Abstract
Background
A high signal intensity cleft between the labrum and articular cartilage of the posterior glenoid is commonly visible on MRI and has been suggested to be anatomic variation [3, 10, 23]. The association of a posterior cleft with variations in glenoid morphology or with shoulder instability is unknown.
Questions/Purposes
The purposes of this study were to determine if posterior chondrolabral clefts are associated with variations in glenoid morphology, and to determine if they are associated with shoulder instability.
Patients and Methods
Shoulder MRI was performed in 1,264 shoulders, 1,135 male (89.8%), and 129 female (10.2%). A musculoskeletal radiologist blinded to history and outcomes evaluated the MR images for linear high signal intensity at the posterior chondrolabral junction and a rounded or truncated contour of the posterior glenoid. Glenoid version and depth were measured. Patients were followed prospectively for shoulder instability for 4 years. Univariate and multivariate statistical analysis were performed.
Results
Posterior chondrolabral cleft was present in 114/1,264. Posterior chondrolabral cleft was associated with a rounded or truncated posterior glenoid. There were 9.5° retroversion in shoulders with a posterior cleft, and 7.7° retroversion in shoulders without a cleft. Shoulders with a posterior chondrolabral cleft were more likely to develop shoulder instability.
Conclusions
Posterior chondrolabral clefts are not uncommon on MRI. They are associated with a rounded or truncated posterior glenoid and a small but significant increase in glenoid retroversion. They are associated with shoulder instability.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-014-9404-x) contains supplementary material, which is available to authorized users.
Keywords: shoulder MRI, posterior chondrolabral cleft, glenoid version, shoulder instability
Introduction
A cleft of high signal intensity between the posterior glenoid labrum and articular cartilage is commonly visible on magnetic resonance imaging (MRI) and computed tomography (CT) studies of the shoulder [10, 23] (Fig. 1). Cadaver dissections have also demonstrated a “crevice” between the fibrous labrum and articular cartilage of the posteroinferior glenoid [3]. Posterior chondrolabral clefts have been hypothesized to represent anatomic variation [3, 10, 23]. In our clinical experience, posterior chondrolabral clefts have often seemed to be associated with a rounded or truncated shape of the posterior glenoid. Yet previous imaging studies [10, 23] focused on the labral morphology without evaluating for an association with glenoid morphology. Also, previous studies have not attempted to determine if posterior chondrolabral clefts are associated with shoulder instability.
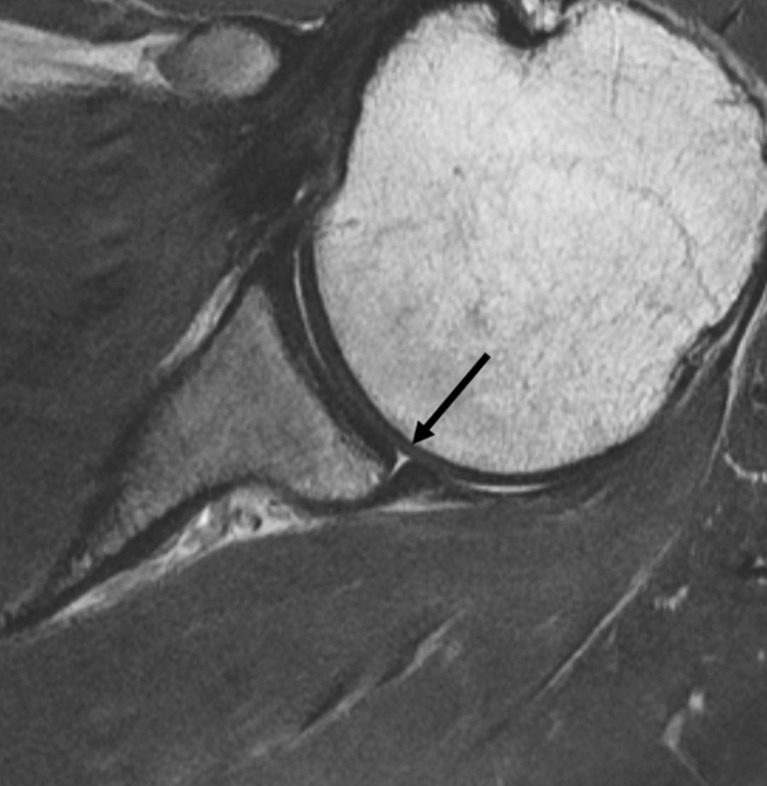
Fig. 1.
