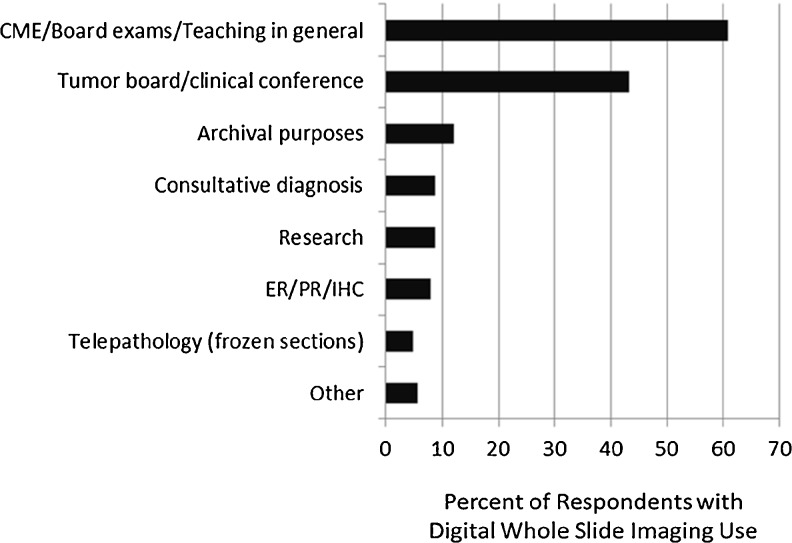
Pathologists (N = 691) were invited to participate in an intensive CME program; 146 were not eligible, and among the remaining 545, 137 (25 %) were not interested, 156 (29 %) did not respond to the invitations, and 252 (46 %) were eligible and completed the survey. The majority of respondents were male (63 %; Table 1). The age distribution was <40 (12 %), 40–49 (33 %), 50–59 (37 %), and ≥60(18 %) years. Most pathologists were not affiliated with an academic medical center (72 %). Of those with no academic medical center affiliation, 60 % did not use WSI, compared to 74 % of those with an adjunct affiliation, and 78 % with a primary academic medical center appointment. Overall experience using WSI was split, with 49 % of pathologists indicating they previously used WSI, while 51 % did not. For those who used WSI, types of use included continuing medical education (CME), board exams, and teaching (28 %); tumor board or clinical conference (22 %); archival purposes (6 %); consultative diagnosis (4 %); research (4 %); and other uses (12 %), such as intradepartmental review (Fig. 1).
Table 1.
Characteristics of study pathologists (N = 252)
| Characteristics | N (%) |
|---|---|
| Age (years) | |
| <40 | 31 (12) |
| 40–49 | 83 (33) |
| 50–59 | 92 (37) |
| ≥60 | 46 (18) |
| Gender | |
| Female | 93 (37) |
| Male | 159 (63) |
| Affiliation with academic medical center | |
| No | 183 (72) |
| Yes, adjunct/affiliated | 42 (17) |
| Yes, primary appointment | 27 (11) |
| Fellowship training in breast pathologya | |
| No | 129 (51) |
| Yes, surgical | 119 (47) |
| Yes, breast pathology | 12 (5) |
| Years interpreting breast pathologyb | |
| <5 | 46 (18) |
| 5–9 | 44 (18) |
| 10–19 | 89 (35) |
| ≥20 | 73 (29) |
| Percent of caseload interpreting breast specimens | |
| <10 % | 126 (50) |
| 10–24 % | 104 (41) |
| >25 % | 22 (9) |
| Number of breast cases per week | |
| <5 | 57 (23) |
| 5–9 | 109 (43) |
| 10–19 | 64 (25) |
| >20 | 22 (9) |
| Considered an expert in breast pathology by colleagues | |
| No | 200 (79) |
| Yes | 52 (21) |
aEight respondents were trained in both surgical and breast pathology, resulting in a column total >100 % for this variable
bNot including residency/fellowship training
Fig. 1.
