Introduction
Lesions of the long head of the biceps (LHB) tendon linked with rotator cuff tears can be responsible for considerable shoulder pain and dysfunction [10]. The two most commonly performed procedures for biceps pathology by orthopedic surgeons today are arthroscopic biceps tenotomy and tenodesis. Although the optimal surgical procedure is controversial, there is considerable agreement that operative treatment provides significant pain relief, with no major functional impairment [4]. While ultrasound-guided percutaneous tenotomy of the LHB tendon has been reported in cadavers [7], to our knowledge, no one has successfully reported the procedure in a patient. In the ever-changing health care environment, a less invasive procedure that can be performed without the risks and costs of anesthesia and surgery could be of great benefit. This is particularly important for patients who are not ideal surgical candidates due to comorbid conditions (i.e., cardiac disease, pulmonary insufficiency).
Case Report
A 59-year-old male, status-post rotator cuff repair in 2010, presented with “horrific” pain in the right arm along the route of the proximal LHB tendon. The pain became progressively worse over the prior month despite prior ultrasound-guided steroid and anesthetic mixture injections into his right glenohumeral joint and biceps tendon sheath at our clinic approximately 3 months prior. The patient was participating in physical therapy twice a week.
The physical examination was relevant for active range of motion from 0–90° in abduction and forward flexion. External rotation was 0–20° with limited internal range of motion. Passive range of motion was 0–100° in abduction and forward flexion. External rotation was 0–40°, and internal rotation was limited by pain. There was tenderness to palpation at the right upper arm along the biceps tendon, which he rated 10 out of 10. There was a positive Speed’s test, pain with O’Brien’s test, and equivocal impingement signs.
Postoperative MRI of the right shoulder at the patient’s initial presentation to our clinic showed bicipital tendinosis and tenosynovitis, without tendon tear (Fig. 1). Diagnostic ultrasound performed approximately 1 year later revealed persistent long head of the biceps tendinosis with tenosynovitis (Fig. 2).
Fig. 1.
Axial proton density (a), and T2 fat suppressed (b, c, d) images of the right shoulder demonstrate long head of the biceps tendinosis and fraying more proximally (closed arrows), with reactive tenosynovitis more distally (open arrows).
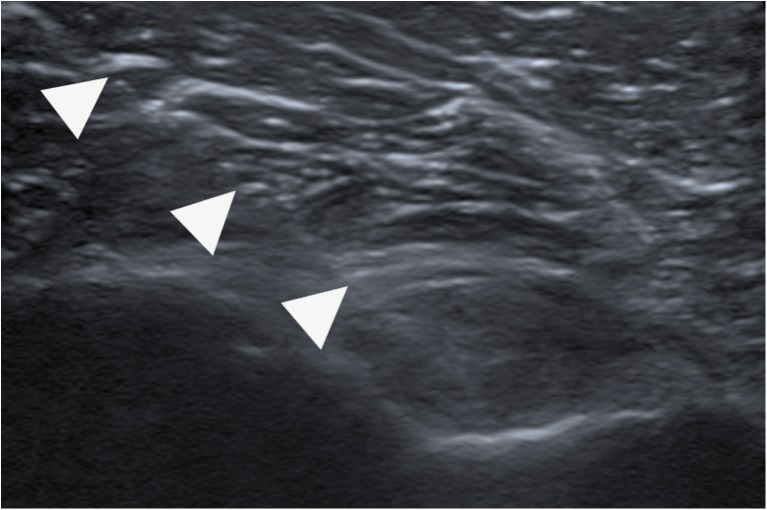
Fig. 2.
Short-axis (transverse) gray scale ultrasound images (a, b) show long head of the biceps tendinosis more proximally (closed arrows), with reactive tenosynovitis more distally (open arrows). The long head of the biceps tendon is enlarged and hypoechoic in a, and surrounded by fluid in b.
Since his initial presentation to our clinic, the pain in his biceps had become significantly worse and was now waking him up at night. The patient was not a reasonable surgical candidate due to his recent cervical fusion and a high risk cardiovascular profile. Instead, we offered the patient the option of a less invasive technique for relieving his pain.
Sonographic Technique and Injection Materials
We perfected the sonographic technique of percutaneous LHB tenotomy by practicing in our lab on cadaveric shoulders. After performing each tenotomy, careful open dissection of the shoulder specimen was done to ensure there was no harm to the subscapularis or pectoralis major tendon (Fig. 3).