Axial intermediate echo time proton density weighted image of the shoulder (TE/TR 34/4000). There is a triangular cleft of fluid signal intensity between the posterior labrum and articular cartilage (arrow).
The purposes of this study were to determine if posterior chondrolabral clefts are associated with variations in glenoid morphology, and to determine if they are associated with shoulder instability.
Patients and Methods
This study was approved by our institutional review board, and HIPAA compliant. Enrollment was offered to all incoming freshman entering the United States Military Academy in 2006 as part of a prospective cohort study to evaluate for risk factors for shoulder instability in high-risk athletes. MR imaging was performed at the outset of the study for all participants to identify anatomic risk factors at baseline that were associated with the subsequent risk of glenohumeral instability during 4 years of follow-up. Adequate MR images were obtained of 1,264 shoulders in 714 subjects, including 1,135 (89.8%) in males and 129 (10.2%) in females. Mean patient age was 18.8 ± 1.0 years among males and 18.7 ± 0.9 years among females. All subjects were asked if they had ever had a shoulder dislocation. All subjects were subsequently followed for four consecutive years in a closed health care system for acute shoulder instability, including both anterior and posterior instability events.
Magnetic resonance imaging (MRI) examinations were performed on a 1.5 Tesla imaging system (Intera, Philips Medical Systems, Andover, MA), using a phased array surface coil (Synergy Flex-M, Philips Medical Systems, Andover, MA). Oblique coronal, turbo spin-echo, fat suppressed T2 weighted images were performed (TE/TR 50/2000; FOV 160–180 mm; slice 4 mm; interslice gap 0.4 mm; matrix 256 × 256; ETL 8–10; NEX 2). Additionally, an axial three-dimensional fast field-echo sequence was performed (TE/TR/FA 9/18/15°; FOV 160–180 mm; slice 2.4 mm; slice overlap 1.2 mm; matrix 256 × 256; NEX 2), from which multiplanar reformatted (MPR) images in oblique coronal and oblique sagittal planes were obtained at 1.3-mm intervals.
All MR images were interpreted by a musculoskeletal radiologist with 7 years of experience (SEC), who was blinded to baseline data and to clinical or imaging findings during the follow-up period. Axial MR images were evaluated for a medially curved [23] or triangular cleft of high signal intensity between the posterior glenoid labrum and articular cartilage (Fig. 2). The labrum needed to have smooth, regular margins for the lesion to be diagnosed as a labral cleft. If there were extension of the signal abnormality through the labrum, labral detachment from the glenoid, a complex pattern of high signal intensity through the labrum, labral, or periosteal irregularity, the lesion was classified as a tear rather than a cleft [9, 10, 12, 16, 22].
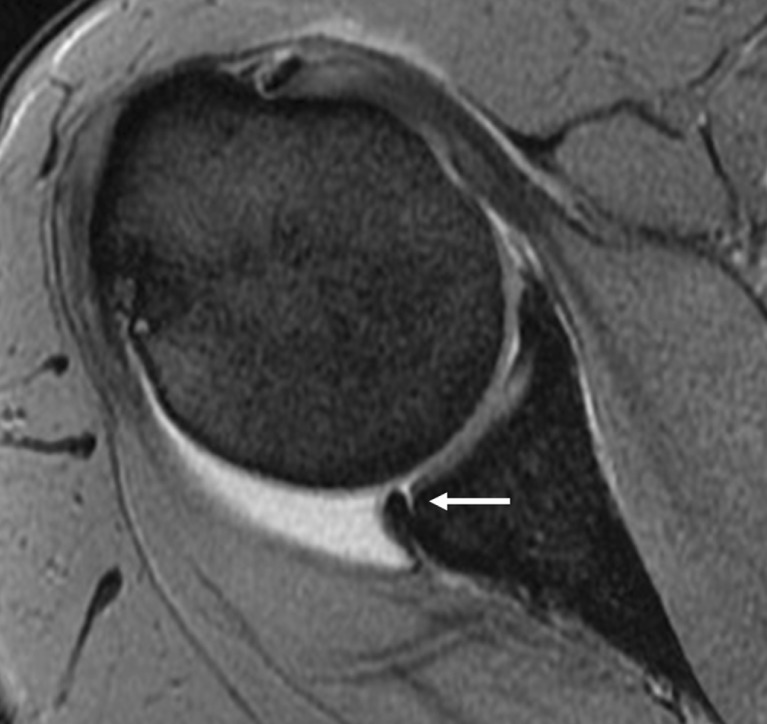
Fig. 2.