Types of use of whole slide imaging from pathologists reporting previous use (124/252; 49 %). Users could indicate more than one category
Most participants agreed that accurate diagnoses can be made with WHS (79 % agree), and that WSI is useful for obtaining a second opinion (88 % agree; Fig. 2). However, 78 % of pathologists believed that digital slides are too slow for routine initial clinical interpretation. Most pathologists were not concerned that the use of WSI would increase their exposure to medical malpractice suits or that it would be difficult to learn. When asked if the benefits of WSI outweigh the concerns, 59 % agreed. Just over half of the pathologists (51 %) agreed that they would like to adopt WSI into their practices.
Fig. 2.
Pathologists’ (N = 252) perceptions of digital whole slide imaging in breast pathology practice
Characteristics of pathologists who agreed that the benefits of WSI outweigh the concerns or that they would like to adopt WSI or increase its use were not different according to age, gender, training, and clinical experience in breast pathology (Table 2). However, a significantly higher proportion of pathologists who agreed with both of these statements had an adjunct affiliation with an academic medical center. Correlation was fairly high (Spearman’s rho 0.66) among agreement responses for those who would like to adopt or increase use, and those who overall think the benefits of WSI outweigh the concerns.
Table 2.
Characteristics of pathologists (N = 252) who agreed with the perception statements about digital whole slide imaging
| Overall I think the benefits of digital whole slide imaging outweigh the concerns | P value for agree versus disagree | I would like to adopt digital whole slide imaging or increase use of it in my personal practice | P value for agree versus disagree | |
|---|---|---|---|---|
| N (row %) Agree | N (row %) Agree | |||
| Total | 129 (58.7) | 129 (51.4) | ||
| Age (years) | ||||
| <40 | 20 (64.5) | 0.70 | 17 (54.8) | 0.94 |
| 40–49 | 44 (54.7) | 40 (48.2) | ||
| 50–59 | 55 (59.8) | 48 (52.2) | ||
| ≥60 | 46 (60.9) | 24 (52.2) | ||
| Gender | ||||
| Male | 96 (60.4) | 0.44 | 84 (52.8) | 0.55 |
| Female | 51 (55.4) | 45 (48.4) | ||
| Affiliation with academic medical center | ||||
| No | 100 (55.0) | 0.04 | 83 (45.4) | 0.01 |
| Yes, adjunct/affiliated | 32 (76.2) | 30 (71.4) | ||
| Yes, primary appointment | 15 (55.6) | 16 (59.3) | ||
| Fellowship training in breast pathology | ||||
| No | 73 (57.0) | 0.62 | 69 (53.9) | 0.42 |
| Yes, surgical and/or breast pathology | 74 (60.2) | 60 (48.8) | ||
| Years interpreting breast pathologya | ||||
| <5 | 28 (62.2) | 0.89 | 22 (48.9) | 0.47 |
| 5–9 | 27 (61.4) | 27 (61.4) | ||
| 10–19 | 50 (56.2) | 42 (47.2) | ||
| ≥20 | 42 (57.5) | 38 (52.1) | ||
| Percent of caseload interpreting breast specimens | ||||
| <10 % | 76 (59.4) | 0.30 | 65 (50.8) | 0.29 |
| 10–24 % | 57 (54.8) | 51 (49.0) | ||
| >25 % | 14 (73.7) | 13 (68.4) | ||
| Number of breast cases per week | ||||
| <5 | 33 (57.9) | 0.81 | 28 (49.1) | 0.88 |
| 5–9 | 66 (60.5) | 55 (50.5) | ||
| 10–19 | 34 (54.0) | 33 (52.4) | ||
| >20 | 14 (63.6) | 13 (59.1) | ||
| Considered an expert in breast pathology by colleagues | ||||
| No | 113 (79.3) | 0.26 | 97 (48.7) | 0.10 |
| Yes | 34 (65.4) | 32 (61.5) | ||
aNot including residency/fellowship training
Discussion
This is the first study describing pathologists’ practice patterns and perceptions regarding the use of WSI for breast specimens. About half of all surveyed pathologists used WSI for various purposes, including tumor boards, clinical conferences, continuing medical education, board exams, teaching, archiving, research, and consultative diagnosis. WSI was perceived as accurate diagnostically and useful for obtaining second opinions. Although the majority of pathologists agreed that overall the benefits of WSI outweigh the concerns, only about half of surveyed pathologists were interested in adopting it in their own practice, which may be due, in part, to the perception of WSI being too slow for routine interpretation.
