Abstract
Background
People with schizophrenia and severe mental illness may require considerable support from health care professionals, in most cases over a long period of time. Research on the effects of psychotherapy for schizophrenia has shown mixed results. Although pharmacological interventions remain the treatment of choice, the effects of treatments focusing on psychosocial factors affecting schizophrenia are important.
Objectives
To review the effects of psychodynamic psychotherapy, psychoanalysis, or both, for people with schizophrenia or severe mental illness.
Search methods
For the updated review, we searched the Cochrane Schizophrenia Group Trials Register (June 2008) which is based on regular searches of BIOSIS, CENTRAL, CINAHL, EMBASE, MEDLINE and PsycINFO.
Selection criteria
We sought all randomised trials of individual psychodynamic psychotherapy or psychoanalysis for people with schizophrenia or severe mental illness.
Data collection and analysis
We extracted data independently. For dichotomous data we calculated relative risks (RR) and their 95% confidence intervals (CI) on an intention‐to‐treat basis using a fixed‐effect model. We calculated numbers needed to treat/harm (NNT/NNH) where appropriate. For continuous data, we calculated mean differences (MD) and weighted mean differences (WMD) using a fixed‐effect model.
Main results
We included four randomised trials (total 528 participants, 5 comparisons). All used a psychodynamic approach and reported limited data.
For individual psychodynamic therapy versus medication alone we found significantly more participants in the therapy group were unable to be discharged (n=92, RR 8.35 CI 2.0 to 34.3, NNH 3 CI 2 to 6). We found no significant difference between groups in the number of participants who were re‐hospitalised (n=24, RR 0.63 CI 0.3 to 1.4) during long‐term analyses. At 12 months, fewer participants in the psychotherapy groups needed additional medications compared with those who did receive medication (n=74, RR 0.64 CI 0.5 to 0.8, NNT 3 CI 3 to 6), and also at three years follow up (n=87, RR 0.85 CI 0.8 to 1.0, NNT 7 CI 5 to 26).
For individual psychodynamic therapy plus medication versus medication alone we found no significant difference in suicide (n=92, RR 0.16 CI 0.01 to 2.9) or suitability for discharge (n=92, RR 1.09 CI 0.2 to 7.4). Also, we found re‐hospitalisation rates in long‐term analyses were equivocal (n=24, RR 1.00 CI 0.4 to 2.6). For insight‐orientated psychodynamic psychotherapy versus reality adaptive psychotherapy we found no significant difference in re‐hospitalisation rates (n=164, RR 1.20 CI 0.9 to 1.6), but we found study attrition favoured the insight‐orientated psychodynamic psychotherapy group at 12 months (n=164, RR 0.46 CI 0.3 to 0.6, NNT 2 CI 2 to 4). For individual psychodynamic psychotherapy versus group psychotherapy we found no significant difference in global state 'not improved' (n=100, RR 1.27 CI 1.0 to 1.7). For individual psychodynamic therapy plus medication versus individual psychodynamic therapy we found rates of re‐hospitalisation during long‐term analyses were equivocal (n=24, RR 1.00 CI 0.4 to 2.6). There is no clear evidence of any positive effect of psychodynamic therapy and the possibility of adverse effects seems never to have been considered. We did not identify any trials using a psychoanalytic approach.
Authors' conclusions
Current data do not support the use of psychodynamic psychotherapy techniques for hospitalised people with schizophrenia. If psychoanalytic therapy is being used for people with schizophrenia there is an urgent need for trials.
Keywords: Humans, Psychoanalytic Therapy, Psychotherapy, Hospitalization, Mental Disorders, Mental Disorders/therapy, Randomized Controlled Trials as Topic, Schizophrenia, Schizophrenia/therapy
Plain language summary
Individual psychodynamic psychotherapy and psychoanalysis for schizophrenia and severe mental illness
Psychodynamic treatment is an intervention that can be classed as one of the 'talking' therapies. The relationship between the person seeking therapy and the therapist form the main component of the therapy. Its use for people with schizophrenia as a sole treatment, without medication, has not been evaluated very well, apart from four studies in the early 1970s and 1980s. It is clear from the limited studies available that medication is an important part of any treatment for people with psychotic illnesses and should be used in conjunction with any talking treatments.
Summary of findings
Summary of findings for the main comparison. INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY versus MEDICATION for schizophrenia and severe mental illness.
| INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY versus MEDICATION for schizophrenia and severe mental illness | ||||||
| Patient or population: patients with schizophrenia and severe mental illness Settings: in hospital Intervention: INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY versus MEDICATION | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY versus MEDICATION | |||||
| Committed suicide by three years | 42 per 1000 | 22 per 1000 (2 to 234) | RR 0.52 (0.05 to 5.56) | 94 (1 study) | ⊕⊕⊝⊝ low1,2 | |
| Global impression: 1. Not able to be discharged (long term) | 42 per 1000 | 351 per 1000 (85 to 1000) | RR 8.35 (2.03 to 34.3) | 94 (1 study) | ⊕⊕⊝⊝ low1,2 | |
| Global impression: 2. Given medication during 12 months to three years follow up ‐ by 12 months | 958 per 1000 | 613 per 1000 (479 to 776) | RR 0.64 (0.5 to 0.81) | 94 (1 study) | ⊕⊕⊝⊝ low1,2 | |
| Global impression: 2. Given medication during 12 months to three years follow up ‐ by three years | 1000 per 1000 | 850 per 1000 (750 to 960) | RR 0.85 (0.75 to 0.96) | 94 (1 study) | ⊕⊕⊝⊝ low1,2 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Randomisation undertaken but not clearly described. 2 One small single study.
Background
Description of the condition
People with schizophrenia and severe mental illness may require considerable support from health care professionals, in most cases over a long period of time. This support can take many forms including supportive counselling (McIntosh 2006), family interventions (Pharoah 2006), cognitive behavioural approaches (Jones 2004) and psychodynamic psychotherapy (Malmberg 1999). Research on the effectiveness of psychotherapy for schizophrenia shows mixed results (Fenton 1995, Jones 2004). Some investigators promote the use of an integrated model of rehabilitation for people with schizophrenia, where biological, individual psychological, system‐psychological, social and ecological aspects are all taken into account. Treatment of schizophrenia should be based on an understanding of each participant's needs and make further psychological development possible through interactive relations (Alanen 1997).
Description of the intervention
In recent years, biological theories of schizophrenia have been supported by brain imaging techniques (Lawrie 1998). Medications such as clozapine and new atypical antipsychotic drugs have found their place in reducing psychotic symptoms (Duggan 2005, Essali 2009, Hunter 2003). Although antipsychotic drugs remain a treatment of choice for most people with schizophrenia, it is also of interest to look at the effects of treatment methods focusing on psychosocial factors affecting schizophrenia.
How the intervention might work
Psychoanalysis is not a completely integrated and consistent system of thought ‐ although it is often regarded as such. Psychoanalytic concepts are not all well defined and changes in meaning have occurred as psychoanalysis has changed and theory developed. Psychoanalysis developed to a very great extent in and through the work of Sigmund Freud (1856‐1939) but during the course of its evolution Freud himself modified his formulations many times, revising concepts and adding new dimensions to technical procedures (Sandler 1992). In the modern era the term psychoanalysis is considered to mean a method of eliciting from patients their past emotional experiences and their role in influencing their current mental life. This is done in order to discover the conflicts and mechanisms by which their pathologic mental state has been preceded and to furnish hints for psychotherapeutic procedures. The method employs free association, recall and interpretation of dreams and interpretation of transference and resistance phenomena.
Why it is important to do this review
The effects of psychoanalytic techniques for people with schizophrenia and similar mental illnesses has been disputed. However, the use of more flexible techniques, including supportive and directive elements, has led to a reappraisal of individual psychodynamic psychotherapy for schizophrenia (Fenton 1995). In this review we examine the possible effects of individual psychoanalytic psychotherapy or psychoanalysis in treatment of schizophrenia, alone or as a complement to traditional care.
Objectives
To review the effects of individual psychodynamic psychotherapy or psychoanalysis, with or without standard care, in comparison to standard care (antipsychotic drugs, skills training), other psychosocial interventions or no care.
We also proposed to examine if there are differences in response between:
(i) in‐ and outpatients; (ii) participants living alone or with family; (iii) people having their first episode of schizophrenia compared to those whose illness was of longer duration; (iv) strict psychoanalytic techniques and techniques incorporating supportive and directive activity.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials. Where a trial is described as 'double‐blind' but it is only implied that the study is randomised, we included these trials in a sensitivity analysis. If no substantive difference within primary outcomes (see Types of outcome measures) was found when these 'implied randomisation' studies were added then we included these in the final analysis. If there was a substantive difference, we only used clearly randomised trials and described the results of the sensitivity analysis in the text. We excluded quasi‐randomised studies, such as those allocating by using alternate days of the week.
Types of participants
We included people with schizophrenia and other types of schizophrenia‐like psychoses (e.g. schizophreniform and schizoaffective disorders), irrespective of the diagnostic criteria used. There is no clear evidence that the schizophrenia‐like psychoses are caused by fundamentally different disease processes or require different treatment approaches (Carpenter 1994).
Types of interventions
As there could be as many definitions of psychodynamic or psychoanalytic therapy as there are studies, we constructed criteria that were felt to be both workable and to capture the elements of good practice in psychodynamic or psychoanalytic therapy. All interventions that did not meet these criteria but were labelled as 'psychodynamic/analytic therapy' or 'psychoanalysis', were included as 'less well defined' therapies. Where appropriate we performed a sensitivity analysis (see Data Collection and analysis ‐ Sensitivity analysis) in order to investigate if this hierarchy of definition made any difference.
1. Psychodynamic psychotherapy We defined psychodynamic psychotherapy as regular individual therapy sessions with a trained psychotherapist, or a therapist under supervision. Therapy sessions were to be based on a psychodynamic or psychoanalytic model. Sessions could rely on a variety of strategies, including explorative insight‐oriented, supportive or directive activity, applied flexibly. However, therapists should use a less strict technique than in psychoanalysis. To be considered well‐defined psychodynamic psychotherapy, trialists needed to include working with transference.
2. Psychoanalysis We defined psychoanalysis as regular individual sessions, planned to last a minimum of 30 minutes, with a trained psychoanalyst three to five times a week. Additionally psychoanalysis should have been planned to continue for at least one year. Analysts were required to adhere to a strict definition of psychoanalytic technique. To be considered well‐defined psychoanalysis, trialists needed to report working at the infantile sexual relations level of psychoanalytic theory.
3. Standard care The care a person would normally receive had they not been included in the research trial. The category 'standard care' also incorporates 'waiting list control groups' where participants receive drug or other interventions.
4. Other psychosocial therapies Additional psychological and/or social interventions, such as non‐directive counselling, supportive therapy, cognitive‐behavioural therapy and other 'talking therapies'.
5. No care This group included people randomised to no treatment or to a waiting list without receiving any care.
Types of outcome measures
Where possible, we grouped outcomes into the following time periods: 1 to 6 months (short term), 7 to 12 months (medium term), and more than 12 months (long term).
Primary outcomes
1. No clinically important response as defined by the individual studies (e.g. global impression less than much improved or less than 50% reduction on a rating scale).
Secondary outcomes
1. Leaving the studies early (any reason, adverse effects, inefficacy of treatment)
2. Global state 2.1 No clinically important change in global state (as defined by individual studies) 2.2 Relapse (as defined by the individual studies)
3. Mental state (with particular reference to the positive and negative symptoms of schizophrenia) 3.1 No clinically important change in general mental state score 3.2 Average endpoint general mental state score 3.3 Average change in general mental state score 3.4 No clinically important change in specific symptoms (positive symptoms of schizophrenia, negative symptoms of schizophrenia) 3.5 Average endpoint specific symptom score 3.6 Average change in specific symptom score
4. General functioning 4.1 No clinically important change in general functioning 4.2 Average endpoint general functioning score 4.3 Average change in general functioning score
5. Quality of life/satisfaction with treatment 5.1 No clinically important change in general quality of life 5.2 Average endpoint general quality of life score 5.3 Average change in general quality of life score
6. Cognitive functioning 6.1 No clinically important change in overall cognitive functioning 6.2 Average endpoint of overall cognitive functioning score 6.3 Average change of overall cognitive functioning score
7. Service use 7.1 Number of participants hospitalised
8. Adverse effects 8.1 Number of participants with at least one adverse effect 8.2 Clinically important specific adverse effects (cardiac effects, death, movement disorders, prolactin increase and associated effects, weight gain, effects on white blood cell count) 8.3 Average endpoint in specific adverse effects 8.4 Average change in specific adverse effects
Search methods for identification of studies
Electronic searches
1. Update search We searched the Cochrane Schizophrenia Group Trials Register (June 2008) using the phrase:
(psychoanaly* or psychodynamic* or insight?orient* or * EIO* or analytic* or dynamic*) in title, abstract and index fields in REFERENCE) OR (psychoanalys* or psychodynam* or insight?orient* or reality?adap* in interventions field in STUDY)]
This register is compiled by systematic searches of major databases, hand searches and conference proceedings (see Group Module).
2. Previous electronic searches Please see Appendix 1.
Searching other resources
1. Reference searching We inspected references of all identified studies for more trials.
2. Personal contact We contacted the first author of each included study for missing information.
Data collection and analysis
Selection of studies
Two reviewers independently inspected all study citations identified by the searches and full reports of the studies of agreed relevance were obtained. Where disputes arose, we acquired the full report for more detailed scrutiny. These articles were then inspected, independently, by two reviewers to assess their relevance to this review. Again, where disagreement occurred attempts were made to resolve this through discussion; if doubt still remained we added these trials to the list of those awaiting assessment pending acquisition of further information.
Data extraction and management
1. Data Extraction We independently extracted data. Where disagreement occurred attempts were made to resolve this by discussion, where doubt still remained we sought further information from the study authors to resolve the dilemma, and added the trial to the list of those awaiting assessment.
2. Management We extracted the data onto standard, simple forms. Where possible we entered data into RevMan in such a way that the area to the left of the line of no effect indicated a favourable outcome for the treatment group. Where this was not possible, for example for scales that calculate higher scores = improvement, graphs in RevMan analyses were labelled accordingly so that the direction of effects were clear.