Axial fast field echo (FFE) image of the shoulder demonstrating a high signal intensity cleft between the posterior labrum and articular cartilage.
Qualitative and quantitative evaluations of the glenoid were performed as part of the MRI interpretation. The glenoid morphology was evaluated qualitatively on the axial MR images for hypoplasia, which was diagnosed as either a “sharp falling away” [4] or a rounded contour of the posteroinferior osseous glenoid (Fig. 3), excluding the inferiormost images [4, 6]. Also, axial MR images were used to measure the version angle of the osseous glenoid. At the level of the mid-glenoid, a first line was drawn from the posteromedial margin of the scapular body through the center of the glenoid. A second line was drawn perpendicular to the first. A third line was drawn from the anterior rim to the posterior rim of the bony glenoid, and its angle relative to line #2 was measured (Fig. 4) as the glenoid version [15, 21]. Glenoid retroversion was recorded as a negative number, and anteversion as a positive number. In addition, glenoid depth was measured by drawing one line from the anterior rim to the posterior rim of the glenoid labrum. The second line, perpendicular to line #1, extended from line #1 to the deepest portion of the articular surface of the glenoid (Fig. 5). This measurement was recorded in millimeters as glenoid depth.
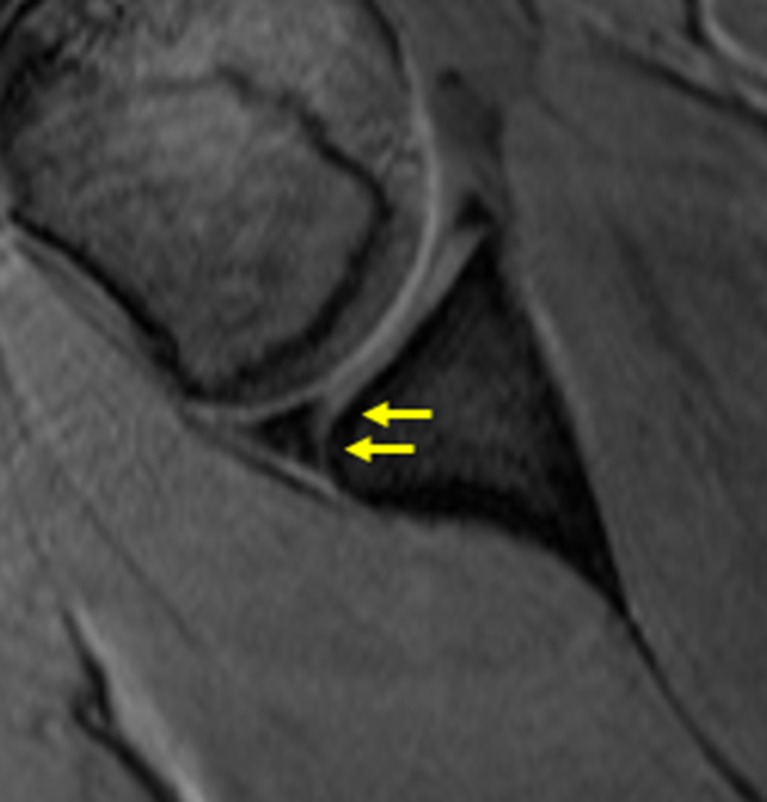
Fig. 3.