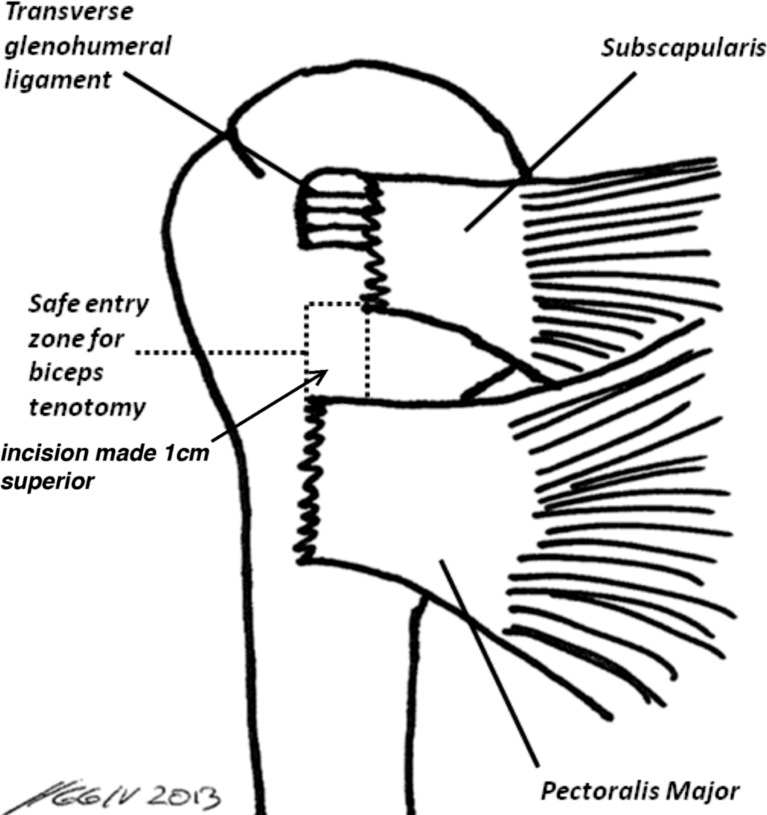
Fig. 3.
Cadaver shoulder status-post ultrasound-guided LHB tenotomy. Careful dissection demonstrated an intact subscapularis tendon (arrow).
Ultrasound confirmed the diagnosis of a LHB tendinopathy and provided guidance for tenotomy and subsequent steroid injection. Scans were performed with a 12- to 5-Mhz linear transducer on an IU22 scanner (Philips Medical Systems, Bothell, WA, USA).
In the ultrasound suite, the musculoskeletal radiologist and assisting ultrasound technician placed the patient in a supine position, with the scan plane corresponding to the anatomic axial (transverse) plane, in order to facilitate needle guidance. The skin was prepped and draped in the usual sterile fashion utilizing Betadine solution (Purdue Pharma, Stamford, CT, USA), and the procedure performed with a sterile gel (Acquasonic 100 ultrasound transmission gel, Parker laboratories, Fairfield, NJ, USA) and a sterile probe cover (48-in. site rite ultrasound probe sheath, Bard Access Systems Inc., Salt Lake City, UT, USA). The transducer was placed along the anterior aspect of the right arm, over the area of the long head of the biceps. Under ultrasound guidance, a location on the skin that was inferior to the transverse humeral ligament and approximately 1 cm superior to the superior border of the pectoralis major tendon humeral insertion was marked in the arm (Fig. 4). Local anesthesia was obtained, under sterile technique, with injection of 1% lidocaine through a 22-gauge, 3.5-in. spinal needle into the subcutaneous tissues and long head of the biceps tendon sheath (Fig. 5). A 0.5-cm incision with a number 10 scalpel was then made superficially along the needle track. With the transducer in the transverse plane, a 3.0-mm Acufex hook knife (Smith & Nephew, London, England) was subsequently percutaneously introduced into the long head of the biceps tendon sheath from a lateral approach. The tip of the hook knife was placed between the bone and the LHB tendon (Fig. 6a, b). Once proper knife position was assured sonographically, the sharp end of the cutting shaft was pulled through the tendon using the device handle until resistance was no longer felt. Three passes with the hook knife inside the tendon sheath were necessary to completely release the tendon, and this was confirmed sonographically by noting a fluid gap between the severed tendon ends. Subsequently, the tendon sheath was infiltrated with a mixture containing 1.0 ml Kenalog (40 mg/ml) triamcinolone (Kenalog; Apothecon, Bristol-Myers Squibb Company, Princeton, NJ, USA) and 0.5 ml of 0.2% Naropin (ropivacaine HCL; AstraZeneca Pharmaceuticals LP, Wilmington, DE, USA) delivered through a 22-gauge, 3.5-in. spinal needle. LHB percutaneous tenotomy, without sonographic evidence of injury to the subscapularis and pectoralis tendons was considered the short-term determining factor for a successful completion of the procedure (Fig. 7).