3. Scale‐derived data 3.1 Valid scales A wide range of instruments are available to measure outcomes in mental health studies. These instruments vary in quality and many are not validated or are even ad hoc. It is accepted generally that measuring instruments should have the properties of reliability (the extent to which a test effectively measures anything at all) and validity (the extent to which a test measures that which it is supposed to measure) (Rust 1989). Unpublished scales are known to be subject to bias in trials of treatments for schizophrenia (Marshall 2000). Therefore continuous data from rating scales were included only if the measuring instrument had been described in a peer reviewed journal. In addition, the following minimum standards for instruments were set: the instrument should either be (a) a self‐report or (b) completed by an independent rater or relative (not the therapist) and (c) the instrument should be a global assessment of an area of functioning.
3.2 Binary outcomes from scale data Where possible, efforts were made to convert outcome measures to binary data. This can be done by identifying cut‐off points on rating scales and dividing participants accordingly into 'clinically improved' or 'not clinically improved'. It was generally assumed that if there had been a 50% reduction in a scale‐derived score such as the Brief Psychiatric Rating Scale (BPRS, Overall 1962) or the Positive and Negative Syndrome Scale (PANSS, Kay 1986), this could be considered as a clinically significant response (Leucht 2005a, Leucht 2005b). It was recognised that for many people, especially those with chronic or severe illness, a less rigorous definition of important improvement (e.g. 25% on the BPRS) would be equally valid. If individual patient data were available, the 50% cut‐off was used for the definition in the case of non‐chronically ill people and 25% for those with chronic illness. If data based on these thresholds were not available, we used the primary cut‐off presented by the original authors.
Assessment of risk of bias in included studies
We assessed the risk of bias by using the criteria described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008) to assess trial quality. The assessment considers how the sequence was generated, how allocation was concealed, the integrity of blinding at outcome, the completeness of outcome data, selective reporting and other biases. We would not have included studies where sequence generation was at high risk of bias or where allocation was clearly not concealed.
The categories are defined below: YES ‐ low risk of bias NO ‐ high risk of bias UNCLEAR ‐ uncertain risk of bias
If disputes arose as to which category a trial has to be allocated, again, resolution was made by discussion, after working with a third reviewer.
Earlier versions of this review used a different means of categorising risk of bias (see Appendix 2).
Measures of treatment effect
1. Binary data We calculated the relative risk (RR) and its 95% confidence interval (CI) based on the fixed‐effect model. Relative risk is more intuitive (Boissel 1999) than odds ratios and odds ratios tend to be interpreted as RR by clinicians (Deeks 2000). This misinterpretation then leads to an overestimate of the impression of the effect. When the overall results were significant we calculated the number needed to treat (NNT) and the number needed to harm (NNH) using Visual Rx (http://www.nntonline.net/). Where people were lost to follow up at the end of the study, we assumed that they had had a poor outcome and once they were randomised they were included in the analysis (intention‐to‐treat (ITT) analysis).
2. Continuous data 2.1 Normal distribution Continuous data on outcomes in trials relevant to mental health issues are often not normally distributed. To avoid the pitfall of applying parametric tests to non‐parametric data we applied the following standards to continuous final value endpoint data before inclusion: (a) standard deviations and means were reported in the paper or were obtainable from the authors; (b) when a scale started from zero, the standard deviation, when multiplied by two, should be less than the mean (otherwise the mean is unlikely to be an appropriate measure of the centre of the distribution ‐ Altman 1996); In cases with data that are greater than the mean they were entered into 'Other data' table as skewed data. If a scale starts from a positive value (such as PANSS, which can have values from 30 to 210) the calculation described above in (b) should be modified to take the scale starting point into account. In these cases skewness is present if 2SD>(S‐Smin), where S is the mean score and Smin is the minimum score.
Skewed endpoint data from studies with less the 200 participants were not shown graphically, but were added to 'Other data' tables and briefly commented on in the text. However, skewed endpoint data from larger studies (≥200 participants) pose less of a problem and we entered the data for analysis.
For change data (mean change from baseline on a rating scale) it is impossible to tell whether data are non‐normally distributed (skewed) or not, unless individual patient data are available. After consulting the ALLSTAT electronic statistics mailing list, we entered change data in RevMan analyses and reported the finding in the text to summarise available information. In doing this, we assumed either that data were not skewed or that the analysis could cope with the unknown degree of skew.
2.2 Data synthesis For continuous outcomes we estimated a weighted mean difference (MD) between groups based on a fixed‐effect model.
2.3 Final endpoint value versus change data Where both final endpoint data and change data were available for the same outcome category, only final endpoint data were presented. We acknowledge that by doing this much of the published change data may be excluded, but argue that endpoint data is more clinically relevant and that if change data were to be presented along with endpoint data, it would be given undeserved equal prominence.
Unit of analysis issues
1. Cluster trials Studies increasingly employ cluster randomisation (such as randomisation by clinician or practice) but analysis and pooling of clustered data poses problems. Firstly, authors often fail to account for intraclass correlation in clustered studies, leading to a 'unit of analysis' error (Divine 1992) whereby p values are spuriously low, confidence intervals unduly narrow and statistical significance overestimated. This can cause Type I errors (Bland 1997, Gulliford 1999).
Where clustering had not been accounted for in primary studies, we presented the data in a table with a (*) symbol to indicate the presence of a probable unit of analysis error. In subsequent versions of this review we will seek to contact first authors of studies to obtain intraclass correlation coefficients of their clustered data and to adjust for this using accepted methods (Gulliford 1999). Where clustering has been incorporated into the analysis of primary studies, we will also present these data as if from a non‐cluster randomised study, but adjusted for the clustering effect.
We have sought statistical advice and have been advised that the binary data as presented in a report should be divided by a design effect. This is calculated using the mean number of participants per cluster (m) and the intraclass correlation coefficient (ICC) [Design effect=1+(m‐1)*ICC] (Donner 2002). If the ICC is not reported we assumed it to be 0.1 (Ukoumunne 1999).
If cluster studies had been appropriately analysed taking into account intraclass correlation coefficients and relevant data documented in the report, we synthesised these with other studies using the generic inverse variance technique.
2. Cross‐over trials A major concern of cross‐over trials is the carry‐over effect. It occurs if an effect (e.g. pharmacological, physiological or psychological) of the treatment in the first phase is carried over to the second phase. As a consequence on entry to the second phase the participants can differ systematically from their initial state despite a wash‐out phase. For the same reason cross‐over trials are not appropriate if the condition of interest is unstable (Elbourne 2002). As both effects are very likely in schizophrenia, we will only use data of the first phase of cross‐over studies.
3. Studies with multiple treatment groups Where a study involved more than two treatment arms, if relevant, the additional treatment arms were presented in comparisons. Where the additional treatment arms were not relevant, these data were not reproduced.
Dealing with missing data
At some degree of loss to follow‐up data must lose credibility (Xia 2007). We excluded data from studies where more than 50% of participants in any group were lost to follow up (this did not include the outcome of 'leaving the study early'). In studies with less than 50% dropout rate, people leaving early were considered to have had the negative outcome, except for the event of death. Where high attrition occurred in primary outcomes we analysed the impact of including studies with high attrition rates (25‐50%) in a sensitivity analysis. If inclusion of data from this latter group resulted in a substantive change in the estimate of effect, we did not add their data to trials with less attrition, but presented them separately.
Assessment of heterogeneity
1. Clinical heterogeneity We considered all included studies without any comparison to judge clinical heterogeneity.
2. Statistical 2.1 Visual inspection We visually inspected graphs to investigate the possibility of statistical heterogeneity.
2.2 Employing the I‐squared statistic This provided an estimate of the percentage of inconsistency thought to be due to chance. I‐squared estimate greater than or equal to 50% was interpreted as evidence of high levels of heterogeneity (Higgins 2003).
Assessment of reporting biases
Reporting biases arise when the dissemination of research findings is influenced by the nature and direction of results. These are described in section 10.1 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008). We are aware that funnel plots may be useful in investigating reporting biases but are of limited power to detect small‐study effects (Egger 1997). Funnel plots were not used for outcomes involving 10 or fewer studies, or where all studies were of similar sizes. In other cases, where funnel plots were possible, we sought statistical advice in their interpretation.
Data synthesis
Where possible we used a random‐effect model for analyses. We understand that there is no closed argument for preference for use of fixed or random‐effects models. The random‐effects method incorporates an assumption that the different studies are estimating different, yet related, intervention effects. This does seem true to us, however, random‐effects does put added weight onto the smaller studies ‐ those trials that are most vulnerable to bias.
Subgroup analysis and investigation of heterogeneity
When heterogeneous results were found, we investigated the reasons for this. Where heterogeneous data substantially altered the results and the reasons for the heterogeneity were identified, these studies were not summated in the meta‐analysis, but presented separately and discussed in the text.
Sensitivity analysis
The effects of including studies with high attrition rates would be analysed in a sensitivity analysis. Where data is available, sensitivity analyses will be performed to investigate whether there were differences:
1. in response between in‐ and outpatients; 2. between participants living alone or with family; 3. in people having their first episode of schizophrenia compared to those whose illness was of longer duration; 4. between strict psychoanalytic techniques and techniques incorporating supportive and directive activity; and 5. between studies of well‐defined psychotherapy (as defined by the reviewers) and studies of less well defined psychotherapy (as defined by the reviewers).
Results
Description of studies
Results of the search
The update search (June 2008) of the Cochrane Schizophrenia Groups Register produced 32 citations relating to 25 trials. No studies were selected for further inspection. In an earlier update search of the Cochrane Schizophrenia Group Trials Register (December 2006) we found 350 new references from 154 studies identified since the last search (August 2000). From these, 12 citations were selected for further inspection. Three were further reports of studies included in the review which did not contain additional data. Seven were excluded because they were not psychodynamic interventions. We included one newly identified study (Karon 1981) bringing the total number of included trials to four. We also identified a further report of May 1976 and were able to extract some additional outcome data.
Included studies
1. Design Only four studies reported data in a way that could be extracted for inclusion (O'Brien 1972, May 1976, Karon 1981 and Gunderson 1984). All included trials were randomised and none double‐blind. Grants from the US National Institute of Mental Health supported all of the included studies.
2. Length of trials Gunderson 1984 followed participants for two years. Karon 1981 lasted for 20 months and O'Brien 1972 continued intervention for 20 months. In May 1976 participants were initially treated for 6‐12 months and when treatment stopped, participants were followed for up to five years, although complete data are only available up to three years.
3. Participants One study used an operational diagnosis of schizophrenia (Gunderson 1984). This study spanned the changeover from DSM (Diagnostic Statistical Manual) version II to III. None of the other studies appeared to use operational diagnoses of schizophrenia. May 1976 excluded those who were 'obviously not going to be discharged within two years and those whose illness went into remission during the assessment period'. O'Brien 1972 included those whose diagnosis was schizophrenia and whose case notes contained 'clear evidence of a psychotic episode'. Karon 1981 aimed to include people who were acutely ill, but clearly identified as having schizophrenia.
Gunderson 1984 and Karon 1981 did not report the gender of the included participants. Both May 1976 and O'Brien 1972 included men and women. The participants age ranged from 18‐35 years in the Gunderson 1984 study and O'Brien 1972 reported a mean age of 36 to 37 years. Participants ages were not reported by Karon 1981 or May 1976. Participants in the O'Brien 1972 study had a mean number of admissions of about three. May 1976 only included people having their first admission. Gunderson 1984 selected those who had minimal prior treatment, no history of alcohol dependence or drug abuse, and had been able to function outside of hospital in some major role without medication for four consecutive months in the previous two years, which suggests that participants were not similar to those seen in clinical practice. Karon 1981 specified acute first episode participants, but at least one third were discovered to have had previous hospital admissions.
4. Setting Most participants in the included studies were initially in hospital, with all eventually proceeding to outpatient status.
5. Study size Gunderson 1984 initially randomised 164 people and 69 left the study early (before six months); only details of the 95 who stayed in therapy beyond six months are reported. May 1976 randomised 228 people, O'Brien 1972 100, and Karon 1981 36.
6. Interventions We are unable to make definitive comments on whether the initial definitions of psychoanalytic or psychodynamic treatment in this review are the same as those employed in the included studies. Information is poor within the studies, especially relating to frequency of administration and orientation of the therapists. In effect, inclusion of O'Brien 1972 and May 1976 resulted from supposition that lengthy psychotherapy, undertaken in the 1970s by people who did not explicitly mention that the intervention was psychoanalytic in nature, would mean that it is a psychodynamic therapy. May 1976 presented no descriptions of the orientation of the therapy or therapists. He mentioned the supervision of the treatment. "Each patient's treatment was supervised by an experienced consultant who believed in the efficacy of the particular treatment that he supervised" (May 1976). O'Brien 1972 also gave no mention of the orientation of the therapists or therapy. "The purpose of our study was to determine the relative effectiveness of group and individual therapy for schizophrenic aftercare patients" (O'Brien 1972). Therapists were said to be supervised if they were students (normally medical), but other therapists were not said to be in supervision. The treatment duration had not been reported, but follow up was intended to be for 24 months. No explicit definition of the therapy is mentioned for Gunderson 1984, but several references are made to Stanton's psychodynamic/psychoanalytic orientation (one of the main authors). "Stanton in designing this project, made use of the technique of the randomised trial to 'test' his cherished beliefs that individual psychodynamically‐orientated psychotherapy would have a therapeutic effect on the cognitive functioning, psychopathology and social functioning of schizophrenic patients" (Klerman 1984). In Karon 1981 three interventions were used. Group 'A', the psychodynamic group without medication, received five sessions per week for the first two to eight weeks until discharge. Thereafter, psychotherapy sessions were provided once per week until the end of the study. Group 'B', the psychodynamic group with medication, received an 'ego‐analytic' psychotherapy approach three times per week for at least 20 sessions which then reduced to one session per week. These participants also received adjunctive phenothiazines. Group 'C' received standard care.
7. Outcomes 7.1 Improvement Definition of improvement varied but seemed to be based on more pragmatic ‐ and more useful ‐ outcomes than have been measured in many other systematic reviews of schizophrenia treatments. Days in hospital, ability to be discharged, role functioning and self‐support were the primary outcomes.
7.2 Missing outcomes Data on adverse effects were not collected and do not seem to have been considered by any of the trialists. Data on use of medication seemed to have been collected in the studies, but were not reported, except when it was the comparator treatment. May 1976 gives long term follow‐up data for those who received additional medication or eventually received medication. No trial reported on economic outcomes. The scales used for measuring some of the outcomes do not seem to be global measures. Many trials presented findings in graphs or by p‐values alone. Graphical presentation made it impossible to acquire data for synthesis; p‐values were commonly used as a measure of association between intervention and outcomes instead of showing the strength of the association. Many did not provide standard deviations of means or did not give any information.