On axial images, excluding the inferior-most axial images, glenoid hypoplasia was diagnosed as a sharp falling away or rounding of the posterior osseous glenoid (arrows).
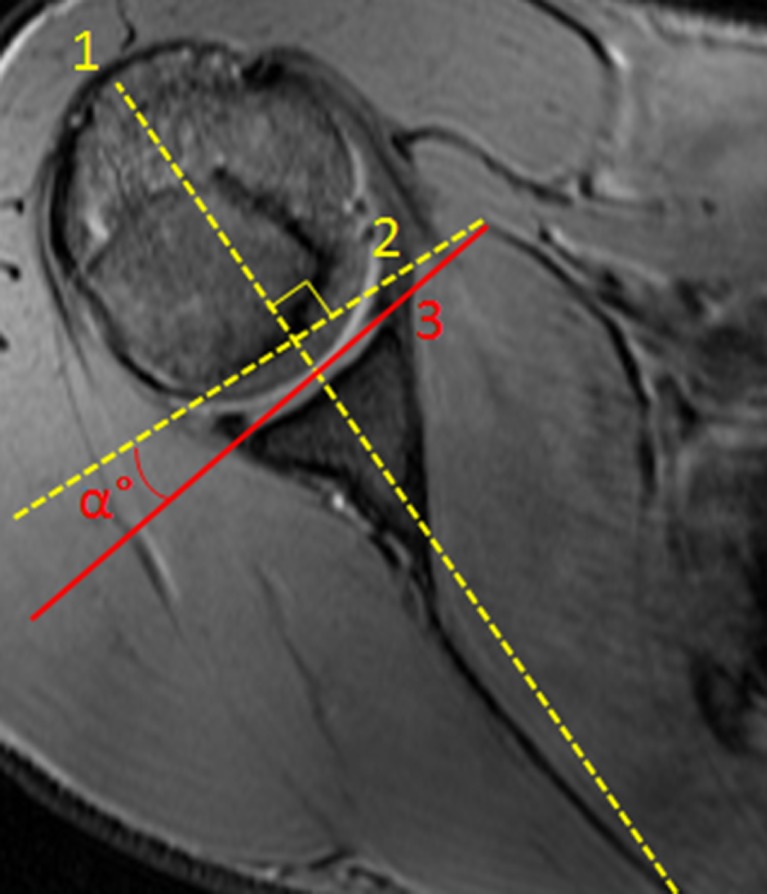
Fig. 4.
Glenoid version was measured at the mid-glenoid on axial images. Line 1 was drawn from the posteromedial margin of the scapular body through the mid glenoid. Line 2 was perpendicular to line 1. Line 3 was drawn from the anterior rim to the posterior rim of the osseous glenoid. The angle between lines 2 and 3 was glenoid version. Retroversion was recorded as a negative number, while anteversion was recorded as a positive number.
Fig. 5.
The glenoid depth was measured at the central glenoid on axial images. The first line was drawn from the anterior margin of the labrum to the posterior margin of the labrum. The second line, perpendicular to the first, was drawn from the first line to the deepest portion of the articular surface of the glenoid.
Subjects were followed prospectively in a closed health care system for 4 years, during which all acute shoulder instability injuries were documented. Instability events were diagnosed by history, physical examination by a single sports medicine trained orthopedic surgeon, who was blinded to all baseline data, and MR imaging after the injury. Anterior instability events were defined as painful shoulder injuries resulting in a sensation of instability, with or without the need for manual reduction by a health care professional, and associated with physical examination findings of anterior apprehension, a load-shift test revealing pathologic anterior translation, and/or symptom relief with relocation test [20, 25]. Posterior instability events were diagnosed with a painful shoulder injury with sensation of instability, a history of pain with push-ups, a positive posterior apprehension test, and a posterior labral tear on subsequent MRI [18].