Fig. 4.
Demonstration of the location of skin anesthesia and safe entry site for the LHB tenotomy.
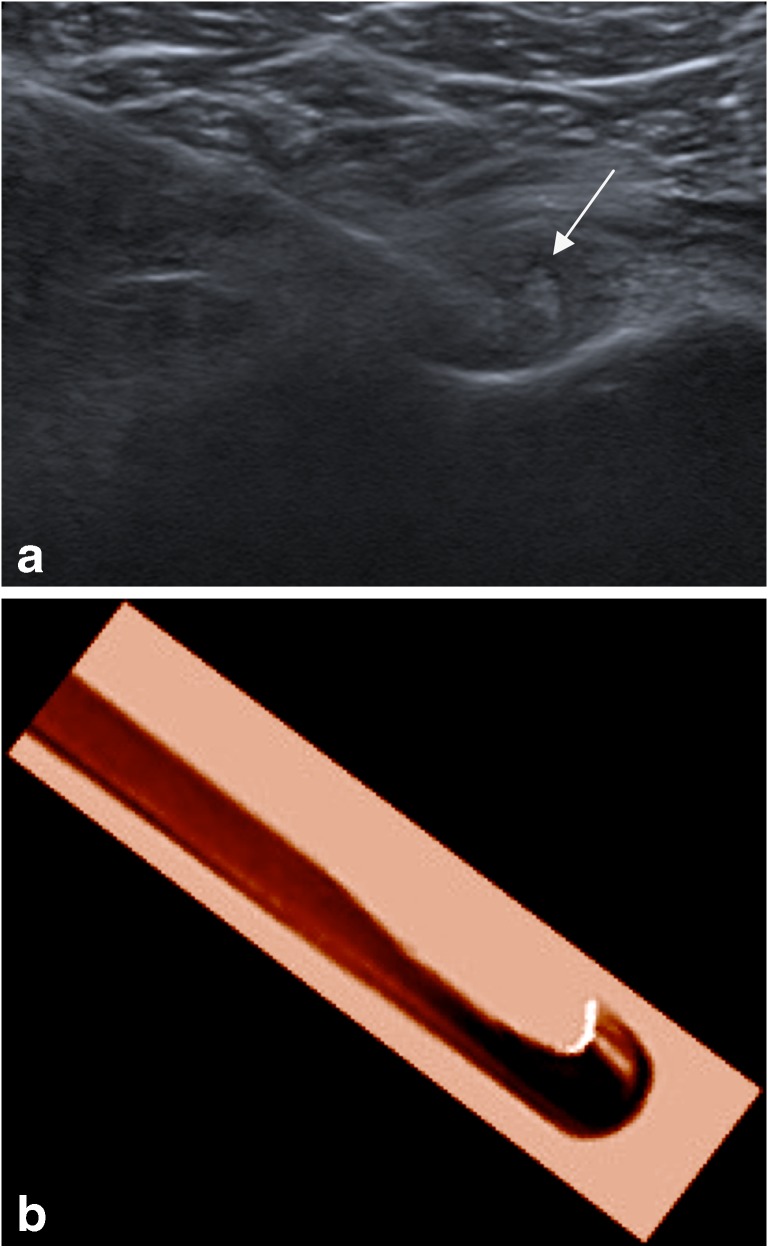
Fig. 5.
Partial-thickness long head of biceps brachii tendon tear. Short-axis ultrasound image shows spinal needle (arrow) infiltrating area with anesthetic.
Fig. 6.
a Short-axis ultrasound image shows arthroscopic hook knife (arrow) severing the long head of biceps tendon. b Short-axis view shows the 3.0-mm trigger finger release hook knife.
Fig. 7.
Long-axis ultrasound image shows the severed (arrow) long head of biceps tendon status-post tenotomy.