7.3 Continuous data On the whole, no scale‐derived continuous data were provided in initial reports of any of the studies. May 1976 does give a continuous result from the Menninger Health Sickness Scale, which is included in this review. Other continuous outcomes were measured, such as days in hospital, but the standard deviation is not reported. Reasons for exclusion of data from other instruments are given under 'Outcomes' in the 'Characteristics of included studies' tables.
7.4 Outcome scales 7.4.1 Menninger Health Sickness Rating Scale ‐ HSRS (Luborsky 1962) Scoring 0 to 100, the Health Sickness Rating Scale was developed to provide a simple survey instrument to record shorthand judgements of a patient's status, recording changes over time and allowing comparisons between patients. It provides a global rating with seven criteria and with other personality qualities. May 1976 reported usable data from this scale.
Excluded studies
Fifty‐seven studies are excluded; the majority because they are reviews of either the included studies or of the literature. Many were excluded because they were studies of other types of interventions (short versus long hospitalisation, family management, what seems to be cognitive behavioural therapy, cognitive behavioural therapy and attitudinal changes); two were comparisons of the effects of drugs on ego function or symbol formation; one seemed to be psychoanalysis, but used a case‐control study with a heterogeneous group of participants, with no data being available just for those with schizophrenia; and another used a retrospective design (Lindberg 1981). Three did not include participants with schizophrenia (Guthrie 1997, Chiesa 1999, Schachter 2001). Three studies were excluded because they had no available data (Karon 1969, Sjostrom 1990, Volterra 1996).
Awaiting assessment
We are currently seeking further information from one potentially randomised study (Wilner 1985).
Ongoing studies
We are not aware of any ongoing studies.
Risk of bias in included studies
The barely adequate reporting of randomisation and lack of double‐blindness for these outcomes would suggest that all estimates of effect of the experimental intervention are prone to exaggeration (Moher 1998). Judgement of risks are illustrated in Figure 1.
1.
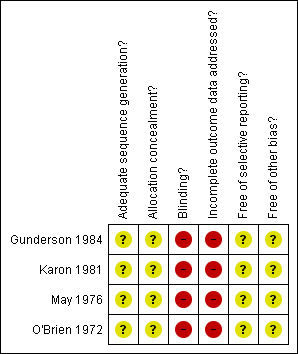
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Allocation
All four trials were stated to be randomised, but none described how randomisation had been achieved nor who performed the procedure. The reader is not assured that biases were not introduced. Studies have shown that poor reporting of randomisation increases the odds of presenting 'significant' outcomes (Chalmers 1983, Schulz 1995).
Blinding
None of the studies attempted to blind participants or investigators to the type of treatment intervention. Gunderson 1984 and May 1976 used independent assessors, whereas in O'Brien 1972 the study staff rated the participants of the other therapists, with no one eligible to rate their own work or the participants they were working with. Karon 1981 reported that the assessors were blinded to treatment groups, but did not describe whether this had been implemented successfully. No study clearly described adequate precautions for blinding of assessment. It is important that those extracting data from studies are assured that trialists minimised the introduction of bias when assessing the impact of interventions.
Incomplete outcome data
Gunderson 1984 only followed up those who completed six months of treatment giving a rate of attrition of 42% from the start. At 12 months, 56% had left and at 24 months, 71%. Participants who were discharged or dropped out after six months, seem, nevertheless, to have been followed up ‐ a practice that is rare in schizophrenia research ‐ and very informative. In May 1976 most participants remained in the study with over 90% completion for both groups. This study is also remarkable as it managed to follow up participants for up to five years. In O'Brien 1972 at 12 months, the percentage who left the study early is 58% in the individual analysis group and 38% in the group psychotherapy group, giving an overall rate at 12 months of 48%. At 20 months, it is 90% and 82% respectively, with a pooled rate of 86%. This includes those who were eligible for discharge. Again, the authors were able to follow people up. In Karon 1981 a total of 36 participants were randomised. Subsequently, three participants were excluded from the study but it is not clear from which of the three intervention groups this occurred.
No study stated that they analysed their data on an intention‐to‐treat basis. Once people leave, unless trialists continue to follow and collect data, assumptions have to be made about outcome. As many people left these studies early, the results do incorporate considerable assumptions. In this review those leaving the studies early were classified as a 'bad outcome' and analysed accordingly (except for the outcome of death). Whatever the management of lost data, interpretation of results with large degrees of attrition must be undertaken with caution. Where greater than 50% of those randomised were lost to follow up outcomes are marked with an asterisk (*) in order to draw the attention of the reader to the 'prone to bias' footnote.
Selective reporting
Much of the available data were rendered unusable due to missing standard deviations or a complete absence of data (BPRS) on mental states scores. It is unclear whether this was due to the data being selectively reported or simply as a result of poor reporting.
Effects of interventions
See: Table 1
Only one study is available for inclusion in each comparison.
1. COMPARISON 1. INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY versus MEDICATION May 1976 is included in this comparison (Table 1).
1.1 Committed suicide by three years We found no significance difference for the outcome of committing suicide at three years. Three people in the group which received medication and one in the group treated solely with psychotherapy committed suicide (n=92, RR 0.52 CI 0.1 to 5.6, Analysis 1.1).
1.1. Analysis.
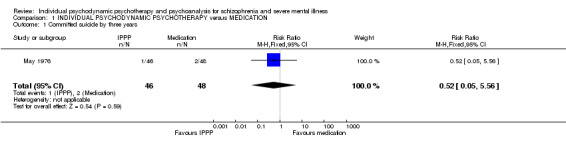
Comparison 1 INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY versus MEDICATION, Outcome 1 Committed suicide by three years.
1.2 Global impression: not able to be discharged We found more participants in the psychotherapy group were not eligible for discharge compared with the participants given only medication (1 RCT, n=92, RR 8.35 CI 2.0 to 34.3, NNH 3 CI 2 to 6, Analysis 1.2).
1.2. Analysis.
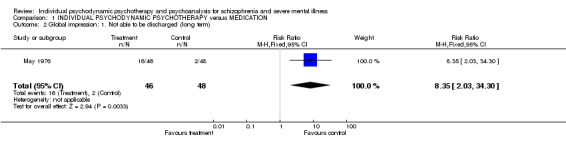
Comparison 1 INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY versus MEDICATION, Outcome 2 Global impression: 1. Not able to be discharged (long term).
1.3 Global impression: given additional medication or received medication by 12 months to three years follow up At 12 months, we found fewer participants in the psychotherapy groups needed additional medications compared with those who received medication (1 RCT, n=74, RR 0.64 CI 0.5 to 0.8, NNT 3 CI 3 to 6), and also at three years follow up (1 RCT, n=87, RR 0.85 CI 0.8 to 1.0, NNT 7 CI 5 to 26, Analysis 1.3).
1.3. Analysis.
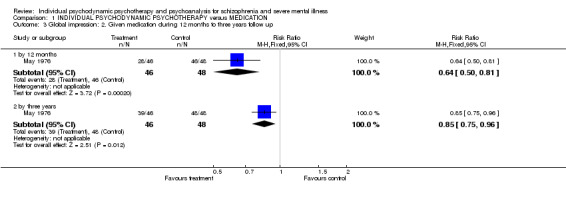
Comparison 1 INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY versus MEDICATION, Outcome 3 Global impression: 2. Given medication during 12 months to three years follow up.
1.4 Global impression: Achieved best level of health at two years (Menninger Health Sickness Scale, high=better) We found participants who took medication achieved the 'best level of health' by the care team (1 RCT, n=92, MD ‐5.8 CI ‐10 to ‐1.6, Analysis 1.4) compared with the individual psychotherapy group.
1.4. Analysis.
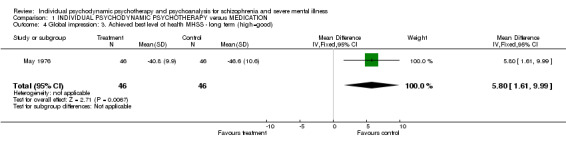
Comparison 1 INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY versus MEDICATION, Outcome 4 Global impression: 3. Achieved best level of health MHSS ‐ long term (high=good).
1.5 Global impression: Treatment not considered successful by treatment team Participants who received individual psychodynamic therapy were more likely to have been treated unsuccessfully by the treatment team than those who received drug therapy alone (1 RCT, n=92, RR 16.4 CI 2.3 to 118.8, NNH 4 CI 2 to 39, Analysis 1.5).
1.5. Analysis.
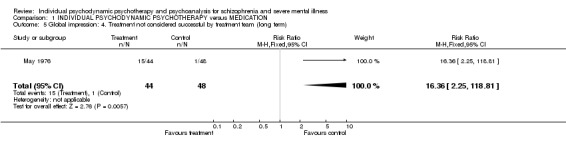
Comparison 1 INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY versus MEDICATION, Outcome 5 Global impression: 4. Treatment not considered successful by treatment team (long term).
1.6 Global impression: Hospital re‐admission We found no significant difference in the rates of re‐hospitalisation between psychotherapy without medication and those given medication alone (1 RCT, n=24, RR 0.63 CI 0.3 to 1.4, Analysis 1.6).
1.6. Analysis.
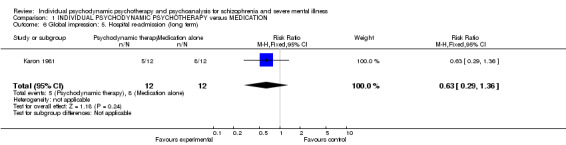
Comparison 1 INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY versus MEDICATION, Outcome 6 Global impression: 5. Hospital re‐admission (long term).
1.7 Leaving the study early During long‐term evaluation we found no significant difference in study attrition (1 RCT, n=94, RR 1.04 CI 0.3 to 3.9, Analysis 1.7).
1.7. Analysis.
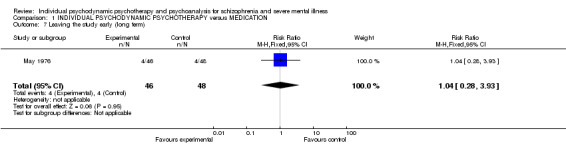
Comparison 1 INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY versus MEDICATION, Outcome 7 Leaving the study early (long term).
2. COMPARISON 2. INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY AND MEDICATION versus MEDICATION May 1976 is the only study included in this comparison.
2.1 Committed suicide We found no clear difference in participants receiving individual therapy plus medication and those given only medication (1 RCT, n=92, RR 0.16 CI 0.01 to 2.9, Analysis 2.1). Three people who only received medication committed suicide by three years, with nobody receiving medication and individual therapy killing themselves.
2.1. Analysis.
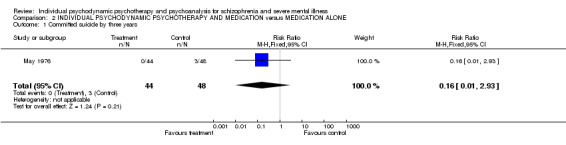
Comparison 2 INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY AND MEDICATION versus MEDICATION ALONE, Outcome 1 Committed suicide by three years.
2.2 Global impression: Not able to be discharged No significant differences were found in discharge eligibility between individual therapy combined with antipsychotic drugs and drugs alone (1 RCT, n=92, RR 1.09 CI 0.2 to 7.4, Analysis 2.2).
2.2. Analysis.
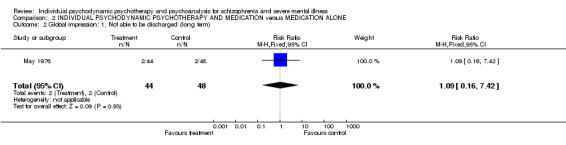
Comparison 2 INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY AND MEDICATION versus MEDICATION ALONE, Outcome 2 Global impression: 1. Not able to be discharged (long term).
2.3 Global impression: given additional medication or received medication by 12 months to three years follow up We found no significant difference between the two groups for the outcome of being given additional medication at 12 months (1 RCT, n=86, RR 0.95 CI 0.9 to 1.1) or at three years (1 RCT, n=90, RR 0.95 CI 0.9 to 1.0, Analysis 2.3).
2.3. Analysis.
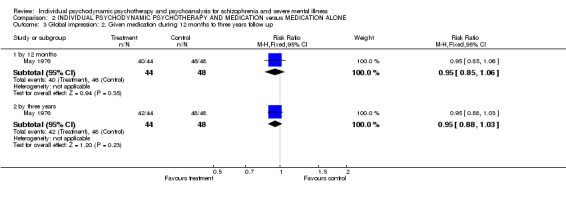
Comparison 2 INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY AND MEDICATION versus MEDICATION ALONE, Outcome 3 Global impression: 2. Given medication during 12 months to three years follow up.
2.4 Global impression: Achieved best level of health (Menninger Health Sickness scale: high=good) From the health sickness scales, we found no significant difference between groups for having achieved the best level of health (1 RCT, n=90, MD ‐0.80 CI ‐5.4 to 3.8, Analysis 2.4).
2.4. Analysis.
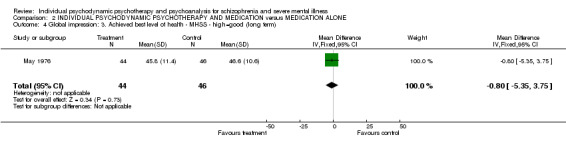
Comparison 2 INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY AND MEDICATION versus MEDICATION ALONE, Outcome 4 Global impression: 3. Achieved best level of health ‐ MHSS ‐ high=good (long term).
2.5 Global impression: Treatment not considered successful by treatment team No significant differences were found for the outcome of 'treatment not considered successful' (1 RCT, n=92, RR 2.18 CI 0.2 to 23.2, Analysis 2.5) between the two groups.
2.5. Analysis.
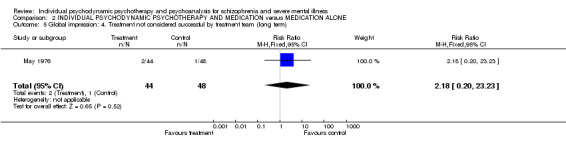
Comparison 2 INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY AND MEDICATION versus MEDICATION ALONE, Outcome 5 Global impression: 4. Treatment not considered successful by treatment team (long term).
2.6 Global impression: Hospital re‐admission We found rates of re‐hospitalisation in long‐term analysis were equivocal between psychotherapy with medication and participants given only medication (1 RCT, n=24, RR 1.00 CI 0.4 to 2.6, Analysis 2.6).
2.6. Analysis.
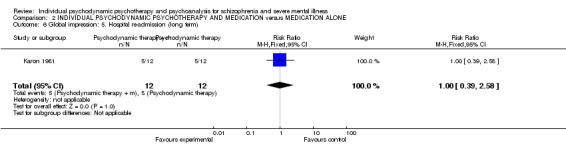
Comparison 2 INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY AND MEDICATION versus MEDICATION ALONE, Outcome 6 Global impression: 5. Hospital re‐admission (long term).