For continuous variables, we used independent t tests to examine differences between those with posterior chondrolabral clefts and those without, as well as differences between those that suffered acute shoulder instability injuries and those that did not. For categorical variables, we examined associations between the variables and shoulder instability during the follow-up period using the Pearson chi-square or Fisher’s exact test. Univariate and multivariate Cox proportional hazards regression models were used to analyze the data. Multivariate models controlled for the influence of both gender and a history of instability. All analyses were performed using Stata SE version 10.1.
Results
There were 114/1,264 shoulders with a posterior chondrolabral cleft (9%). These involved the right shoulder in 60/114 (52.6%), and the left shoulder in 54/114 (47.4%). There were 40/114 shoulders (35%) in which a posterior chondrolabral cleft was present bilaterally.
Shoulders with posterior chondrolabral clefts were found to commonly have a specific glenoid morphology. A rounded or truncated posterior glenoid rim was present in 25/114 (21.9%) of shoulders with a posterior chondrolabral cleft, and in 18/1,193 (1.5%) of shoulders without a posterior chondrolabral cleft (P < 0.0001). In shoulders with a posterior chondrolabral cleft, the mean glenoid version was 9.5° of retroversion (95% confidence interval: 8.3 to 10.7° of retroversion). In shoulders without a posterior chondrolabral cleft, the mean glenoid version was 7.7° of retroversion (95% confidence interval: 7.4 to 8.0° of retroversion) [P(|T| > |t|) = 0.0056; P(T > t) = 0.006]. In shoulders with a posterior chondrolabral cleft, the mean glenoid depth was 6.40 mm (95% confidence interval: 6.1–6.7 mm), while in shoulders without a posterior chondrolabral cleft, the mean glenoid depth was 6.36 mm (95% confidence interval: 6.3–6.4 mm; P = 0.606).
The presence of a chondrolabral cleft was associated with a greater incidence of anterior shoulder instability. A history of prior shoulder instability was found in 16/114 (14%) of shoulders with a posterior chondrolabral cleft, and in 93/1,148 (8.1%) without a posterior chondrolabral cleft (P = 0.018). During the 4-year follow-up period, there were 46 acute glenohumeral instability injuries in the study cohort, of which 39/46 (84.8%) were anterior and 7/46 (15.2%) were posterior. An acute instability event (in any direction) occurred in 9/114 (7.9%) of shoulders with a posterior chondrolabral cleft, and in 37/1,194 (3.1%) of shoulders without a posterior chondrolabral cleft (P = 0.005). Focusing only on anterior instability, an acute anterior shoulder instability injury occurred in 9/114 (7.9%) of shoulders with a posterior chondrolabral cleft, and in 30/1,187 (2.5%) of shoulders without a posterior chondrolabral cleft (P = 0.001). No shoulders with a posterior chondrolabral cleft developed a posterior instability event, while 7/1,166 (0.6%) of shoulders without a posterior chondrolabral cleft developed a posterior instability event (P = 0.428). Since shoulder instability injuries are commonly recurrent [19], we also isolated those shoulders without any history of prior instability to see if there was a relationship with posterior chondrolabral clefts. Excluding shoulders with a history of prior instability, acute anterior instability occurred in 6/97 (6.2%) of shoulders with a posterior chondrolabral cleft, and in 19/1,096 (1.7%) of shoulders without a posterior chondrolabral cleft (P = 0.003). Using a Cox regression analysis, hazard ratio was 3.5 for the development of instability in shoulders with a posterior chondrolabral cleft (95% confidence interval 1.54–9.21). Controlling for both gender and a history of prior shoulder instability, hazard ratio (HR) was 2.8 for development of instability in shoulders with a posterior chondrolabral cleft (95% confidence interval 1.04–7.61).
Discussion
This was a prospective cohort study to determine if posterior chondrolabral clefts were associated with variations in glenoid morphology, and to determine if they were associated with glenohumeral instability. We found that posterior chondrolabral clefts were significantly associated with a rounded or truncated posterior glenoid rim and a small but significant increase in glenoid retroversion. Also, posterior chondrolabral clefts were significantly associated with anterior glenohumeral instability.