Results
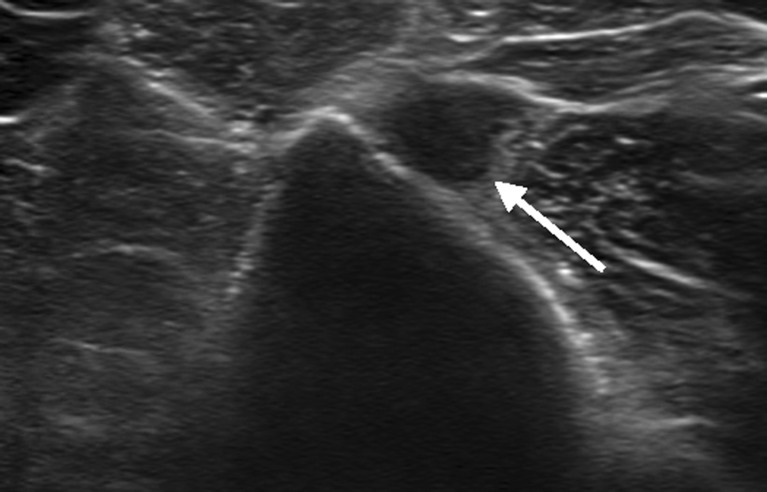
Fifteen months following the procedure, the patient rated his right arm pain as 0 out of 10. Active and passive range of motion extended from 0–120° in both forward flexion and abduction. No tenderness to palpation at the right shoulder was elicited during the examination. There were negative Speed’s and O’Brien’s tests. The patient stated that he had been able to return to his normal level of activity. Cosmetically, there was evidence of a Popeye deformity. Follow-up sonographic images demonstrated an empty long head of the biceps tendon sheath, reflecting complete tendon rupture (Fig. 8). The proximal tendon stump was still present within the biceps proximal groove, without intra-articular displacement.
Fig. 8.
Diagnostic ultrasound of the shoulder performed at 15-month follow-up showed “empty bicipital groove” (arrow), reflecting successful long head of the biceps tenotomy. The pectoralis tendon and subscapularis tendons were intact (not shown).
Discussion
The most significant finding of our case study is the promise of a safe and minimally invasive technique for biceps tenotomy in patients who are not ideal surgical candidates. The critical step in the procedure is an entry window that is inferior to the transverse humeral ligament/subscapularis tendon and superior to the attachment of the pectoralis major tendon into the humerus. Additionally, we have found that the use of an arthroscopic hook knife is an effective way to sever the LHB tendon.
Operative management for LHB disorders includes tendon debridement, transfer, repair of partial tears, and reconstruction of the damaged pulley; however, tenotomy and tenodesis are the most common surgical choices [9]. There remains great controversy in the orthopedic literature regarding relative efficacy of the two procedures. In a large retrospective study by Delle Rose et al. [2], 104 patients who underwent either arthroscopic tenotomy or tenodesis were observed. Probably the most significant finding of the study was the clinical scores improved in both groups as well as similar range of motion. Additionally, the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire revealed that patients in both groups were satisfied with the procedure. The presence of a Popeye deformity was 37.5% in the tenotomy group compared to 5.3% of the tenodesis group.
However, arthroscopic LHB tenotomy is a relatively quick and simple procedure with a brisk rehabilitation period when compared to tenodesis [2]. Additionally, the recent success with professional football quarterbacks has spiked interest in this alternative [3]. Still due to the relatively high rate of Popeye deformity resulting from tenotomy, biceps tenodesis is usually still recommended for younger individuals and women for cosmetic reasons.
Indication for biceps tenotomy or tenodesis is persistent pain with a rotator cuff tear after conservative treatment has failed [1]. However, tenotomy or tenodesis is contraindicated in patients with a rotator cuff tear and evidence of pseudoparalysis in spite of rehabilitation. These patients should accordingly be treated with reverse shoulder arthroplasty [1, 5]. Additionally, tenotomy or tenodesis is contraindicated in patients with glenohumeral osteoarthritis or humeral head necrosis (stage 4 or 5) [6, 8, 11].
Complication rates are similar between the two procedures; patients undergoing tenodesis generally report higher rates of postoperative bicipital pain than those undergoing tenotomy. Contrarily, the incidence of postoperative biceps deformity is seen primarily in patients undergoing tenotomy and occurs in approximately 45% of cases [8]. Otherwise, the risks of arthroscopic biceps tenotomy are the same as the risks during shoulder arthroscopy, including anesthesia-induced injuries, neurovascular injuries, upper extremity deep venous thrombosis, brachial plexus traction injuries, and cartilage damage [6].