2.7 Leaving the study early During long‐term evaluation we found study attrition to be equivocal (1 RCT, n=94, RR 0.82 CI 0.2 to 3.5, Analysis 2.7).
2.7. Analysis.
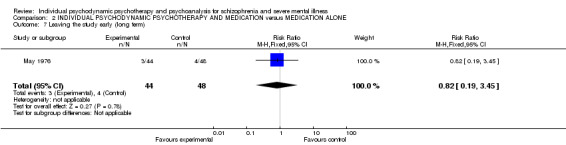
Comparison 2 INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY AND MEDICATION versus MEDICATION ALONE, Outcome 7 Leaving the study early (long term).
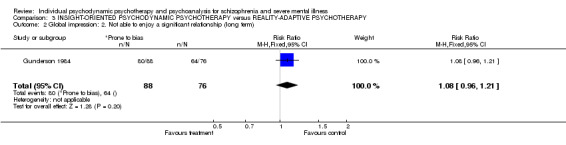
3. COMPARISON 3. INSIGHT‐ORIENTED PSYCHODYNAMIC PSYCHOTHERAPY versus REALITY‐ADAPTIVE PSYCHOTHERAPY 3.1 Global impression Data on ability to perform major household tasks (n=164, RR 1.1 CI 1.0 to 1.3, p=0.06) almost reached statistical significance in the Gunderson 1984 trial. No significant differences were found between groups for enjoying major relationships (1 RCT, n=164, RR 1.1 CI 1.0 to 1.2). For the outcome of not being self‐supporting, we again found no significant difference between groups (1 RCT, n=164, RR 1.05 CI 0.9 to 1.2). For the outcome of re‐hospitalisation we found no significant difference between the psychodynamic approach and the more cognitive‐based therapy (1 RCT, n=164, RR 1.20 CI 0.9 to 1.6, Analysis 3.1).
3.1. Analysis.
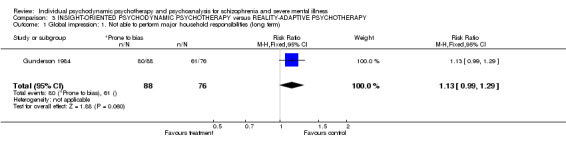
Comparison 3 INSIGHT‐ORIENTED PSYCHODYNAMIC PSYCHOTHERAPY versus REALITY‐ADAPTIVE PSYCHOTHERAPY, Outcome 1 Global impression: 1. Not able to perform major household responsibilities (long term).
3.2 Leaving the study early People receiving the psychodynamic approach were more likely to continue in the study than those allocated to reality‐adaptive therapy at six months (1 RCT, n=164, RR 0.46 CI 0.3 to 0.7, NNT 3 CI 3 to 6), at 12 months (1 RCT, n=164, RR 0.46 CI 0.3 to 0.6, NNT 2 CI 2 to 4) and at 24 months (1 RCT, n=164, RR 0.54 CI 0.4 to 0.7, NNT 2 CI 2 to 3, Analysis 3.2).
3.2. Analysis.
Comparison 3 INSIGHT‐ORIENTED PSYCHODYNAMIC PSYCHOTHERAPY versus REALITY‐ADAPTIVE PSYCHOTHERAPY, Outcome 2 Global impression: 2. Not able to enjoy a significant relationship (long term).
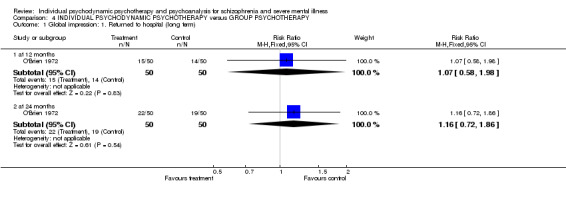
4. COMPARISON 4. INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY versus GROUP PSYCHOTHERAPY 4.1 Global impression For the outcome of 'returned to hospital' we found no significant difference between the therapies at one and two years in the O'Brien 1972 study. For global state 'not improved' we found no significant difference between groups (1 RCT, n=100, RR 1.27 CI 1.0 to 1.7). We found no significant difference in the number of participants who were actively discharged from therapy at two years (1 RCT, n=100, RR 0.60 CI 0.3 to 1.1). Twelve month data were equivocal. Fewer participants remained in therapy in the individual psychodynamic group at 12 months compared with group psychotherapy, although the upper confidence interval reached the line of no effect (1 RCT, n=100, RR 0.68 CI 0.5 to 1.0, Analysis 4.1). Two year data were equivocal.
4.1. Analysis.
Comparison 4 INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY versus GROUP PSYCHOTHERAPY, Outcome 1 Global impression: 1. Returned to hospital (long term).
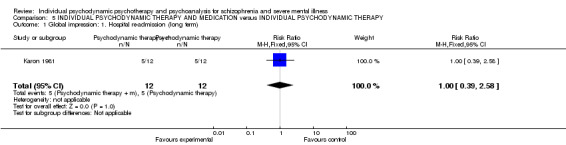
5. COMPARISON 5. INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY WITH MEDICATION versus INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY 5.1 Global impression: Re‐hospitalisation We found rates of re‐hospitalisation during long‐term analyses were equivocal in participants receiving psychotherapy with medication, and psychotherapy without medication (1 RCT, n=24, RR 1.00 CI 0.4 to 2.6, Analysis 5.1).
5.1. Analysis.
Comparison 5 INDIVIDUAL PSYCHODYNAMIC THERAPY AND MEDICATION versus INDIVIDUAL PSYCHODYNAMIC THERAPY, Outcome 1 Global impression: 1. Hospital re‐admission (long term).
Discussion
Summary of main results
Before any summary of the findings are presented we think it is important to remember that no comparison has more than 164 people in any trial. The trials are pioneering and important ‐ but very, very small and any finding or suggestion of a finding should be replicated.
1. COMPARISON 1. INDIVIDUAL PSYCHODYNAMIC THERAPY versus MEDICATION 1.1 Suicide During three years of participant evaluation, psychodynamic therapy does not appear to reduce the risk of suicide compared with standard care. This is based on few events in small numbers of people.
1.2 Global impression All treatment took place in hospital and participants were discharged when ready to go home. More people on medication only were eligible for discharge than those allocated to the psychodynamic group. Although numbers are small (n=92) this is a strong finding (RR 8.35 CI 2.0 to 34.3, Analysis 1.2) that most clinicians would find intuitive.
Unsurprisingly, those who were randomised to receive medication only as part of the trial either continued to receive, or received additional medication at 12 months and three years (46/48 at 12 months; 48/48 at three years). What is surprising, though, is that those who received individual therapy did not, on the whole, go on to receive medication. It seems that, upon reading the reports of the trials, those who participated were not discharged from hospital on medication, but only received it for the duration of their stay. This outcome reports on the number of people who received prescriptions for medication after being discharged from hospital. At 12 months, statistical significance is found between the two groups for those who received individual therapy and those who received medication only, with psychotherapy needing to be given to three people to avoid one extra person receiving medication (NNT 3 CI 3 to 6). Those who did not receive medication in hospital, as part of the study, continued to be less likely to receive medication outside of hospital at three years also (NNT 7 CI 5 to 26). However, when continuous data are presented for having achieved best level of health, those who received medication were deemed to have a better outcome than those who received therapy alone. Using these two results and taking the outcome of 'not considered to have been treated successfully', (15/46 versus 1/48, NNH 4 CI 2 to 39), the clinician would need to be certain of their reasons for not implementing medication. Individual psychodynamic therapy seems no better ‐ and probably worse ‐ than medication for people with schizophrenia and the therapy may have a longer term effect in discouraging the use of medication ‐ and in this way could have deleterious effects of considerable duration.
1.3 Hospital re‐admission Participants who received psychodynamic therapy faired no better than people given only standard care for the outcome of hospital re‐admission, but this is based upon a small sample (n=24, Karon 1981) and is under powered making such an evaluation unreliable.
1.4 Leaving the study early Study attrition is only reported in the May 1976 with only four participants leaving early from each group (4/46, 4/48), which is low by the standards of modern schizophrenia randomised controlled trials.
2. Comparison 2. INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY AND MEDICATION versus MEDICATION The core of any discussion for this comparison is that there are too few data to make firm conclusions. There are some interesting findings but all data are few, out of date and of limited quality.
2.1 Suicide We found no significant advantage for the use of psychodynamic therapy in combination with antipsychotic drugs for preventing suicide compared with participants given only medication. Perhaps a larger study may have shown significant differences ‐ May 1976 evaluated outcomes from only 92 people.
2.2 Global impression From limited data (May 1976, n=92) we found no significant advantage for the use of psychodynamic therapy in combination with antipsychotic drugs for the outcomes 'not able to be discharged', 'needing additional medication' or for achieving the best level of health from the Menninger Health Sickness scale, compared with participants given only antipsychotics.
2.3 Hospital re‐admission We did not find any significant difference in re‐hospitalisation rates between psychodynamic therapy plus antipsychotics, and participants given only standard care. Again hospital re‐admission is only evaluated by Karon 1981 with a total of 24 participants included in the analysis.
2.4 Treatment not considered successful by treatment team 'Successful treatment' as judged by a treatment team did not reveal any significant advantage for the psychodynamic therapy and antipsychotics group compared with standard care treatment (May 1976, n=92).
2.5 Leaving the study early Again, we could only extract data on study attrition from May 1976. Only three participants left early from the combined psychodynamic therapy plus antipsychotic group, and four left from the drugs only group (3/44, 4/48) suggesting that psychodynamic therapy combined with antipsychotics is no less acceptable to participants than standard care.
3. COMPARISON 3. INSIGHT‐ORIENTED PSYCHODYNAMIC PSYCHOTHERAPY versus REALITY‐ADAPTIVE PSYCHOTHERAPY 3.1 Global impression The largest of the four included studies (Gunderson 1984, n=164) reported outcomes for ability to perform household tasks, enjoy major relationships, re‐hospitalisation and not being able to self‐support, and we found no significant difference between groups. This is in keeping with other findings that there is little differences between different psychotherapeutic approaches when it comes to several aspects of mental health.
3.2 Leaving the study early Psychodynamic therapy proved to be more acceptable to participants than reality‐adaptive therapy in this unusual and highly selective study at six months (NNT 3 CI 3 to 6), 12 months (NNT 2 CI 2 to 4) and at 24 months (NNT 2 CI 2 to 3) with significantly fewer leaving the study early. This finding is in need of replication.
4. COMPARISON 4. INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY versus GROUP PSYCHOTHERAPY 4.1 Global impression The O'Brien 1972 study reported outcome data for global state 'not improved', 'number of patients actively discharged from therapy' and 'remaining in therapy' and we found no significant differences between individual psychodynamic therapy and the more cost efficient therapeutic group approach. Considering how cost‐efficient group therapy could be this is type of comparison should be considered again for almost any psychotherapeutic approach.
5. COMPARISON 5. INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY WITH MEDICATION versus INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY 5.1 Re‐hospitalisation We were only able to include one study for this comparison (Karon 1981) and from limited data (n=24) no significant differences emerged. It is not clear that there are additive effects of individual psychodynamic psychotherapy to medication, but, again, this study is under powered and a larger sample size is needed to be able to detect any treatment effect.
Overall completeness and applicability of evidence
1. General All studies were set in North America and mostly randomised participants without operationally diagnosed disorders. Participants also seemed to have illnesses uncomplicated by co‐morbidity. The inclusion criteria were so strict in Gunderson 1984 (diagnosis of schizophrenia, DSM II & III, confirmed three times and only 164 out of nearly 2000 screened), it is likely that people entering the study were not like those seen in clinical practice. How participants in May 1976 resemble those normally seen in practice is hard to know, with entry criteria of 'not likely to improve' and those who responded quickly being excluded. Karon 1981 intended to include participants who were acutely ill with no previous hospitalisations but it emerged that a third of participants had withheld relevant information during the screening and had been previously hospitalised.
2. Limited data The collection and quality of reporting of data is disappointing, although the outcomes measured do have more clinical meaning than much scale‐derived data commonly reported in trials (Thornley 1998). Where continuous data were reported, such as days in hospital, means and standard deviations were not given, or data were presented in graphs that made it impossible to extract useful information. Much data were unable to be included in this review as a result of inadequate reporting. There seemed to be no consideration given to adverse effects from the treatments in the included studies.
3. Psychoanalytic therapy No trials were identified investigating the value of a psychoanalytic approach for people with schizophrenia.
4. Sensitivity analysis and publication bias We were unable to undertake the proposed funnel graph for publication bias or undertake a sensitivity analysis for the effects of including studies with high attrition versus those with lower loss to follow up. Despite not being able to undertake a funnel plot for publication bias, the absence of any controlled studies that have attempted to replicate the included studies surprises us, and leads us to question whether there is a bias away from research in this understudied area.
Quality of the evidence
The quality of reporting in most studies was poor. There are likely to be significant biases in the results favouring psychodynamic‐psychotherapy. The magnitude of the effects of these biases on, for example, the primary outcome, could be considerable with an overestimate of 30% being entirely credible (Jüni 2001).
Potential biases in the review process
We have only been able to identify a small number of studies that were published in the 1970s and 1980s and each study used its own approach to psychodynamic psychotherapy and therefore they do not necessarily reflect current practice.
Agreements and disagreements with other studies or reviews
This review updates and improves past work and agrees with findings from previous versions.
Authors' conclusions
Implications for practice.
There are too few data to guide clinical implications with confidence.
1. People with schizophrenia Taking medication seems far more effective than psychodynamic therapy for helping achieve hospital discharge. Although all other data are sparse, there is no indication of any beneficial effect at all of psychodynamic therapy for those with schizophrenia, except if you consider not being given additional medication in the twelve months to three years after discharge. Those receiving psychotherapy alone were less likely to be seen as treated successfully or achieving best level of health, compared to those who received medication alone. When compared to a more cognitive approach, psychodynamic therapy may be more acceptable, but data on possible harm were not recorded.
2. Clinicians People receiving an insight‐oriented psychodynamic therapy tend to stay in contact with therapists longer than those receiving a more cognitive‐based reality adaptive therapy, but there is little evidence of any positive effect from a psychodynamic approach. This is due to a lack of evidence, rather than a presence of evidence which demonstrates a lack of positive effect. There are some hints from the data that a group approach may be a cost effective way of providing the intervention ‐ but that the intervention may put people off taking medication.