In this study, the majority of pathologists thought that WSI was accurate, a view that is counter to concerns raised in the literature about the use of WSI in routine pathology practice. Specifically, some factors that may influence accuracy are of concern, such as of image quality, user training/experience, and comparative accuracy to glass slides [17–19]. A key criticism of image quality with WSI is that of focus, given that tissue thickness may be variable within a specimen. Furthermore, tradeoffs exist between file size and resolution/image detail. Compounding these issues is the lack of image standards in pathology and image quality evaluation methods, unlike in radiology, where they are well developed [8, 20]. Agreement studies comparing glass slides with digital slides for pathology interpretation have begun to provide evidence that supports the use of WSI [22, 23, 24], including a recent study demonstrating 96.5 % concordance between WSI and light microscopy [24]. Even within breast pathology specifically, concordance studies provide evidence that reliable histopathologic diagnoses can be made with WSI [25]. However, until the evidence translates into FDA approval for primary diagnosis, the clinical applications will be limited in the US.
This study showed a concern over the slowness of using WSI, which could be due to a number of factors related to imaging speed, such as software/viewers, technical capacity, and number of images per case. Prior work suggests that improvements in image-viewing browsers may help the adoption of WSI. Browsers typically have tools for navigation, annotation, and noting regions of interest, but viewing of the complete slide can be slow, and their limited integration into laboratory information systems often requires manual entry of data associated with the slides [8]. Understanding these issues related to slowness such as hardware, software, usability, clinical workflow, accuracy, and pathologists’ perceptions will allow for adoption of WSI in a more guided, effective manner.
Although little evidence exists for pathologist perceptions of WSI in the US [26], a recent study of Canadian pathologists’ perceptions of WSI provided an interesting glimpse into practice that includes primary diagnosis [27]. Similar to our findings, the most common use for WSI was for teaching purposes, with consultation being the second most common use in the Canadian study [28]. The proportion of pathologists using digital images in their practice or for training was higher than in our US study (85 vs. 49 %), which may reflect the more comprehensive adoption of WSI by regulatory bodies in Canada, or may reflect bias among responders. In the US, advances in WSI technology, systems, and overall trends in health information technology will continue to drive adoption of WSI, particularly as user experience and perceptions evolve.
Conclusion
In our study of a national sample of pathologists who diagnose breast lesions, our reported pathologist use and perceptions of WSI provide an important snapshot into the current state of pathologists’ perception about digital pathology adoption in the US. We identified possible barriers to uptake among pathologists, such as WSI being slow to use. Overall, as evidenced by current use patterns, it seems that for some applications, particularly teaching, CME, board exams, and clinical conferences, the advantages of WSI outweigh the disadvantages. For applications such as consultative diagnosis, technological improvements will likely be required to shift the balance to being advantageous.
Acknowledgments
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under award number R01 CA140560 and KO5 CA104699. The content is solely the responsibility of the authors and does not necessarily represent the views of the National Cancer Institute or the National Institutes of Health. We would also like to acknowledge Thomas Morgan at the University of Washington, Seattle WA and Paul Litwin of the Fred Hutchinson Cancer Center, Seattle, WA for valuable assistance with data preparation and transfer.