This study had limitations. The MR imaging examinations used in this study were neither MR arthrograms nor optimized high-resolution studies. This may lead to a bias in our data toward larger clefts. When compared to the prevalence of posterior chondrolabral clefts in our study cohort (9%), the high prevalence of small (1 mm) clefts found in other studies [23] suggests that these small or shallow clefts may have been below diagnostic threshold on the MR images used in this study. Also, true axial images of the shoulder were used in this study, as opposed to the oblique axial images used in some other studies [23]. This may lead our data to be biased toward the posterior and posteroinferior quadrants. It is interesting to note that the prevalence of labral clefts within the posterior or posteroinferior quadrants in other studies [23] was similar to that found in our population. In addition, in our MRI interpretations, we attempted to distinguish labral tears from chondrolabral clefts using established criteria for labral tears [9, 10, 12, 16, 22]. However, as other authors [10] have demonstrated, there may be overlap between the imaging appearances of labral tears and clefts. Since surgical correlation was not available in these predominantly asymptomatic subjects, there is no way to be certain that each lesion was actually a cleft, rather than a tear. Another limitation was the interpretation of the MRI examinations by a single observer. However, high interobserver and intraobserver reliability have been previously shown using established measurement methods for glenoid version [13, 17], and posteroinferior labral clefts [10].
In young subjects, posterior chondrolabral clefts are not uncommon (9% in our series), occurring with nearly equal frequency in right and left shoulders. This finding was similar to other studies in which no significant laterality was observed [10, 23]. Posterior clefts are commonly bilateral (35%).
Prior studies have not attempted to identify an association of posterior labral clefts with variations in glenoid morphology. In our study, shoulders with posterior chondrolabral clefts were significantly more likely to have a rounded or truncated posterior glenoid rim. Also, a mild but significant increase in glenoid retroversion was observed in shoulders with posterior chondrolabral clefts. This morphology is in the spectrum of mild glenoid hypoplasia. There was no significant association with glenoid depth.
No prior study has attempted to evaluate for an association of posterior chondrolabral clefts with glenohumeral instability. We found the MRI finding of a posterior chondrolabral cleft to be associated with an increased risk for anterior shoulder instability. Even when controlling for a history of prior instability, shoulders with a posterior chondrolabral cleft on initial MRI were significantly more likely to develop anterior instability during the 4-year follow-up period in our study. It is not obvious why these clefts would be associated with anterior shoulder instability. One possible explanation is that the underlying glenoid morphology may increase the degree of glenohumeral translation, even in the extremes of shoulder motion. It is well known that active glenohumeral stabilization from concavity compression occurs in the mid-range of shoulder motion as a result of muscle contraction [3, 14]. Instability in this range can result from a number of factors, a few of which are decreased articular concavity [14], increased glenoid retroversion [8], decreased anteroposterior glenoid width [1], or a hypoplastic posteroinferior glenoid rim [4, 7, 8]. In extremes of motion, the glenohumeral ligaments are thought to be the dominant factors in shoulder stability [1, 2]. Yet compression from muscle contraction has been shown to be an important stabilization factor in high degrees of shoulder motion as well [11, 24]. It is possible that the glenoid morphological variations seen in our cohort may decrease concavity compression even in extremes of shoulder motion. Another possibility is that the presence of a chondrolabral cleft may decrease the degree of negative intraarticular pressure, which has been shown to reduce the force required to subluxate the humeral head from the glenoid fossa [5]. This is likely a lesser factor than compression due to muscle contraction [24]. Further studies are needed to shed light on the biomechanical properties associated with this anatomy.
It is reasonable to consider that the posterior chondrolabral clefts identified in this series may include a combination of traumatic and developmental lesions. A history of prior shoulder instability was found in 14% of shoulders with a posterior chondrolabral cleft, suggesting a traumatic origin for the MRI finding in some cases. On the other hand, the significant association with a rounded or truncated posterior glenoid rim, the prevalence in a cohort of young adults, and the common presence in bilateral shoulders support a developmental origin.