3. Managers or policy makers More recent therapies have eclipsed the psychodynamic approach for schizophrenia (Jones 1999) but the psychodynamic approach could still be of value ‐ we do not have the data to dismiss its effects entirely.
Implications for research.
1. General If any studies are being conducted or planned they should strictly adhere to the CONSORT statement (Begg 1996, Moher 2001, CONSORT) in order to present usable data.
2. Specific It is feasible that real effects of psychodynamic therapy have been missed through poor recording, or loss of limited data, or because the trials just have not been done. Funding for a randomised trial would probably be difficult to acquire. Nevertheless, should psychodynamic therapy be recommended for someone with schizophrenia it should, if possible, be given within a context of a well‐designed, clinically relevant randomised trial (see Table 2 for a suggestion of a design). Data relating to hospitalisation, role function, independence, mental state and behaviour need replication and expansion. More high‐quality trial‐derived data relating to satisfaction with care, social functioning, family burden, employment and adverse effects would be of great interest. Data on psychotherapy effects in people who are not in hospital are missing.
1. . Suggested design of study.
| Methods | Allocation: randomised, block, fully explicit description. Blinding: single, tested. Duration: 12 weeks treatment, and then follow up to at least 26 weeks. |
| Participants | Diagnosis: schizophrenia (ICD). N=300.* Age: adults. Sex: both. |
| Interventions | 1. Individual Psychodynamic Psychotherapy. N=150. 2. Standard care. N=150. |
| Outcomes | General: time to all‐cause treatment failure marked by its discontinuation, relapse, general impression of clinician (CGI), career/other (CGI), compliance with treatment., healthy days, Mental state: CGI. Quality of life. CGI. Family burden: CGI. Social functioning: return to everyday living for 80% of time.* Adverse events: any adverse event recorded. Economic outcomes. |
| Notes | * Powered to be able to identify a difference of ˜20% between groups for primary outcome with adequate degree of certainty. |
What's new
| Date | Event | Description |
|---|---|---|
| 18 January 2012 | Amended | Contact details updated. |
History
Protocol first published: Issue 1, 1999 Review first published: Issue 2, 2000
| Date | Event | Description |
|---|---|---|
| 26 February 2009 | New search has been performed | One new included study (Karon 1981) bringing the total number of included trials to four. We also identified a further report of the May 1976 study and were able to extract additional outcome data. |
| 10 December 2008 | Amended | Converted to new review format. |
| 24 May 2001 | New citation required and conclusions have changed | Substantive amendment |
Notes
This review has undergone external peer review and internal editorial review.
Acknowledgements
The past and present editors and staff of the Cochrane Schizophrenia Group's editorial base are acknowledged for their help and comments. Deborah Stacey and Hannu Juvonen are also acknowledged for their help at the protocol stage and Hannu Juvonen for comments on the finished review.
Appendices
Appendix 1. Details of past searches for earlier versions of this review
1. December 2006 We searched The Cochrane Schizophrenia Group Trials Register (December 2006) using the phrase:
(psychoanaly* or psychodynamic* or insight?orient* or * EIO* or analytic* or dynamic*) in title, abstract and index fields in REFERENCE) OR (psychoanalys* or psychodynam* .. in interventions field in STUDY)]
2. The following search phrase was constructed to assist identification for previous versions of this review (Malmberg 2001)
[and (psychoanaly* or ((analytic* or dynamic* or psychodynamic*) and (therap* or psychotherap*)))]
1. We searched Biological Abstracts (January 1985 to January 1999) using the Cochrane Schizophrenia Group's terms for both randomised controlled trials and schizophrenia combined with the phrase:
[and (psychoanaly* or ((analytic* or dynamic* or psychodynamic*) near2 (therap* or psychotherap*)))]
2. We searched CINAHL (January 1982 to January 1999) using the Cochrane Schizophrenia Group's terms for both randomised controlled trials and schizophrenia combined with the phrase:
[and (psychoanaly* or ((analytic* or dynamic* or psychodynamic*) near2 (therap* or psychotherap* or "PSYCHOANALYSIS"/ all topical subheadings / all age subheadings or explode "PSYCHOANALYTIC‐THEORY"/ all topical subheadings / all age subheadings)))]
3. We searched The Cochrane Library CENTRAL (Issue 1, 1999) using the Cochrane Schizophrenia Group's terms for randomised controlled trials and for schizophrenia combined with the phrase:
[and (psychoanaly* or explode psychoanalysis(MeSH) or explode psychoanalytic‐therapy(MeSH) or ((analytic* or dynamic* or psychodynamic* or insight‐oriented) and (therap* or psychotherap*)))]
4. We searched Dissertation Abstracts (1866 to December 1999) using the Cochrane Schizophrenia Group's terms for both randomised controlled trials and schizophrenia combined with the phrase:
[and ((psychoanaly? or psychotherap?) or ((analytic or dynamic or psychodynamic) and therap?))]
5. We searched EMBASE (January 1980 to January 1999) using the Cochrane Schizophrenia Group's terms for both randomised controlled trials and schizophrenia combined with the phrase:
[and (psychoanaly* or ((analytic* or dynamic* or psychodynamic*) near2 (therap* or psychotherap* or "PSYCHOANALYTIC‐THEORY"/ all subheadings or "PSYCHOANALYSIS"/ all subheadings)))]
6. We searched MEDLINE (January 1966 to January 1999) using the Cochrane Schizophrenia Group's terms for both randomised controlled trials and schizophrenia combined with the phrase:
[and (exp psychoanalysis/all subheadings or exp psychoanalytic therapy/all subheadings or (psychoanaly* or ((analytic* or dynamic* or psychodynamic*) near2 (therap* or psychotherap*))))]
7. We searched National Research Register (August 2000) using the term:
[randomi* [and (psychoanaly* or explode psychoanalysis(MeSH) or explode psychoanalytic‐therapy(MeSH) or ((analytic* or dynamic* or psychodynamic* or insight‐oriented) and (therap* or psychotherap*)))]
8. We searched PsycLIT (January 1974 to January 1999) using the Cochrane Schizophrenia Group's terms for both randomised controlled trials and schizophrenia combined with the phrase:
[and (psychoanaly* or ((analytic* or dynamic* or psychodynamic*) near2 (therap* or psychotherap*or explode "PSYCHOANALYSIS" or explode "PSYCHOANALYSTS" or "PSYCHODYNAMICS‐" IN DE")))]
9. We searched Sociofile (January 1974‐October 1998) using the Cochrane Schizophrenia Group's terms for both randomised controlled trials and schizophrenia combined with the phrase:
[and ((psychoanaly* or psychotherap*) or ((analytic or dynamic or psychodynamic) and therap*))]
10. Searching other resources 10.1 Unjpublished studies We appealed to practitioners on the Psych‐couns mailbase list (http://www.mailbase.ac.uk/lists/psych‐couns/) in June 1999 for unpublished studies.
Appendix 2. Risk of bias assessed in earlier versions of this review
We assessed the methodological quality of included studies using the criteria described in the Cochrane Handbook (Higgins 2008) which is based on the degree of allocation concealment. Poor concealment has been associated with overestimation of treatment effect (Schulz 1995). Category A includes studies in which allocation has been randomised and concealment is explicit. Category B studies are those which have randomised allocation but in which concealment is not explicit. Category C studies are those in which allocation has neither been randomised nor concealed. Only trials that are stated to be randomised (categories A or B of the handbook) will be included in this review. The categories are defined below:
A. Low risk of bias (adequate allocation concealment) B. Moderate risk of bias (some doubt about the results) C. High risk of bias (inadequate allocation concealment).
When disputes arose as to which category a trial should be allocated, again resolution was attempted by discussion. When this was not possible we did not enter the data and the trial was added to the list of those awaiting assessment until further information could be obtained.
Data and analyses
Comparison 1. INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY versus MEDICATION.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Committed suicide by three years | 1 | 94 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.05, 5.56] |
| 2 Global impression: 1. Not able to be discharged (long term) | 1 | 94 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.35 [2.03, 34.30] |
| 3 Global impression: 2. Given medication during 12 months to three years follow up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 by 12 months | 1 | 94 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.50, 0.81] |
| 3.2 by three years | 1 | 94 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.75, 0.96] |
| 4 Global impression: 3. Achieved best level of health MHSS ‐ long term (high=good) | 1 | 92 | Mean Difference (IV, Fixed, 95% CI) | 5.80 [1.61, 9.99] |
| 5 Global impression: 4. Treatment not considered successful by treatment team (long term) | 1 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 16.36 [2.25, 118.81] |
| 6 Global impression: 5. Hospital re‐admission (long term) | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.29, 1.36] |
| 7 Leaving the study early (long term) | 1 | 94 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.28, 3.93] |
Comparison 2. INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY AND MEDICATION versus MEDICATION ALONE.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Committed suicide by three years | 1 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.01, 2.93] |
| 2 Global impression: 1. Not able to be discharged (long term) | 1 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.16, 7.42] |
| 3 Global impression: 2. Given medication during 12 months to three years follow up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 by 12 months | 1 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.85, 1.06] |
| 3.2 by three years | 1 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.88, 1.03] |
| 4 Global impression: 3. Achieved best level of health ‐ MHSS ‐ high=good (long term) | 1 | 90 | Mean Difference (IV, Fixed, 95% CI) | ‐0.80 [‐5.35, 3.75] |
| 5 Global impression: 4. Treatment not considered successful by treatment team (long term) | 1 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.18 [0.20, 23.23] |
| 6 Global impression: 5. Hospital re‐admission (long term) | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.39, 2.58] |
| 7 Leaving the study early (long term) | 1 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.19, 3.45] |
Comparison 3. INSIGHT‐ORIENTED PSYCHODYNAMIC PSYCHOTHERAPY versus REALITY‐ADAPTIVE PSYCHOTHERAPY.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Global impression: 1. Not able to perform major household responsibilities (long term) | 1 | 164 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.99, 1.29] |
| 2 Global impression: 2. Not able to enjoy a significant relationship (long term) | 1 | 164 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.96, 1.21] |
| 3 Global impression: 3. Not self supporting (long term) | 1 | 164 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.90, 1.23] |
| 4 Global impression: 4. Hospital re‐admission (long term) | 1 | 164 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.93, 1.56] |
| 5 Leaving the study early: | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 at six months | 1 | 164 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.31, 0.68] |
| 5.2 at 12 months | 1 | 164 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.34, 0.62] |
| 5.3 at 24 months | 1 | 164 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.44, 0.67] |
3.3. Analysis.
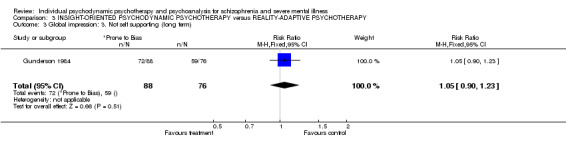
Comparison 3 INSIGHT‐ORIENTED PSYCHODYNAMIC PSYCHOTHERAPY versus REALITY‐ADAPTIVE PSYCHOTHERAPY, Outcome 3 Global impression: 3. Not self supporting (long term).
3.4. Analysis.
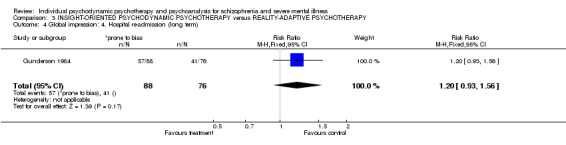
Comparison 3 INSIGHT‐ORIENTED PSYCHODYNAMIC PSYCHOTHERAPY versus REALITY‐ADAPTIVE PSYCHOTHERAPY, Outcome 4 Global impression: 4. Hospital re‐admission (long term).
3.5. Analysis.
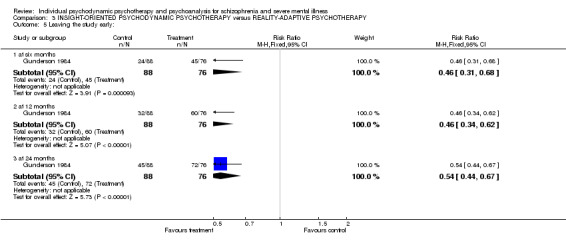
Comparison 3 INSIGHT‐ORIENTED PSYCHODYNAMIC PSYCHOTHERAPY versus REALITY‐ADAPTIVE PSYCHOTHERAPY, Outcome 5 Leaving the study early:.
Comparison 4. INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY versus GROUP PSYCHOTHERAPY.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Global impression: 1. Returned to hospital (long term) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 at 12 months | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.58, 1.98] |
| 1.2 at 24 months | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.72, 1.86] |
| 2 Global impression: 2. Not improved at 24 months | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.96, 1.67] |
| 3 Global impression: 3. Discharged from therapy (long term) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 at 12 months | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.18, 3.18] |
| 3.2 at 24 months | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.6 [0.33, 1.09] |
| 4 Global impression: 4. Remaining in therapy (long term) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 at 12 months | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.46, 1.00] |
| 4.2 at 24 months | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.20, 1.54] |
4.2. Analysis.
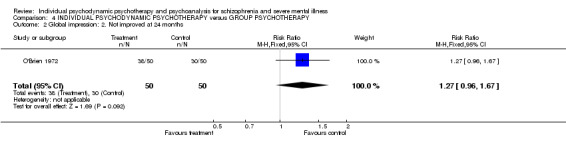
Comparison 4 INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY versus GROUP PSYCHOTHERAPY, Outcome 2 Global impression: 2. Not improved at 24 months.
4.3. Analysis.
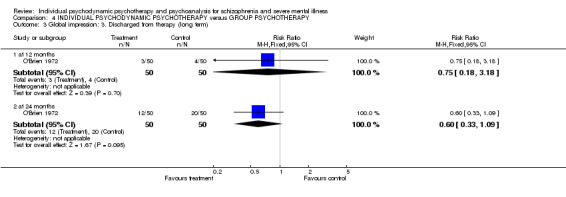
Comparison 4 INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY versus GROUP PSYCHOTHERAPY, Outcome 3 Global impression: 3. Discharged from therapy (long term).
4.4. Analysis.
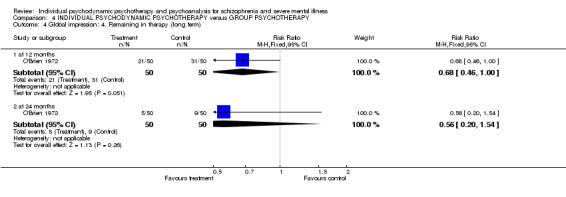
Comparison 4 INDIVIDUAL PSYCHODYNAMIC PSYCHOTHERAPY versus GROUP PSYCHOTHERAPY, Outcome 4 Global impression: 4. Remaining in therapy (long term).