References
- 1.May M. A better lens on disease. Scientific American. May 1, 2010. https://www.scientificamerican.com/article.cfm?id=a-better-lens-on-disease [DOI] [PubMed]
- 2.Al-Janabi S, Huisman A, Vink A, Leguit RJ, Offerhaus JA, ten Kate FJW, et al. Whole slide images for primary diagnostics in dermatopathology: a feasibility study. J Clin Pathol. 2012;65:152–158. doi: 10.1136/jclinpath-2011-200277. [DOI] [PubMed] [Google Scholar]
- 3.Al-Janabi S, Huisman A, Van Diest PJ. Digital pathology; current status and future perspectives. Histopathology. 2012;61:1–9. doi: 10.1111/j.1365-2559.2011.03814.x. [DOI] [PubMed] [Google Scholar]
- 4.Joel F, Leong WM, Leong ASY. Digital imaging in pathology: theoretical and practical considerations, and applications. Pathology. 2004;36(3):234–241. doi: 10.1080/00313020410001692576. [DOI] [PubMed] [Google Scholar]
- 5.Dangott B, Parwani A. Whole slide imaging for teleconsultation and clinical use. J Pathol Inform. 2010;1:7. doi: 10.4103/2153-3539.65342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hedvat CV. Digital microscopy: past, present, and future. Arch Pathol Lab Med. 2010;134:1666–1670. doi: 10.5858/2009-0579-RAR1.1. [DOI] [PubMed] [Google Scholar]
- 7.Brachtel E, Yagi Y. Digital imaging in pathology—current applications and challenges. J Biophotonics. 2012;5:327–335. doi: 10.1002/jbio.201100103. [DOI] [PubMed] [Google Scholar]
- 8.Pantanowitz L, Valenstein PN, Evans AJ, Kaplan KJ, Pfeifer JD, Wilbur DC. Review of the current state of whole slide imaging in pathology. J Pathol Inform. 2011;2:36. doi: 10.4103/2153-3539.83746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patterson ES, Rayo M, Gil C, Gurcan MN. Barriers and facilitators to adoption of soft copy interpretation from the user perspective: lessons learned from filmless radiology for slideless pathology. J Pathol Inform. 2011;2:1. doi: 10.4103/2153-3539.74940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rocha R, Vassallo J, Soares F, Miller K, Gobbi H. Digital slides: present status of a tool for consultation, teaching, and quality control in pathology. Pathol Res Pract. 2009;205(11):73–741. doi: 10.1016/j.prp.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 11.College of American Pathologists. http://www.cap.org/apps/cap.portal?_nfpb=true&cntvwrPtlt_actionOverride=%2Fportlets%2FcontentViewer%2Fshow&_windowLabel=cntvwrPtlt&cntvwrPtlt%7BactionForm.contentReference%7D=cap_today%2F0112%2F0112a_regulators.html&_state=maximized&_pageLabel=cntvwr, last accessed 2/14/14.
- 12.U.S. Food and Drug Administration. http://www.fda.gov/MedicalDevices/DeviceRegulationandGuidance/Overview/ClassifyYourDevice/. Last accessed: 06/14/13.