In conclusion, high signal intensity clefts at the posterior chondrolabral junction are associated with a rounded or truncated posterior glenoid rim and a small but significantly increased degree of glenoid retroversion. They are associated with anterior shoulder instability.
Electronic supplementary material
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
Acknowledgments
Disclosures
ᅟ
Conflict of Interest:
Scot E. Campbell, MD, Robert M. Dewitt, MD, MPH, ATC, and Adrianne K. Thompson, MD have declared that they have no conflict of interest. Kenneth L Cameron, PhD reports grants from Orthopedic Research and Education Foundation, during the study. Brett D. Owens, MD reports grants from OREF, during the conduct of the study; personal fees from Mitek Sports Medicine and Musculoskeletal Transplant Foundation, outside the work.
Human/Animal Rights:
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 [5].
Informed Consent:
Informed consent was obtained from all patients for being included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Level IV: Cohort study.
The views and opinions expressed in this manuscript are those of the author(s) and do not reflect the official policy of the Department of the Army, the US Air Force, the Department of Defense, or the US Government.
References
- 1.Bigliani LU, Kelkar R, Flatow EL, Pollock RG, Mow VC. Glenohumeral stability. Biomechanical properties of passive and active stabilizers. Clin Orthop Relat Res. 1996;330:13–30. doi: 10.1097/00003086-199609000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Blasier RB, Guldberg RE, Rothman ED. Anterior shoulder stability: contributions of rotator cuff forces and capsular ligaments in a cadaver model. J Shoulder Elbow Surg. 1992;1:140–150. doi: 10.1016/1058-2746(92)90091-G. [DOI] [PubMed] [Google Scholar]
- 3.Cooper DE, Arnoczky SP, O’Brien SJ, Warren RF, DiCarlo E, Allen AA. Anatomy, histology, and vascularity of the glenoid labrum. J Bone Joint Surg Am. 1992;74A(1):46–52. [PubMed] [Google Scholar]
- 4.Edelson JG. Localized glenoid hypoplasia: an anatomic variation of possible clinical significance. Clin Orthop Relat Res. 1995;321:189–195. [PubMed] [Google Scholar]
- 5.Gibb TD, Sidles JA, Harryman DT, McQuade KJ, Matsen FA., III The effect of capsular venting on glenohumeral laxity. Clin Orthop. 1991;268:120–127. [PubMed] [Google Scholar]
- 6.Harper KW, Helms CA, Haystead CM, Higgins LD. Glenoid dysplasia: incidence and association with posterior labral tears as evaluated by MRI. Am J Roentgenol. 2005;184:984–988. doi: 10.2214/ajr.184.3.01840984. [DOI] [PubMed] [Google Scholar]
- 7.Ikeda H, Tsukanishi S, Nobuhara K. Shoulder instability: its relationship to glenoid dysplasia. Seikeisaigaigeka. 1984;27:1757–1765. [Google Scholar]
- 8.Inui H, Sugamoto K, Miyamoto T, et al. Glenoid shape in atraumatic posterior instability of the shoulder. Clin Orthop. 2002;403:87–92. doi: 10.1097/00003086-200210000-00014. [DOI] [PubMed] [Google Scholar]
- 9.Kim SH, Ha KI, Yoo JC, Noh KC. Kim’s lesion: an incomplete and concealed avulsion of the posteroinferior labrum in posterior or multidirectional posteroinferior instability of the shoulder. Arthroscopy. 2004;20:712–720. doi: 10.1016/j.arthro.2004.06.012. [DOI] [PubMed] [Google Scholar]
- 10.Lee GY, Choi JA, Oh JH, Choi JH, Hong SH, Kang HS. Posteroinferior labral cleft at direct CT arthrography of the shoulder by using multidetector CT: is this a normal variant? Radiology. 2009;253:765–770. doi: 10.1148/radiol.2533081997. [DOI] [PubMed] [Google Scholar]