Comparison 5. INDIVIDUAL PSYCHODYNAMIC THERAPY AND MEDICATION versus INDIVIDUAL PSYCHODYNAMIC THERAPY.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Global impression: 1. Hospital re‐admission (long term) | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.39, 2.58] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Gunderson 1984.
| Methods | Allocation: randomised, no further details. Blindness: open study. Duration: two years, had to stay in therapy for six months to be eligible to go on to two year follow up. Setting: all hospitalised initially, then in community. | |
| Participants | Diagnosis: schizophrenia (DSM II & III) diagnosis confirmed three times. N=164 (almost 2000 screened). Age:18 to 35 years. Sex: not reported. Inclusion criteria: minimal prior treatment, no drug or alcohol problems, no organic illnesses, able to function outside of hospital for four consecutive months in some major role without medication in the previous two years. | |
| Interventions | 1. Insight‐oriented psychotherapy. N=88*. 2. Reality‐adaptive, supportive psychotherapy. N=76*. | |
| Outcomes | Leaving the study early.
Global impression: re‐hospitalised, unable to take household responsibilities, unable to have key relationship, not self supporting. Unable to use ‐ Mental state: cognition, ego functioning (no SD). Signs and symptoms of illness: no SD. Use of medication: no SD. Hospitalisation: no SD. |
|
| Notes | *Gunderson reports randomising 95 people. In earlier report of same study (Stanton 1984) 164 people were said to have been randomised. For the 69 people that left early there are no other available data other than leaving the study early. There are only usable data of 95 people staying in therapy beyond six months. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Randomised, no further details. |
| Allocation concealment? | Unclear risk | No further details. |
| Blinding? All outcomes | High risk | Open study. |
| Incomplete outcome data addressed? All outcomes | High risk | Numbers randomised were not clearly reported. |
| Free of selective reporting? | Unclear risk | No further details. |
| Free of other bias? | Unclear risk | No details. |
Karon 1981.
| Methods | Allocation: randomised, no further details. Blindness: unclear, 'blind outcome evaluations'. Duration: 20 months. Setting: inpatients and outpatients. | |
| Participants | Diagnosis: mostly schizophrenia. N=36. Age: not reported. Sex: not reported. Inclusion criteria: aim to include 'acutely ill, but clearly schizophrenic' participants, first admission. Exclusion criteria: no history of ECT, or insulin shock treatment; no organic brain damage; no history of alcoholism, or drug addiction. History: it later emerged that about one third of participants had been previously hospitalised; range 7 to 72 days, mean 23.7 days. | |
| Interventions | 1. Psychotherapy without medication. N=12. 2. Psychotherapy with medication (phenothiazines, typically 400 mg/day chlorpromazine or equivalent). N=12. 3. Hospital comparison with medication (phenothiazines, typically 400 mg/day chlorpromazine or equivalent). N=12. | |
| Outcomes | Re‐hospitalisation. Unable to use ‐ Cognitive functions: WAIS (no usable data). Days hospitalised: no SD. Leaving the study early: no usable data. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Randomised, no further details. |
| Allocation concealment? | Unclear risk | No further details. |
| Blinding? All outcomes | High risk | Not reported for therapists or participants, probably open design. |
| Incomplete outcome data addressed? All outcomes | High risk | Study attrition not clearly reported. |
| Free of selective reporting? | Unclear risk | No details. |
| Free of other bias? | Unclear risk | No details. |
May 1976.
| Methods | Allocation: randomised, no further details. Blindness: open study. Duration: until discharge or 6 to12 months of treatment. Setting: Camarillo State hospital. Follow up after discharge (and from assigned interventions) up to five years. | |
| Participants | Diagnosis: schizophrenia, no further details. N=228. Age: no details. Sex: men and women. Inclusion criteria: age 16 to 45 years; no evidence of organic brain damage or epilepsy; no major physical illness; no history of alcohol or drug addiction. Exclusions: people who were 'obviously not going to be discharged within two years', and those whose illness went into remission during 18‐day assessment period. History: first admission with no significant prior treatment. | |
| Interventions | 1. Individual psychotherapy. N=46. 2. Ataraxic drugs (trifluoperazine). N=48. 3. Individual psychotherapy and ataraxic drugs. N=44. 4. ECT. N=47. 5. Milieu therapy and ataraxic drugs. N=43. | |
| Outcomes | Leaving the study early.
Global impression: discharge from hospital.
Menninger Health Sickness Scale.
Medication use after discharge.
Best level of functioning.
Usable data available for three years. Unable to use ‐ Relapse: no usable data. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Randomised, no further details. |
| Allocation concealment? | Unclear risk | No further details. |
| Blinding? All outcomes | High risk | Open study. |
| Incomplete outcome data addressed? All outcomes | High risk | Study attrition not reported. |
| Free of selective reporting? | Unclear risk | No details. |
| Free of other bias? | Unclear risk | No details. |
O'Brien 1972.
| Methods | Allocation: randomised, no further details. Blindness: open study. Duration: 20 months. | |
| Participants | Diagnosis: schizophrenia, case notes contained clear evidence of a psychotic episode, no further details. N=100. Age: mean˜37 years. Sex: 39M, 61F. History: newly discharged from acute inpatient care; mean number of hospitalisations ˜ 2.9. | |
| Interventions | 1. Individual psychotherapy. N=50.
2. Group psychotherapy. N=50. All participants on medication at the start of the study. |
|
| Outcomes | Global impression: re‐hospitalisation, not improved, discharged, remaining in therapy. Unable to use ‐ Mental state: BPRS (no usable data), Zung Self Rating Scale (no data). Mental status: Mental Status Scale (no usable data). Social functioning: Social Effectiveness Scale (no usable data). Leaving the study early: no data. |
|
| Notes | Dropped 13 participants from analysis, but it was clear from which groups, so they were added back in in an effort to undertake an intention‐to‐treat analysis. No details of orientation or frequency of sessions. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Random, no further details. |
| Allocation concealment? | Unclear risk | No further details. |
| Blinding? All outcomes | High risk | Open study. |
| Incomplete outcome data addressed? All outcomes | High risk | Study attrition not adequately reported. |
| Free of selective reporting? | Unclear risk | No details. |
| Free of other bias? | Unclear risk | No details. |
BPRS: Brief Psychiatric Rating Scale DCS: Discrimination Criteria for Schizophrenia DSM II & III: Diagnostic and Statistical Manual of Mental Disorders ECT: electroconvulsive therapy EIO: insight‐oriented psychotherapy MHSS: Menninger Health Sickness Scale RAS: reality‐adaptive supportive psychotherapy
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Appelbaum 1986 | Allocation: not randomised, description of organisation of psychotherapy wards. |
| Armstrong 1991 | Allocation: randomised. Participants: unclear. Interventions: life skills programme in day hospital versus supportive psychotherapeutic milieu in day hospital; not psychoanalytic or psychodynamic therapy. |
| Azima 1959 | Allocation: unclear. Methods: drugs given and observations collected using a double‐blind method, likely A‐B‐C‐A crossover trial. Interventions: phenobarbital or reserpine, not psychodynamic therapy. |
| Bellak 1973 | Allocation: not randomised, case report. |
| Cancro 1987 | Allocation: not randomised, review. |
| Carpenter 1984 | Allocation: not randomised, review. |
| Carpenter 1993 | Allocation: not randomised, review. |
| Chiesa 1999 | Allocation: random. Participants: not people with schizophrenia. |
| Chodoff 1982 | Allocation: not randomised, review. |
| Cormier 1987 | Allocation: not randomised, before and after study. |
| De Socarraz 1978 | Allocation: random. Participants: neurotic patients, not people with schizophrenia. |
| Docherty 1984 | Allocation: not randomised, review. |
| Dyrud 1973 | Allocation: not randomised, review. |
| Epstein 1981 | Allocation: not randomised, review. |
| Falloon 1983 | Allocation: random. Participants: people with schizophrenia. Intervention: family therapy and supportive individual therapy, not psychodynamic therapy. |
| Friedman 1973 | Allocation: not randomised, review. |
| Gabbard 1997 | Allocation: not randomised, review. |
| Gillieron 1980 | Allocation: not randomised, survey and factorial analysis of a questionnaire. |
| Glick 1974 | Allocation: randomised. Participants: people with schizophrenia. Interventions: short versus long hospitalisation, not psychoanalytic therapy. |
| Green 1984 | Allocation: randomised. Participants: people with schizophrenia. Interventions: type of psychotherapy, no further details (author contacted, no reply). |
| Guthrie 1997 | Allocation: random. Participants: people without psychosis (personal communication from Dr Guthrie). |
| Harding 1994 | Allocation: not randomised, review. |
| Hogarty 1997 | Allocation: random, no further details. Participants: people with schizophrenia or schizoaffective disorder. N=186. Interventions: personal therapy, family psycho‐education, combined personal therapy and family psycho‐education or supportive therapy. Personal therapy seemed to have a definition akin to cognitive behavioural therapy. "Through a process called 'internal coping', personal therapy encouraged the patient to identify the affective, cognitive and physiological experience of stress." |
| Jones 2001 | Allocation: randomised. Participants: people with auditory hallucinations. Interventions: cognitive behavioural therapy versus standard care, not psychodynamic therapy. |
| Kaplan 1985 | Allocation: not randomised. |
| Karon 1969 | Allocation: randomised. Participants: people with schizophrenia. Interventions: psychoanalytic individual therapy versus ego analytic therapy versus supportive psychotherapy versus medication. Outcomes: psychological tests (Thorndyke Gallup Vocabulary, Porteus Mazes, WAIS IQ test, VVT), use of medication (no usable data). |
| Karon 1984 | Allocation: not randomised, review. |
| Klerman 1984 | Allocation: not randomised, review. |
| Krull 1987 | Allocation: not randomised, review. |
| Lindberg 1981 | Allocation: non randomised, matched pairs retrospective study. |
| Luborsky 1975 | Allocation: not randomised, review. |
| Matthews 1981 | Allocation: randomised. Participants: people with schizophrenia. Interventions: practitioners 'A' versus practitioners 'B' (according to level of experience in psychotherapy). Outcomes: no usable data. |
| Matussek 1974 | Allocation: not randomised, cohort study. |
| May 1984 | Allocation: not randomised, review. |
| Mueser 1990 | Allocation: not randomised, review and editorial. |
| Muller 1978 | Allocation: not randomised, review. |
| Muller 1984 | Allocation: not randomised, review. |
| Res. committee 1975 | Allocation: not randomised, review. |
| Resch 1994 | Allocation: not randomised, review. |
| Roback 1972 | Allocation: randomised. Participants: men, n=24 (20 diagnosed with schizophrenia). Interventions: interpretive group therapy versus interactive group therapy. Outcomes: self rating of insight, psychometric tests (no usable data). |
| Rogers 1967 | Allocation: randomised. Participants: people with schizophrenia, with people without schizophrenia as controls. Interventions: therapeutic relationships, no psychodynamic therapy. |
| Rohriht 2001 | Allocation: randomised. Participants: people with schizophrenia. Interventions: body‐oriented psychotherapeutic intervention versus standard care; body‐oriented psychotherapy have as their primary principle to overcome communication barriers through the introduction of non‐verbal techniques; not psychoanalytic or psychodynamic therapy. |
| Rubins 1974 | Allocation: not randomised, review. |
| Schachter 2001 | Allocation: random. Participants: unclear if schizophrenia. |
| Schneider 1993 | Allocation: not randomised, review. |
| Scott 1995 | Allocation: not randomised, review. |
| Silverman 1978 | Allocation: not randomised, review. |
| Sines 1961 | Allocation: participants allocated to 'psychiatric aides'. Participants: 40 people with schizophrenia, 7 "mental defectives" and 13 other diagnoses. Interventions: twice weekly meetings of 50 minutes for the purpose of 'improving the patients psychiatric and behavioural status'; during the 50 minutes, aides engaged in various activities, none of which resembled psychodynamic therapy. |
| Sjostrom 1990 | Allocation: randomised. Participants: people with schizophrenia. Intervention: psychotherapy with dynamic elements versus standard care. Outcomes: no usable data. |
| Stevens 1973 | Allocation: not randomised. |
| Sverdlov 1980 | Allocation: not randomised. |
| Tarrier 1999 | Allocation: randomised. Participants: people with chronic schizophrenia suffering residual psychotic symptoms. Interventions: cognitive behavorial psychotherapy. |
| Tienari 1986 | Allocation: not randomised, review. |
| Volterra 1996 | Allocation: randomised. Participants: people with schizophrenia. Intervention: group and individual psychotherapy (plus haloperidol 2 mg/day) versus drug treatment alone. Outcome: no data available (Congress abstract). |
| Vora 1977 | Allocation: randomised. Participants: clinic attenders who received therapy in excess of one year, 53% neurotic, 47% either psychotic or characterological disorders, data not presented for people with schizophrenia alone. |
| Werbart 1988 | Allocation: not randomised, review. |
| Young 1979 | Allocation: randomised. Participants: people with schizophrenia (n=141) and 94 with other diagnoses. Interventions: long versus short hospitalisation and therapists A‐B‐scores, not psychodynamic psychotherapy. |
Characteristics of studies awaiting assessment [ordered by study ID]
Wilner 1985.
| Methods | Randomised |
| Participants | Unknown |
| Interventions | Unknown |
| Outcomes | Unknown |
| Notes |
Differences between protocol and review
Upgrade of review into RevMan 5 resulted in changed order of text within 'Methods' section but no fundamental changes to the conduct of the review or the update.
Contributions of authors
Lena Malmberg ‐ prepared protocol, selected and acquired studies, extracted data, summated data, produced report. Mark Fenton ‐ prepared protocol, selected studies, extracted data, summated data, produced report. John Rathbone ‐ selected studies, extracted data, summated data, produced report.
Sources of support
Internal sources
Porvoo Hospital, Finland.
Cochrane Schizophrenia Group, UK.
External sources
Finnish Office for Health Technology Assessment (FinOHTA ), Finland.
Finska Läkaresällskapet, Finland.
Declarations of interest
Mark Fenton: has been a patient in both individual and group psychoanalytic psychotherapy and worked as a nurse psychotherapist in the National Health System (UK) and believes that psychoanalytic treatment has a place in any healthcare system. Lena Malmberg: works as a doctor on a psychodynamically‐oriented rehabilitation unit for patients living in the community with schizophrenia in Porvoo, Finland. John Rathbone: none known.