Regarding ultrasound-guided LHB tenotomy, no patient cases have been documented (to the authors knowledge) until the current study. The number one limitation of the procedure is the inability to remove or debride the proximal LHB stump. The potential consequence of which the stump can become locked in the biceps sheath causing pain. In this situation, surgical tenotomy would need to be performed to ensure complete removal. Thus, our procedure is potentially inferior to arthroscopic LHB tenotomy, and it is recommended that this is reserved for non-operative candidates. Given this is the lone report of this procedure on a live patient, we are unable to predict what the consequences of leaving the proximal long head of the biceps tendon stump. There is a possibility of the stump becoming a mechanical obstruction in the glenohumeral joint; however, our patient had no complaints to lead us to believe that this had occurred at 15 months, and follow-up ultrasound images did not demonstrate this. Previous studies have evaluated the feasibility of this procedure with cadaver specimens and were complicated by partial sectioning of the subscapularis as well as lacerations of the humeral head cartilage [7]. We believe that using our procedure window described above significantly limits the aforementioned complications. Additionally, our technique uses an endoscopic release hook needle compared to the size 11 scalpel used in the study by Levy et al. We believe this tool/technique is not only safe but is more effective in severing the tendon than the abovementioned scalpel.
Our report of an ultrasound-guided biceps tenotomy illustrates a potentially minimally invasive and safe treatment of LHB pathology for patients who are not surgical candidates. However, longer-term follow-up studies, preferably with a large number of subjects, are necessary to determine the efficacy of the procedure.
Electronic supplementary material
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
Acknowledgments
Disclosures
ᅟ
Conflict of Interest:
Harry G. Greditzer IV, MD, Jean Jose, DO, Lee D. Kaplan, MD, Bryson P. Lesniak, MD have declared that they have no conflict of interest.
Human/Animal Rights:
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed Consent:
Informed consent was waived from all patients for being included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Work performed at: UHealth Sports Performance and Wellness Institute; Department of Orthopaedics, University of Miami Miller School of Medicine, Miami, FL.
References
- 1.Boileau P, Watkinson DJ, Hatzidakis AM, et al. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005;14:147S–161S. doi: 10.1016/j.jse.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 2.Delle Rose G, Borroni M, Silvestro A, et al. The long head of biceps as a source of pain in active population: tenotomy or tenodesis? A comparison of 2 case series with isolated lesions. Musculoskelet Surg. 2012;96(1):S47–S52. doi: 10.1007/s12306-012-0189-0. [DOI] [PubMed] [Google Scholar]
- 3.Dodd M. For pitchers, shoulder surgery cuts both ways. USA Today, Gannett Co., Inc.;2010. Retrieved from http://www.usatoday30.usatoday.com/sports/baseball/2010-11-16-shoulder_N.html
- 4.Frost A, Zafar MS, Maffulli N. Tenotomy versus tenodesis in the management of pathologic lesions of the tendon of the long head of the biceps brachii. Am J Sports Med. 2009;37(4):828–833. doi: 10.1177/0363546508322179. [DOI] [PubMed] [Google Scholar]
- 5.Grammont PM, Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics. 1993;16:65–68. doi: 10.3928/0147-7447-19930101-11. [DOI] [PubMed] [Google Scholar]
- 6.Johnson DH, Pedowitz RA. Practical Orthopaedic Sports Medicine and Arthroscopy. 1. Philadelphia: Lippincott Williams & Wilkins; 2007. [Google Scholar]
- 7.Levy B, Ducat A, Gaudin P, et al. Ultrasound-guided percutaneous tenotomy of the long head of the biceps tendon: a non-reliable technique. Knee Surg Sports Traumatol Arthrosc. 2012;20:1027–1030. doi: 10.1007/s00167-011-1671-1. [DOI] [PubMed] [Google Scholar]
- 8.Lim TK, Moon ES, Koh KH, et al. Patient-related factors and complications after arthroscopic tenotomy of the long head of the biceps tendon. Am J Sports Med. 2011;39:783–789. doi: 10.1177/0363546510388158. [DOI] [PubMed] [Google Scholar]
- 9.Narvani AA, Atoun E, Tongel AV, et al. The “Anchor Shape” technique for long head of the biceps tenotomy to avoid the popeye deformity. Arthrosc Tech. 2013;2(2):e167–e170. doi: 10.1016/j.eats.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Szabo I, Boileau P, Walch G. The proximal biceps as a pain generator and results of tenotomy. Sports Med Arthrosc Rev. 2008;16:180–186. doi: 10.1097/JSA.0b013e3181824f1e. [DOI] [PubMed] [Google Scholar]
- 11.Werner CM, Steinmann PA, Gilbart M, et al. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the delta III Reverse-Balland-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005;87:1476–1486. doi: 10.2106/JBJS.D.02342. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)