- 11.Lee SB, Kim KJ, O'Driscoll SW, Morrey BF, An KN. Dynamic glenohumeral stability provided by the rotator cuff muscles in the mid-range and end-range of motion. A study in cadavera. J Bone Joint Surg Am. 2000;82(6):849–857. doi: 10.2106/00004623-200006000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Legan JM, Burkhard TK, Goff WB, II, et al. Tears of the glenoid labrum: MR imaging of 88 arthroscopically confirmed cases. Radiology. 1991;179:241–246. doi: 10.1148/radiology.179.1.2006284. [DOI] [PubMed] [Google Scholar]
- 13.Lippert WC, Mahlman CT, Cornwall R, et al. The intrarater and interrater reliability of glenoid version and glenohumeral subluxation measurements in neonatal brachial plexus palsy. J Pediatr Orthop. 2012;32(4):378–384. doi: 10.1097/BPO.0b013e31825611bd. [DOI] [PubMed] [Google Scholar]
- 14.Lippitt WB, Vanderhooft JE, Harris SL, Sidles JA, Harryman DT, Matsen FA., III Glenohumeral stability from concavity-compression: a quantitative analysis. J Shoulder Elbow Surg. 1993;2:27–35. doi: 10.1016/S1058-2746(09)80134-1. [DOI] [PubMed] [Google Scholar]
- 15.Mallon WJ, Brown HR, Vogler JB, Martinez S. Radiographic and geometric anatomy of the scapula. Clin Orthop Relat Res. 1992;277:142–154. [PubMed] [Google Scholar]
- 16.Mohana-Borges AV, Chung CB, Resnick D. Superior labral anteroposterior tear: classification and diagnosis on MRI and MR arthrography. Am J Roentgenol. 2003;181:1449–1462. doi: 10.2214/ajr.181.6.1811449. [DOI] [PubMed] [Google Scholar]
- 17.Nyffeler RW, Jost B, Pfirrmann CWA, Gerber C. Measurement of glenoid version: conventional radiographs versus computed tomography scans. J Shoulder Elbow Surg. 2003;12(5):493–496. doi: 10.1016/S1058-2746(03)00181-2. [DOI] [PubMed] [Google Scholar]
- 18.Owens BD, Campbell SE, Cameron KL. Risk factors for posterior shoulder instability in young athletes. Am J Sports Med. 2013;41:2645–2649. doi: 10.1177/0363546513501508. [DOI] [PubMed] [Google Scholar]
- 19.Owens BD, Duffey ML, Nelson BJ, DeBerardino TM, Taylor DC, Mountcastle SB. The incidence and characteristics of shoulder instability at the United States Military Academy. Am J Sports Med. 2007;35(7):1168-73. [DOI] [PubMed]
- 20.Owens BD, Nelson BJ, Duffey ML, et al. Pathoanatomy of first-time, traumatic, anterior glenohumeral subluxation events. J Bone Joint Surg Am. 2010;92:1605–1611. doi: 10.2106/JBJS.I.00851. [DOI] [PubMed] [Google Scholar]
- 21.Randelli M, Gambrioli PL. Glenohumeral osteometry by computed tomography in normal and unstable shoulder. Clin Orthop Rel Res. 1986;208:151–156. [PubMed] [Google Scholar]
- 22.Snyder SJ, Karzel RP, Del Pizzo W, et al. SLAP lesions of the shoulder. Arthroscopy. 1990;6:274–279. doi: 10.1016/0749-8063(90)90056-J. [DOI] [PubMed] [Google Scholar]
- 23.Tuite MJ, Currie JW, Orwin JF, Baer GS, Munoz del Rio A. Sublabral clefts and recesses in the anterior, inferior, and posterior glenoid labrum at MR arthrography. Skeletal Radiol 2012. doi:10.1007/s10639-014-9333-9. [DOI] [PubMed]
- 24.Warner JJ, Bowen MK, Deng X, Torzilli PA, Warren RF. Effect of joint compression on inferior stability of the glenohumeral joint. J Shoulder Elbow Surg. 1999;8(1):31–36. doi: 10.1016/S1058-2746(99)90051-4. [DOI] [PubMed] [Google Scholar]
- 25.Warren RF. Subluxation of the shoulder in athletes. Clin Sports Med. 1983;2(2):339–354. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)