Edited (no change to conclusions)
References
References to studies included in this review
Gunderson 1984 {published data only}
- Frank AF, Gunderson JG. The role of the therapeutic alliance in the treatment of schizophrenia. Relationship to course and outcome. Archives of General Psychiatry 1990;47:228‐36. [DOI] [PubMed] [Google Scholar]
- Gunderson JG, Frank AF. Effects of psychotherapy in schizophrenia. Yale Journal of Biological Medicine 1985;58(4):373‐81. [PMC free article] [PubMed] [Google Scholar]
- Gunderson JG, Frank AF, Katz HM, Vannicelli ML, Frosch JP, Knapp PH. Effects of psychotherapy in schizophrenia. II. Comparative outcome of two forms of treatment. Schizophrenia Bulletin 1984;10(4):564‐98. [DOI] [PubMed] [Google Scholar]
- Stanton AH, Gunderson JG, Knapp PH, Frank AF, Vannicelli ML, Schnitzer R, Rosenthal R. Effects of psychotherapy in schizophrenia. I. Design and implementation of a controlled study. Schizophrenia Bulletin 1984;10(4):520‐63. [DOI] [PubMed] [Google Scholar]
Karon 1981 {published data only}
- Karon BP, Vandenbos GR. Psychotherapy of schizophrenia: The treatment of choice. Psychoanalytic Review 1981;71:505‐7. [Google Scholar]
May 1976 {published data only}
- May PR, Tuma AH. The Paul H. Hoch award lecture: a follow up study of the results of treatment of schizophrenia. Proceedings of the Annual Meeting of the American Psychopathological Association 1976;64:256‐84. [MEDLINE: ] [PubMed] [Google Scholar]
- May PR, Tuma AH. Treatment of schizophrenia: an experimental study of five treatments. British Journal of Psychiatry 1965;111:503‐10. [Google Scholar]
- May PR, Tuma AH, Dixon WJ. Schizophrenia: a follow‐up study of results of treatment. I. Design and other problems. Archives of General Psychiatry 1976;33(4):474‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- May PR, Tuma AH, Dixon WJ. Schizophrenia: a follow‐up study of the results of five forms of treatment. Archives of General Psychiatry 1981;38(7):776‐84. [DOI] [PubMed] [Google Scholar]
- May PR, Tuma AH, Dixon WJ, Yale C, Theile DA, Kraude WH. Schizophrenia: a follow‐up study of results of treatment. II. Hospital stay over two to five years. Archives of General Psychiatry 1976;33(4):481‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Tuma AH, May PR, Yale C, Forsythe AB. Therapist characteristics and the outcome of treatment in schizophrenia. Archives of General Psychiatry 1978;35:81‐5. [DOI] [PubMed] [Google Scholar]
- Tuma AH, May PR, Yale C, Forsythe AB. Therapist experience, general clinical ability, and treatment outcome in schizophrenia. Journal of Consulting and Clinical Psychology 1978;46(5):1120‐6. [DOI] [PubMed] [Google Scholar]
- Tuma H, May P. Psychotherapy, drugs and therapist experience in the treatment of schizophrenia: a critique of the Michigan State Project. Psychotherapy Theory, Research and Practice 1975;12(2):138‐42. [Google Scholar]
O'Brien 1972 {published data only}
- Mintz J, O'Brien C, Luborsky L. Predicting the outcome of psychotherapy for schizophrenics: relative contributions of patient, therapist, and treatment characteristics. Archives of General Psychiatry 1976;33(10):1183‐6. [DOI] [PubMed] [Google Scholar]
- O'Brien CP, Hamm KB, Ray BA, Pierce JF. Group versus individual psychotherapy with schizophrenics. Archives of General Psychiatry 1972;27:474‐8. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Appelbaum 1986 {published data only}
- Appelbaum AH, Munich RL. Reinventing moral treatment: the effects upon patients and staff members of a program of psychosocial rehabilitation. Psychiatric Hospital 1986;17(1):11‐9. [PubMed] [Google Scholar]
Armstrong 1991 {published data only}
- Armstrong HE, Cox GB, Short BA, Allmon DJ. A comparative evaluation of two day treatment programs. Psychosocial Rehabilitation Journal 1991;14(4):53‐67. [Google Scholar]
Azima 1959 {published data only}
- Azima H, Azima FJ, Durost HB. Psychoanalytic formations of effects of reserpine on schizophrenic organization. Archives of General Psychiatry 1959;1:662‐70. [DOI] [PubMed] [Google Scholar]
Bellak 1973 {published data only}
- Bellak L, Chassan JB, Gediman HK, Hurvich M. Ego function assessment of analytic psychotherapy combined with drug therapy. Journal of Nervous and Mental Disease 1973;157(6):465‐9. [DOI] [PubMed] [Google Scholar]
Cancro 1987 {published data only}
- Cancro R. Schizophrenic disturbances [Os disturbios esquizofrenicos]. Jornal Brasileiro de Psiquiatria 1987;36(2):85‐91. [Google Scholar]
Carpenter 1984 {published data only}
- Carpenter WT. A perspective on the psychotherapy of schizophrenia project. Schizophrenia Bulletin 1984;10(4):599‐603. [DOI] [PubMed] [Google Scholar]
Carpenter 1993 {published data only}
- Carpenter WT. Commentary: psychosocial treatment of schizophrenia. Psychiatry 1993;56:301‐5. [DOI] [PubMed] [Google Scholar]
Chiesa 1999 {published data only}
- Chiesa M. Time limited psychosocial intervention with patients with severe personality disorder following short inpatient stay. National Research Register 1999.
Chodoff 1982 {published data only}
- Chodoff P. Assessment of psychotherapy: reflections of a practitioner. Archives of General Psychiatry 1982;39(9):1097‐103. [DOI] [PubMed] [Google Scholar]
Cormier 1987 {published data only}
- Cormier HJ, Allard L, Vaillancourt S, Gingras C. An evaluation of mental health programs for young adult psychotics. [Special issue: community mental health services for the chronically mentally disabled] [Evaluation d'un programme de sante mentale pour jeunes adultes psychotiques]. Canadian Journal of Community Mental Health 1987;6:107‐16. [Google Scholar]
De Socarraz 1978 {published data only}
- Socarraz ML, Randolph DL. Responses given by A and B quasi‐therapists to differing sexual roles in an intropunitive‐neurotic prototype: an analogue study. Journal of Clinical Psychology 1978;34(1):165‐70. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Docherty 1984 {published data only}
- Docherty PJ. O tempora, o mores: directions in research on the psychotherapeutic treatment of schizophrenia. Schizophrenia Bulletin 1984;10(4):621‐3. [DOI] [PubMed] [Google Scholar]
Dyrud 1973 {published data only}
- Dyrud J, Holzman P. The psychotherapy of schizophrenia: does it work?. American Journal of Psychiatry 1973;130(6):670‐3. [DOI] [PubMed] [Google Scholar]
Epstein 1981 {published data only}
- Epstein N, Vlok L. Research on the results of psychotherapy: a summary of evidence. American Journal of Psychiatry 1981;138(8):1027‐35. [DOI] [PubMed] [Google Scholar]
Falloon 1983 {published data only}
- Falloon I, Razani J, Moss HB, Boyd JL, McGill CW, Pederson J. Community management of schizophrenia. A one‐year study of family and individual therapy [Gemeindenahe Versorgung von Schizophrenen. Eine einjahringe Kontrolluntersuchung bei Familien und Einzeltherapie]. Partnerberatung 1983;20(2‐3):73‐9. [Google Scholar]
- Falloon IRH, Boyd JL, McGill CW, Williamson M, Razani J, Moss HB. Family management in the prevention of morbidity of schizophrenia: clinical outcome of a two‐year longitudinal study. Archives of General Psychiatry 1985;42(9):887‐96. [DOI] [PubMed] [Google Scholar]
- Falloon IRH, McGill CW, Boyd JL, Pederson J. Family management in the prevention of morbidity of schizophrenia: social outcome of a two‐year longitudinal study. Psychological Medicine 1987;17(1):59‐66. [DOI] [PubMed] [Google Scholar]
Friedman 1973 {published data only}
- Friedman R, Gunderson J, Feinsilver D. The psychotherapy of schizophrenia: an NIMH program. American Journal of Psychiatry 1973;130(6):674‐7. [DOI] [PubMed] [Google Scholar]
Gabbard 1997 {published data only}
- Gabbard G, Lazar S, Hornberger J, Spiegel D. The economic impact of psychotherapy: a review. American Journal of Psychiatry 1997;154(2):147‐55. [DOI] [PubMed] [Google Scholar]
Gillieron 1980 {published data only}
- Gillieron E, Bovet J. Evaluation of psychotherapies and osgood's semantic differential: a tentative approach. Psychotherapy and Psychosomatics 1980;33(1‐2):46‐58. [DOI] [PubMed] [Google Scholar]
Glick 1974 {published data only}
- Glick ID, Hargreaves WA, Goldfield M. Short versus long hospitalization: a prospective controlled study. I. The preliminary results of a one‐year follow‐up of schizophrenics. Archives of General Psychiatry 1974;30(3):363‐9. [DOI] [PubMed] [Google Scholar]
- Glick ID, Hargreaves WA, Raskin M, Kutner SJ. Short versus long hospitalization: a prospective controlled study. II. Results for schizophrenic inpatients. American Journal of Psychiatry 1975;132(4):385‐90. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Green 1984 {published data only}
- Green D. The effect of psychotherapy on the schizophrenic's human percept: a study of object representations in schizophrenia. Michigan, USA: Univ. of Michigan State, 1984. [Google Scholar]
Guthrie 1997 {published data only}
- Guthrie E. Cost effectiveness of psychotherapy for treatment resistant psychiatric outpatients. National Research Register 1997.
Harding 1994 {published data only}
- Harding C, Zahniser J. Empirical correction of seven myths about schizophrenia with implications for treatment. Acta Psychiatrica Scandinavica 1994;384:140‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Hogarty 1997 {published data only}
- Hogarty G, Kornblith S, Greenwald D, DiBarry A, Cooley S, Ulrich R. Three‐year trials of personal therapy among schizophrenic patients living with or independent of family. 1. Description of study and effects of relapse rates. American Journal of Psychiatry 1997;154(11):1504‐13. [DOI] [PubMed] [Google Scholar]
Jones 2001 {published data only}
- Jones P. INSIGHT ‐ Institute ‐ Nottingham ‐ Salford Investigation of group hallucinations treatment. National Research Register 2001.
Kaplan 1985 {published data only}
- Kaplan R, Thornton P, Silverman L. Further data on the effects of subliminal symbiotic stimulation on schizophrenics. Journal of Nervous and Mental Diseases 1985;173(11):658‐66. [DOI] [PubMed] [Google Scholar]
Karon 1969 {published data only}
- Karon BP, VandenBos GR. Intellectual test changes in schizophrenic patients in the first six months of treatment. Psychotherapy Theory Research and Practice 1969;6(2):88‐96. [Google Scholar]
- Karon BP, Vandenbos GR. Experience, medication and the effectiveness of psychotherapy with schizophrenics. British Journal of Psychiatry 1970;116:427‐8. [DOI] [PubMed] [Google Scholar]
- Karon BP, Vandenbos GR. The consequences of psychotherapy for schizophrenia patients. Psychotherapy Theory Research and Practice 1972;9(2):111‐9. [Google Scholar]
- Karon BP, Vandenbos GR. Thought disorder in schizophrenia, length of hospitalization, and clinical status ratings: validity for the Feldman‐Drasgow Visual‐Verbal Test. Journal of Clinical Psychology 1974;30(3):264‐6. [DOI] [PubMed] [Google Scholar]
Karon 1984 {published data only}
- Karon BP. The fear of reducing medication, and where have all the patients gone?. Schizophrenia Bulletin 1984;10(4):613‐7. [DOI] [PubMed] [Google Scholar]
Klerman 1984 {published data only}
- Klerman GL. Ideology and science in the individual psychotherapy of schizophrenia. Schizophrenia Bulletin 1984;10(4):608‐12. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Krull 1987 {published data only}
- Krull, F. Individual psychotherapy of schizophrenia: a review of theories and therapeutic practice [Psychotherapie bei schizophrenie: theorie und praxis der einzelbehandlung: eine Übersicht]. Fortschritte der Neurologie Psychiatrie 1987;55(2):54‐67. [DOI] [PubMed] [Google Scholar]
Lindberg 1981 {published data only}
- Lindberg D. A controlled study of five years' treatment with psychotherapy in combination with depot neuroleptics in schizophrenia. II. Personality changes measured by ten selected rorschach variables. Acta Psychiatrica Scandinavica 1981;Suppl 289:56‐66. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Lindberg D. Personality changes in chronic schizophrenic patients during five years' treatment with intensive psychotherapy in combination with depot neuroleptics. I. Analysis of changes as measured by the Holtzman Inkblot Technique. Acta Psychiatrica Scandinavica 1981;Suppl 289:27‐55. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Luborsky 1975 {published data only}
- Luborsky L, Singer B, Luborsky L. Comparative studies of psychotherapies. Is it true that "everywon has one and all must have prizes"?. Archives of General Psychiatry 1975;32(8):995‐1008. [DOI] [PubMed] [Google Scholar]
Matthews 1981 {published data only}
- Matthews J. The process and outcome of therapy of outpatient schizophrenics by A and B therapists: does psychotherapy add to the effects of psychopharmacotherapy?. Auburn, USA: Univ. of Auburn, 1981. [Google Scholar]
Matussek 1974 {published data only}
- Matussek P, Triebel A. The effectiveness of psychotherapy in 44 schizophrenics [Die wirksamkeit der psychotherapie bei 44 schizophrenen]. Nervenarzt 1974;45:569‐75. [PubMed] [Google Scholar]
May 1984 {published data only}
- May P. A step forward in research on psychotherapy of schizophrenia. Schizophrenia Bulletin 1984;10(4):604‐7. [DOI] [PubMed] [Google Scholar]
Mueser 1990 {published data only}
- Mueser KT, Berenbaum H. Psychodynamic treatment of schizophrenia: is there a future?. Psychological Medicine 1990;20(2):253‐62. [DOI] [PubMed] [Google Scholar]
Muller 1978 {published data only}
- Muller P. Depressive syndromes during schizophrenic psychoses [Depressive syndrome im verlauf schizophrener psychosen]. Fortschritte der Medizin 1978;96:1518‐20. [PubMed] [Google Scholar]
Muller 1984 {published data only}
- Muller C. Psychotherapy in schizophrenia: the end of the pioneers' period. Schizophrenia Bulletin 1984;10(4):618‐20. [DOI] [PubMed] [Google Scholar]
Res. committee 1975 {published data only}
- Committee on Research. Pharmacotherapy and psychotherapy: paradoxes problems and progress. Report/Group for the Advancement of Psychiatry 1975;9(93):263‐434. [MEDLINE: ] [PubMed] [Google Scholar]
Resch 1994 {published data only}
- Resch F. Psychotherapeutic and sociotherapeutic aspects in children and adolescents with schizophrenia [Psychotherapeutische und soziotherapeutische Aspekte bei schizophrenen Psychosen des Kindes‐ und Jugendalters]. Zeitschrift für Kinder‐ und Jugendpsychiatrie 1994;22(4):275‐84. [MEDLINE: ] [PubMed] [Google Scholar]
Roback 1972 {published data only}
- Roback HB. Experimental comparison of outcomes in insight and non insight oriented therapy groups. Journal of Consulting and Clinical Psychology 1972;38(3):411‐7. [DOI] [PubMed] [Google Scholar]
Rogers 1967 {published data only}
- Rogers C, Gendlin E, Kiesler DJ, Truax CB. In: Rogers C editor(s). The therapeutic relationship and its impact: a study of psychotherapy with schizophrenics. Madison, Milwaukee, and London: The University of Wisconsin Press, 1967:23‐366. [Google Scholar]
Rohriht 2001 {published data only}
- Rohriht F. RCT in effectiveness of body oriented psychotherapy on anergia in patients with chronic schizophrenia. National Research Register 2001.