- 13.Allen TC. Digital pathology and federalism. Archives of Pathology and Laboratory Medicine. 2012. 0.5858/arpa.2013-0258-ED [DOI] [PubMed]
- 14.Wilbur DC, Madi K, Colvin RB, Duncan LM, Faquin WC, Ferry JA, et al. Whole-slide imaging digital pathology as a platform for teleconsultation: a pilot study using paired subspecialist correlations. Arch Pathol Lab Med. 2009;133:1949–1953. doi: 10.1043/1543-2165-133.12.1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krenacs T, Zsakovics I, Diczhazi L, Ficsor VS, Varga VS, Molnar B. The potential of digital microscopy in breast pathology. Pathol Oncol Res. 2009;15:55–58. doi: 10.1007/s12253-008-9087-z. [DOI] [PubMed] [Google Scholar]
- 16.Rossing HH, Møller Talman M-L, Lænkholm A-V, Wielenga VT. Implementation of TMA and digitalization in routine diagnostics of breast pathology. APMIS Acta Pathol Microbiol Immunol Scand. 2012;120:341–347. doi: 10.1111/j.1600-0463.2011.02871.x. [DOI] [PubMed] [Google Scholar]
- 17.Fung KM, Hassell LA, Talbert ML, Wiechmann AF, Chaser BE, Ramey J. Whole slide images and digital media in pathology education, testing, and practice: the Oklahoma experience. Anal Cell Pathol. 2012;35:37–40. doi: 10.3233/ACP-2011-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cornish TC, Swapp RE, Kaplan KJ. Whole-slide imaging: routine pathologic diagnosis. Adv Anat Pathol. 2012;19:152–159. doi: 10.1097/PAP.0b013e318253459e. [DOI] [PubMed] [Google Scholar]
- 19.Henricks WH. Evaluation of whole slide imaging for routine surgical pathology: looking through a broader scope. J Pathol Inform. 2012;3:39. doi: 10.4103/2153-3539.103009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hashimoto N, Bautista PA, Yamaguchi M, Ohyama N, Yagi Y. Referenceless image quality evaluation for whole slide imaging. J Pathol Inform. 2012;3:9. doi: 10.4103/2153-3539.93891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oster NV, Carney PA, Allison KH, Weaver D, Reisch L, Longton G, Onega T, Pepe M, Geller BM, Nelson H, Ross T, Tosteson AN, Elmore JG: Development of a diagnostic test set to assess agreement in breast pathology: practical application of the guidelines for reporting reliability and agreement studies (GRRAS). BMC Womens Health 13:3, 2013 [DOI] [PMC free article] [PubMed]
- 22.Jara-Lazaro AR, Thamboo TB, The M, Tan PH. Digital pathology: exploring its applications in diagnostic surgical pathology practice. Pathology. 2010;42:512–518. doi: 10.3109/00313025.2010.508787. [DOI] [PubMed] [Google Scholar]
- 23.Shaw EC, Hanby AM, Wheeler K, et al. Observer agreement comparing the use of virtual slides with glass slides in the pathology review component of the POSH breast cancer cohort study. J Clin Pathol. 2012;65:403–408. doi: 10.1136/jclinpath-2011-200369. [DOI] [PubMed] [Google Scholar]
- 24.Ho J, Parwani AV, Jukic CM, et al. Use of whole slide imaging in surgical pathology quality assurance: design and pilot validation studies. Hum Pathol. 2006;37:322–331. doi: 10.1016/j.humpath.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 25.Campbell WS, Lele SM, West WW, Lazenby AJ, Smith LM, Hinrichs SH. Concordance between whole-slide imaging and light microscopy for routine surgical pathology. Hum Pathol. 2012;43:1739–1744. doi: 10.1016/j.humpath.2011.12.023. [DOI] [PubMed] [Google Scholar]
- 26.Al-Janabi S, Hulsman A, Willems SM, Van Diest PJ. Digital slide images for primary diagnostics in breast pathology: a feasibility study. Hum Pathol. 2012;43:2318–2325. doi: 10.1016/j.humpath.2012.03.027. [DOI] [PubMed] [Google Scholar]
- 27.Mea VD, Demichelis F, Viel F, Palma PD, Betlrami CA. User attitudes in analyzing digital slides in a quality control test bed: a preliminary study. Comput Meth Prog Bio. 2006;82:177–186. doi: 10.1016/j.cmpb.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 28.Bellis M, Metias S, Naugler C, Pollett A, Jothy S, Yousef GM: Digital pathology: attitudes and practices in the Canadian pathology community. J Pathol Inform. 4:3, 2013. doi:10.4103/2153-3539.108540. Print 2013 [DOI] [PMC free article] [PubMed]