Rubins 1974 {published data only}
- Rubins J, Rucker M. On evaluating the effectiveness of psychoanalytic therapy for the acute schizophrenias. American Journal of Psychoanalysis 1974;34(3):241‐56. [Google Scholar]
Schachter 2001 {published data only}
- Schachter J. Multi‐centre study: the effectiveness of psychodynamic psychotherapy: an ongoing evaluation of treatment. National Research Register 2001.
Schneider 1993 {published data only}
- Schneider L. Efficacy of treatment for geropsychiatric patients with severe mental illness. Psychopharmacology Bulletin 1993;29(4):501‐24. [PubMed] [Google Scholar]
Scott 1995 {published data only}
- Scott JE, Dixon LB. Psychological interventions for schizophrenia. Schizophrenia Bulletin 1995;21(4):621‐30. [DOI] [PubMed] [Google Scholar]
Silverman 1978 {published data only (unpublished sought but not used)}
- Silverman LH. Unconscious symbiotic fantasy: A ubiquitous therapeutic agent. International Journal of Psychoanalytic Psychotherapy 1978;79(7):562‐85. [MEDLINE: ] [PubMed] [Google Scholar]
Sines 1961 {published data only}
- Sines LK, Silver RJ, Lucero RJ. The effect of therapeutic intervention by untrained therapists. Journal of Clinical Psychology 1961;17(4):394‐6. [Google Scholar]
Sjostrom 1990 {published data only}
- Sjostrom R. Psychotherapy in schizophrenia: a prospective study [Psykoterapi vid schizofreni: en prospektiv studie]. Läkartidningen 1990;87:3279‐82. [PubMed] [Google Scholar]
Stevens 1973 {published data only}
- Stevens BC. Evaluation of rehabilitation for psychotic patients in the community. Acta Psychiatrica Scandinavica 1973;49:169‐80. [DOI] [PubMed] [Google Scholar]
Sverdlov 1980 {published data only}
- Sverdlov L. Clinico‐psychopathological and clinico‐psychological analyses of the process of formation of therapeutic remission in acute schizophrenic psychoses. Trudy Leningradskogo Nauchno Issledovatel'skogo Psikhonevrologicheskogo Instituta im VM Bekhtereva 1980;95:48‐60. [Google Scholar]
Tarrier 1999 {published data only}
- Tarrier N. A psychological intervention programme to reduce positive symptoms and prevent relapse in psychotic patients. National Research Register 1999.
Tienari 1986 {published data only}
- Tienari P. Psychotherapy research on schizophrenia. Psychiatria Fennica 1986;17:127‐35. [Google Scholar]
Volterra 1996 {published data only}
- Volterra V, Ronchi D, Belelli G, Ruggeri M, Borsetti G, Cotani P. Effects of psychodynamic therapy in schizophrenic patients. Proceeding of the 10th World Congress of Psychiatry;1996 Aug 23‐28; Madrid. Madrid, 1996.
- Volterra V, Ronchi D, Belelli G, Ruggeri M, Lunardi A. Effects of psychodynamic therapy in schizophrenic patients. Proceedings of the 149th Annual Meeting of the American Psychiatric Association;1996 May 4‐9; New York. New York, 1996.
Vora 1977 {published data only}
- Vora S, Layman WA, Mann ET, Danesino A. The effects of long‐term psychotherapy on patients' self‐perception. Diseases of the Nervous System 1977;38(9):717‐21. [MEDLINE: ] [PubMed] [Google Scholar]
Werbart 1988 {published data only}
- Werbart A. Guidelines for qualitative analysis in clinical evaluation research [Riktlinjer för kvalitativ analys vid klinisk utvärderingsforskning]. Psykisk Hälsa 1988;29(1):40‐4. [Google Scholar]
Young 1979 {published data only}
- Young RC, Glick ID, Hargreaves WA, Braff D, Drues J. Therapist A‐B score and treatment outcome with psychiatric in patients: a table of random numbers. British Journal of Medical Psychology 1979;52(2):119‐21. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Wilner 1985 {published data only}
- Wilner D, Freeman H, Surber M, Goldstein M. Success in mental health treatment interventions: a review of 211 random assignment studies. Journal of Social Service Research 1985;8(4):1‐21. [Google Scholar]
Additional references
Alanen 1997
- Alanen YO. Schizophrenia: its origins and need‐adapted treatment. London: Karnac Books, 1997. [Google Scholar]
Altman 1996
- Altman DG, Bland JM. Detecting skewness from summary information. BMJ 1996;313:1200. [MEDLINE: ; IPPP020600] [DOI] [PMC free article] [PubMed] [Google Scholar]
Begg 1996
- Begg C, Cho M, Eastwood S, Horton R, Moher D, Olkin I, Pitkin R, Rennie D, Schulz KF, Simel D, Stroup DF. Improving the quality of randomized controlled trials. The CONSORT statement. JAMA 1996;276:637‐9. [DOI] [PubMed] [Google Scholar]
Bland 1997
- Bland JM. Statistics notes. Trials randomised in clusters. BMJ 1997;315:600. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boissel 1999
- Boissel JP, Cucherat M, Li W, Chatellier G, Gueyffier F, Buyse M, Boutitie F, Nony P, Haugh M, Mignot G. The problem of therapeutic efficacy indices. 3. Comparison of the indices and their use. Therapie 1999;54(4):405‐11. [PubMed] [Google Scholar]
Carpenter 1994
- Carpenter WT Jr, Buchanan RW. Schizophrenia. New England Journal of Medicine 1994;330:681‐90. [DOI] [PubMed] [Google Scholar]
Chalmers 1983
- Chalmers TC, Celano P, Sacks HS, Smith H Jr. Bias in treatment assignment in controlled clinical trials. New England Journal of Medicine 1983;309:1358‐61. [DOI] [PubMed] [Google Scholar]
Deeks 2000
- Deeks J. Issues in the selection for meta‐analyses of binary data. Proceeding of the 8th International Cochrane Colloquium; 2000 Oct 25‐28th; Cape Town, South Africa. Cape Town, 2000.
Divine 1992
- Divine GW, Brown JT, Frazier LM. The unit of analysis error in studies about physicians' patient care behavior. Journal of General Internal Medicine 1992;7(6):623‐9. [DOI] [PubMed] [Google Scholar]
Donner 2002
- Donner A, Klar N. Issues in the meta‐analysis of cluster randomized trials. Statistics in Medicine 2002;21:2971‐80. [DOI] [PubMed] [Google Scholar]
Duggan 2005
- Duggan L, Fenton M, Rathbone J, Dardennes R, El‐Dosoky A, Indran S. Olanzapine for schizophrenia. Cochrane Database of Systematic Reviews 2005, Issue 2. [DOI: 10.1002/14651858.CD001359.pub2] [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elbourne 2002
- Elbourne DR, Altman DG, Higgins JP, Curtin F, Worthington HV, Vail A. Meta‐analyses involving cross‐over trials:Sulpiride versus placebo for schizophrenia18 / 22methodological issues. International journal of epidemiology 2002;31(1):140‐9. [DOI] [PubMed] [Google Scholar]
Essali 2009
- Essali A, Al‐Haj Haasan N, Li C, Rathbone J. Clozapine versus 'typical' neuroleptic medication for schizophrenia. Cochrane Database of Systematic Reviews 2009, Issue 1. [DOI: 10.1002/14651858] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fenton 1995
- Fenton WS, McGlashan TH. Schizophrenia: individual psychotherapy. In: Kaplan H, Sadock B editor(s). Comprehensive textbook of psychiatry. Baltimore, MD: Williams and Wilkins, 1995. [Google Scholar]
Gulliford 1999
- Gulliford MC. Components of variance and intraclass correlations for the design of community‐based surveys and intervention studies: data from the Health Survey for England 1994. American Journal of Epidemiology 1999;149:876‐83. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 5.0.1 [updated September 2008]. The Cochrane Collaboration 2008.
Hunter 2003
- Hunter R, Kennedy E, Song F, Gadon L, Irving CB. Risperidone versus typical antipsychotic medication for schizophrenia. Cochrane Database of Systematic Reviews 2003, Issue 2. [DOI: 10.1002/14651858] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jones 1999
- Jones C, Cormac I, Mota J, Campbell C. Cognitive behaviour therapy for schizophrenia. Cochrane Database of Systematic Reviews 1999, Issue 1. [DOI: 10.1002/14651858] [DOI] [PubMed] [Google Scholar]
Jones 2004
- Jones C, Cormac I, Silveira da Mota Neto JI, Campbell C. Cognitive behaviour therapy for schizophrenia. Cochrane Database of Systematic Reviews 2004, Issue 4. [DOI: 10.1002/14651858] [DOI] [PubMed] [Google Scholar]
Jüni 2001
- Jüni P, Altman DG, Egger M. Systematic reviews in health care: Assessing the quality of controlled clinical trials. BMJ 2001;323:42‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kay 1986
- Kay SR, Opler LA, Fiszbein A. Positive and negative syndrome scale (PANSS) manual. North Tonawanda (NY): Multi‐Health Systems, 1986. [Google Scholar]
Lawrie 1998
- Lawrie SM, Abukmeil SS. Brain abnormality in schizophrenia. A systematic and quantitative review of volumetric magnetic resonance imaging studies. British Journal of Psychiatry 1998;172:110‐20. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Leucht 2005a
- Leucht S, Kane JM, Kissling W, Hamann J, Etschel E, Engel R. Clinical implications of Brief Psychiatric Rating Scale Scores. British Journal of Psychiatry 2005;187:366‐71. [DOI] [PubMed] [Google Scholar]
Leucht 2005b
- Leucht S, Kane JM, Kissling W, Hamann J, Etschel E, Engel R. What does the PANSS mean?. Schizophrenia Research 2005;79:231‐8. [DOI] [PubMed] [Google Scholar]
Luborsky 1962
- Luborsky L. Clinicians judgements of mental health: a proposed scale. Archives of General Psychiatry 1962;7:407‐17. [DOI] [PubMed] [Google Scholar]
Malmberg 2001
- Malmberg L, Fenton M. Individual psychodynamic psychotherapy and psychoanalysis for schizophrenia and severe mental illness. Cochrane Database of Systematic Reviews 2001, Issue 3. [DOI: 10.1002/14651858.CD001360.] [DOI] [PMC free article] [PubMed] [Google Scholar]
Marshall 2000
- Marshall M, Lockwood A, Bradley C, Adams C, Joy C, Fenton M. Unpublished rating scales: a major source of bias in randomised controlled trials of treatments for schizophrenia. British Journal of Psychiatry 2000;176:249‐52. [DOI] [PubMed] [Google Scholar]
McIntosh 2006
- McIntosh A, Conlon L, Lawrie S, Stanfield AC. Compliance therapy for schizophrenia. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 1998
- Moher D, Pham B, Jones A, Cook DJ, Jadad AR, Moher M, Tugwell P, Klassen TP. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta‐analyses?. Lancet 1998;352:609‐13. [DOI] [PubMed] [Google Scholar]
Moher 2001
- Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel‐group randomised trials. Lancet 2001;357(9263):1191‐94. [PubMed] [Google Scholar]
Overall 1962
- Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychological Reports 1962;10:799‐812. [Google Scholar]
Pharoah 2006
- Pharoah F, Mari J, Rathbone J, Wong W. Family intervention for schizophrenia. Cochrane Database of Systematic Reviews 2006, Issue 4. [DOI: 10.1002/14651858] [DOI] [PubMed] [Google Scholar]
Rust 1989
- Rust J, Golombok S. Modern Psychometrics. London: Routledge, 1989. [Google Scholar]
Sandler 1992
- Sandler J. Reflections on developments in the theory of psychoanalytic technique. International Journal of Psychoanalysis 1992;73(2):189‐98. [MEDLINE: ] [PubMed] [Google Scholar]
Schulz 1995
- Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias: dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408‐12. [DOI] [PubMed] [Google Scholar]
Stanton 1984
- Stanton AH, Gunderson JG, Knapp PH, Frank AF, Vannicelli ML, Schnitzer R, Rosenthal R. Effects of psychotherapy in schizophrenia. I. Design and implementation of a controlled study. Schizophrenia Bulletin 1984;10(4):520‐63. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Thornley 1998
- Thornley B, Adams CE. Content and quality of 2000 controlled trials in schizophrenia over 50 years. BMJ 1998;317:1181‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ukoumunne 1999
- Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ. Methods for evaluating area‐wide and organisation‐based intervention in health and health care: a systematic review. Health Technology Assessment 1999;3(5):1‐75. [PubMed] [Google Scholar]
Xia 2007
- Xia J, Adams CE, Bhagat N, Bhagat V, Bhoopathi P, El‐Sayeh H, Pinfold V, Takriti Y. The Leeds Outcomes Stakeholders Survey (LOSS) Study. Proceedings of the 15th Cochrane Colloquium; 2007 Oct 23‐27; Sao Paulo. 2007.
References to other published versions of this review
Malmberg 1999
- Malmberg L, Fenton M. Individual psychodynamic psychotherapy and psychoanalysis for schizophrenia and severe mental illness. Cochrane Database of Systematic Reviews 2001, Issue 2. [DOI: 10.1002/14651858.CD001360.] [DOI] [PMC free article] [PubMed] [Google Scholar]


